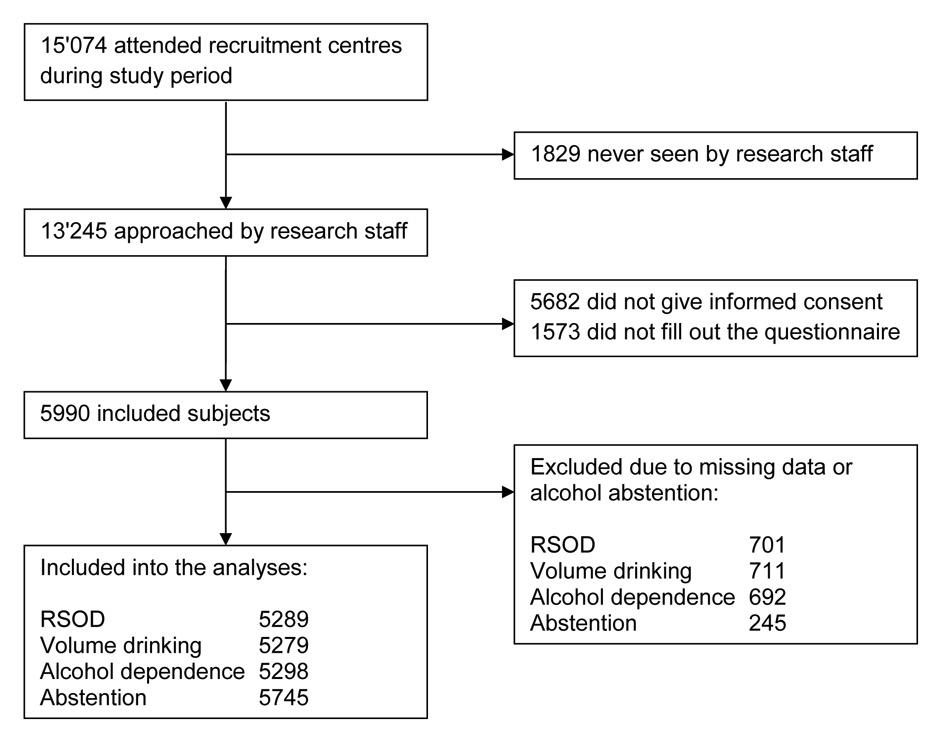
Figure 1
Flow chart of sample recruitment.
DOI: https://doi.org/10.4414/smw.2014.14007
A baseline-analysis of the C-SURF-study (Cohort Study on Substance Use Risk Factors)
In adolescents and young adults, the use of substances like alcohol, tobacco, cannabis and other illicit substances is a common phenomenon. Alcohol is quantitatively the most widely used substance that is consumed by adolescents and young adults especially in developed countries [1]. In this age group, epidemiological data show a continuous increase of alcohol consumption up to intoxication in several European countries [2, 3]. Often, excessive consumption of alcohol begins in adolescence. One report of the ESPAD-study (European School Survey on Alcohol and other Drugs) showed that more than half of the students at the age of 13 years or younger have already consumed alcohol [4]. According to the HBSC-study (Health Behaviour in School-aged Children) several countries had a significant increase in the proportion of 15–year-olds having been drunk twice or more times in their life [2]. In a Swiss population study similar to ours, subjects who reported first alcohol intoxication before age 15 were more likely to present risky single occasion drinking (RSOD), volume drinking, current cannabis use and other illicit drug use [5]. Therefore, alcohol prevention has to start early in life.
Switzerland has a relatively high rate of alcohol consumption per capita in comparison with other European countries [6, 7]. According to data from 2011, the average consumption was about 10.6 g pure alcohol per day for men 15 years and older, and 4.7 g pure alcohol for women in this age group, more than 50% above the global average [7]. The number of alcohol-dependent persons in Switzerland was conservatively estimated at about 250,000, representing approximately 3.9% of the population aged 15 and higher [6].
Alcohol consumption contributes to morbidity and mortality worldwide and is the third largest risk factor for disease burden in developed countries [8]. In adolescents and young adults, however, excessive alcohol consumption is the biggest risk factor for mortality and morbidity in developed countries. In Switzerland, it was estimated that 8.7% of all deaths among 15 to 74 year olds and 20.9% of all deaths among 15 to 24 year old men are attributable to alcohol [7]. Harmful alcohol use is often associated with risk behaviours such as use of other substances (tobacco, cannabis, other illicit drugs), violence, sexual risk behaviour and motor vehicle accidents [3, 5, 9, 10]. Alcohol consumption by minors can lead to numerous consequences, including academic problems, delinquency or other judicial consequences, or unintended pregnancy [3]. Adverse consequences extend into the social environment (family, friends, employers, educational institutions, society) and have high social costs [11, 12].
Previous studies described the family environment as risk factor for the development of problematic alcohol use among adolescents and young adults [13–15]. The family and the role of the parents can have an influence on the addictive behaviour of the offspring in different ways: family structure such as growing up in a single – or two-parent family, the level of education of the parents, their socio-economic position, the parental control of leisure behaviour and reaction to detected substance use, parental affection and support, satisfaction with the relationship with the parents and known parental substance abuse [4, 13, 16–18]. Reviews describe the relevance of the family environment [15, 19] and emphasise an intact family structure and an active supportive parental behaviour as a protective factor and disruption in normal family functioning as a negative factor for adolescent substance use. In the existing literature, there is no uniform way to define and examine parenting. We used a quantitative parenting variable consisting of the following elements: monitoring, rule-setting and knowing the whereabouts. This combination of parenting parameters has been formerly used and was identified as predictive of college student drinking [20]. We did not investigate gender-specific parenting by differentiating between mother or father authoritativeness as recommended by others [21]. Neither did we examine up to what degree higher active parenting influences alcohol consumption patterns.
