Toward standardised documentation in psychiatric evaluations: Identifying functioning aspects and contextual factors in psychiatric reports of Swiss disability claimants with chronic widespread pain
DOI: https://doi.org/10.4414/smw.2014.14008
Urban
Schwegler, Claudio
Peter, Jessica
Anner, Bruno
Trezzini
Summary
QUESTIONS UNDER STUDY: In Switzerland, psychiatric evaluations are crucial for deciding on eligibility of disability benefits for claimants with chronic widespread pain (CWP). However, the poor standardisation and low transparency of such evaluations have been criticised. Standardisation and transparency may be enhanced by comprehensive functioning documentation using the International Classification of Functioning, Disability and Health (ICF). We applied the ICF as a reference frame to determine a list of functioning aspects and contextual factors commonly reported in psychiatric work capacity evaluations of Swiss disability claimants with CWP.
METHODS: We conducted a retrospective qualitative and quantitative content analysis of 24 psychiatric reports of claimants with CWP by using the ICF taxonomy and a personal factor categorisation for data coding. Coded categories were considered candidate items for standardised documentation in psychiatric evaluations involving CWP if they passed a predetermined threshold based on their relative frequency across reports.
RESULTS: A total of 71 second level ICF and personal factor categories passed the threshold. In total, 21 categories referred to the ICF component personal factors, 19 to body functions, 18 to activities and participation, and 13 to environmental factors.
CONCLUSIONS: The list of ICF and personal factor categories we determined in this study addresses concepts commonly reported in psychiatric evaluations of medical work capacity involving CWP. It can serve as a starting point in developing a standard for comprehensive functioning documentation in the present context.
List of abbreviations
CWP: chronic widespread pain
GE-C: personal factor categorisation of Geyh et al.
ICF: International Classification of Functioning, Disability and Health
Mini ICF-APP: Mini-ICF-rating for limitations of activities and participation in psychological disorders
PEMWC: psychiatric evaluations of medical work capacity
Introduction
Chronic pain disorders account for a large number of disability claims and cause high costs for disability insurance providers [1]. Decisions on the eligibility of disability benefits are based on evaluations that determine the claimant’s diagnosis andmedical work capacity. Medical work capacity evaluations for chronic pain disorders are particularly challenging because of complex biopsychosocial interactions that determine functioning [2]. In claimants with chronic widespread pain (CWP), such as somatoform pain disorders or fibromyalgia, functional limitations often cannot be attributed to physical impairments and are considered to be caused predominantly by contextual factors such as the environment or personal factors [3].
In Switzerland, reduced medical work capacity is attested only when functional limitations result from a health condition and not merely from contextual factors. Swiss Social Security jurisprudence, therefore, does not accept CWP as a sufficient reason for a disability pension, except if accompanied by a severe psychiatric co-morbidity [4]. In fact, CWP is often accompanied by psychiatric co-morbidities like depression [5] or anxiety disorders [6], and mental problems such as post-traumatic stress [7] or attention deficits [8]. Such co-morbidities, and their effect on work function, are assessed in psychiatric evaluations of medical work capacity (PEMWC). Psychiatric evaluations are, thus, crucial for determining medical work capacity of claimants with CWP [9].
Accurate assessment and transparent documentation of functioning represent prerequisites for fair medical work capacity evaluations [10]. Swiss PEMWC usually report about a claimant’s functioning. However, they (1.) often fail to comprehensibly illustrate if functional limitations at work are more likely to result from a health condition (e.g., depression) or from environmental factors (e.g. family problems) or from personal factors (e.g., lack of motivation), and (2.) are generally reported using technical jargon [11]. Thus, current psychiatric reports hardly explain why claimants are declared able or unable to work, and they often do not allow for comparison between claimants’ functional limitations and the demands of potential workplaces either [12]. Moreover, although the evaluations should be comparable [13], PEMWC are often poorly standardised and lack inter-rater reliability [14, 15]. Swiss guidelines on PEMWC, for instance, are not generally binding and focus on formal aspects rather than on content-related issues [16, 17].
The International Classification of Functioning, Disability and Health(ICF) is the worldwide standard for reporting on functioning and disability [18]. The ICF framework conceptualises functioning holistically as the interplay between ahealth condition,
body functions and body structures, activities and participation as well as environmental and personal factors. In PEMWC, the ICF framework may facilitate a transparent illustration of how psychiatric symptoms affect a claimant’s functioning at work and of how contextual factors influence this process [12, 19]. The ICF taxonomy could promote standardised and comprehensible documentation of PEMWC in providing a common language for the description of functioning in mental disorders [20].
