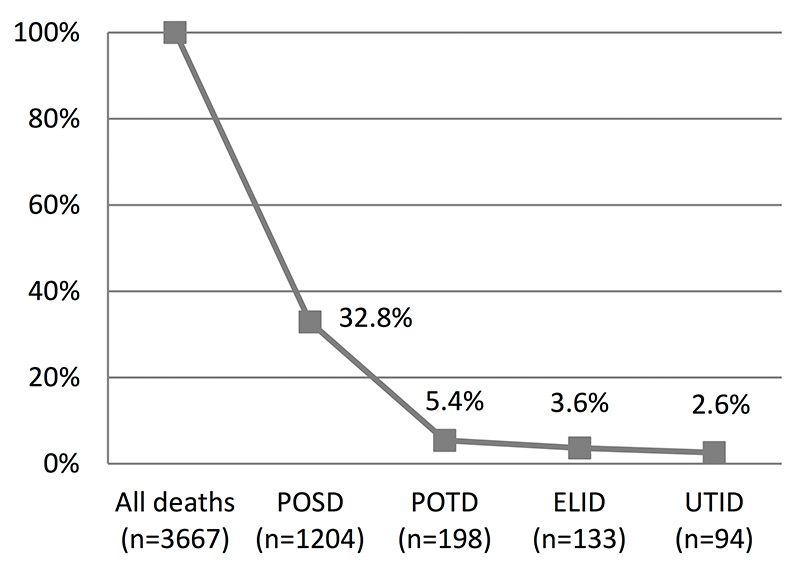
Figure 1
Losses by step in the donation process.
ELID = eligible donor; POSD = possible donor; POTD = potential donor; UTID = utilised donor
DOI: https://doi.org/10.4414/smw.2014.14045
List of abbreviations
A&E accident and emergency department
DBD donation after brain death
DCD donation after circulatory death
CNDO Comité National du Don d’Organes
CVA cerebrovascular accident
ELID eligible donor
ICD-10 International Statistical Classification of Diseases and Related Health Problems, 10th revision
ICU intensive care unit
NOK next of kin
pmp per million of population
POSD possible donor
POTD potential donor
SOAS Swiss Organ Allocation System
SSICM Swiss Society of Intensive Care Medicine
SwissPOD Swiss Monitoring of Potential Organ Donors
UTID utilised donor
Switzerland’s post mortem organ donation rate is one of the lowest in Europe [1]. During the last decade, it remained relatively stable with an average of 12.2 donors per million of population (pmp) and year. In the meantime, the number of patients with end-stage organ disease waiting for a transplant almost doubled [2]. As a consequence, the lack of donor organs severely impacts the patients’ hope for a timely, often lifesaving, transplantation. Moreover, a prolonged waiting time often entails comorbidities in patients (which otherwise might have been prevented), which generally impairs the early outcome.
Organ shortage, however, is not unique to Switzerland, as the lack of organs for transplantation and growing waiting lists are issues prevalent in most countries worldwide [3]. Two main determinants are often referred to as influencing a country’s donation rate, namely the pool of potential donors and consent rate to donation. The number of potential donors seems to be linked to the population age structure, mortality rates from cerebrovascular accident and traumatic brain injury, as well as the availability of intensive care unit (ICU) beds and neurosurgical facilities [4–8]. Various studies have shown that consent to donation might be influenced by legislation (explicit or presumed consent), religious beliefs, cultural influences, or the attitude towards and awareness of organ donation in both healthcare professionals and the public [9–21]. Studies in numerous countries have tried to identify their potential for organ donation and to gain insight into what actions would help to increase the donation rate [5, 7, 8, 12, 22–28]. In addition, targeted initiatives to increase donation rates have been undertaken in some countries showing considerable effect [29–37].
In this context, the Swiss Monitoring of Potential Organ Donors (SwissPOD) was initiated by the Federal Office of Public Health as well as the Swiss university hospitals and transplant centres to investigate the causes of the overall low donation rate in Switzerland. In 2010, Swisstransplant, the Swiss National Foundation for organ donation and transplantation, and the Comité National du Don d’Organes (CNDO) were commissioned with developing the SwissPOD framework and subsequently performing this national study. We present our analysis on deaths in adult ICUs which represented approximately 80% of all deaths registered in the data base. The goal of our study was an assessment of the donation after brain death (DBD) process in Swiss adult ICUs, and to provide an overview of the donation efficiency as well as of the reasons for non-donation.
SwissPOD was designed as a prospective cohort study of all deaths in Swiss ICUs and accident and emergency departments (A&E). Study sites included all 76 hospitals with an ICU recognised by the Swiss Society of Intensive Care Medicine (SSICM) and their associated A&E. Following approval by all cantonal ethics committees and the Eidgenössische Expertenkommission für das Berufsgeheimnis in der medizinischen Forschung (Federal ethics committee), patient data were collected between 1 September 2011 and 31 August 2012. In SwissPOD all patients who died in an ICU or A&E were registered. All deaths under the age of 44 weeks gestation, and all patients who in life refused to participate in a clinical study were excluded.