The aim of this study was to determine in a population-based sample of Swiss men whether their earlier family situation was associated with alcohol consumption at the age of around 20 years. The earlier family situation parameters included active parenting (monitoring, rule-setting and knowing the whereabouts), single parent family and a parental substance use problem. We hypothesise that active parenting, living with both parents and no known parental alcohol or drug problem are associated with lower alcohol consumption of the son.
This study was a retrospective observational cross-sectional analysis of baseline data from the Cohort Study on Substance Use Risk Factors (C-SURF) [22, 23]. C-SURF is a prospective cohort study in Switzerland aimed at investigating the use of alcohol, tobacco, cannabis and other drugs in young men. Between August 2010 and November 2011 the participants were recruited during a mandatory army conscription process in three out of six recruitment centres in Switzerland, covering 21 of 26 Swiss cantons. Virtually all Swiss men must go through this recruitment process to determine their eligibility for military, civil or no service around the age of 19. As there is no pre-selection to army conscription, a representative sample of young Swiss men was thereby eligible for the study. Representativeness was not given for Switzerland as a whole because, for example, the canton Zurich and the Italian-speaking canton Ticino were missing. However, the study covered all French-speaking cantons and a wide range of German-speaking cantons, including more urban regions (e.g., Basel) and more rural regions (e.g., Uri). As virtually all young men pass the conscription procedures, the sample included socio-economically advantaged conscripts as well as conscripts from poorer family backgrounds. This was an advantage over many studies mainly using college students [24–26]. The conscripts were informed that the study was not connected with the army in any way and that they received a remuneration of CHF 30 for completing the questionnaire. All participants gave written, informed consent, as required by the Ethics Committee for Clinical Research at the Lausanne University Medical School, which approved the study (protocol number 15/07). Conscripts who provided informed consent were invited to fill out a questionnaire about socio-demographic status, family situation, physical and mental health, alcohol, tobacco, cannabis, other substances or drugs, recreational activities, sexuality and personality. The English version of the C-SURF questionnaire is freely accessible on the C-SURF webpage (http://www.c-surf.ch/img/pdf/q1_baseline_en.pdf).
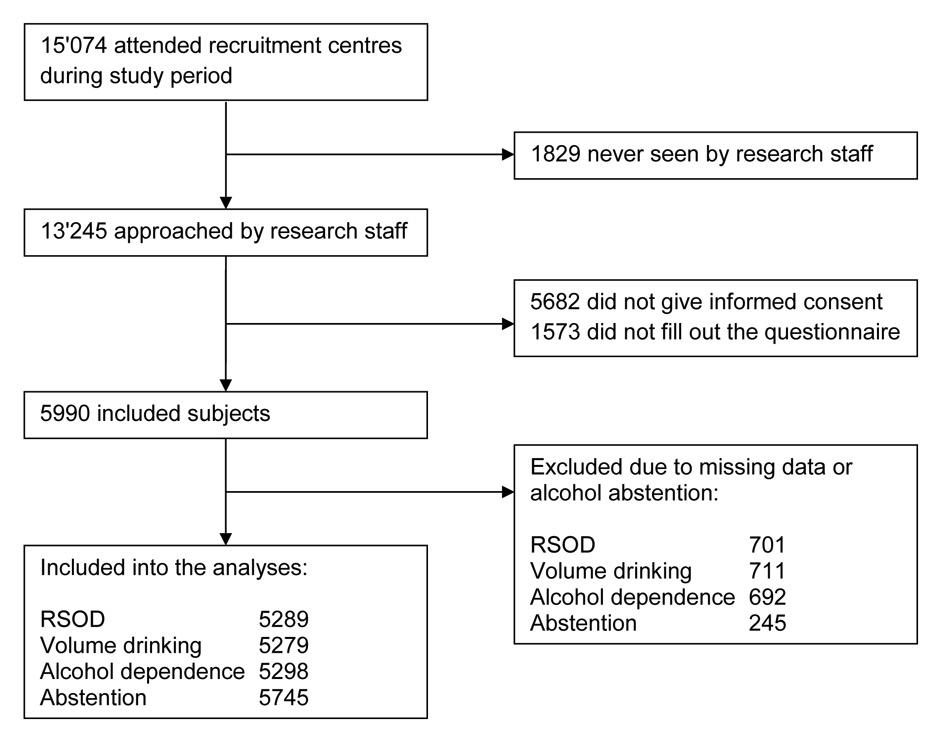
Figure 1
Flow chart of sample recruitment.
Of the 15,074 conscripts who presented to one of the three recruitment centers, 1,829 were never seen by the research staff because they were randomly selected for another study or because they were not informed by the military staff about the study. Of the remaining conscripts, 57.1% (7,563) provided informed consent. There were only small differences regarding substance use between consenters and non-consenters [27], and differences went into different direction (e.g., more smokers but fewer alcohol consumers among non-consenters). Among consenters, 79.2% (5,990) subsequently filled out the questionnaire (German speaking 82.2%, French speaking 74.3%). To sum up, the study was not a convenience sample as it was intended to enroll all conscripts in these three centres. Non-response and lack of informed consent of some participants compromised representativeness to a small degree. Enrolment and response rate of the C-SURF-study were further described and investigated by Studer et al. [28]. Figure 1 shows the sample recruitment.
Alcohol use was assessed with four different measures: alcohol abstention, risky single occasion drinking (RSOD), volume drinking and alcohol dependence.
Alcohol abstention was defined as reported lifetime abstention or the combination of less than 12 drinks per lifetime and no consumption of an alcoholic beverage during the last 12 months. Abstention from alcohol consumption was investigated by asking the following questions: ‘did you ever drink alcohol (in your lifetime)?’, ‘did you ever consume at least 12 alcoholic standard drinks (in your lifetime)?’ and ‘did you drink at least one alcoholic standard drink in the last 12 months?’.