However, even though its framework is holistic and its taxonomy offers numerous categories for body functions, body structures, activities and participation, and environmental factors, the ICF fails to classify personal factors. Yet personal factors, such as a claimant’s occupational background or work motivation, also affect work functioning [21] and are thus of particular importance for PEMWC involving CWP [22]. Several authors have emphasised the need for personal factor categories within the ICF taxonomy [23, 24], and different personal factor categorisations have been developed for broader contexts [25, 26], but also specifically for medical work capacity evaluations [27, 28]. The most comprehensive categorisation available is the one by Geyh et al. [25] (henceforth GE-C), whose preliminary version comprises of 167 categories. The categorisation by Grotkamp et al. [28] represents the most up to date personal factor categorisation for medical work capacity evaluations and includes 59 categories specifically developed for this particular context. Table 1 provides an overview on these two categorisations.
|
Table 1: Overview of the personal factor categorisation by Geyh et al. and Grotkamp et al. |
|
Geyh-categorisation
|
|
Chapters
|
Number of categories
|
| |
Total |
2nd level |
3rd level |
4th level |
| i1 Socio-demographical factors |
11 |
8 |
3 |
|
| i2 Position in the immediate social and physical context |
7 |
5 |
2 |
|
| i3 Personal history and biography |
2 |
2 |
|
|
| i4 Feelings |
10 |
2 |
8 |
|
| i5 Thoughts and beliefs |
83 |
8 |
51 |
24 |
| i6 Motives |
37 |
3 |
18 |
16 |
| i7 General patterns of experience and behaviour |
17 |
4 |
8 |
5 |
| |
167
|
32
|
90
|
45
|
| |
|
Grotkamp-categorisation
|
|
Chapters
|
Number of categories
|
| |
Total |
2nd level |
3rd level |
4th level |
| i1 General personal characteristics |
9 |
3 |
6 |
|
| i2 Physical factors |
9 |
2 |
7 |
|
| i3 Mental factors |
10 |
10 |
|
|
| i4 Attitudes, basic skills and behaviour patterns |
20 |
20 |
|
|
| i5 Life situation and socio-economic/-cultural factors |
9 |
9 |
|
|
| i6 Other factors of health |
2 |
2 |
|
|
| |
59
|
46
|
13
|
|
| Based on Schwegler et al. [22]. The detailed version of the Geyh-categorisation is available from the corresponding author upon request. |
Applying the entire ICF taxonomy, including 362 categories on the second level (e.g. b280Sensation of pain) and up to 1,424 on the more precise third or fourth levels (e.g., b2801 Pain in body part or b28011 Pain in chest), would be too cumbersome for PEMWC [29]. A more parsimonious tool for documenting PEMWC represents the “Mini-ICF-rating for limitations of activities and participation in psychological disorders” (Mini ICF-APP) [29]. It is based on the activities and participation component of the ICF and offers category classifications for 13 mental work activities (i.e. activities requiring mental functions such as affective flexibility or cognitive planning). However, because the Mini-ICF-APP does not address body functions, or environmental or personal factors, it is presumably not sufficiently broad for comprehensive PEMWC. The condition-specific ICF Core Sets for CWP [30] are indeed comprehensive, but not specifically developed for psychiatry and thus may lack aspects relevant for PEMWC.
Since none of the existing approaches appears suitable for comprehensive documentation of PEMWC involving CWP, there is a need to determine an encompassing list of items relevant for this particular context. Believing that current psychiatric reports collectively comprise most of these relevant aspects, a content analysis of a number of such reports, using the ICF in combination with a personal factor categorisation as a coding frame, offers one possible mechanism for establishing candidate categories for comprehensive functioning documentation in PEMWC involving CWP.
Objective
The objective of this study was to determine functioning aspects and contextual factors commonly reported in PEMWC on Swiss disability claimants with CWP, using the ICF as a reference frame.
Specific aims
The specific aims were (1.) to content analyse and categorise the information contained in psychiatric reports of claimants with CWP using the ICF taxonomy and the GE-C and (2.) to determine candidate categories for standardised reporting of functioning and contextual factors in PEMWC involving CWP.
Methods
Study design
A retrospective qualitative and quantitative content analysis of psychiatric reports was conducted [31]. In the qualitative part, the content of the reports was coded using the ICF and the GE-C for personal factors. The categorisation by Grotkamp et al., which includes categories for coding specific personal factors in PEMWC, was used for specifying concepts not adequately classifiable with the GE-C. The quantitative part of the study consisted in a frequency analysis of the coded categories.
