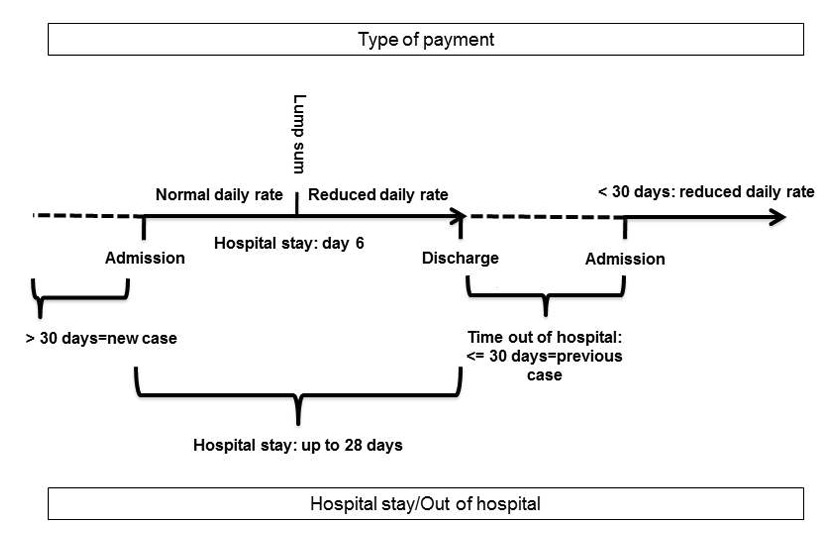
Figure 1
New Remuneration System (NRS): Illustration by several inpatient episodes.
DOI: https://doi.org/10.4414/smw.2014.13991
Due to the cuts in government budgets in recent years, many OECD countries spent less money on health between 2009 and 2011 compared to the years before the economic crisis [1]. However, the percentage of gross domestic product (GDP) spent on healthcare is a marker of a country’s commitment to the promotion of health and health-related quality of life [2]. Accordingly, improving health care systems with respect to productivity, efficiency and affordability [1] whilst safeguarding quality of care [3] is a major challenge for the future.
Switzerland belongs to the countries with high expenditures for health [4] and with high inpatient capacities [5]. Regarding psychiatry, the costs for treatment in psychiatric hospitals were about 2 billion Swiss francs in 2010, which is 10% of all hospital costs [6]. Further, the average length of stay for patients with a mental disorder remained at 30 days in 2010 and is high in international comparison [7]. In contrast, the number of psychiatric admissions increased over time, with a rise in readmissions of more than 30% between 2000 and 2006 [8]. In the future, a clear reduction in psychiatric inpatient stays is expected and needed due to factors such as economy and the increasing use of outpatient and complementary services [9]. Accordingly, clinical evidence supports a balance between community and hospital mental health services [10].
Worldwide, new financial incentives are being implemented or under discussion to control inpatient service consumption by financial incentives and restrictions. In western Europe, case-based payment systems, usually Diagnosis Related Groups (DRGs), are on the rise for mental health-related services [11]. DRGs are economically homogenous patient groups and consist of a fixed payment for each treatment episode. They are widely implemented for physical health problems with the aim to control the resource use by standardising treatment, usually according to diagnosis and procedures. Such case-based systems provide a strong incentive to shorten length of stay because each additional treatment day is less profitable for the hospital [12]. In previous studies, psychiatric DRGs implemented in general DRG systems did not explain a sufficient amount of the variation in the length of stay (LOS) [13–15]. Even if there was evidence for a reduction in the length of stay by case-based financing [12, 16–18], a risk of premature discharge and of a higher level of readmission or patient transfers persisted [19, 20]. Further, due to high variation within diagnostic groups, appropriate LOS cannot be predicted. Accordingly, European studies on DRG-like systems in psychiatry report an underfunding of mental health [21, 22] and the need to make revisions in terms of cost adjustments linked to the length of stay to cover costs or even generate a surplus [23].