SwissPOD data were collected using an audit tool which was designed on a hierarchical basis with a series of forms, following the process of organ donation from deceased persons as described in the “Critical Pathway of Deceased Donation” [38]. Patient data were gathered and entered into the web-based system database by the local donor coordinator in each hospital. Data monitors at Swisstransplant, validated and archived each form with any queries being resolved directly with the person who completed the form. Treating clinicians were interviewed if the information in the medical record was not clear. Patient data included basic demographic information, detailed information on the causes of brain injury, and medical suitability for organ donation. Further data were collected on brain death testing and diagnosis, whether organ donation was considered, the process of obtaining consent from next of kin (NOK), and finally regarding whether or not organ donation took place. Information on whether organs were offered for transplantation, and if not why, were extracted from the Swiss Organ Allocation System (SOAS). The presented data include SwissPOD data of patients who died in adult ICU only (≈80% of records). Patients who died in paediatric ICUs or A&Es (≈20%) were excluded from the analysis. Patients who were considered for donation after circulatory death (DCD) were not excluded from the analysis. However, they were counted as a reason for the DBD process to stop, as this study focuses on donation after brain death. This explains why 6 utilised DCD donors (Maastricht category III) are not included in the total of utilised donors.
The primary endpoint of this study was the number of possible, potential, eligible, and utilised DBD donors. Secondary endpoints included reasons for not progressing in the donation process, donation efficiency (consent rate, conversion rate), and point in time of NOK approaches.
Conforming with the definitions in the “Critical Pathway of Deceased Donation” [38], possible endpoints in the DBD process are possible donor (POSD; a patient with a devastating brain lesion or circulatory failure, apparently medically suitable for organ donation), potential donor (POTD; a patient whose clinical conditions are suspected to fulfil brain death criteria), eligible donor (ELID; a patient medically suitable for donation who has been declared dead based on neurological criteria as stipulated by the Swiss Academy of Medical Sciences), and utilised donor (UTID; an ELID with consent for organ donation from whom at least one organ was transplanted).
Absolute contraindications to organ donation as stipulated by the Swiss Transplantation Ordinance are: coma of an unknown origin, unresolved systemic infection or infections from an unknown origin, suspicion or risk of prion disease, suspicion of rabies, degenerative diseases of the nervous system from an unknown origin, and malignancy or <5 year history of treated malignancy (with the exception of carcinoma in situ, primary central nervous system tumours that rarely metastasise outside the nervous system, or low-grade skin tumours with little metastatic capacity such as basocellular carcinoma) [39].
Donation efficiency is assessed by calculating the conversion rate (the number of UTID expressed as a percentage of the number of POTD) and the consent rate (the number of consents to organ donation expressed as a percentage of the total consents and objections). In cases where a patient had a donor card, and the NOK were also asked for consent, only one answer was counted. If the answers were diverging, an objection would always override any consent. This holds also if the patient and/or the NOK consented to donation, but there was a formal objection to donation (e.g., by the coroner). As required by law, patients who neither had a donor card nor NOK were excluded from the donation process.
During the one-year study period, 3,667 patients died in one of the 79 adult ICUs participating in SwissPOD. Of these, 1,204 were POSD, 198 POTD, 133 ELID, and 94 UTID. These four groups were analysed for secondary outcomes and characteristics (table 1). Due to the hierarchical structure of the donation process, patient data of each step are included in the data shown for the previous step (i.e., data of POSD are included in the adult ICU deaths group, data of POTD are included in the POSD group, etc.). Percentages in each column refer to the total number of patients in the respective group.
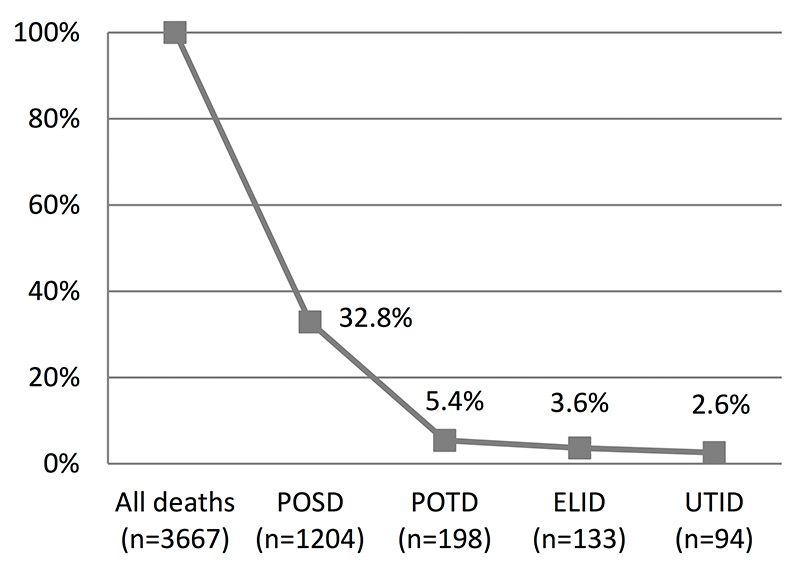
Figure 1
Losses by step in the donation process.
