Hospital disaster preparedness in Switzerland
DOI: https://doi.org/10.4414/smw.2014.14032
fabrice
Dami, Bertrand
Yersin, Alexandre H
Hirzel, Olivier
Hugli
Summary
STUDY OBJECTIVE: Hospital preparedness is an essential component of any developed health care system. However, there is no national legislation in Switzerland. The objective of this inquiry was to establish the geographic distribution, availability and characteristics of hospital preparedness across Switzerland.
METHODS: A questionnaire regarding hospital preparedness in 2006 was addressed to all heads responsible for emergency departments (ED). The survey was initiated in 2007 and finalised in 2012.
RESULTS: Of the 138 ED, 122 (88%) returned the survey. Eighty nine EDs (82%) had a disaster plan.
CONCLUSIONS: Our study identified an insufficient rate of hospitals in which emergency physicians reported a disaster plan. The lack of national or cantonal legislation regulating disaster preparedness may be partially responsible for this.
Introduction
Switzerland is a federation of 26 States. As in the USA [1] or in Germany [2], the health care system is fragmented and highly decentralised. Each state is sovereign to rule on hospital disaster preparedness legislation [3]. There is no national standard [4], except for pandemic crises [5], infectious diseases such as HIV/AIDS, vaccines [3] and nuclear incidents. Switzerland is a small country of 41,285 km2 (15,940 square miles) populated by 8.1 million inhabitants, mostly living in the central lowlands. Switzerland is at risk of both natural and man-made disasters. The country is at medium risk of earthquake and flood. Furthermore, climate change has increased the risk of extreme weather events; the retreat of permafrost due to warming may cause more rock-falls and landslides in mountainous areas that are now more densely populated [6]. Switzerland has 3,600 km of railway lines, 7,850 km of roads, 2,200 km of high-pressure natural gas pipelines, 250 km of oil pipelines and 2,600 plants that are considered possible originators of major chemical or biological accidents; 10% of these plants have the potential to cause severe damage in the event of a major accident [7]. In addition, Switzerland has four aging nuclear power plants, all of which are located in the central lowlands. The risk of major chemical, biological or nuclear accidents is concentrated around the largest cities of Switzerland and would likely involve a large number of people. In a 2012 risk report, the Swiss federal office for civil protection (FOCP) estimated that an epidemic or pandemic was the most severe risk, followed by an earthquake [8].
Switzerland is among the richest countries in the world [9] and has a system of public health surpassed only by the USA in per capita costs [10]. However, disaster preparedness is costly for hospitals to achieve and maintain, with costs ranging from one to more than three million dollars per hospital in the USA [11, 12]. Federal or state funding may be insufficient to support such costs, even in countries like the USA, which have had to activate disaster plans on several occasions since September 11th, 2001 [11]. Furthermore, some privately funded hospitals are exposed to competition in the hospital market or insurance market [3]. Some data suggest that their level of preparedness may be less efficient than that seen in public institutions [13].
Following a natural or man-made disaster, a large proportion of patients are likely to present to local hospitals, and hospital-based EDs will face a surge of patients whilst being chronically overcrowded. Both ED and hospital preparedness are key factors in managing acutely ill or injured patients, as demonstrated recently after the bombing during the Boston Marathon [14].
In 2006, an inquiry was conducted to establish the geographic distribution, volume of consultations and system of organisation of EDs across Switzerland, as well as pre-hospital medical systems and hospital preparedness. The results regarding EDs were published in 2013 [15]. The part of this inquiry that was specifically dedicated to hospital disaster preparedness is the topic of this publication, as Switzerland does not currently possess a description of this essential component of its public healthcare system.
Methods
The detailed methods have been published elsewhere [15]. Data collection was conducted from 2007 to 2012, describing Swiss EDs, pre-hospital settings and hospital disaster preparedness in 2006. EDs were defined as any emergency room in a hospital offering acute care on a 24/7 basis. EDs admitting adult as well as paediatric patients were included. Specialty ERs dedicated only to ophthalmology or psychiatry were excluded on account of their highly specialised structures and technical capabilities. The contents of the questionnaire were drawn up using structural and organisational recommendations for Swiss hospital EDs as far as the medical and technical aspects were concerned [16]. The questionnaire from the National Emergency Department Inventory (NEDI) of the Emergency Medicine Network (EMNet) was used to formulate questions to assess activity levels [17]. Crowding was defined as the presence of more patients than available triage rooms or beds at 6 p.m. on a typical day, whilst boarding was defined as a wait in the ED >2 h before transfer to the hospital floors by 6 p.m. on a typical day [18]. Crowding and boarding are important indicators of the ED surge capacity in case of a major incident. Questionnaire respondents were also asked whether bed capacity for inpatients and the intensive care unit was estimated to be insufficient. The EDs were further stratified according to the average number of annual visits: 1 to 5,000, 5,001 to 10,000, 10,001 to 20,000, and >20,000 visits. EDs were also stratified by hospital size (number of stationary beds): <100 beds, 100–199 beds, 200–499, and 500 or more beds.