A prospective ‘per diem’ system has some advantages over a ‘per case’ system. For the former, the price is set for each inpatient day with or without limits on the number of reimbursable days [12]. A per diem system with limits means a mixture of a per case and per diem system. The case-based component with strong incentives to control the costs of care is mitigated under lower-powered payment systems with additional payments for providing more services [20]. Generally, in a per diem system, the risk of premature discharges would seem to be weaker. Further, the latter system better considers the heterogeneity of psychiatric patients with respect to LOS and the course of costs during treatment [20, 24]. Usually, the required amount of care is more intense within the initial period of hospital stay, which is generally when an acute crisis and/or diagnoses take place. Here, it is necessary to clinically assess the patient and to establish an individual treatment plan. Within the course of hospital stay, the mental state of the patient should improve, accompanied by decreasing needs for clinical assessment, treatment and nursing. Like DRGs, per diem costs are difficult to predict using characteristics like diagnosis or LOS. Some, but not all, previous findings have shown reductions in the LOS related to prospective per diem systems with limits [12, 25]. In the US, a per diem system (Prospective Remuneration system for Inpatient Psychiatric Facilities (IPF PPS)) is being used based on degressive rates [26, 27]. In this system, case linking for readmissions within three days is used to prevent premature discharge. Another example is the German prospective per diem system “Pauschalierendes Entgeltsystem für Psychiatrie und Psychosomatik, PEPP” introduced in 2013, based on clinical and treatment components [28].
In Switzerland, psychiatric hospitals are usually financed by a per diem system with fixed daily rates. This implies a greater financial benefit with longer hospital stays for the providers. Unlike somatic medicine, psychiatry is still exempt from DRGs. However, according to a new law introduced in 2011, Swiss psychiatric hospitals need to implement a unique, sustainable and competitive payment structure within the next few years. Implementation of a remuneration system combining a case-based and a per diem system is planned, taking the advantages of the two systems into account: substantial incentives to reduce the length of stay by a lump sum, less money over time through degressive daily rates, and quality aspects in terms of less money for cases with early readmissions. The new remuneration system (NRS) was introduced in 2009, only in the University Hospital of Psychiatry of the Canton of Zurich, which served as the NRS-hospital in this study. The aim of this study was a preliminary evaluation of the first NRS in terms of an intended reduction in LOS and a prevention of early readmission. We considered specific outcome categories corresponding to the design of the NRS. We assumed a decrease in the LOS for the time period when the hospital earned less money (here: >28 days). Further, the NRS might lead to a shorter LOS in terms of a higher proportion of discharges within 28 days. Finally, we focused on early readmissions within 30 days assuming they would decrease due to financial disadvantages for the hospital. We compared the time period before and after the introduction of the NRS, and also compared data from the NRS-hospital with the data of other cantonal hospitals, using an observation period of seven years.
The catchment area comprised regions within the Canton of Zurich, with a population of approximately 1,350,000 inhabitants.
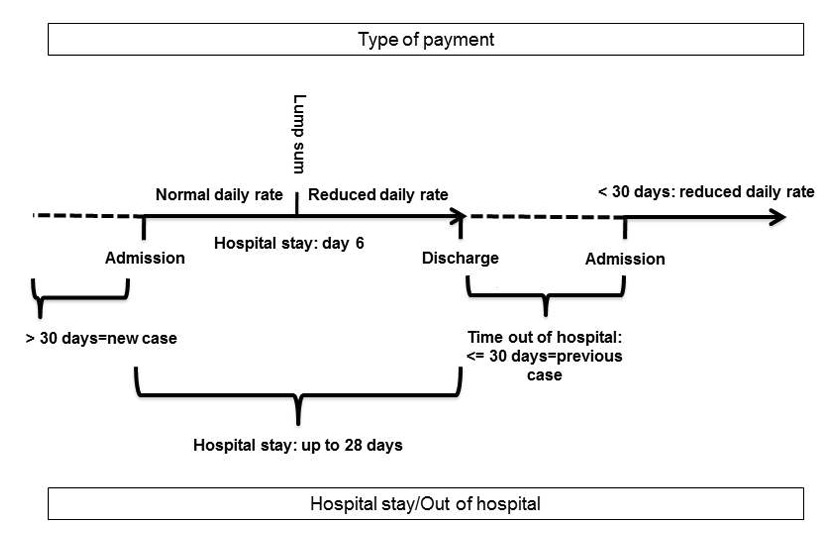
Figure 1
New Remuneration System (NRS): Illustration by several inpatient episodes.