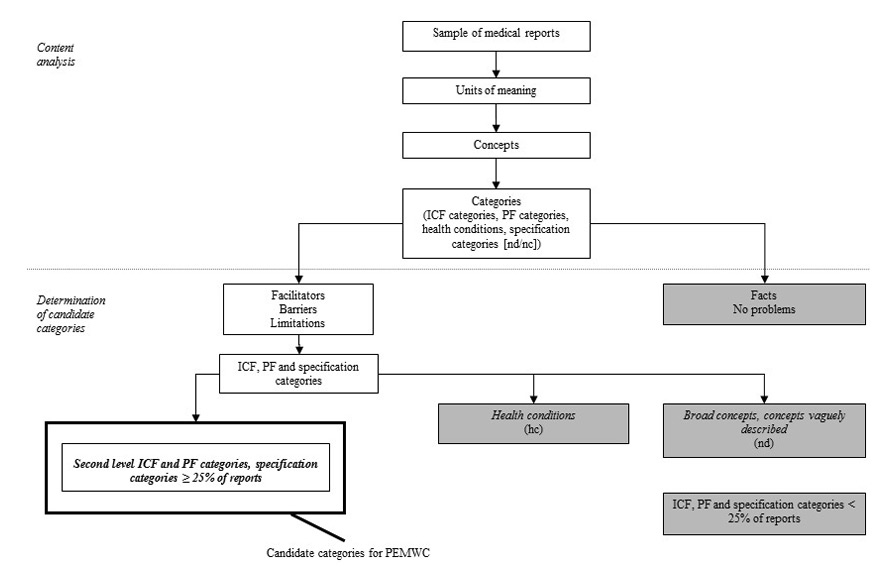
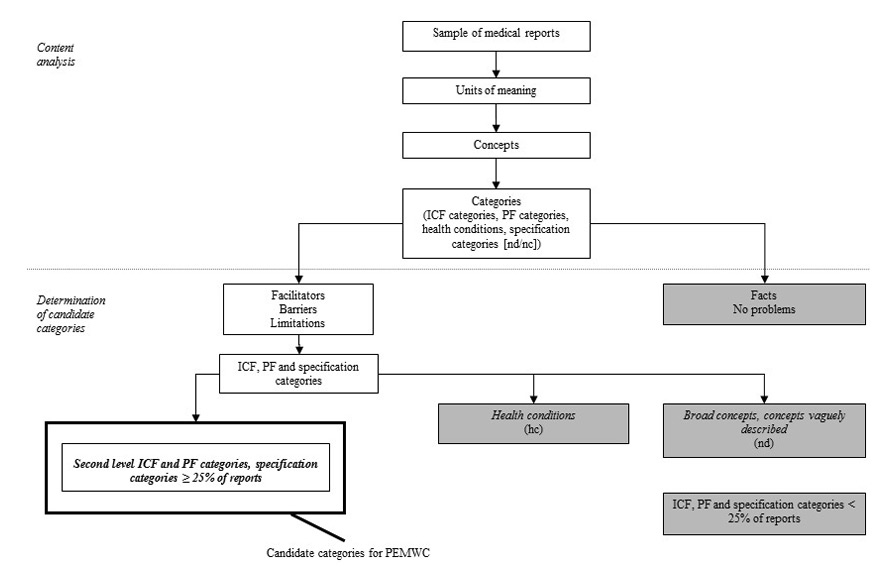
Figure 1
Overview of the selection process for the candidate categories.
PF = personal factor; hc = health conditions; nd = not definable with the ICF; nc = not covered by ICF; boxes shaded in grey refer to concepts that were excluded in the selection process for the candidate categories.
Ethics
The original study was approved by the Ethics Commission of Basel, Switzerland, project number 134/08, and conducted in accordance with the Declaration of Helsinki.
Sample
All medical reports submitted to the Swiss national disability insurance scheme between February 1st and April 30th, 2008, had been collected as part of a larger study [32]. From this pool of reports, all psychiatric reports in German involving claimants with anInternational Classification of Diseases (ICD-10) diagnosis of CWP (see table 2) were considered eligible for the present study. Due to limited resources, however, a random sub-sample was drawn, representing about one third of the eligible reports. The reports were either monodisciplinary or part of a multidisciplinary evaluation. In the latter case only the psychiatric part was analysed.
|
Table 2: ICD-10 diagnoses for CWP included in the sample. |
|
ICD-10 diagnoses for CWP
|
| F45.0
F45.1
F45.4
F54
F62.8
F32
F33
F34.1
F43.2
F54.8
M79
R52.2
R52.9
Z76 |
Somatisation disorder
Undifferentiated somatoform disorder
Persistent somatoform disorder
Psychological and behavioural factors associated with disorders or diseases classified elsewhere
Chronic pain personality syndrome
Mild, moderate and severe depressive episode, with somatic symptoms
Recurrent depressive disorder, with somatic symptoms
Dysthymia (in relation with pain)
Adjustment disorders (in relation with pain)
Other dorsalgia (e.g., panvertebral syndrome)
Other soft tissue disorders, not elsewhere classified (e.g., fibromyalgia)
Other chronic pain
Pain, unspecified
Persons encountering health services in other circumstances (e.g., conscious simulation) |
Analysis
Content analysis
The content of the reports was coded with the ICF taxonomy and the GE-C, following established linking rules [33]. The reports were first subdivided into units of meaningreferring to text parts with a common theme (e.g. “the claimant suffers from attention problems while driving”). Then, the concepts underlying a unit of meaning were specified (e.g., attention problems; driving) and coded to the most precise ICF or personal factor category (e.g., b140 Attention functions; d475 Driving). A concept could be coded to more than one category.
Concepts not appropriately codeable with ICF or personal factor categories represented either health conditions (e.g., depression) or specification categories. The latter were further distinguished into not covered by the ICF (e.g., self-mutilation) and not definable within the ICF (e.g., alternating activities). Personal factors not adequately classifiable with the GE-C were specified, where possible, with a code from the Grotkamp-categorisation. To ensure data quality, the coding was performed by two psychologists who had to reach agreement on the selected codes. Any disagreement was solved in consultation with a third subject matter specialist.
The coders also assessed whether functioning concepts expressed limitations (e.g., “suffering from lack of energy”), no problems (e.g., “being able to handle stress”) or facts (e.g., “working part-time”). If concepts referred to environmental or personal factors, the coders assessed whether they were barriers (e.g., “side-effects of drugs”) or facilitators (e.g., “having a high education”).