ELID = eligible donor; POSD = possible donor; POTD = potential donor; UTID = utilised donor
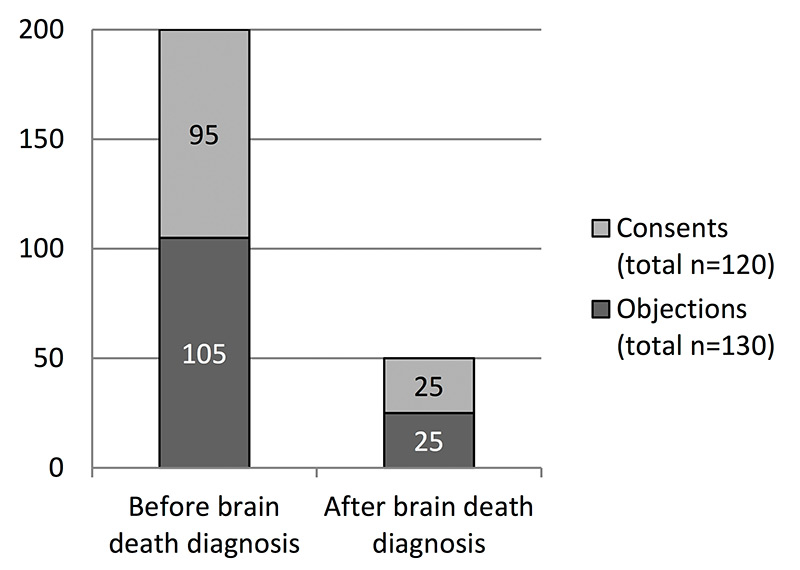
Figure 2
Consent vs objection to donation.
Table 1 shows that, of all ICU adult deaths (n = 3,667), 39.4% were female (n = 1,444) and 60.6% male (n = 2,223). The mean age was 69.8 ± 14.0 years, and average ICU stay was 5.4 ± 9.2 days. An absolute contraindication to organ donation was present in 33.5% of cases (n = 1,227). Of all subjects, 67.3% were ventilated (n = 2,466), and 22.8% were never ventilated (n = 836). Among those who were ventilated, 1,250 had a neurological pathology (34.1% of all deaths, 50.7% of subjects ventilated). In the group of subjects who were never ventilated, 120 had a neurological pathology (3.3% of all deaths, 14.4% of subjects never ventilated). 62.6% (n = 2,297) of patients died of a pathology with non-primary cerebral cause. The principal causes of brain injuries were anoxia/hypoxia or cardiac arrest (20.6%, n = 757), intracranial haemorrhage/ischaemia (12.7%, n = 465), and open/closed traumatic brain injury (3.2 %, n = 118).
On the POSD step (n = 1204), 38.8% of the subjects were female (n = 467) and 61.2% male (n = 737). The mean age was 64.9±15.8 years and the average ICU stay was 3.4±5.0 days. The main causes of brain injury in this group were anoxia / hypoxia or cardiac arrest (45.3%, n = 545), intracranial haemorrhage/ischaemia (32.0%, n = 385), and open / closed traumatic brain injury (8.8%, n = 106).
On the POTD step (n = 198), the proportion of females and males was almost equal (98 vs 100 cases). Compared with the POSD step, the subjects in the POTD group were on average 10.4 years younger (54.5 ± 17.3 years), and the mean ICU stay was clearly shorter (1.7 ± 2.1 days). Intracranial haemorrhage/ischaemia was the main cause of brain injury (56.1 %, n = 111), followed by anoxia/hypoxia or cardiac arrest (24.2%, n = 48), and open/closed traumatic brain injury (17.7%, n = 35).
Out of the 133 subjects included in the ELID group, 47.4% were female (n = 63) and 52.6% male (n = 70). The mean age was 54.5 ± 16.6 years, and the average ICU stay 1.8 ± 2.2 days. 61.7% of patients suffered from intracranial haemorrhage / ischaemia (n = 82), 18.8% from anoxia/hypoxia or cardiac arrest (n = 25), and 18.8% from open/closed traumatic brain injury (n = 25).
In the UTID group (n = 94), 48.9% were female (n = 46) and 51.1% male (n = 48). The mean age was 55.0 ± 17.3 years, and the average ICU stay 1.8 ± 2.0 days. The causes of brain injury were intracranial haemorrhage/ischaemia (62.8%, n = 59), open/closed traumatic brain injury (20.2 %, n = 19), and anoxia/hypoxia or cardiac arrest (17.0%, n = 16).
Figure 1 visualises the reduction in the potential for organ donation, from all deaths to UTID. It shows that approximately two thirds of all ICU adult deaths (2,463/3,667) were not considered to be POSD. Except for three deaths who had neither a donor card nor next of kin (which stops the donation process by legal requirement), all deaths which did not qualify for POSD did so because of medical reasons (table 2). On the POSD step, 54.0% of subjects were not expected to fulfil the brain death criteria, being the main reason for the donation process to stop. On the POTD and the ELID steps, objection to donation by the patients (as expressed in the donor card) or their NOK was the most frequent reason for the donation process being stopped (in 50.8% and 74.4% of cases on the respective step). On the POTD step (n = 198), 78.8% of subjects had no donor card (n = 156). Of the 42 patients who had a donor card, 51.1% wanted a person of trust to make the decision (n = 24), 31.0% consented to any donation (n = 13), 7.1% consented to organ donation only (n = 3), and 4.8% objected to any donation (n = 2). As shown in table 2 (POTD column), the comprehensive number of objections by donor card and by the next of kin was actually higher (n = 33), and in 5 cases, the patients had neither a donor card nor next of kin which, by law, excludes them form donation.