In total, data covered information from four psychiatric hospitals fully or partly subsidised by the canton: the NRS-hospital and three comparison hospitals. Two other hospitals were excluded: one dedicated to a specific patient group, and another that is completely private without any state subsidies. The NRS-hospital is one of six psychiatric institutions serving a defined catchment area in the canton. It treats the whole spectrum of mental health problems and covers about one third of the treatment episodes of all these hospitals.
We used patient data from the Canton of Zurich, collecting information on socio-demographic variables, diagnosis according to the International Classification of Diseases (ICD-10) and treatment at hospital admission and / or discharge [29]. The collection of inpatient data in psychiatric hospitals was approved by federal law. The responsible regional legal authority, the Department of Health of the Canton of Zurich, provided the permissions to work with those data and to publish the data. The federal legal authority for collecting the respective patient data in all cantons is the Federal Statistical Office (FSO).
The patient data included in our study were anonymised, thus individual hospitals are not identifiable. The ethical basis for the investigation, following the declaration of Helsinki, was provided by general permission of the legal authorities.
The new remuneration system (NRS) is illustrated in figure 1. It takes decreasing treatment needs over time in a psychiatric hospital and disadvantaging early readmissions into account. The intention is a reduction of the LOS and, at the same, a prevention of readmissions considered to be too early. The system consists of variable daily rates corresponding to the different courses of treatment combined with a fixed lump sum delivered on day 6 of the hospital stay. In detail, a higher daily rate is provided within the first five days. The lump sum paid on day 6 represents approximately eight times the amount of the initial daily rate. From day 6 on, a reduced daily payment is provided. The calculation of this per diem and per case payment is designed in such a way that hospital stays of exactly 28 days are as profitable as before the introduction of the new remuneration system. Accordingly, hospital stays of less than 28 days are more profitable for the hospital than under the old system, especially shortly after day 6. From day 29 on, they are less profitable. Thus, the hospital has relatively more resources with which to treat the patient more efficiently during the initial 28 days (e.g., by additional treatments or an increase in hospital staff).
Discharges with readmissions within 30 days were considered to be too early or to belong to the same disease episode and therefore to be avoided. Accordingly, patients who were readmitted within 30 days were administratively and financially linked with their previous case. The lump sum is delivered only once within one such linked treatment period. Further, this implies financing with a continuation of the reduced daily rate if the cumulative length of stay is at least 6 days. The latter is intended to be an incentive to prevent early readmissions (e.g., by optimising health care during previous admissions as well as aftercare planning) and may therefore ensure service quality.
We were interested in specific categories of LOS and proportions of early readmissions according to the design of the NRS. For our final analyses, we considered two samples. Concerning the analyses of the LOS-categories, we finally included N = 66,626 inpatient episodes of patients discharged between the years 2005 and 2011, irrespective of the year of admission. There were N = 21,166 (31.8%) discharges from the NRS-hospital and N = 45,460 (68.2%) discharges from the other psychiatric hospitals of the canton. The patients were 18 years of age or older. We considered all mental disorders according to ICD-10 (F0–F9) because we were interested in all acute inpatient episodes financed by the new system. Further, we included all departments of the NRS-hospital eligible for the new remuneration system. Accordingly, we excluded admissions to the Crisis Intervention Centre of the NRS-hospital with obligatory hospital stay of up to a maximum of five days. We connected inpatient stays with discharge and admission on the same day within the same hospital.