RSOD was defined as having six or more standard drinks of about 10 grams per standard drink (>= 60 g alcohol) on one occasion at least monthly. This corresponded with the meaning of binge drinking introduced by Wechsler and colleagues [29, 30] with five or more US standard drinks (a standard drink being 12 grams of pure ethanol) on a single occasion. We assessed RSOD by asking ‘How often do you drink six or more alcoholic beverages on one occasion?’. The answer categories were: ‘every day or almost every day’, ‘every week’, ‘every month’, ‘less than once a month’ and ‘never’.
Volume drinking was defined as a weekly average intake of at least 210 g pure alcohol (equivalent to 21 or more standard drinks) [31, 32]. Pictures of standard drinks with approximately 10 g of pure ethanol were provided, e.g., 250 ml beer, 100 ml wine, 275 ml mixed drinks with high-proof alcohol or 50 ml of aperitifs.
Volume drinking was assessed by asking on the frequency and on the quantity of alcohol usually drank per drinking day using the following questions: ‘On how many days per week do you usually drink alcohol?’ and ‘How many alcoholic standard drinks do you consume on average during a day, on which you drink alcohol?’
Alcohol dependence was defined according to DSM-IV as a presentation of at least three of seven criteria occurring at any time during a 12–month period [33]. These criteria were transformed into questions like ‘Did it happen in the last 12 months that you spent a great deal of time in activities necessary to obtain, to use or to recover from the effect of drinking?’ [34].
Single parent family was defined as living with parents being divorced or having separated permanently sometimes before the 18th birthday. The conscripts answered in dichotomised answer categories ‘yes’ or ‘no’.
Parental problematic substance use was defined as the conscripts’ perception of an alcohol or drug substance problem of his mother or father or both. We combined the answer categories ‘no’, ‘alcohol’ and ‘drugs’ of each parent into a dichotomised variable ‘yes’ or ‘no’.
To examine the parental influence through rule-setting, monitoring and knowing the whereabouts, a parenting-variable was defined with a sum of scores from four questions: ‘My parents were setting clear rules, what I could do at home’, ‘My parents were setting clear roles, what I could do outside of home’, ‘My parents knew with whom I spent the evenings’, ‘My parents knew where I spent my evenings’. Each question scored 0 to 4 points with the answers ‘almost never’, ‘rarely’, ‘sometimes’, ‘often’, ‘almost always’. The range of the parenting variable was 0 to 16 with higher numbers describing higher active parenting (more rule-setting, monitoring and knowing the whereabouts) and lower numbers describing passive parenting (less rule-setting, monitoring and knowing the whereabouts). Questions have been developed for the ESPAD-survey [35], and were used in a recent study on the same sample [36].
Analyses were adjusted for the following potential confounding variables: age, language region, marriage or solid partnership, financial situation of the family, and highest completed education of either parent. The confounding variables were selected based on previous evidence and clinical experience. The financial situation of the family was measured by the recruits' perception of their own family’s socio-economic circumstances with the following question: ‘How do you rate the financial situation of your family compared to other families in Switzerland?’ We recoded the response categories in the categories: worse off, average, better off.
Baseline characteristics of the examined population were described using means, proportions and frequencies. For each outcome, we estimated unadjusted and fully adjusted logistic regression models [37] to assess the associations between the outcome and the exposure variables and confounders. Results were reported as odds ratios (OR) with associated 95% confidence intervals (CI). Parameters were considered statistically significant when the CI did not include 1, corresponding to a p-value <0.05. We used the Wald-test to determine whether the categorical variables significantly contributed to the outcomes and Nagelkerke R-square to assess goodness of fit [37]. We only included those cases which had no missing values. All analyses were performed using the statistical software package SPSS (version 19.0).
| Table 1:Baseline characteristics of the analysed sample. | ||
| total n* | % | |
| Age | ||
| 18 years and younger | 1091 | 18.2 |
| 19 years | 2467 | 41.2 |
| 20 years | 1445 | 24.1 |
| 21 years | 562 | 9.4 |
| over 22 years | 423 | 7.1 |
| Region | ||
| French | 3314 | 55.3 |
| German | 2676 | 44.7 |
| Partnership | ||
| marriage or steady partnership | 302 | 5.1 |
| single or non-steady partnership | 5636 | 94.9 |
| Family factors | ||
| parents separated | 1505 | 25.6 |
| parents not separated | 4373 | 74.4 |
| parental alcohol or drug problem | 412 | 6.9 |
| no parental alcohol or drug problem | 5547 | 93.1 |
| Parent's highest education | ||
| mandatory | 376 | 6.4 |
| vocational training | 2069 | 35.2 |
| grammar school | 912 | 15.5 |
| tertiary | 2515 | 42.8 |
| Family finance | ||