Consent to organ donation was sought in a total of 250 cases, resulting in 120 consents and 130 objections. This is equivalent to an overall 48.0% consent rate (the number of consents to organ donation expressed as a percentage of the total of consents and objections). As shown in figure 2, 80.0% of requests were made before brain death diagnosis was completed and only 20.0% after. The proportion of consents and objections was very similar regardless whether the requests took place before or after brain death was diagnosed. The conversion rate (the number of UTID expressed as the proportion of the number of POTD) was 47.5%.
| Table 1: Demographic and clinical data. | |||||
| All deaths (n = 3,667/100%) | POSD (n = 1,204/100%) | POTD (n = 198/100%) | ELID (n = 133/100%) | UTID (n = 94/100%) | |
| Sex (female/male; n, %) | 1,444/2,223 | 467/737 | 98/100 | 63/70 | 46/48 |
| (39.4%/60.6%) | (38.8%/61.2%) | (49.5%/50.5%) | (47.4%/52.6%) | (48.9%/51.1%) | |
| Age (years; mean, ±1SD, min./max.) | 69.8 ± 14.0 | 64.9 ± 15.8 | 54.5 ± 17.3 | 54.5 ± 16.6 | 55.0 ± 17.3 |
| 11/99 | 11/92 | 11/87 | 11/87 | 11/87 | |
| ICU stay* (days; mean, ±1SD, min./max.) | 5.4 ± 9.2 | 3.4 ± 5.0 | 1.7 ± 2.1 | 1.8 ± 2.2 | 1.8 ± 2.0 |
| 0.0/132.9 | 0.0/46.8 | 0.0/11.7 | 0.1/11.7 | 0.1/11.2 | |
| Patients with an absolute contraindication to donation | 1,227 (33.5%) | 248 (20.6%) | 10 (5.1%) | ||
| Patients never ventilated | 836 (22.8%) | ||||
| with neurological pathology | 120 (3.3%) | ||||
| Patients ventilated | 2,466 (67.3%) | 1,204 (100%) | 198 (100%) | 133 (100%) | 94 (100%) |
| with neurological pathology | 1,250 (34.1%) | 1,056 (87.7%) | 198 (100%) | 133 (100%) | 94 (100%) |
| Cause of brain injury | |||||
| Intracranial haemorrhage | 327 (8.9%) | 296 (24.6%) | 102 (51.5%) | 74 (55.6%) | 55 (58.5%) |
| Intracranial ischaemia | 138 (3.8%) | 89 (7.4%) | 9 (4.6%) | 8 (6.0%) | 4 (4.3%) |
| Open traumatic brain injury | 19 (0.5%) | 18 (1.5%) | 7 (3.5%) | 4 (3.0%) | 3 (3.2%) |
| Closed traumatic brain injury | 99 (2.7%) | 88 (7.3%) | 28 (14.1%) | 21 (15.8%) | 16 (17.0%) |
| Anoxia / hypoxia (all causes), cardiac arrest | 757 (20.6%) | 545 (45.3%) | 48 (24.2%) | 25 (18.8%) | 16 (17.0%) |
| Primary brain cancer | 3 (0.1%) | ||||
| Meningitis / encephalitis | 13 (0.4%) | 12 (1.0%) | 3 (1.5%) | 1 (0.8%) | |
| Intoxication | 14 (0.4%) | 8 (0.7%) | |||
| Other diagnoses from non primary cerebral causes | 2,297 (62.6%) | 148 (12.3%) | 1 (0.5%) | ||
| Brain death testing performed | 151 (12.5%) | 146 (73.7%) | |||
| *Minimal ICU stay is reported as 0.0 for values <72 minutes. ELID = eligible donor; ICU = intensive care unit; POSD = possible donor; POTD = potential donor; SD = standard deviation; UTID = utilised donor | |||||
| Table 2: Summary of the reasons why the DBD process stopped. | ||||||||
| All deaths (n = 3,667) | POSD (n = 1,204) | POTD (n = 198) | ELID (n = 133) | |||||
| Total losses by step of the donation process | 2,463 | (100.0%) | 1,006 | (100.0%) | 65 | (100.0%) | 39 | (100.0%) |
| Medical reasons* | ||||||||
| Absolute contraindication to donation | 979 | (39.7%) | 237 | (23.6%) | 10 | (15.4%) | ||
| Medical condition considered as contraindication | 7 | (0.7%) | 1 | (1.5%) | ||||
| No signs of brain damage and/or never ventilated | 1,368 | (55.5%) | ||||||
| Not expected to fulfil brain death criteria | 543 | (54.0%) | ||||||
| No absence of cerebral flow | 4 | (6.2%) | ||||||
| Cardiac arrest with failed resuscitation | 113 | (4.6%) | 87 | (8.6%) | 2 | (5.1%) | ||
| End stage therapeutic treatment | 31 | (3.1%) | 3 | (4.6%) | ||||
| Multi-organ failure / maintenance problems | 5 | (0.5%) | 6 | (9.2%) | ||||
| Considered for donation after circulatory death | 18 | (1.8%) | ||||||
| Patient considered unsuitable for organ donation by hospital / network / Swisstransplant | 6 | (0.6%) | 3 | (4.6%) | ||||
| No procurement: anatomical, histological and/or functional abnormalities of organs | 8 | (20.5%) | ||||||
| Objection to organ donation (donor card / next of kin)† | 68 | (6.8%) | 33 | (50.8%) | 29 | (74.4%) | ||
| No donor card and no next of kin (stops the donation process) | 3 | (0.1%) | 4 | (0.4%) | 5 | (7.7%) | ||
| *Among the medical reasons for the losses, an absolute contraindication to donation is prioritised (i.e., patients with an absolute contraindication may also have been excluded from the donation process for other medical reasons; however, they are only counted in the absolute contraindication category). †Objection to organ donation is prioritised over other reasons that may have resulted in an exclusion of a patient from the donation process. ELID = eligible donor; ICU = intensive care unit; POSD = possible donor; POTD = potential donor; UTID = utilised donor | ||||||||
Our analysis of one-year SwissPOD data showed that out of 3,667 adult ICU deaths, there were 94 eligible consented donors from whom at least one organ was transplanted. With 94 UTID of 198 POTD, the conversion rate was 47.5% of our study cohort. One of the major impediments to achieve a higher conversion rate was the relatively large proportion of patients or NOK objecting to donation. Our evaluation showed that consent was given in only 48.0% of cases where permission for organ donation was sought.