Determination of candidate categories
The importance of a limitation, barrier or facilitator related to functioning in a given population may be operationalised in two ways: (1.) based on its frequency across individuals, and (2.) based on its extent or severity in different individuals. The reports analysed provided information about the mere existence of a limitation, barrier or facilitator, but usually not about its extent or severity. Therefore, the importance of a category was defined as its relative frequency across reports (i.e. the percentage of reports it was addressed in at least once). Only categories assessed as limitations, barriers or facilitators, and thus assumed to influence the claimant’s functioning, were included in the analysis. Categories assessed as no problem or facts were excluded. Concepts referring to health conditionswere also removed as they can be classified using ICD-10. Finally, broad concepts(e.g., mental health) orconcepts vaguely described in the reports (e.g., shoulder complaints) were omitted because they cannot be described with one or a few specific categories.
The categories were aggregated to the second level of the ICF and the GE-C. All second level categories that passed a predetermined threshold at 25% (or more) of the reports, were considered candidate categories for standardised reporting on functioning and contextual factors in PEMWC involving CWP. Selecting a particular threshold value involves an arbitrary element. However, a 25% threshold was assumed to be sufficiently lenient to comprehensively capture the concepts contained in the reports.
Figure 1 gives an overview on the selection process for the candidate categories.
|
Table 3: Results of the coding process with the ICF and the personal factor categorisation by Geyh et al. (GE-C). |
| |
Psychiatric reports (n = 24)
|
| |
n
|
%
|
| Number of meaning units |
4209 |
|
| Number of identified concepts total |
7801 |
|
| Average number of categories used to code one concept |
1.2 |
|
| Number of codings (total) |
9314 |
|
| Number of codings (no problems/facts) |
4184 |
|
| Number of codings (limitation/barrier/facilitator) |
5130 |
|
| |
|
|
|
Per ICF component (limitation/barrier/facilitator)
|
4249
|
82.8
|
| Body functions |
1354 |
26.4 |
| Body structures |
61 |
1.2 |
| Activity and participation |
690 |
13.5 |
| Environmental factors |
651 |
12.7 |
| Personal factors |
1493 |
29.1 |
| |
|
|
|
Not appropriately codeable with ICF or GE-C (limitation/barrier/facilitator)
|
881
|
17.2
|
| Health conditions |
289 |
5.6 |
| Specification categories – not definable with ICF |
503 |
9.8 |
| Specification categories – not covered by ICF |
89 |
1.7 |
Results
Sample
The analysed sample included 24 psychiatric reports, representing about one third of the 67 eligible reports. Of these 24 reports, 15 reports were monodisciplinary and 9 were part of a multidisciplinary evaluation.
“F45.4 Persistent somatoform pain disorder” was the most frequent ICD-10 diagnosis of CWP and appeared in 13 (54.2%) reports. Four (16.7%) reports involved the diagnosis “M54.8 Panvertebral syndrome”, 3 (12.5%) involved “F45.1 Undifferentiated somatoform disorder”, and 2 (8.3%) involved “F33 Recurrent depressive disorder, with somatic symptoms” and “M79.7 Fibromyalgia”.
“F32 Depressive episode” appeared in 5 (20.8%) reports and was the most common co-morbidity, followed by “F33 Recurrent depressive disorder” and “F34.1 Dysthymia”, which were diagnosed in 3 (12.5%) reports.
Content analysis
Table 3 shows an overview of the results of the content analysis. A total of 4209 units of meaning were coded, resulting in 9314 codings. A total of 5130 (55.1%) of them referred to limitations, barriers or facilitators. Out of these, 4249 (82.8%) involved ICF or personal factor categories; the remainder (881; 17.2%) were not appropriately codeable with the ICF and the GE-C. Personal factors represented the most frequent ICF component with 1493 codings (29.1%), followed by body functions with 1354 (26.4%).
Candidate categories
Table 4 gives a detailed overview of the candidate categories and their relative frequency across reports. Overall, 71 second level ICF and personal factor categories passed the 25% threshold. In total, 21 of them referred to personal factors, 19 to body functions, 18 to activities and participation and 13 to environmental factors. In addition, one specification category of the ICF taxonomy and nine personal factors not adequately classifiable with the GE-C, and thus specified with a code from the Grotkamp-categorisation, passed the threshold.