| lower than average | 2627 | 44.1 |
| average | 2473 | 41.5 |
| above average | 862 | 14.5 |
| Alcohol use | ||
| abstainer | 349 | 5.8 |
| non-abstainer | 5635 | 94.2 |
| Volume drinking (at least 21 drinks/week) | ||
| volume drinker | 375 | 6.9 |
| not volume drinker | 5097 | 93.1 |
| RSOD (at least 6 drinks once/month) | ||
| RSOD | 2746 | 50.1 |
| no RSOD | 2739 | 49.9 |
| Alcohol dependence (DSM IV) | ||
| non-dependence: score 0–2 | 4888 | 89.0 |
| dependence: score 3–7 | 606 | 11.0 |
| Notes: | ||
| * | the number of subjects (n) varies between the subscale scores due to missing data | |
| RSOD | risky single occasion drinking | |
| DSM IV | Diagnostic and Statistical Manual of Mental Disorders, 4th Edition | |
| Table 2:Unadjusted and adjusted models for RSOD. | |||||||
| unadjusted | adjusted | ||||||
| Exposures | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Single parent family | yes vs no | 0.97 | (0.86–1.10) | 0.610 | 0.94 | (0.82–1.07) | 0.344 |
| Parental drug or alcohol problem | yes vs no | 1.13 | (0.91–1.39) | 0.279 | 1.24 | (0.99–1.56) | 0.059 |
| Parenting | per increase scale 0 – 16 | 0.95 | (0.94–0.97) | <0.001 | 0.94 | (0.93–0.96) | <0.001 |
| Confounders | |||||||
| Age | <0.001a | <0.001a | |||||
| 18: reference | 1 | 1 | |||||
| 19 | 1.02 | (0.88–1.18) | 1.02 | (0.88–1.19) | |||
| 20 | 0.94 | (0.80–1.11) | 0.95 | (0.80–1.12) | |||
| 21 | 0.74 | (0.60–0.92) | 0.75 | (0.60–0.94) | |||
| >21 | 0.58 | (0.45–0.74) | 0.59 | (0.46–0.77) | |||
| Language | German vs French | 1.08 | (0.97–1.20) | 0.157 | 0.99 | (0.89–1.12) | 0.922 |
| Married | yes vs no | 0.76 | (0.59–0.97) | 0.030 | 0.79 | (0.61–1.02) | 0.074 |
| Parents‘ Education | <0.001a | <0.001a | |||||
| mandatory | 0.53 | (0.41–0.68) | 0.54 | (0.42–0.71) | |||
| vocational training | 0.95 | (0.84–1.07) | 0.97 | (0.86–1.10) | |||
| grammar school | 0.85 | (0.73–1.00) | 0.87 | (0.74–1.03) | |||
| tertiary: reference | 1 | 1 | |||||
| Family finance | 0.008a | 0.021a | |||||
| below average | 1.30 | (1.10–1.53) | 1.28 | (1.07–1.52) | |||
| average | 1.22 | (1.03–1.44) | 1.25 | (1.05–1.49) | |||
| above average: reference | 1 | 1 | |||||
| Notes: N= 5289 a: Wald-test: test of significance for categorical variables unadjusted: bivariate logistic regression analysis – adjusted: multivariate logistic regression analysis Parenting: sum of score from four questions (each 0–4), higher numbers meaning higher active parenting (monitoring, rule-setting, knowing the whereabouts) Reference: reference group for OR calculations with polytomous categorical or ordinal variables | |||||||
The socio-demographic characteristics and alcohol use patterns of the sample are shown in table 1. The mean age of the examined conscripts was 19.51 years (SD 1.27, range 18 to 31 years). 83.5% of all were 20 years old or younger. The mean age of the French speaking participants was somewhat higher than the mean age of those speaking German: 19.79 years (SD 1.31) versus 19.17 years (SD 1.11). Alcohol consumption was very common in this sample of young men in Switzerland. Only 5.8% of all examined Swiss conscripts reported being abstinent from alcohol. Among the non-abstainers, 50.1% reported RSOD behavior and 6.9% reported volume drinking. Alcohol dependence was found in 11%.
Tables 2 to 5 report the results of the logistic regression models for each outcome. RSOD was negatively associated with active parenting (OR 0.94, 95% CI 0.93–0.96) but not associated with single parent family and only as a tendency with parental problematic substance use (OR 1.24, 95% CI 0.99–1.56) in the adjusted multiple logistic regression model. Younger people and persons whose parents had a tertiary school education were more likely to report RSOD. RSOD was also negatively associated with the self-perceived financial situation of the family. We found no association of RSOD with marital status or language.
Volume drinking was negatively associated with active parenting (OR 0.92, 95% CI 0.89–0.95) and positively associated with parental problematic substance use (OR 1.86, 95% CI 1.30–2.66) in the adjusted model. Volume drinking was not associated with single parent family and any of the confounders.
Dependence was negatively associated with parenting (OR 0.94, 95% CI 0.92–0.97) and positively associated with parental problematic substance use (OR 1.76, 95% CI 1.30–2.39) in the adjusted model. Dependence was not associated with single parent family. Persons from the German language region were more likely to report alcohol dependence than those from the French region. The other confounders were not associated with alcohol dependence.
Alcohol abstention was not associated with single parent family, parental problematic substance use and parenting in the adjusted model. Among the confounders, age and self-perceived financial situation of the family were positively associated with abstention, tertiary parents’ education was negatively associated with abstention.
The analysis of RSOD, volume drinking and dependence did not include the abstinent participants, therefore the number of analysed subjects was lower for these outcomes. Due to missing data the number of analysed participants varied slightly between outcomes.