For each zip code with a hospital-based ED, we applied one of the 14 Swiss spatial mobility regions (SSMR) codes defined in 2000, which were based on the 2000 Swiss census [19]. Switzerland was categorised in four hierarchical levels, including three urban areas and one rural area: (1.) metropolitan area, (2.) large non-metropolitan urban area with 40,000 to 120,000 residents, (3.) small non-metropolitan urban area with <40,000 residents, and IV) rural area [7].
Statistical analysis
Continuous variables are presented by the average and standard deviation (SD), while data with a non-normal distribution are presented by the median and interquartile range (IQR). Categorical variables are presented as percentages. Inter-group comparisons were performed using ANOVA for continuous variables with a normal distribution and the Kruskal Wallis test for data with a non-normal distribution; categorical data were analysed with the Chi-square test or Fisher exact test. Missing data were not imputed. Statistical analyses were done using Stata 12.0 (StataCorp, College Station, TX, USA).
Results
In 2006 [15], Switzerland had a total of 124 hospital-based EDs, which equates to 30 EDs/10,000 km2, or 16.5 EDs/1,000,000 inhabitants. The total number of EDs that we surveyed was 138, which is greater than the number of hospitals because some hospitals had separate and autonomous EDs for paediatrics (n = 11) or gynaecology (n = 3) within the same hospital. 99 EDs (72%) were located in the German-speaking region of Switzerland, 30 (22%) in the French-speaking region and 9 (7%) in the Italian-speaking region. Of the 124 hospitals, 111 (90%) returned at least one survey. Of the 138 EDs, 122 (88%) returned the survey, with 108 completely filled (78%) and 14 (10%) partially filled surveys. The response rate was similar between the three linguistic regions. The vast majority (95%) of EDs was based in teaching hospitals, including some in private institutions; 87% were in public institutions including 9% in university hospitals. Nearly two thirds of EDs were located in a metropolitan area or a non-metropolitan city with ≥40,000 residents. Based on the average number of annual visits, 31 (25%) EDs had 1 to 5,000, 38 (31%) 5,001 to 10,000, 32 (26%) 10,001 to 20,000, and 21 (17%) >20,000 visits. Almost all EDs with >10,000 annual visits were located in an urban setting. Based on hospital size, EDs were located in hospitals with <100 beds in 41 (30%), 100–199 beds in 47 (34%), 200–499 in 26 (19%) of EDs, and 500 or more beds in 23 (17%) of EDs.