|
Table 4: Second level candidate categories referring to ICF body functions (b), activities and participation (d), environmental factors (e), personal factors (i) and specification categories. |
|
ICF Code
|
ICF Category
|
Relative frequency across psychiatric reports (n = 24) in %
|
|
Body functions
|
|
| b280 |
Sensation of pain |
95.8 |
| b152 |
Emotional functions |
91.7 |
| b134 |
Sleep functions |
87.5 |
| b160 |
Thought functions |
83.3 |
| b130 |
Energy and drive functions |
75.0 |
| b455 |
Exercise tolerance functions |
58.3 |
| b147 |
Psychomotor functions |
45.8 |
| b270 |
Sensory functions related to temperature and other stimuli |
41.7 |
| b435 |
Immunological system functions |
41.7 |
| b140 |
Attention functions |
37.5 |
| b144 |
Memory functions |
37.5 |
| b460 |
Sensations associated with cardiovascular and respiratory functions |
33.3 |
| b530 |
Weight maintenance functions |
33.3 |
| b110 |
Consciousness functions |
29.2 |
| b240 |
Sensations associated with hearing and vestibular functions |
29.2 |
| b510 |
Ingestion functions |
29.2 |
| b640 |
Sexual functions |
29.2 |
| b730 |
Muscle power functions |
29.2 |
| b535 |
Sensations associated with the digestive system |
25.0 |
|
Activities and participation
|
|
| d850 |
Remunerative employment |
79.2 |
| d570 |
Looking after one's health |
75.0 |
| d240 |
Handling stress and other psychological demands |
70.8 |
| d760 |
Family relationships |
62.5 |
| d770 |
Intimate relationships |
62.5 |
| d720 |
Complex interpersonal interactions |
58.3 |
| d350 |
Conversation |
54.2 |
| d230 |
Carrying out daily routine |
41.7 |
| d330 |
Speaking |
33.3 |
| d845 |
Acquiring, keeping and terminating a job |
33.3 |
| d335 |
Producing nonverbal messages |
29.2 |
| d710 |
Basic interpersonal interactions |
29.2 |
| d740 |
Formal relationships |
29.2 |
| d430 |
Lifting and carrying objects |
25.0 |
| d445 |
Hand and arm use |
25.0 |
| d450 |
Walking |
25.0 |
| d475 |
Driving |
25.0 |
| d750 |
Informal social relationships |
25.0 |
|
Environmental factors
|
|
| e310 |
Immediate family |
95.8 |
| e165 |
Assets |
75.0 |
| e580 |
Health services, systems and policies |
75.0 |
| e110 |
Product or substances for personal consumption |
62.5 |
| e570 |
Social security services, systems and policies |
62.5 |
| e410 |
Individual attitudes of immediate family members |
41.7 |
| e325 |
Acquaintances, peers, colleagues, neighbours and community members |
37.5 |
| e315 |
Extended family |
33.3 |
| e355 |
Health professionals |
33.3 |
| e225 |
Climate |
29.2 |
| e245 |
Time-related changes |
29.2 |
| e320 |
Friends |
29.2 |
| e565 |
Economic services, systems and policies |
29.2 |
|
Personal factors
|
|
| i410 |
Emotions |
100.0 |
| i560 |
Personal evaluations |
100.0 |
| i740 |
Patterns of behaviours and handling behaviours |
91.7 |
| i310 |
Life events |
87.5 |
| i540 |
Personal beliefs |
87.5 |
| i160 |
Occupational background |
83.3 |
| i720 |
Patterns of thoughts and handling thoughts |
83.3 |
| i170 |
Economical background |
75.0 |
| i320 |
Biographical course |
75.0 |
| i630 |
Personal goals |
75.0 |
| i150 |
Educational background |
62.5 |
| i140 |
Language |
62.5 |
| i510 |
Knowledge and concepts |
58.3 |
| i710 |
Patterns of feelings and handling feelings |
58.3 |
| i580 |
Imagination, fantasy and dreams |
54.2 |
| i520 |
Personal memories |
41.7 |
| i620 |
Personal interests |
37.5 |
| i420 |
Moods |
37.5 |
| i530 |
Personal attitudes |
37.5 |
| i220 |
Position in partnership and marriage |
33.3 |
| i730 |
Patterns of motives and handling motives |
33.3 |
|
Specification categories
|
|
| nc(i130)* |
Genetic factors |
62.5 |
| i7(i453)* |
General patterns of experience and behaviour (use of stimulants) |
58.3 |
| i7(i433)* |
General patterns of experience and behaviour (methodological skills) |
41.7 |
| i7(i310–349)* |
General patterns of experience and behaviour (personality factors) |
33.3 |
| i7(i340)* |
Patterns of thoughts and handling thoughts (optimism) |
29.2 |
| i7(i436)* |
Patterns of thoughts and handling thoughts (self-competence) |
29.2 |
| i7(i335)* |
Patterns of thoughts and handling thoughts (self-confidence) |
25.0 |
| i7(i456)* |
General patterns of experience and behaviour (Physical activity habits) |
25.0 |
| i7(i430)* |
General patterns of experience and behaviour (social skills) |
25.0 |
| nd-selim†
|
Self-limitation |
25.0 |
| * = Personal factor categories specified with the categorisation by Grotkamp et al. [28];
† = Specification category of the ICF taxonomy. Categories grouped into ICF components and ordered by their relative frequency across reports. Threshold at 25%. |
Discussion
Drawing on a sample of current psychiatric reports and using the ICF as a reference frame, we determined a list of functioning aspects and contextual factors commonly reported in PEMWC on Swiss disability claimants with CWP. The content of the reports could be largely captured with the ICF and the GE-C. The most common categories referred to the ICF components personal factors, body functions, activities and participation, and environmental factors (see table 4).
The most common ICF component in terms of both absolute frequency of codings and number of categories above the threshold was personal factors (see table 3 and 4), the component not classified in the ICF taxonomy. This finding indicates the key role of personal factors in PEMWC involving CWP and is in line with current guidelines on PEMWC [16] and literature on personal factors in the present context [22].
Emotions (i410) and personal evaluations (i560) related to one’s health condition or job were addressed in all reports (see table 4). Documenting these concepts, which may represent barriers or facilitators related to functioning, could help clarify the relationship between a claimant’s objective functioning and subjective experience [34]. Personal beliefs (i540), such as personal expectations regarding return to work, were commonly addressed as potential predictors for work participation [35]. Patterns of behaviour (i740) referring to daily routine and personal hobbies were also frequently reported. Comparing them with complaints about functional limitations may be useful for testing the consistency of a claimant’s subjective statements [36]. Finally, life events (i310) referring to traumatic experiences and information on the claimant’s occupational background (i160) were frequently reported too; the former as potential predictors for CWP [36], the latter as determinant of a claimant’s ability to perform certain jobs [37].