| Table 3:Unadjusted and adjusted models for volume drinking. | |||||||
| unadjusted | adjusted | ||||||
| Exposures | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Single parent family | yes vs no | 1.28 | (1.01–1.62) | 0.040 | 1.09 | (0.84–1.40) | 0.527 |
| Parental drug or alcohol problem | yes vs no | 1.97 | (1.41–2.77) | <0.001 | 1.86 | (1.30–2.66) | <0.001 |
| Parenting | per increase scale 0 – 16 | 0.92 | (0.89–0.95) | <0.001 | 0.92 | (0.89–0.95) | <0.001 |
| Confounders | |||||||
| Age | 0.155a | 0.092a | |||||
| 18: reference | 1 | 1 | |||||
| 19 | 1.20 | (0.89–1.62) | 1.13 | (0.83–1.53) | |||
| 20 | 1.11 | (0.80–1.55) | 1.02 | (0.72–1.44) | |||
| 21 | 0.72 | (0.44–1.19) | 0.63 | (0.38–1.05) | |||
| >21 | 0.84 | (0.50–1.43) | 0.74 | (0.43–1.28) | |||
| Language | German vs French | 0.98 | (0.79–1.22) | 0.860 | 0.97 | (0.77–1.22) | 0.796 |
| Married | yes vs no | 1.09 | (0.68–1.77) | 0.715 | 1.03 | (0.63–1.67) | 0.921 |
| Parents‘ Education | 0.507a | 0.429a | |||||
| mandatory | 0.80 | (0.47–1.39) | 0.76 | (0.43–1.33) | |||
| vocational training | 1.05 | (0.82–1.34) | 1.06 | (0.82–1.36) | |||
| grammar school | 1.20 | (0.88–1.63) | 1.20 | (0.88–1.64) | |||
| tertiary: reference | 1 | 1 | |||||
| Family finance | 0.750a | 0.566a | |||||
| below average | 0.99 | (0.71–1.38) | 1.16 | (0.81–1.66) | |||
| average | 1.08 | (0.77–1.51) | 1.21 | (0.85–1.71) | |||
| above average: reference | 1 | 1 | |||||
| Notes: N= 5279 a: Wald-test: test of significance for categorical variables unadjusted: bivariate logistic regression analysis – adjusted: multivariate logistic regression analysis Parenting: sum of score from four questions (each 0–4), higher numbers meaning higher active parenting (monitoring, rule-setting, knowing the whereabouts) Reference: reference group for OR calculations with polytomous categorical or ordinal variables | |||||||
| Table 4:Unadjusted and adjusted models for alcohol dependence. | |||||||
| unadjusted | adjusted | ||||||
| Exposures | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Single parent family | yes vs no | 1.22 | (1.01–1.47) | 0.041 | 1.11 | (0.90–1.35) | 0.330 |
| Parental drug or alcohol problem | yes vs no | 1.78 | (1.33–2.36) | <0.001 | 1.76 | (1.30–2.39) | <0.001 |
| Parenting | per increase scale 0 – 16 | 0.94 | (0.91–0.96) | <0.001 | 0.94 | (0.92–0.97) | <0.001 |
| Confounders | |||||||
| Age | 0.514a | 0.437a | |||||
| 18: reference | 1 | 1 | |||||
| 19 | 0.97 | (0.76–1.22) | 1.00 | (0.78–1.27) | |||
| 20 | 1.07 | (0.83–1.39) | 1.13 | (0.86–1.48) | |||
| 21 | 0.87 | (0.61–1.24) | 0.91 | (0.63–1.33) | |||
| >21 | 0.78 | (0.52–1.18) | 0.79 | (0.51–1.22) | |||
| Language | German vs French | 1.26 | (1.06–1.49) | 0.009 | 1.27 | (1.06–1.53) | 0.011 |
| Married | yes vs no | 0.85 | (0.56–1.29) | 0.438 | 0.82 | (0.54–1.26) | 0.374 |
| Parents' Education | 0.094a | 0.085a | |||||
| mandatory | 0.72 | (0.47–1.09) | 0.69 | (0.45–1.07) | |||
| vocational training | 0.82 | (0.68–1.00) | 0.80 | (0.65–0.98) | |||
| grammar school | 0.81 | (0.62–1.04) | 0.82 | (0.63–1.06) | |||
| tertiary: reference | 1 | 1 | |||||
| Family finance | 0.581a | 0.986a | |||||
| below average | 0.99 | (0.76–1.28) | 0.87 | (0.78–1.35) | |||
| average | 0.90 | (0.69–1.18) | 0.89 | (0.77–1.34) | |||
| above average: reference | 1 | 1 | |||||
| Notes: N= 5298 a: Wald-test: test of significance for categorical variables unadjusted: bivariate logistic regression analysis – adjusted: multivariate logistic regression analysis Parenting: sum of score from four questions (each 0–4), higher numbers meaning higher active parenting (monitoring, rule-setting, knowing the whereabouts) Reference: reference group for OR calculations with polytomous categorical or ordinal variables | |||||||
| Table 5:Unadjusted and adjusted models for alcohol abstention. | |||||||
| unadjusted | adjusted | ||||||
| Exposures | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Single parent family | yes vs no | 0.84 | (0.64–1.09) | 0.187 | 0.79 | (0.59–1.05) | 0.099 |
| Parental drug or alcohol problem | yes vs no | 1.14 | (0.75–1.73) | 0.547 | 1.01 | (0.65–1.58) | 0.973 |
| Parenting | per increase scale 0 – 16 | 1.01 | (0.98–1.05) | 0.427 | 1.03 | (0.99–1.07) | 0.074 |
| Confounders | |||||||
| Age | <0.001a | 0.013a | |||||
| 18: reference | 1 | 1 | |||||
| 19 | 1.06 | (0.74–1.50) | 0.97 | (0.67–1.38) | |||
| 20 | 1.52 | (1.05–2.18) | 1.24 | (0.84–1.82) | |||
| 21 | 2.01 | (1.31–3.08) | 1.62 | (1.03–2.53) | |||
| >21 | 2.39 | (1.53–3.72) | 1.72 | (1.07–2.76) | |||
| Language | German vs French | 0.71 | (0.57–0.90) | 0.004 | 0.87 | (0.68–1.12) | 0.293 |
| Married | yes vs no | 0.98 | (0.59–1.65) | 0.943 | 0.80 | (0.47–1.36) | 0.404 |
| Parents' Education | <0.001a | <0.001a | |||||
| mandatory | 4.67 | (3.33–6.56) | 3.58 | (2.49–5.15) | |||
| vocational training | 1.24 | (0.94–1.64) | 1.13 | (0.84–1.51) | |||
| grammar school | 1.63 | (1.17–2.27) | 1.48 | (1.05–2.08) | |||
| tertiary: reference | 1 | 1 | |||||
| Family finance | <0.001a | <0.001a | |||||
| below average | 0.40 | (0.29–0.54) | 0.46 | (0.33–0.65) | |||
| average | 0.63 | (0.47–0.84) | 0.61 | (0.45–0.83) | |||
| above average: reference | 1 | 1 | |||||
| Notes: N= 5745 a: Wald-test: test of significance for categorical variables unadjusted: bivariate logistic regression analysis – adjusted: multivariate logistic regression analysis Parenting: sum of score from four questions (each 0–4), higher numbers meaning higher active parenting (monitoring, rule-setting, knowing the whereabouts) Reference: reference group for OR calculations with polytomous categorical or ordinal variables | |||||||
This study provides evidence that self-reported parental factors earlier in life are associated with self-reported alcohol use in approximately 20–year-old male Swiss adults.