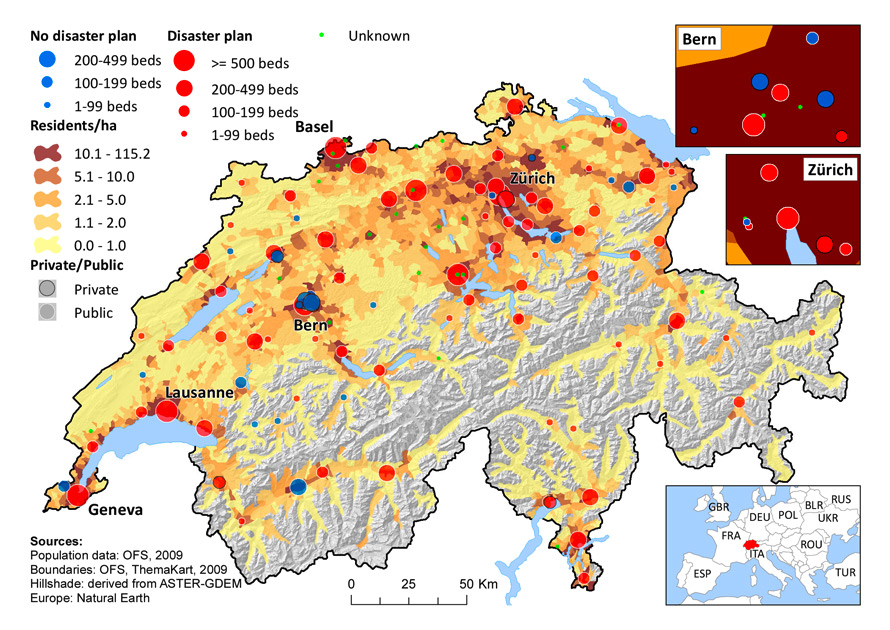
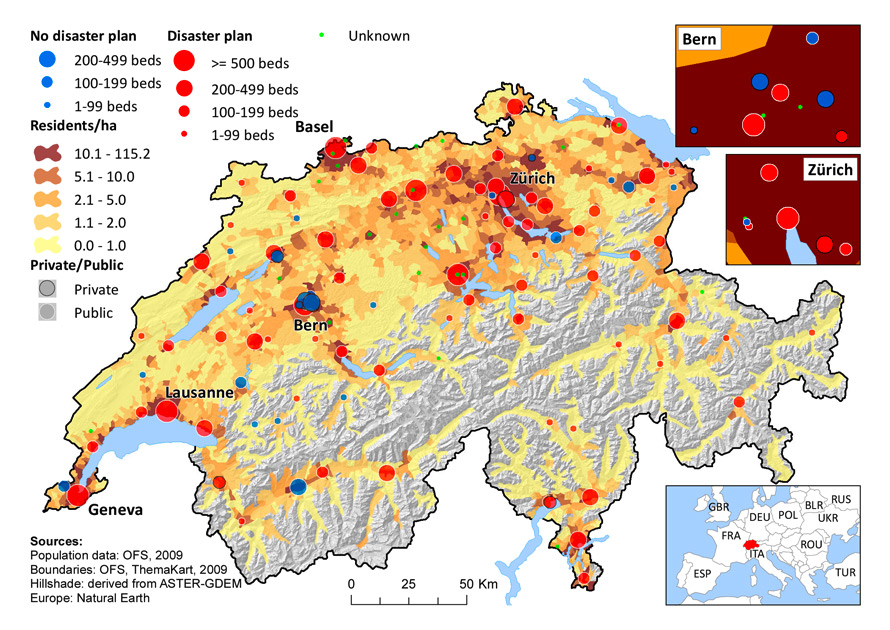
Figure 1
Presence of a hospital disaster plan according to ED and hospital characteristics. (Sources: Population data: OFS, 2009, Boundaries: OFS, ThemaKart, 2009. Hillshade: derived from ASTER-GDEM; Europe: Natural Earth. © Bundesamt für Statistik (BFS), Website Statistik Schweiz.)
Among the 108 EDs that responded to the question on hospital preparedness, eighty nine (81 public and 8 private EDs) had a disaster plan (82%). Public hospitals more frequently had a disaster plan than private ones (p = 0.017). The existence of a disaster plan was not associated with the size of the hospital (p = 0.228), but rather with the number of ED consultations per year (p = 0.043). There were no statistically significant differences in the percentage of disaster plans between the three main linguistic parts of the country. All university EDs that responded [11] had a plan. However, the presence of a plan was not dependent on the population density, as all four categories (see above) had the benefit of a plan in 76–89% of cases.
Hospitals with a disaster plan were slightly more often found to have an intensive care unit (p = 0.06). Nearly a third had an insufficient number of inpatient or ICU beds, according to the ED estimation, which was a similar percentage between hospitals with or without a disaster plan. Nearly half of the EDs suffered from crowding or boarding, again without differences between hospitals with or without a disaster plan. Only 83% of EDs had a plan to reinforce their personnel in case of an increase in patient volume in response to a disaster.