Regarding readmissions, we only considered a subsample (N = 60,847) of patients admitted and discharged within the same year (e.g., admission and discharge in 2005).
In detail, we constructed four meaningful categories of LOS and readmissions for the final statistical analyses: Length of stay between 1–5, 6–10 (the lump sum was delivered on day 6), 11 to 28 (the lump sum was arranged to compensate for lower daily rates from day 6 on up to day 28) and more than 28 days. For our focus on “early readmission”, we constructed the category readmission within 30 days of previous discharge. Further, we considered the variable hospital type (NRS-hospital vs comparison hospitals) and calendar year.
First, we compared sample characteristics by the Chi-Square test and by the Mann-Whitney-U-test.
Second, we conducted general logistic models. The aim was to examine the extent of change of the dependent variables by hospital type and time. Time was the calendar year for (linear) historical time trends. As we were particularly interested in change since the year 2009 in the NRS-hospital (the introduction of the new remuneration system), we considered the main effect “NRS system, since 2009 = yes vs no” as well as a linear time trend between 2005 and 2011, irrespective of the hospital type. Further, the variable NRS-hospital (yes vs no) was used as explanatory variable. According to our outcome variables of interest, we computed five general logistic models.
Therefore, we prepared the dataset for each outcome according to the principle of “cases” (c) and “total numbers” (n) per year and hospital type. Total number equals the number of patients in a given year and hospital type. Cases represent the corresponding number of patients in a given LOS-category or early readmission-category. For example, in the NRS-hospital N = 2,498 patients were discharged in 2005, of which N = 340 were readmitted within 30 days. Thus, the observed proportion of early readmission was 13.6%.
The statistical analyses were conducted by SAS V 8.2 with the procedure “proc genmod” with probability distribution as binomial and link function as logit.
Table 1 summarises the characteristics of the patients with inpatient episodes in the NRS-hospital and in the comparison hospitals of the canton between the years 2005 and 2011. In the NRS-hospital there were more males, non-Swiss patients and compulsorily admitted ones. Further, the patients in that hospital were less frequently married, employed, living in their own home or self-admitted, more frequently had a public compared to a private health insurance and less frequently had an emergency admission. Patients also differed with respect to diagnosis, but the differences in diagnostic groups remained quite stable over time within hospital type. For example, in the NRS hospital, the most frequent diagnosis of psychotic disorders (F2) changed from 27.4% to 27.8%. In the comparison hospitals, the most prevalent diagnosis of affective disorders (F3) changed from 25.0% to 29.9%. Additional analyses showed that in the years 2005 to 2008 the median LOS of the NSR hospital was higher than in the comparison hospitals. In the years 2009 to 2011 hospitals did not differ with respect to the median LOS of 21 days. There was no difference with respect to the number of readmissions within 30 days over time between hospital type. Some of the previous findings might be due to the relatively more urban character of the NRS-hospital and the more mixed rural/urban character of the other hospitals as well as by differences in specialised units and private patients between hospital types.