Both volume drinking and dependence were considerably more prevalent in young men who reported a parental alcohol or drug problem. Earlier studies already suggested that parental problematic substance use is a risk factor for substance misuse in adolescents [38–40]. The present study showed that this association persisted into early adulthood. The primary socialisation theory might shed light on a possible mechanism: it posits that the offspring might have been influenced through parental transmission of norms concerning substance use and familial availability of alcohol and tobacco [41]. Considering primary socialisation theory, parental substance use is an important factor for alcohol prevention in adolescents and young adults.
Active parenting was the most consistent parameter associated with significant lower at-risk alcohol consumption, in both RSOD and volume drinking. Active parenting was also associated with reduced alcohol dependence. This association persisted after controlling for the other parental factors and underlines active parenting as a protective factor. These results were consistent with other studies which emphasise parenting as a key variable in explaining the aetiology of alcohol-related problems [21, 42–44]. Research on familial or parental influences focused mainly on youth alcohol consumption [4, 13–15, 45–49]. The present findings added evidence to other studies that active parenting continued to be important and had an effect until early adulthood [9, 20, 21]. Parents are important as the primary socialisation agency to transmit prosocial norms [41]. However, parenting styles and approaches to adolescent alcohol consumption are variable [50]. To prevent problematic alcohol consumption in adolescents and young adults, it is reasonable to inform parents about the protective effect of active parenting and the negative influence of parental problematic substance use.
Present findings showed that growing up in a single parent family was not a risk factor for alcohol consumption. This correlation disappeared after correcting for the influence of parenting and parental problematic substance use. This finding is in line with previous studies, in which the influences of family structure and family composition were debated. Most studies showed that living in a single parent family was a strong exposure variable for young substance use disorders of adolescents [4, 14, 16, 40, 47, 48]. However, other studies found an unclear influence after correction for other family-variables or gender-specific differences [51–54]. This study did not differentiate between mother- or father-headed one-parent families.
In the sample of young Swiss men at the age of 20 years, alcohol use and problematic alcohol use with RSOD and volume drinking up to dependence was common. These findings corresponded well with other studies based on data of Swiss conscripts [5, 55].
The present study has several strengths and limitations. A main strength of our study is that it is based on a large sample of about 20–year-old Swiss men. Due to the detailed items of the questionnaire, the association between parental factors and alcohol use patterns could be studied. A further strength is that the present study analysed very common exposures and outcomes. The examined parental factors and alcohol use measures have an influence on the individual, familial and societal level. Therefore, the results might be of use in future prevention programmes, public health strategies and research. The present study should be interpreted with some caution and has several considerable limitations. The results are based on a retrospective observational cross-sectional analysis of baseline data of the C-SURF-study. Analysis of cross-sectional data does not provide sufficient information to determine the direction of causality. Longitudinal research is necessary to evaluate potential causal relationships. In the future, prospective data of the C-SURF-study will provide more information. This study only examined young Swiss males of a certain age group. Therefore, generalisations of the results to females or to all Swiss males should not be made. Next, the results rely on self-assessed measures based on a questionnaire. Concerns regarding validity and reliability of self-report measures of alcohol consumption are justified and have been addressed in research [56–59]. To ensure a good measurement precision, these recommendations were included in the design of the C-SURF questionnaire. Furthermore, recent research of US college students from the same age group showed that self-reported data on parenting and alcohol consumption was reliable [20]. Another limitation is that parental parameters were assessed retrospectively, which makes a potential recall bias possible. With a response rate of 79.2% among the consenters, a non-response bias is possible, although strong efforts were made to maximise the response rate and to minimise potential false reports. Studer et al. examined a non-response bias in the same cohort [28]. They showed that non-responders did differ from late respondents: they were more abstentious, but there was no difference concerning volume drinking and RSOD. Taking these results into account, a correction of a non-response bias would probably lead to a higher magnitude of effect and strengthen our findings. As mentioned in the introduction, parenting is not defined in a uniform way in existing literature. This makes comparisons with other studies difficult. The present study did not specify up to which degree more active parenting was protective against at-risk alcohol consumption. Visser et al. found a significant association between overprotection and alcohol use [60].
Future research should include longitudinal data to explore an ongoing effect between parental factors and alcohol consumption and how parental influence and alcohol use patterns change over time. Also, we suggest analysing the association between parental factors and other substance use, such as tobacco, cannabis and other drugs. Furthermore, future research should address the implementation of parental information into practice, such as dissemination of parenting guidelines and the adoption of recommendations into daily life.
The present study adds evidence that earlier parental influences seem to have an ongoing impact on alcohol use patterns in young adult men, while most previous research documented the importance of parental influences on adolescent or college student drinking. In this observational cohort sample of young Swiss conscripts active parenting was a consistent protective measure associated with lower risk of RSOD, volume drinking and alcohol dependence. A parental problematic substance use was positively associated with volume drinking and alcohol dependence in the offspring. A single parent family was not a risk factor for alcohol use in young adult men in this Swiss sample. Alcohol prevention strategies should therefore stress the importance of active parenting and the consumption of alcohol and drugs by the parents.
1 Hibell B, Guttormsson U, Ahlström S, Balakireva O, Bjarnason T, Kokkevi A, et al. The 2007 ESPAD Report: Substance Use Among Students in 35 European Countries. The Swedish Council for Information on Alcohol and Other Drugs (editor). Sweden, Stockholm, 2009.
2 Zaborskis A, Sumskas L, Maser M, Pudule I. Trends in drinking habits among adolescents in the Baltic countries over the period of transition: HBSC survey results, 1993–2002. BMC Public Health. 2006;6:67.