Figure 3
CVA and traffic accident mortality rates vs donation rates in EU 15 countries and Switzerland.
Source: Eurostat database, © European Union, 1995–2012; the International Registry in Organ Donation and Transplantation (IRODaT).
pmp = per million of population
The 47.5% conversion rate is comparable with the rates in other European countries, such as France (47.1%), Germany (47.0%), the United Kingdom (45.0%), or Belgium (44.3%) [5, 22, 23]. It is substantially higher than conversion rates published in a Dutch study (30.0%) as well as for Poland (30.5%) [22, 26]. Two countries, Finland and Spain, reported conversion rates of more than 50 percent (51.4% and 54.6%, respectively) [22, 40]. This implies that Swiss adult ICUs are predominantly doing an excellent job in the detection and referral of potential donors.
Swiss law requires explicit consent to donation, therefore the NOK approach is a crucial moment in the donation process. It is well documented that there are various factors that may influence patient and NOK decisions. Among these are the timing and setting of request, national legislation (explicit vs presumed consent), public attitude towards and awareness of organ donation and transplantation (including trust in the health care system and the validity of brain death), the level of education, as well as ethnic or cultural differences and religious beliefs [5, 7, 10, 11, 21, 41–54]. Our results – more than half of all patients or NOK objected to organ donation – confirmed that obtaining consent clearly is a hurdle in the donation process. Data published by the Council of Europe reveal that in 2011, refusal rates (the number of families refusing consent expressed as a percentage of number of interviews) ranged from 9.3% in Poland to 52.4% in the Netherlands, with Spain (15.9%), Italy (28.7%), and the United Kingdom (43.4%) in-between [55]. Remarkably, data from 28,977 audited ICU and A&E deaths in the UK in 2011/12 showed a major drop in the refusal rate to 34.0% for DBD [56]. Refusal rates reported by Roels et al. range from 14.6% (Finland) to 32.7% (France), with Belgium (20.3%), and Poland (23.4%) in-between [22]. In a review of published data from a selection of European countries and the USA, Jansen et al. found refusal rates varying from 10.5% (Belgium and Finland) to 59.0% (the Netherlands), with Italy (29.0%), France (34.3%), the UK (41.0%), Germany (42.9%), and USA (46.0%) in-between [57]. As consent rates seem dependent on a multitude of factors, improving modifiable components such as the hospital staff being aware of and committed to organ donation, a straightforward communication of the subject, or the quality of interaction with the caregiver appear to be the best way to enhance consent rates. For this reason, the Federal Office of Public Health has defined four action fields to foster organ donation in Switzerland. The action fields cover the training of medical staff, quality and process management, structural and finance improvements in hospitals, and information campaigns aimed at the general public. Except for the last-mentioned, these action fields have been delegated to the CNDO and Swisstransplant for execution. In the hospitals, several measures to establish national standards in the donation process on the educational, structural and process levels are in the implementation phase.
Similar to the consent rate, which is subject to heterogeneous influences, several factors may influence the potential for organ donation. Such variables include the population age structure, the availability of ICU beds and/or neurosurgical facilities, as well as mortality rates from cerebrovascular accident (CVA) or traumatic brain injury [4–6, 58]. In our study, the main causes of brain injury on the POTD step were CVA (56.1%), trauma (17.6%), and anoxia/hypoxia or cardiac arrest (24.2%). Even though there is some variability among the data published from different countries, the general picture of the proportions is similar. A study that evaluated the donor potential in the north-east region of Germany found that out of 2,019 deaths with primary or secondary brain damage, the causes were nontraumatic intracranial haemorrhage (51.0%), craniocerebral injury (22.1%), ischaemia (11.9%), and hypoxic damage (10.4%) [23]. In a review of medical records for multiple-organ donors in Belgium, the principal causes of brain death were cerebrovascular disease (46.0%), craniocerebral trauma (38.0%), and hypoxia (15.0%) [59]. Results from the audit of potential organ donors in the Republic of Ireland showed that the causes of death in patients diagnosed with brain stem death were intracranial haemorrhage (54.1%), traumatic brain injury (28.7%), and hypoxic brain injury (12.1%) [24]. In a large US study, the main causes of death were stroke (40.6%), head trauma (36.0%), and anoxia (20.1%) [60].
In order to evaluate the potential for organ donation, two studies compared mortality rates from CVA and traffic accidents with actual donation rates in different countries [7, 61]. Both studies found considerable differences between the mortality rates in the countries included in their analyses. Since in our study, 83.0% of the UTID died of either CVA (62.8%) or traumatic brain injury (20.2%), we wanted to compare mortality rates from these diagnoses with donation rates in selected European countries. Assuming that traumatic brain injuries were mostly resulting from traffic accidents, we extracted CVA and traffic accident mortality rates from the Eurostat statistics database (ICD-10 I60–69 and V01–99; age standardised, 2010 data or nearest year for EU 15 countries and Switzerland) [62]. The donation rates for these selected countries were taken from the International Registry in Organ Donation and Transplantation (IRODaT) [63].