In fifty-one EDs (63%), the head of the ED was responsible for the plan. This rate rose to 90% in university EDs, and 59% in non-university EDs (p = 0.08).
|
Table 1: Hospital preparedness. |
|
Characteristics
|
Total answers
|
yes
|
no
|
p
|
|
Presence of a disaster plan
|
|
|
|
|
|
Number of EDs response, n(%)
|
108 |
89 (82) |
19 (18) |
|
|
Public vs Private hospital
|
108 |
|
|
0.017 |
| Private hospital |
14 (13) |
8 (57) |
6 (43) |
|
| Public hospital |
94 (87) |
81 (86) |
13 (14) |
|
|
Hospital's size-nb of beds (%)
|
108 |
|
|
0.228 |
| <100 |
35 (32) |
25 (71) |
10 (29) |
|
| 100–199 |
42 (39) |
36 (86) |
6 (14) |
|
| 200–499 |
23 (21) |
20 (87) |
3 (13) |
|
| ≥500 |
7 (8) |
7 (100) |
0 (0) |
|
| Hospital with intensive care unit, n (%) |
64 (63) |
55 (86) |
9 (14) |
0.04 |
| Insufficient inpatient bed capacity, n (%) |
31 (29) |
28 (90) |
3 (10) |
0.34 |
| Insufficient intensive care bed capacity, n (%) |
24 (26) |
24 (100) |
0 (0) |
0.02 |
|
ED's number of visits/year
|
108 |
|
|
0.043 |
| 0–5,000 |
25 (23) |
16 (64) |
9 (36) |
|
| 5,001–10,000 |
35 (32) |
29 (83) |
6 (17) |
|
| 10,001–20,000 |
29 (27) |
26 (90) |
3 (10) |
|
| >20,000 |
19 (18) |
18 (95) |
1 (5) |
|
| Crowding |
51 (48) |
44 (86) |
7 (14) |
|
| Boarding |
51 (48) |
44 (86) |
7 (14) |
|
| Personnel reinforcement planning |
61 (56) |
50 (82) |
11 (18) |
|
|
Linguistic region
|
108 |
|
|
0.55 |
| French part |
29 (27) |
24 (83) |
5 (17) |
|
| German part |
71 (66) |
57 (80) |
14 (20) |
|
| Italian part |
8 (7) |
8 (100) |
0 (0) |
|
|
University vs non-University hospital
|
108 |
|
|
0.21 |
| University hospital |
11 (10) |
11 (100) |
0 (0) |
|
| Non university hospital |
97 (90) |
78 (80) |
19 (20) |
|
|
Urbanisation level
|
108 |
|
|
0.75 |
| Metropolitan area |
46 (43) |
38 (83) |
8 (17) |
|
| Large non metropolitan area |
22 (20) |
18 (82) |
4 (18) |
|
| Small non-metropolitan urban area |
19 (18) |
17 (89) |
2 (11) |
|
| Rural area |
21 (19) |
16 (76) |
5 (24) |
|
Discussion
Hospital preparedness is an essential component for any highly developed health care system. Our research on data from 2006 is the first to offer a global picture of the component in Switzerland. Hospital preparedness planning has become a major theme in the literature, especially since the terrorist attacks in September 2001 in the USA. A US survey in 2003–2004, completed by the staff members responsible for the plan, showed that out of the representative sample of 739 hospitals that answered (85% response rate), 92% reported having revised their emergency response plans since September 11th 2001 for at least one of those risks (biological, chemical, nuclear-radiological, explosive-incendiary, natural disaster). Hospital plans for institutions with fewer than 100 beds or within a rural area were less likely to cover all risks (biological, nuclear, terrorism) [20]. A similar study in 2008 showed that nearly all hospitals from the sample had response plans for chemical releases, natural disasters, epidemics and biological incidents. Sixty-seven percent of hospitals had a disaster plan for all six categories of expected incidents. Preparedness for explosive or incendiary incidents was less frequent, however [21].
In our study, 82% of EDs stated that they benefited from a hospital disaster plan; our questionnaire was not designed to assert if these disaster plans covered all or only specific risks. All of the largest Swiss institutions have one, and we can speculate that they also benefit from more human and financial capacities to do so. On the other hand, private hospitals less frequently have a disaster plan. The reasons for this may be financial or regulatory issues [13].
The reason for such disparity between hospitals regarding disaster preparedness is well known in other countries. Most EDs have never been confronted with a mass casualty incident, which may also explain the lower rate of hospital disaster plans in Switzerland than in the USA, as these events are viewed as having a low probability. There are also few incentives to deal with this issue in our country. Such work is also restricted by its costs [22]. Auf der Heide, who studied 29 disasters in the USA and compared them to the disaster plans of the hospitals concerned, concluded that the interest for preparedness is proportional to the elapsed time, location and size of the last disaster [23]. State administration or other surveillance structures have a major role to play as it may not be sufficient to count on the hospitals' motivation to draw hospital plans or have regular drills. On occasion, the preparation of an international event may provide an incentive for State Health services to control the existence and functionality of hospital disaster plans. For example, during the European soccer championship in Switzerland in 2008, one of the 26 Swiss states took advantage of this event to encourage hospitals to update their plans [24].