Body functions were the second most frequent ICF component (see table 3 and 4). The category “b280 Sensation of pain” was, not surprisingly, the most frequent body function category and reflects the claimant’s subjective pain complaints (see table 4). The mental functions “b152 Emotional functions” (e.g., emotional ability), “b134 Sleep functions” (e.g., problems with sleep maintenance), “b130 Energy and drive functions” (e.g., energy loss) and “b160 Thought functions” (e.g., somatisation) were common as well and represent symptoms of the major psychiatric co-morbidities of CWP.
Body functions, including mental functions, describe aspects of health and diagnoses but are less helpful for addressing restrictions in mental work activities [38]. However, the high frequency of mental functions as compared to activities and participation categories (see table 3 and 4) suggest that mental functions are often used for explaining work functioning without properly pointing out restrictions in mental work activities caused by the claimant’s symptoms. A similar finding emerged in a recent study on the quality of Swiss PEMWC [11].
Activities and participation were only the third most common ICF component (see table 3 and 4). This result was unexpected since restrictions in mental work activities and their effect on work functioning should usually be discussed in PEMWC. However, previous research has noted that psychiatric evaluations often struggle to properly illustrate how work activities are affected by psychiatric symptoms [38].
The category “d850 Remunerative employment” (i.e. work functioning) was the most frequent activities and participation category, followed by “d570 Looking after one’s health” (e.g., seeking medical assistance) (see table 4). Specific restrictions in mental work activities, such as lack of stamina to perform tasks or difficulties with tasks requiring affective flexibility, were also commonly documented. Although quite different from each other, these activities were mainly coded with the ICF categories “d240 Handling stress and other psychological demands” (e.g., handling responsibility) and “d230 Carrying out daily routine” (e.g., being able to coordinate one’s everyday life). This finding suggests that these categories are conceptualised too broadly and that the ICF lacks specificity for properly addressing mental work activities. A tool that provides specific categories for mental work activities like the Mini-ICF-APP [29] may be more accurate for their documentation in the present context.
Environmental factors were only the fourth most common of the ICF components (see table 3 and 4). However, the categories “e310 Immediate family” (e.g., supportive husband), “e580 Health services, systems and policies” (e.g., therapies) and “e165 Assets” (e.g., financial problems) were reported frequently (see table 4). Documenting these categories is important since family situation or availability of health services may influence work functioning [39]. Moreover, environmental factors can be used for reporting on barriers and facilitators at the workplace, such as the physical work environment or attitudes of authorities [19].
The number of categories used to specify concepts not appropriately classifiable with the ICF taxonomy and the GE-C was small. The nine personal factors that were not adequately classifiable with the GE-C and specified with the Grotkamp-categorisation mainly address personality characteristics and coping styles. The only specification category of the ICF above the threshold referred to the concept “self-limitation”, which reflects a common phenomenon in cognitions and actions of patients with somatoform pain disorders [40].
Study limitations
The current study has some limitations. First, our sample only included psychiatric reports with an ICD-10 diagnosis of CWP that were submitted to the Swiss national disability insurance over a limited time span of three months. The results are therefore not generalisable to other health conditions, nor to other medical disciplines, other insurance schemes or countries with different disability evaluation procedures. Moreover, the robustness of our findings is limited by the small number of 24 reports analysed. The time-consuming coding process did not allow us to analyse the entire sample of 67 eligible reports. A comparison of our sample size to other qualitative studies that used the ICF for data coding in PEMWC is not possible as similar studies are lacking in this context. However, with regard to the determination of an adequate sample size our study might have benefited from the application of a specific saturation criterion. It warrants highlighting that the total number of codings across reports does not affect the robustness of the results as we defined the importance of a coding based on its relative frequency and not based on its absolute frequency across reports. To test the robustness of our results a cross-validation based on a new sample of psychiatric reports on claimants with CWP would be needed.
Secondly, our findings are predicated on the quality and completeness of the psychiatric reports we used as our data source. It is possible that the reports did not always address all aspects considered relevant for PEMWC. In our study, we tried to alleviate this potential limitation by applying a rather lenient threshold at 25% to comprehensively capture the candidate categories across reports. However, other data sources, such as interviews with psychiatrists or claimants, need to be considered to complete and validate our findings.
Thirdly, the exclusion of concepts referring to health conditions, broad concepts and concepts vaguely described in the reports as well as of categories assessed as no problems or facts influenced our findings to a varying degree. The inclusion of concepts referring to health conditions and broad concepts would not have changed our list of candidate categories since these concepts cannot be classified with a particular ICF, personal factor or specification category. A clearer reporting of vaguely described concepts, however, would have allowed us to link them to specific categories, which presumably would have modified our list of candidate categories. The exclusion of categories assessed as no problems or facts may have affected our list of candidate items as well. Yet their exclusion was deemed justifiable because these categories reflect content routinely assessed by psychiatrists which is not related to the claimant’s functional limitations.