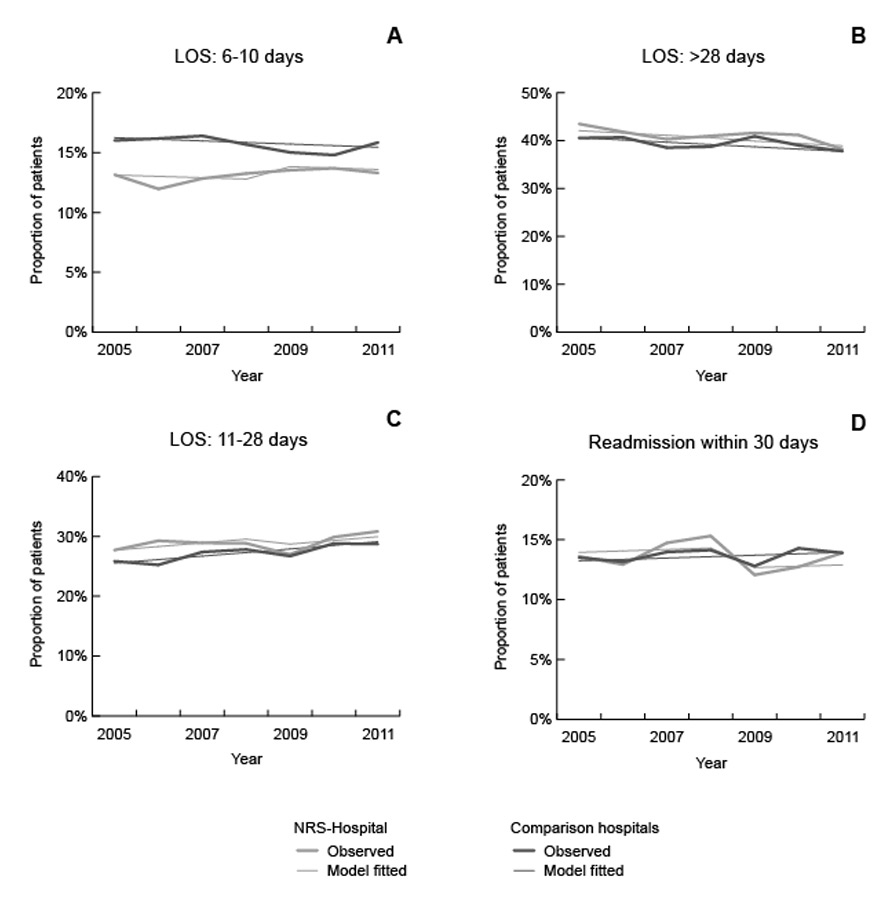
Figure 2
Length of stay-category 6–10 days (A), >28 days (B), 11–28 days (C) and readmission within 30 days (D): raw values and estimated values by the General Linear Model.
The descriptive results for some of the outcome categories are illustrated in four graphs in figure 2. With respect to a LOS between 6 and 10 days, the proportion seemed to be quite stable between 2005 and 2011 in the NRS-hospital (13.1% to 13.3%) and in the comparison hospitals (16.0% to 15.8%; see graph A in fig. 2). However, the difference between the two hospital types diminishes over time. Regarding length of stay over 28 days (see graph B in fig. 2), there was a decrease since the year 2005 in the NRS-hospital (by 5.8% from 43.5% to 38.2%) and also in the comparison hospitals (by 2.7% from 40.5% to 37.8%). In contrast, the proportion of patients with a LOS between 11 and 28 days increased since the year 2005 in the NRS-hospital (by 3.5% from 27.7% to 30.8%) and in the comparison hospitals (by 2.9% from 25.8% to 28.7%; see graph C in fig. 2). Finally, there was little or no change over time in the LOS-category 1–5 days in the NRS-hospital (15.7% to 17.7%) or in the comparison hospitals (17.6% to 17.6%).
With respect to readmissions, we were especially interested in the category readmission within 30 days (see graph D in fig. 2). The descriptive findings showed that there appeared to be no overall change over the time period between 2005 and 2011 in the NRS-hospital (13.6% to 13.9%) and in the comparison hospitals (13.5% to 13.9%). However, the proportion decreased from 2008 (15.3%) to 2009 (12.1%) and to 2010 (12.7%) in the NRS-hospital and increased thereafter, again reaching the initial level in 2011.
The general logistic models are presented in table 2.
We were especially interested in the development of the proportion of LOS and early readmissions since 2009 in the NRS-hospital (referring to the main effect “since 2009, NRS system”), the time when the lump sum was implemented.
In model 2, the data revealed that the proportion of hospital stays between 6 and 10 days increased only in the NRS-hospital since 2009 but did not reach the level of the comparison hospital (see graph A in fig. 2). In terms of odds ratios (OR), in 2005 the NRS-hospital had an OR = 0.78 (95% CI = 0.73–0.83), and thus was 22% lower than in the comparison hospitals. The odds ratio since 2009 in the NRS-hospital was OR = 1.11 (95% CI = 1.01–1.21), meaning an increase of only 11%.