On what criteria should we decide which hospital should have a plan? Lynn et al. believe that only hospitals with minimal criteria, such as having an intensive care unit, should have a disaster plan [25]. Others doubt that concentrating victims in selected hospitals is the right choice, as victims spontaneously go to the nearest and potentially small hospitals [26]. Based on recent experiences, even such frontline hospitals can handle numerous patients if disaster plans have been exercised repeatedly and intensive care capabilities are available [27].
Our study also shows that Swiss hospitals and EDs are affected by crowding, boarding and insufficient access to acute in-hospital beds. Therefore, their capacity to absorb a surge of patients after a disaster may be questioned. Facility-based surge capacity is crucial during the initial response and is even incorporated in the design of recently built EDs, but little is known regarding Swiss surge capacity [28].
As any hospital structure can be confronted by a spontaneous massive inflow of patients or any internal disaster (loss of power, fire, weather conditions such as hurricane), national recommendations should aim for an ideal 100% of disaster plan in hospitals. This is recommended by the Joint Commission in the USA, as well by the American College of Emergency Physicians (ACEP) [29]. As mentioned before, there is currently no requirement in Switzerland for hospitals to impose a disaster plan. Finally, the presence of a plan is not sufficient. The Boston marathon bombings in 2013 showed that the successful management of multiple simultaneous severe trauma patients was in great part due to hospital healthcare providers' knowledge of their role in a disaster, which was acquired during repeated drills of their disaster plans, sometimes on a city-wide scale [30, 31]. Unlike the USA, Switzerland does not require disaster drills for hospital accreditation. Our questionnaire did not, however, address the frequency of drills.
Limitations
Our study provides the largest, most inclusive perspective on Swiss hospital disaster preparedness to date. However, as we covered only 88% of EDs and there are no data from non-responding EDs, we cannot assess whether their characteristics differed significantly. Our survey is roughly quantitative (has/has not) and was not designed to evaluate in detail the volume or quality of the Swiss pre-hospital systems and hospital disaster preparedness. In particular, it does not describe whether the hospital emergency plan is up to date, functional, known to hospital workers, or has been recently tested. These data on hospital disaster preparedness were self-reported by ED personnel, and other staff may not be fully aware of the specifics of a disaster plan. For example, a German survey distributed to physicians working in trauma centres of different categories revealed that only 53% of physicians knew that there was a plan in their hospital [32]. However, such unawareness may be related to a lack of disaster plan drills, which is equivalent to an absence of plan. Finally, our study describes the Swiss situation in 2006. Some information may be outdated.
Conclusion
Our study identified an insufficient rate of hospitals in which emergency physicians reported a disaster plan. The lack of national or state legislation regulating disaster preparedness may be partially responsible for this. Our rate may not increase as the obstacles to their development are numerous. This survey could help raise interest in developing a disaster plan in Swiss hospitals.
Acknowledgement:We thank Ulrich Burgi (Aarau), Dagmar Keller (Zürich), Olivier Rutschmann (Geneva), and Schwendinger (Baden) for their help in completing the survey and enrolling additional EDs.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.
References
1 Moore S. Policy brief: Delivery system redesign. Brandeis University 2010. Available from: http://www.niatx.net/pdf/ARC/Delivery_System_Redesign.pdf
2 Domres B, Schauwecker HH, Rohrmann K, Roller G, Maier GW, Manger A. The German approach to emergency/disaster management. Med Arch. 2000;54:201–3.
3 Wyss K, Lorenz N. Decentralisation and central and regional coordination of health services: the case of Switzerland. Int J Health Plann Manage. 2000;15:103–14.
4 Osterwalder JJ. Emergency medicine in Switzerland. Ann Emerg Med. 1998;32:243–7.
5 Federal Office of Public Health. Swiss plan for influenza pandemic. Available at: http://www.bag.admin.ch/influenza/01120/01134/03058/index.html?lang=fr&download=
6 Federal Office for the Environment. Status Report on Natural Hazards. Available at: http://www.bafu.admin.ch/umwelt/status/03995/index.html?lang=en
7 Federal Office for the Environment. Status report on major accidents. Available at: http://www.bafu.admin.ch/umwelt/status/04017/index.html?lang=en
8 Federal Office for Civil protection. The national risk analysis of Disaster and Emergencies in Switzerland. Available at: http://www.bevoelkerungsschutz.admin.ch/internet/bs/en/home/themen/gefaehrdungen-risiken/nat__gefaehrdungsanlayse.html
9 WorldBank.org GDP per capita (current US$) Available at: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD/countries?display=default
10 Anderson GF, Reinhardt UE, Hussey PS, Petrosyan V. It's the prices, stupid: why the United States is so different from other countries. Health Aff 2003;22:89–105.