Finally, our results are dependent on the coding methodology we used. The two psychologists who conducted the linking sometimes experienced difficulties in assigning concepts to the appropriate ICF component. Especially with regard to feelings and personality aspects, it was challenging to decide whether a concept reflects a mental function or a personal factor. For some of the identified concepts, this led to the selection of categories from both components. On the one hand, these challenges arose because the reports did not always provide sufficient information to retrospectively determine whether a psychiatrist’s statements referred to psychiatric symptoms or to personal factors. On the other hand, the ICF and personal factor category definitions are not always sufficiently clear to allow for an unequivocal differentiation between components. Clearer, mutually exclusive category definitions or a study design based on expert interviews might have led to different results.
Practical implications
The suggested list of candidate categories could facilitate standardised ICF-based documentation of PEMWC involving CWP. Such documentation could enhance the inter-rater reliability of PEMWC with regard to what should be reported. Moreover, the identified categories could help to illustrate in a more transparent way how restrictions in mental work activities are related to psychiatric symptoms and contextual factors. Thus, the categories provide a common language for reporting on mental work functioning that is comprehensible for all persons involved in the process of PEMWC.
However, before implementing such a standardised documentation, further development, validation, and practical testing is required. For instance, further research is needed to arrive at more accurate categories for describing mental work activities. Additionally, whereas the identified categories indicate what aspects should be reported in PEMWC, they do not show how these aspects should be measured. The ICF taxonomy and the GE-C do not offer an appropriate operationalisation for their categories. Therefore, the categories may be linked to tools like the Mini-ICF-APP or validated measurement instruments like the Screening for Somatoform Disorders (SOMS) [41] to ensure proper operationalisation and measurement.
Conclusions
Most of the candidate categories we determined for PEMWC involving CWP refer to personal factors and body functions. Activities and participation categories and environmental factors were found to be less common in the psychiatric reports analysed. The identified categories can serve as a starting point towards the development of a standard of what to report in a comprehensive functioning documentation in PEMWC. However, how the categories could be operationalised and measured needs further research.
Acknowledgment:We thank Wolfgang Segerer for his support in preparing the database, and Szilvia Geyh for her guidance in the planning of the study and for critical revisions to the manuscript. In addition, the authors thank Academy of Swiss Insurance Medicine (asim) for their support in the data collection.
References
1 Silverman S, Dukes EM, Johnston SS, Brandenburg NA, Sadosky A, Huse DM. The economic burden of fibromyalgia: comparative analysis with rheumatoid arthritis. Curr Med Res Opin. 2009;25(4):829–40.
2 Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624.
3 Marelli R. Die Beurteilung der Arbeitsfähigkeit im Grenzbereich von Psyche und Soma. Schweizerische Ärztezeitung. 2008;89(25):1140–3.
4 Meyer-Blaser U. Der Rechtsbegriff der Arbeitsunfähigkeit und seine Bedeutung in der Sozialversicherung, namentlich für den Einkommensvergleich in der Invalidenversicherung. Schriftenreihe des Institutes für Rechtswissenschaft und Rechtspraxis IRP-HSG St Gallen 2003, Band 23:27–119.
5 Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–45.
6 Asmundson GJ, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety. 2009;26(10):888–901.
7 Kulich RJ, Mencher P, Bertrand C, Maciewicz R. Comorbidity of post-traumatic stress disorder and chronic pain: implications for clinical and forensic assessment. Curr Rev Pain. 2000;4(1):36–48.
8 Dick B, Eccleston C, Crombez G. Attentional functioning in fibromyalgia, rheumatoid arthritis, and musculoskeletal pain patients. Arthritis Rheum. 2002;47(6):639–44.
9 Schwegler U, Anner J, Boldt C, Glässel A, Lay V, De Boer WE, et al. Aspects of functioning and environmental factors in medical work capacity evaluations of persons with chronic widespread pain and low back pain can be represented by a combination of applicable ICF Core Sets. BMC Public Health. 2012;12(1):1088.
10 Meershoek A, Krumeich A, Vos R. Judging without criteria? Sickness certification in Dutch disability schemes. Sociol Health Illn. 2007;29(4):497–514.
11 Pizala H. Evaluation psychiatrischer Gutachten. PhD thesis. University of Basel; 2011.
12 Baron S, Linden M. The role of the “International Classification of Functioning, Disability and Health, ICF” in the description and classification of mental disorders. Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl 5):81–5.
13 Rudbeck M, Fonager K. Agreement between medical expert assessments in social medicine. Scand J Public Health. 2011;39(7):766–72.
14 Slebus FG, Kuijer PP, Willems JH, Frings-Dresen MH, Sluiter JK. Work ability assessment in prolonged depressive illness. Occup Med. (Lond) 2010;60(4):307–9.
15 Schandelmaier S, Fischer K, Mager R, Hoffmann-Richter U, Leibold A, Bachmann MS, et al. Evaluation of work capacity in Switzerland: a survey among psychiatrists about practice and problems. Swiss Med Wkly. 2013;143:w13890.
16 Schweizerische Gesellschaft für Psychiatrie und Psychotherapie (ed.): Qualitätsleitlinien für psychiatrische Gutachten in der Eidgenössischen Invalidenversicherung. Bern; 2012.