In model 5, the proportion of early readmissions decreased by 14% since 2009 in the NRS-hospital (OR = 0.86; 95% CI = 0.78–0.95). Because in 2005 the proportion of early readmission was not significantly higher than in the comparison hospitals, the significant change since 2009 in the NRS-hospital did not lead to a substantially different readmission rate than in the comparison hospitals (see graph D in fig. 2).
Further, models 3 and 4 show that the proportion of hospital stays of over 28 days and between 11 and 28 days was higher in the NRS-hospital than in the comparison hospitals between the years 2005 and 2011 (see graphs D and C). However, the proportion of these LOS-categories changed between 2005 and 2011 in the NRS-hospital as well as in the comparison hospitals. We found a small annual reduction in proportion in the over 28 day LOS-category (OR = 0.98; 95% CI = 0.97–0.99) and a slight increase of proportion in the 11 to 28 day LOS-category (OR = 1.03; 95% CI = 1.02–1.04). There was no change in those LOS-category proportions since 2009.
| Table 1:Characteristics of patients of the NRS-hospital vs comparison hospitals, 2005–2011. | |||||
| Characteristics | NRS-hospital N = 21166 | Comparison hospitals N = 45460 | Total N = 66626 | χ2 | p |
| Sociodemography | N (%) | N (%) | N (%) | ||
| Age (median, IQR) ‡ | 43 (55–32) | 43 (56–31) | 43 (56–32) | –2.22 | 0.026 |
| Sex, male | 11,094 (52.4) | 21,326 (46.9) | 32,420 (48.7) | 175.04 | <0.001 |
| Marital status, married | 5,392 (26.7) | 13,831 (32.3) | 19,223 (30.5) | 205.86 | <0.001 |
| Employment status, employed | 4,555 (22.7) | 12,609 (27.8) | 17,164 (26.2) | 193.19 | <0.001 |
| Living situation, own home | 13,257 (71.7) | 32,173 (74.9) | 45,430 (73.9) | 70.67 | <0.001 |
| Nationality, Swiss | 15,631 (74.9) | 37,900 (85.8) | 53,531 (82.3) | 1,146.35 | <0.001 |
| Clinical variables | |||||
| Psychiatric diagnosis at discharge | 1,021.71 | <0.001 | |||
| Organic disorder (F0) | 1,654 (7.8) | 3,898 (8.6) | 5,552 (8.3) | ||
| Substance disorder (F1) | 4,672 (22.1) | 9,734 (21.4) | 14,406 (21.6) | ||
| Psychotic disorder (F2) | 5,832 (27.6) | 8,424 (18.5) | 14,256 (21.4) | ||
| Affective disorder (F3) | 4,627 (21.9) | 12,358 (27.2) | 16,985 (25.5) | ||
| Neurotic disorder, (F4) | 2,121 (10.0) | 6,342 (14.0) | ,8463 (12.7) | ||
| Behavioral disorder (F5) | 69 (0.3) | 371 (0.8) | 440 (0.7) | ||
| Personality disorder (F6) | 1,583 (7.5) | 3,493 (7.7) | 5,076 (7.6) | ||
| Mental retardation (F7), Developmental disorder (F8), behavioural and emotional disorders (F9) | 608 (2.9) | 840 (1.8) | 1,448 (2.2) | ||
| Severity of illness at admission (median, IQR) | 4 (4–3) | 4 (4–3) | 4 (4–3) | –0.63 | 0.533 |
| Hospitalisation-specific variables | |||||
| Type of referral, self | 4,602 (23.6) | 13,024 (29.5) | 17,626 (27.7) | 237.42 | <0.001 |
| Insurance type, public | 19,778 (93.5) | 40,127 (89.5) | 59,905 (90.7) | 273.61 | <0.001 |
| Compulsory admission | 7,212 (34.1) | 11,332 (25.1) | 18,544 (28.0) | 577.23 | <0.001 |