11 De Lorenzo RA. Financing hospital disaster preparedness. Prehosp Disaster Med. 2007;22(5):436–9.
12 Petinaux B. Financial burden of emergency preparedness on an urban, academic hospital. Prehosp Disaster Med. 2009;24(5):372–5.
13 Mahdaviazad H .Assessing hospital disaster preparedness in Shiraz, Iran 2011: teaching versus private hospitals. Am J Dis Med. 2013;8:65–73.
14 Biddinger PD, Baggish A, Harrington L, d'Hemecourt P, Hooley J, Jones J, et al. Be prepared – the Boston Marathon and mass-casualty events. N Engl J Med. 2013;368:1958–60.
15 Sanchez B, Hirzel AH, Bingisser R, Ciurea A, Exadaktylos A, Lehman B, et al. State of Emergency Medicine in Switzerland: a national profile of emergency departments in 2006. Int J Emerg Med. 2013;6(1):23.
16 Groupe de travail de la Communauté d'intérêt des directeurs médicaux des urgences. Centres d'urgence hospitaliers: Recommandations structurelles et organisationnelles en matière d'assurance qualité. Bull Med Suisses. 2005;86:1974–84.
17 Sullivan AF, Richman IB, Ahn CJ, Auerbarch BS, Pallin DJ, Schafermeyer RW, et al. A profile of US emergency departments in 2001. Ann Emerg Med. 2006;48:694–701.
18 Schneider SM, Gallery ME, Schafermeyer R, Zwemer FL. Emergency department crowding: a point in time. Ann Emerg Med. 2003;42:167–72.
19 Schuler M, Dessemontet P, Joye D. Les niveaux géographiques de la Suisse, Office Fédéral de la Statistique; Neuchâtel 2005.
20 Niska RW, Burt C. Emergency Response Planning in Hospitals, United States: 2003–2004. Adv Data. 2007;391:1–13.
21 Niska RW, Shimizu IM. Hospital preparedness for Emergency Response: United States, 2008. Natl Health Stat Report. 2011;37:1–14.
22 Ministère de la Santé et des Solidarités – République Française. Plan blanc et gestion de crise. Guide à l'élaboration des plans blancs élargis et des plans blancs des établissements de santé. Paris, 2006.
23 Auf der Heide E. The importance of evidence-based disaster planning. Ann Emerg Med. 2006;47:34–49.
24 Staines A. Trame, guide et standards pour l'élaboration des plans catastrophe des hôpitaux vaudois. Service Santé Publique Canton de Vaud, 2008.
25 Lynn M, Gurr D, Memon A, Kaliff J. Management of conventional mass casualty incidents: ten commandments for hospital planning. J Burn Case Res. 2006;27:649–58.
26 ED management 2013;25(7):78–80
27 Shih FY, Koenig KL. Improving surge capacity for biothreats: experience from Taiwan. Acad Emerg Med. 2006;13:1114–7.
28 Zilm F, Berry R, Pietrzak MP, Paratore A. Integrating disaster preparedness and surge capacity in emergency facility planning. J Ambul Care Manage. 2008;31:377–85.
29 American College of Emergency Physicians (ACEP). Health Care System Surge Capacity Recognition, Preparedness, and Response. Ann Emerg Med. 2012;59:240–1.
30 Walls RM, Zinner MJ. The Boston Marathon response: why did it work so well? JAMA. 2013;309(23):2441–2.
31 Conn A. Marathon day at Massachusetts General. Ann Intern Med. 2013;159(2):143–4.
32 Fischer P, Wafaisade A, Neugebauer EAM, Kees T, Bail H, Weber O, et al. Wie gut sind Aerzte auf einen Massenanfall von Verletzten vorbereitet? [Preparedness of hospital physicians for a mass casualty incident. A German survey amongst 7,700 physicians]. Unfallchirurg. 2013;116:34–8.