Figure 3 displays a comparison of the CVA and traffic accident mortality rates with the donation rate (all rates are shown as pmp). It shows that Switzerland has the lowest combined CVA and traffic mortality rate (292 pmp). Average values (EU 15 countries plus Switzerland) are 462 pmp combined mortality, and 17.3 pmp deceased donors. In the diagram, the “x”-mark indicates the conversion value (numerals displayed on the right side of the mark). It is calculated from the donation rate divided by the total mortality rate, multiplied by 1000. Example for the calculation of the value for Switzerland: 12.6 / (252 + 40) x 1000 = 43. The Swiss conversion value is slightly above the average, being 40. In a ±5 range from the average, it is similar to Italy (44), Germany (40), and Portugal (39), notably all countries with a higher donation rate. Other countries with higher donation rates than Switzerland’s, such as Finland, the United Kingdom, the Netherlands or Denmark also show conversion values below the average. When taking into account the 52.0% patient and NOK refusal rate in Switzerland, the data presented in figure 3 support our argument that a majority of potential organ donors are being detected and referred.
This study is the first comprehensive, nationwide assessment of the donation process and its outcomes for patients who died in an adult ICU. In view of the fact that the detection and referral of potential donors is required by law, SwissPOD had a 100% participation rate from the ICUs accredited by the SSICM. Since our assessment was based on the first year of SwissPOD data, we were not able to perform any benchmarking, and consequently refrained from doing statistical analyses, except for descriptive statistics. Furthermore, one should keep in mind that the number of patients included in this study represents only approximately 6% of all deaths in Switzerland during the investigation period. Thus, there may exist an additional potential for DBD or donation after circulatory death from paediatric ICU deaths, from patients who died in A&E, intermediate care units, on general hospital wards, or out-of-hospital. However, we assume that the additional potential of organ donors, especially in the last patient group, is relatively small.
Our analysis of SwissPOD data showed that despite the undeniably low donation rate, Swiss adult ICUs are generally doing an excellent job in considering the option of donation at end of life care. This is reflected by the fact that the Swiss conversion rate is comparable to data published from major European countries such as France, Germany, or the United Kingdom. This finding is supported by an international comparison of CVA and traffic accident mortality rates with donation rates. It showed that the Swiss conversion value is comparable with countries that have lower refusal rates as well as higher donation rates. Our study also showed that in Switzerland, the rate of NOK refusal to organ donation is among the highest in Europe. Unsurprisingly, this fact clearly has a negative impact on the donation rate. The reasons for the high percentage of patients and NOK refusing consent to organ donation require further study. From our findings we conclude that optimising the NOK approach seems to be the most effective means of increasing the post mortem organ donation rate in Switzerland.
Acknowledgement:The authors would like to thank the participating ICU and A&E staff for data collection, Caroline Spaight for data validation, and Danick Gut for proofreading the manuscript.
1 The International Registry in Organ Donation and Transplantation (IRODaT). Preliminary 2012 Data. 2013.
2 Swisstransplant. Jahresbericht 2011. The Swiss National Foundation for organ donation and transplantation; Bern, 2012 [Annual Report; cited 2013 Dec 4]. Available from: http://www.swisstransplant.org/
3 Abouna GM. Organ shortage crisis: problems and possible solutions. Transplant Proc. 2008;40:34–8.
4 Cuende N, Cuende JI, Fajardo J, Huet J, Alonso M. Effect of population aging on the international organ donation rates and the effectiveness of the donation process. Am J Transplant. 2007;7:1526–35.
5 Barber K, Falvey S, Hamilton C, Collett D, Rudge C. Potential for organ donation in the United Kingdom: audit of intensive care records. BMJ. 2006;332:1124–7.
6 Sheehy E, O’Connor KJ, Luskin RS, Howard RJ, Cornell D, Finn J, et al. Investigating geographic variation in mortality in the context of organ donation. Am J Transplant. 2012;12:1598–602.
7 Coppen R, Friele RD, Gevers SKM, Blok GA, van der Zee J. The impact of donor policies in Europe: a steady increase, but not everywhere. BMC Health Serv Res. 2008;8:235.
8 Friele RD, Coppen R, Marquet RL, Gevers JKM. Explaining differences between hospitals in number of organ donors. Am J Transplant. 2006;6:539–43.
9 Mossialos E, Costa-Font J, Rudisill C. Does organ donation legislation affect individuals’ willingness to donate their own or their relative’s organs? Evidence from European Union survey data. BMC Health Serv Res. 2008;8:48.
10 Rithalia A, McDaid C, Suekarran S, Myers L, Sowden A. Impact of presumed consent for organ donation on donation rates: a systematic review. BMJ. 2009;338:a3162.
11 Irving MJ, Tong A, Jan S, Cass A, Rose J, Chadban S, et al. Factors that influence the decision to be an organ donor: a systematic review of the qualitative literature. Nephrol Dial Transplant. 2012;27:2526–33.
12 Salim A, Malinoski D, Schulman D, Desai C, Navarro S, Ley EJ. The combination of an online organ and tissue registry with a public education campaign can increase the number of organs available for transplantation. J Trauma. 2010;69:451–4.