| Emergency admission | 8,912 (43.3) | 19,859 (47.4) | 28,771 (46.0) | 90.55 | <0.001 |
| Median LOS, 2005–2008 ‡ | 22 (46–8) | 19 (48–7) | 20 (47–8) | –3.102 | 0.002 |
| Median LOS, 2009–2011 ‡ | 21 (43–8) | 21 (44–8) | 21 (44–8) | –1.795 | 0.073 |
| Readmissions ≤30 day, 2005–2008 | 1,470 (14.2) | 3,119 (13.7) | 4,589 (13.9) | 1.17 | 0.281 |
| Readmissions ≤30 day, 2009–2011 | 1,157 (13.0) | 2,570 (13.7) | 3,727 (13.4) | 2.60 | 0.107 |
| Abbreviations: IQR = interquartile range. Comparison of the NRS-hospital with the comparison hospitals. ‡ Comparison by the non-parametric Mann-Whitney-U-test. Not all variables sum up to N = 66,626 due to missing values as follows: 3,605 missing concerning marital status, 5,168 missing concerning living situation, 1,218 missing concerning employment status, 1,587 missing concerning nationality, 3,203 missing concerning severity of illness at admission, 2,966 missing concerning manner of referral, 314 missing concerning compulsory admission, 4,147 missing concerning emergency admission and 603 missing concerning insurance type. | |||||
| Table 2:Categories of length of stay (LOS) over time and hospital type: GLM. | ||||
| Category, LOS (N = 66,626) | Predictor variables | B (SE) | 95%CI | |
| Model 1 | 1–5 days | Intercept | –1.54 (0.02) **** | –1.58 – –1.50 |
| NRS-hospital | –0.05 (0.03) | –0.11 – 0.01 | ||
| Time since year 2005 | –0.01 (0.01) | –0.01– 0.01 | ||
| NRS system, since 2009 | 0.01 (0.04) | –0.08 – 0.09 | ||
| Model 2 | 6–10 days | Intercept | –1.64 (0.02) **** | –1.69 – –1.61 |
| NRS-hospital | –0.25 (0.03) **** | –0.32 – –0.19 | ||
| Time since year 2005 | –0.01 (0.01) | –0.02 – 0.01 | ||
| NRS system, since 2009 | 0.10 (0.05) * | 0.01 – 0.19 | ||
| Model 3 | 11–28 days | Intercept | –1.07 (0.02) **** | –1.11 – –1.03 |
| NRS-hospital | 0.11 (0.02) **** | 0.07 – 0.16 | ||
| Time since year 2005 | 0.03 (0.01) **** | 0.02 – 0.04 | ||
| NRS system, since 2009 | –0.07 (0.04) | –0.14 – 0.01 | ||
| Model 4 | >28 days | Intercept | –0.38 (0.02) **** | –0.41 – –0.34 |
| NRS-hospital | 0.06 (0.02) ** | 0.02 – 0.11 | ||
| Time since year 2005 | –0.02 (0.01) *** | –0.03 – –0.01 | ||
| NRS system, since 2009 | –0.01 (0.03) | –0.06 – 0.66 | ||
| Category,readmission (N = 60,847) | ||||
| Model 5 | ≤30 days | Intercept | –1.88 (0.03) **** | –1.93 – –1.83 |
| NRS-hospital | 0.06 (0.03) | –0.01 – 0.13 | ||
| Time since year 2005 | 0.01 (0.01) | –0.01 – 0.03 | ||
| NRS system, since 2009 | –0.15 (0.05) *** | –0.24 – –0.05 | ||
| * <0.05; ** <0.01; *** <0.001; ****<0.0001 NRS-hospital = hospital using the new remuneration system; reference category: comparison hospitals. | ||||
This study was conducted in the context of the discussion about appropriate and required incentives to reduce the length of stay in psychiatry. It evaluated the implementation of a new remuneration system in a Swiss psychiatric hospital, the first system of its kind in Swiss psychiatry. We assumed reductions in LOS, here used in terms of specific categories, and the prevention of early readmissions according to the design of the NRS-system.