3 Wicki M, Kuntsche E, Gmel G. Drinking at European universities? A review of students’ alcohol use. Addict Behav. 2010;35:913–24.
4 Tomcikova Z, Geckova AM, van Dijk JP, Reijneveld SA. Characteristics of adolescent excessive drinkers compared with consumers and abstainers. Drug Alcohol Rev. 2011;30:157–65.
5 Adam A, Faouzi M, Gaume J, Gmel G, Daeppen JB, Bertholet N. Age of first alcohol intoxication: Association with risky drinking and other substance use at the age of 20. Swiss Med Wkly. 2011;141:w13226.
6 Kuendig H. Alcohol dependence figures in the Swiss general population: a Sisyphean challenge for epidemiologists. Eur Addict Res. 2010;16:185–92.
7 Marmet S, et al. Alcohol-attributable mortality in Switzerland between 1997 and 2011. Addiction Suisse, Lausanne, 2013.
8 World Health Organization. WHO global status report on alcohol 2004. Geneva, Switzerland: Department of Mental Health and Substance Abuse, 2004.
9 Surkan PJ, Fielding-Miller R, Melchior M. Parental relationship satisfaction in French young adults associated with alcohol abuse and dependence. Addict Behav. 2012;37:313–7.
10 Kirby T, Barry AE. Alcohol as a gateway drug: a study of US 12th graders. J Sch Health. 2012;82:371–9.
11 Jeanrenaud C, Widmer G, Pellegrini S. Le coût social de la consommation de drogues illégales en Suisse. Université de Neuchâtel. Abschlussbericht Sucht Info Schweiz, 2005.
12 Kuntsche E, Gmel G. Alcohol consumption in late adolescence and early adulthood – where is the problem? Swiss Med Wkly. 2013;143:w13826.
13 Gossrau-Breen D, Kuntsche E, Gmel G. My older sibling was drunk – Younger siblings’ drunkenness in relation to parental monitoring and the parent-adolescent relationship. J Adolesc. 2010;33:643–52.
14 Kuntsche E, Kuendig H. What is worse? A hierarchy of family-related risk factors predicting alcohol use in adolescence. Subst Use Misuse. 2006;41:71–86.
15 Vakalahi HF. Adolescent substance use and family-based risk and protective factors: a literature review. J Drug Educ. 2001;31(1):29–46.
16 Foxcroft DR, Lowe G. Adolescent drinking behavior and family socialization factors: a meta-analysis. J Adolesc. 1991;14(3):255–73.
17 Varvil-Weld L, Mallett KA, Turrisi R, Abar CC. Using parental profiles to predict membership in a subset of college students experiencing excessive alcohol consequences: findings from a longitudinal study. J Stud Alcohol Drugs. 2012;73(3):434–43.
18 Petrie J, Bunn F, Byrne G. Parenting programmes for preventing tobacco, alcohol or drugs misuse in children <18: a systematic review. Health Education Research. 2007;22(2):177–91.
19 Weinberg NZ, Rahdert E, Colliver JD, Glantz MD. Adolescent substance abuse: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1998;37(3):252–61.
20 Varvil-Weld L, Turrisi R, Scaglione N, Mallett KA, Ray AE. Parents’ and students’ reports of parenting: which are more reliably associated with college student drinking? Addict Behav. 2013;38(3):1699–703.
21 Patock-Peckham JA, King KM, Morgan-Lopez AA, Ulloa EC, Moses JM. Gender-specific mediational links between parenting styles, parental monitoring, impulsiveness, drinking control, and alcohol-related problems. J Stud Alcohol Drugs. 2011;72(2):247–58.
22 Dey M, Gmel G, Studer J, Dermota P, Mohler-Kuo M. Beverage preferences and associated drinking patterns, consequences and other substance use behaviours. European Journal of Public Health. 2013 Aug 12. [Epub ahead of print].
23 Dermota P, Wang J, Dey M, Gmel G, Studer J, Mohler-Kuo M. Health literacy and substance use in young Swiss men. Int J Public Health. 2013;58(6):939–48.
24 Sessa FM. The influence of perceived parenting on substance use during the transition to college: A comparison of male residential and commuter students. J Coll Stud Dev. 2005;46(1),62–74.
25 Patock-Peckham JA, Morgan-Lopez AA. College drinking behaviors: Mediational links between parenting styles, impulse control, and alcohol-related outcomes. Psychol Addict Behav. 2006;20(2):117.
26 Arria AM, Caldeira KM, O’Grady KE, Vincent KB, Fitzelle DB, Johnson EP, Wish ED. Drug exposure opportunities and use patterns among college students: Results of a longitudinal prospective cohort study. Substance Abuse. 2008;29(4):19–38.
27 Studer J, Mohler Kuo M, Dermota P, Gaume J, Bertholet N, Eidenbenz C, Daeppen J-B, Gmel G. Need for informed consent in substance use studies – harm of bias? J Stud Alcohol Drugs. 2013;74:931–40.
28 Studer J, Baggio S, Mohler-Kuo M, Dermota P, Gaume J, Bertholet N, Daeppen J-B, Gmel G. Examining non-response bias in substance use research. Are late respondents proxies for non-respondents? Drug Alcohol Depend. 2013;132:316–23.
29 Wechsler H, Isaac NE. ‘Binge’ drinkers at Massachusetts colleges. Prevalence, drinking style, time trends, and associated problems. JAMA. 1992;267:2929–31.
30 Wechsler H, Davenport A, Dowdall GW, Moeykens B, Castillio S. Health and behavioural consequences of binge drinking in college—a national survey of students at 140 campuses. JAMA. 1994; 272:1671–7.
31 Dawson DA. Defining Risk Drinking. Alcohol Research & Health (Journal of the National Institute on Alcohol Abuse and Alcoholism). 2011;34(2):144–56.
32 Department of Health. The cost of alcohol harm to the NHS in England: An update to the Cabinet Office (2003) study. London: Department of Health, 2008.