13 Paez G, Valero R, Manyalich M. Training of health care students and professionals: a pivotal element in the process of optimal organ donation awareness and professionalization. Transplant Proc. 2009;41:2025–9.
14 Pelleriaux B, Roels L, Van Deynse D, Smits J, Cornu O, Delloye C. An analysis of critical care staff’s attitudes to donation in a country with presumed-consent legislation. Prog Transplant. 2008;18:173–8.
15 DuBois JM, Anderson EE. Attitudes toward death criteria and organ donation among healthcare personnel and the general public. Prog Transplant. 2006;16:65–73.
16 Georgiadou E, Sounidakis N, Mouloudi E, Giaglis P, Giasnetsova T, Marmanidou K, et al. Attitudes and behavior toward organ donation in Greece. Transplant Proc. 2012;44:2698–2701.
17 Ormrod JA, Ryder T, Chadwick RJ, Bonner SM. Experiences of families when a relative is diagnosed brain stem dead: understanding of death, observation of brain stem death testing and attitudes to organ donation. Anaesthesia. 2005;60:1002–8.
18 Bøgh L, Madsen M. Attitudes, knowledge, and proficiency in relation to organ donation: a questionnaire-based analysis in donor hospitals in northern Denmark. Transplant Proc. 2005;37:3256–7.
19 Morgan SE, Miller JK. Beyond the organ donor card: the effect of knowledge, attitudes, and values on willingness to communicate about organ donation to family members. Health Commun. 2002;14:121–34.
20 Scandroglio B, Domínguez-Gil B, López JS, Valentín MO, Martín MJ, Coll E, et al. Analysis of the attitudes and motivations of the Spanish population towards organ donation after death. Transpl Int. 2011;24:158–66.
21 Siminoff LA, Burant C, Youngner SJ. Death and organ procurement: public beliefs and attitudes. Kennedy Inst Ethic J. 2004;14:217–34.
22 Roels L, Smits J, Cohen B. Potential for deceased donation not optimally exploited: Donor Action data from six countries. Transplantation. 2012;94:1167–71.
23 Wesslau C, Grosse K, Krüger R, Kücük O, Mauer D, Nitschke FP, et al. How large is the organ donor potential in Germany? Results of an analysis of data collected on deceased with primary and secondary brain damage in intensive care unit from 2002 to 2005. Transpl Int. 2007;20:147–55.
24 Organ Procurement Working Group. Audit of potential organ donors Republic of Ireland. Health Service Executive; 2009 [cited 2013 Dec 4]. Available from: http://www.lenus.ie/hse/handle/10147/85814
25 Madsen M, Bøgh L. Estimating the organ donor potential in Denmark: a prospective analysis of deaths in intensive care units in northern Denmark. Transplant Proc. 2005;37:3258–9.
26 Jansen NE, van Leiden HA, Haase-Kromwijk BJJM, Hoitsma AJ. Organ donation performance in the Netherlands 2005–08; medical record review in 64 hospitals. Nephrol Dial Transplant. 2010;25:1992–7.
27 Sheehy E, Conrad SL, Brigham LE, Luskin R, Weber P, Eakin M, et al. Estimating the number of potential organ donors in the United States. N Engl J Med. 2003;349:667–74.
28 Garside J, Garside M, Fletcher S, Finlayson B. Utilisation of an embedded specialist nurse and collaborative care pathway increases potential organ donor referrals in the emergency department. Emerg Med J. 2012;29:228–32.
29 Matesanz R, Domínguez-Gil B, Coll E, de la Rosa G, Marazuela R. Spanish experience as a leading country: what kind of measures were taken? Transpl Int. 2011;24:333–43.
30 Matesanz R, Marazuela R, Domínguez-Gil B, Coll E, Mahillo B, de la Rosa G. The 40 donors per million population plan: an action plan for improvement of organ donation and transplantation in Spain. Transplant Proc. 2009;41:3453–6.
31 Matesanz R, Miranda B. A decade of continuous improvement in cadaveric organ donation: the Spanish model. J Nephrol. 2002;15:22–8.
32 Roels L, Wight C. Donor Action: an international initiative to alleviate organ shortage. Prog Transplant. 2001;11:90–7.
33 Wynn JJ, Alexander CE. Increasing organ donation and transplantation: the U.S. experience over the past decade. Transpl Int. 2011;24:324–32.
34 Howard DH, Siminoff LA, McBride V, Lin M. Does quality improvement work? Evaluation of the Organ Donation Breakthrough Collaborative. Health Serv Res. 2007;42:2160–73.
35 Shafer TJ, Wagner D, Chessare J, Schall MW, McBride V, Zampiello FA, et al. US organ donation breakthrough collaborative increases organ donation. Crit Care Nurs Q. 2008;31:190–210.
36 Griffiths J, Verble M, Falvey S, Bell S, Logan L, Morgan K, et al. Culture change initiatives in the procurement of organs in the United kingdom. Transplant Proc. 2009;41:1459–62.
37 Kong AP, Barrios C, Salim A, Willis L, Cinat ME, Dolich MO, et al. A multidisciplinary organ donor council and performance improvement initiative can improve donation outcomes. Am Surg. 2010;76:1059–62.
38 Domínguez-Gil B, Delmonico FL, Shaheen FAM, Matesanz R, O’Connor K, Minina M, et al. The critical pathway for deceased donation: reportable uniformity in the approach to deceased donation. Transpl Int. 2011;24:373–8.