17 Schweizerische Gesellschaft für Versicherungspsychiatrie, Schweizerische Vereinigung ärztlicher Gutachter in Versicherungsfragen bei psychischen und psychosomatischen Störungen: Leitlinien der Schweizerischen Gesellschaft für Versicherungspsychiatrie für die Begutachtung psychischer Störungen. Schweizerische Ärztezeitung. 2004;85(20):1048–51.
18 World Health Organization: International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization; 2001.
19 Sanderson K, Nicholson J, Graves N, Tilse E, Oldenburg B. Mental health in the workplace: using the ICF to model the prospective associations between symptoms, activities, participation and environmental factors. Disabil Rehabil. 2008;30(17):1289–97.
20 Peterson DB. Psychological aspects of functioning, disability and health. New York: Springer; 2011.
21 Sjögren-Rönkä T, Ojanen MT, Leskinen EK, Tmustalampi S, Mälkiä EA. Physical and psychosocial prerequisites of functioning in relation to work ability and general subjective well-being among office workers. Scand J Work Environ Health. 2002;28(3):184–90.
22 Schwegler U, Peter C, Trezzini B, Anner J, Geyh S. Toward transparent documentation in medical work capacity evaluations: identifying personal factors in medical reports on Swiss disability claimants with chronic widespread pain. Int J Rehabil Res. 2013;36(4):298–307.
23 MacDonald-Wilson K, Nemec P. The International Classification of Functioning, Disability and Health (ICF) in Psychiatric Rehabilitation. Rehabilitation Education. 2005;19(2–3):159–76.
24 Duchan JF. Where is the person in the ICF? Advances in Speech-Language Pathology. 2004;6(1):63–5.
25 Geyh S, Cieza A, Bickenbach JE, Stucki G. ICF Personal Factors Preparatory Outline. In. Nottwil: ICF Research Branch; 2009.
26 Badley E. More than facilitators and barriers: Fitting the full range of environmental and personal contextual factors into the ICF model. In: Proceedings of the twelfth annual North American Collaborating Centre Conference on ICF: 2006; Vancouver; 2006.
27 Viol M, Grotkamp S, van Treeck B, Nüchtern E, Hagen T, Manegold B, et al. Personenbezogene Kontextfaktoren, Teil I. Ein erster Versuch zur systematischen, kommentierten Auflistung von geordneten Anhaltspunkten für die sozialmedizinische Begutachtung im deutschen Sprachraum. Gesundheitswesen. 2006;68(12):747–59.
28 Grotkamp S, Cibis W, Nüchtern E, Baldus A, Behrens J, Bucher PO, et al. Personal factors of the ICF. Gesundheitswesen. 2012;74(7):449–58.
29 Linden M, Baron S. The “Mini-ICF-Rating for Mental Disorders (Mini-ICF-P)”. A short instrument for the assessment of disabilities in mental disorders. Rehabilitation. (Stuttg) 2005;44(3):144–51.
30 Cieza A, Stucki G, Weigl M, Kullmann L, Stoll T, Kamen L, et al. ICF Core Sets for chronic widespread pain. J Rehabil Med. 2004(44 Suppl):63–8.
31 Miller DC, Salkind NJ (eds.). Handbook of research design and social measurement 6th edition. Thousand Oaks: Sage; 2002.
32 Eichler K, Imhof D, Bollag Y, Stohr S, Gyr N, Auerbach H. Satisfaction of staff of Swiss insurance companies with medical appraisals: a cross sectional study. BMC Res Notes. 2011;4:83.
33 Cieza A, Geyh S, Chatterji S, Kostanjsek N, Üstün B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med. 2005;37(4):212–8.
34 Geyh S, Müller R, Peter C, Bickenbach JE, Post MW, Stucki G, et al. Capturing the psychologic-personal perspective in spinal cord injury. Am J Phys Med Rehabil. 2011;90(11 Suppl 2):S79–96.
35 Finger ME, Escorpizo R, Glässel A, Gmünder HP, Lückenkemper M, Chan C, et al. ICF Core Set for vocational rehabilitation: results of an international consensus conference. Disabil Rehabil. 2012;34(5):429–38.
36 Widder B, Dertwinkel R, Egle UT, Foerster K, Schlitenwolf M. Leitlinie für die Begutachtung von Schmerzen. Psychotherapeut. 2007;52(5):334–46.
37 Heerkens Y, Engels J, Kuiper C, Van der Gulden J, Oostendorp R. The use of the ICF to describe work related factors influencing the health of employees. Disabil Rehabil. 2004;26(17):1060–6.
38 Baron S, Linden M. Disorders of functions and disorders of capacity in relation to sick leave in mental disorders. Int J Soc Psychiatry. 2009;55(1):57–63.
39 Bautz-Holter E, Sveen U, Cieza A, Geyh S, Roe C. Does the International Classification of Functioning, Disability and Health (ICF) core set for low back pain cover the patients’ problems? A cross-sectional content-validity study with a Norwegian population. Eur J Phys Rehabil Med. 2008:44(4):387–97.
40 Knecht T. Somatoforme Schmerzstörungen – Kann abnormales Krankheitsverhalten adaptiv sein? Psychiatrie und Neurologie. 2009;3:31–4.
41 Rief W, Hiller W. Screening für Somatoforme Störungen (SOMS). Manual. (2., vollständig überarbeitete und neu normierte Auflage). Bern: Hans Huber; 2008.