33 Samet S, Waxman R, Hatzenbuehler M, Hasin DS. Assessing addiction: concepts and instruments. Addict Sci Clin Pract. 2007;4(1):19–31.
34 Knight JR, Wechsler H, Kuo M, Seibring M, Weitzman ER, Schuckit MA. Alcohol abuse and dependence among U.S. college students. J Stud Alcohol. 2002;63(3):263–70.
35 Hibell B, Guttormsson U, Ahlström S, Balakireva O, Bjarnason T, Kokkevi A, Kraus L. The 2011 ESPAD report. Substance use among students in 36 European counties. The Swedish Council for Information on Alcohol and Other Drugs. Stockholm, Sweden, 2012.
36 Gmel G. Mohler-Kuo M, Dermota P, Gaume J, Bertholet N, Daeppen JB, Studer J. Religion is good, belief is better: Religion, religiosity, and substance use among young Swiss men. Subst Use Misuse: 2013;48:1085–98.
37 Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression. Correlation analysis for the behavioural sciences. (3rd edition). New York: Routledge; 2003.
38 Moore GF, Rothwell H, Segrott J. An exploratory study of the relationship between parental attitudes and behaviour and young people’s consumption of alcohol. Subst Abuse Treat Prev Policy. 2010;5:6.
39 Donovan JE, Molina BS. Childhood risk factors for early-onset drinking. J Stud Alcohol Drugs. 2011;72(5):741–51.
40 Hill SY, Steinhauer SR, Locke-Wellman J, Ulrich R. Childhood risk factors for young adult substance dependence outcome in offspring from multiplex alcohol dependence families: a prospective study. Biological Psychiatry. 2009;66(8):750–7.
41 Oetting ER, Donnermeyer JF. Primary Socialization Theory: The Etiology of Drug Use and Deviance. I. Subst Use Misuse. 1998;33(4):995–1026.
42 Arria AM, Kuhn V, Caldeira KM, O’Grady KE, Vincent KB, Wish ED. High school drinking mediates the relationship between parental monitoring and college drinking: a longitudinal analysis. Subst Abuse Treat Prev Policy. 2008;3:6.
43 Beck KH, Boyle JR, Boekeloo BO. Parental monitoring and adolescent drinking: results of a 12–month follow-up. Am J Health Behav. 2004;28(3):272–9.
44 Walls TA, Fairlie AM, Wood MD. Parents do matter: a longitudinal two-part mixed model of early college alcohol participation and intensity. J Stud Alcohol Drugs. 2009;70(6):908–18.
45 Chaplin TM, Sinha R, Simmons JA, Healy SM, Mayes LC, Hommer RE, Crowley MJ. Parent-adolescent conflict interactions and adolescent alcohol use. Addict Behav. 2012;37:605–12.
46 Bachman JG. O’Malley PM, Johnston LD, Schulenberg JE, Wallace JM. Racial/ethnic differences in the relationship between parental education and substance use among U.S. 8th-, 10th-, and 12th-Grade Students: Findings from the Monitoring the Future Project. J Stud Alcohol Drugs. 2011;72:279–85.
47 Carvalho Malta D, Lopes Porto D, Carvalho Malta Melo F, Monteiro RA, Monteiro Vasconcelos Dardinha L, Horta Lessa B. Family and the protection from use of tobacco, alcohol, and drugs in adolescents, National School. Rev Bras Epidemiol. 2011;14(3):166–77.
48 Ledoux S, Miller P, Choquet M, Plant MA. Family structure, parent-child relationships, and alcohol and other drug use among teenagers in France and the United Kingdom. Alcohol Alcohol. 2002;37(1):52–60.
49 Morleo M, Cook PA, Elliott G, Phillips-Howard PA. Parental knowledge of alcohol consumption: a cross sectional survey of 11–-17 year old schoolchildren and their parents. BMC Public Health. 2013;13(1):412.
50 Gilligan C, Kypri K. Parent attitudes, family dynamics and adolescent drinking: qualitative study of the Australian Parenting Guidelines for Adolescent Alcohol Use. BMC Public Health. 2012;12:491.
51 Barnes GM, Windle M. Family factors in adolescent alcohol and drug abuse. Pediatrician. 1987;14(1–2):13–8.
52 Alamian A, Paradis G. Individual and social determinants of multiple chronic disease behavioral risk factors among youth. BMC Public Health. 2012;12:224.
53 Musick K, Meier A. Are both parents always better than one? Parental conflict and young adult well-being. Social Science Research. 2010;39(5):814–30.
54 Jablonska B, Lindberg L. Risk behaviours, victimisation and mental distress among adolescents in different family structures. Soc Psychiatry Psychiatr Epidemiol. 2007;42(8):656–63.
55 Gmel G, Gaume J, Bertholet N, Daeppen J. Brief alcohol intervention as pragmatic intervention: Who is voluntarily taking an offered intervention? Alcohol. 2012;46(6):551–8.
56 Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. Addiction. 2000;95:S347–S360.
57 Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;Suppl. 2:1–12.
58 Gmel G, Rehm J. Measuring alcohol consumption. Contemp Drug Probl. 2004;31:467–540.
59 Greenfield TK, Kerr WC. Alcohol measurement methodology in epidemiology: recent advances and opportunities. Addiction. 2008;103(7):1082–99.
60 Visser L, de Winter AF, Vollebergh WAM, Verhulst C, Reijneveld SA. The Impact of Parenting Styles on Adolescent Alcohol Use: The TRAILS Study. Eur Addict Res. 2013;19:165–72.
Funding / potential competing interests: This study used data from the Cohort Study on Substance Use Risk Factors (C-SURF). The present study was supported by the Swiss National Research Foundation (FN 33CS30_139467). There were no competing interests.
Authors’ contribution:SS led the analysis and interpretation and produced the first and final draft of the paper. DS contributed to the analysis and interpretation. GG contributed to study design, questionnaire design, interpretation and refining the paper