39 SR 810.211. Verordnung über die Transplantation von menschlichen Organen, Geweben und Zellen (Transplantationsverordnung) vom 16. März 2007 (Stand am 1. Januar 2013) [Transplantation Ordinance; cited 2013 Dec 4]. Available from: http://www.admin.ch/opc/de/classified-compilation/20051806/201301010000/810.211.pdf
40 de la Rosa G, Domínguez-Gil B, Matesanz R, Ramón S, Alonso-Álvarez J, Araiz J, et al. Continuously evaluating performance in deceased donation: the Spanish quality assurance program. Am J Transplant. 2012;12:2507–13.
41 Simpkin AL, Robertson LC, Barber VS, Young JD. Modifiable factors influencing relatives’ decision to offer organ donation: systematic review. BMJ. 2009;338(b991):online first doi:10.1136/bmj.b991.
42 Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transplant. 2006;6:190–8.
43 English V. Is presumed consent the answer to organ shortages? Yes. BMJ. 2007;334:1088.
44 Wright L. Is presumed consent the answer to organ shortages? No. BMJ. 2007;334:1089.
45 Abadie A, Gay S. The impact of presumed consent legislation on cadaveric organ donation: a cross-country study. J Health Econ. 2006;25:599–620.
46 Roels L, Rahmel A. The European experience. Transpl Int. 2011;24:350–67.
47 Quigley M, Brazier M, Chadwick R, Michel MN, Paredes D. The organs crisis and the Spanish model: theoretical versus pragmatic considerations. J Med Ethics. 2008;34:223–4.
48 Directorate General Health and Consumer Protection (SANCO). Special Eurobarometer 272 "Europeans and organ donation". European Commission; 2007 [cited 2013 Dec 4]. Available from: http://ec.europa.eu/public_opinion/archives/ebs/ebs_272d_en.pdf
49 Lock M, Crowley-Makota M. Situating the practice of organ donation in familial, cultural, and political context. Transplant Rev. 2008;22:154–7.
50 Siminoff LA, Gordon N, Hewlett J, Arnold RM. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA. 2001;286:71–7.
51 Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med. 2006;21:995–1000.
52 Schulz PJ, Nakamoto K, Brinberg D, Haes J. More than nation and knowledge: cultural micro-diversity and organ donation in Switzerland. Patient Educ Couns. 2006;64:294–302.
53 Vincent A, Logan L. Consent for organ donation. Br J Anaesth. 2012;108:i80–7.
54 Exley M, White N, Martin JH. Why families say no to organ donation. Crit Care Nurse. 2002;22:44–51.
55 Council of Europe. International figures on donation and transplantation 2011. Newsletter Transplant. 2012;17.
56 Murphy C, Allen J. Potential donor audit annual report, 1 April 2011 to 31 March 2012. NHS Blood and Transplant; 2012 [cited 2013 Dec 4]. Available from: http://www.organdonation.nhs.uk/statistics/potential_donor_audit/pdf/pda_report_1112.pdf
57 Jansen NE, Haase-Kromwijk BJJM, van Leiden HA, Weimar W, Hoitsma AJ. A plea for uniform European definitions for organ donor potential and family refusal rates. Transpl Int. 2009;22:1064–72.
58 Weiss J, Hofmann SP, Immer FF. Patient characteristics of deceased organ donors in Switzerland 1998–2008. Swiss Med Wkly. 2011;141:w13265.
59 Meers C, Van Raemdonck D, Van Gelder F, Van Hees D, Desschans B, De Roey J, et al. Change in donor profile influenced the percentage of organs transplanted from multiple organ donors. Transplant Proc. 2009;41:572–5.
60 Messersmith EE, Arrington C, Alexander C, Orlowski JP, Wolfe R. Development of donor yield models. Am J Transplant. 2011;11:2075–84.
61 Bendorf A, Kerridge IH, Kelly PJ, Pussell B, Guasch X. Explaining failure through success: a critical analysis of reduction in road and stroke deaths as an explanation for Australia’s low deceased organ donation rates. Internal Med. 2012;42:866–73.
62 European Commission. Mortality rates for ICD 10 I60–69 and V01–99 (2010 data, © European Union, 1995–2012). European Commission / Eurostat; 2013 [cited 2013 Dec 4]. Available from: http://epp.eurostat.ec.europa.eu/portal/page/portal/eurostat/home.
63 The International Registry in Organ Donation and Transplantation (IRODaT). Second report data. 2012.
Funding / potential competing interests: The Swiss Monitoring of Potential Organ Donors (SwissPOD) is funded by the Federal Office of Public Health, and the Swiss University Hospitals and transplant centres (G15).
The members of the Scientific Committee of the Comité National du Don d’Organes (CNDO) are: Prof. Dr. med. Christoph Haberthür (President of the CNDO), Dr. med. Jan Wiegand, and PD Dr. med. Franz F. Immer.
Authors’ contribution: JHW performed the literature research and drafted the manuscript. IK was the main responsible for the data extraction and analysis. FFI, JW, and CH conceived of the study, participated in its design and coordination, and revised the manuscript critically for important intellectual content. All authors have read and approved the final version of the manuscript.
Ethics approval:The SwissPOD study obtained ethics approval by the cantonal ethics committees and the Eidgenössische Expertenkommission für das Berufsgeheimnis in der medizinischen Forschung (approval number 035.0001–59/139).