Corresponding to our results, the NRS led to a higher proportion in of the LOS-category 6–10 days and a slightly lower proportion in the category of readmissions within 30 days. The increase in the LOS-category 6–10 days was not accompanied by a reduction in the LOS-category 1–5 days as the latter did not change significantly over time. Besides these results, we found an increase in the proportion of 11–28 day LOS-category in all hospitals, and a proportional reduction in the >28 days LOS-category since the year 2005. The large sample might have contributed to the statistical significance of the small effect sizes of the variable “NRS system, since 2009”. Thus, despite the observation period of three years, the stability of effects over time has to be proven to exclude an oversimplification of the statistical model. We did not find evidence for unpleasant outcomes like a higher proportion of early readmissions or a shift of hospital stays from between 1 and 5 days towards 6–10 days since 2009. Our results on readmissions do not support premature discharge in terms of a revolving door phenomenon. The time effects since the year 2005 argue for a shift from a long hospital stay towards an intermediate length stay. The reduction of the LOS of more than 28 days in both hospitals types might be associated with the previous degressive payment system implemented in 2006 for all hospitals providing a lower daily rate for stays of more than 60 days.
Preliminary analyses on the LOS of up to 365 days (N = 66,338) as a continuous variable showed no significant impact of the NRS and accordingly no changes since 2009 related to the NRS hospital (detailed results not shown). These findings do not contradict our results with little changes in specific LOS categories according to the design of the NRS. In sum, one can conclude that the NRS has so far obviously had no meaningful impact on the overall LOS.
Previous evidence on the relationship between LOS and payment systems is contradictory [12, 30], even if a comparison is difficult due to differences in design and treatment setting. It is known that the LOS varies considerably in psychiatric patients [13–15, 31, 32]. The reduction of long hospital stays corresponds to the European trend towards deinstitutionalisation with less inpatient treatment and improvement of community services [33]. Evidence on the relationship between payment and readmission risk is contradictory as well [18, 19, 30].
Even if not in the focus of this study, the lump sum might have an impact on outcomes other than LOS or readmissions. For example, the lump sum might potentially impact the number of admissions to the NRS hospital. We analysed this aspect by using Poisson regression and found that hospital admissions significantly increased since 2009 from 12.7% to 16.0% in the NRS-hospital (detailed results not shown). Accordingly, the lump sum obviously did not have any negative impact on the patient’s preference of being treated in the NRS hospital since its implementation. Due to the lack of a unique patient identification number, we could not reliably analyse if patients first treated in the NRS hospital had more readmissions in other hospitals since 2009. Further, we did not find evidence for an increase of the number of emergency admissions and lower or higher severity of illness both at admission or discharge since 2009 in the NRS hospital (detailed results not shown). As cost data were only available since 2008, we just focused on the LOS in this study. Available evidence does not support skimming (hospitals admit more of the more profitable and fewer of the less profitable cases) or dumping (hospitals discharge more of the less profitable cases to other hospitals over the same period of time) by psychiatric DRGs [34].
Increasing the impact of a lump sum might necessitate clinical management improvements. Incentives need to be aligned with optimisations in quality and organisational support (e.g., implementation of appropriate care processes and coordination of care across services, reduction of fragmentation of care, incorporation of performance and outcome measurements for improvement and accountability) [35]. The Canton of Zurich promotes and subsidises several structural changes towards outpatient and community care, integrated treatment, treatment continuity and accessability of services [36]. Accordingly, at least in the NRS-hospital new structures of integrated and community care were introduced in recent years along with new inpatient units. Hereby, however, the balance between inpatient and community care remained. Parallel to the implementation of the payment system, hospital staff was provided with structured monthly feedback on their performance with respect to economic data like average LOS, earnings and costs. Accordingly, the awareness of the importance of efficient treatment and of achieved treatment goals might continuously increase, keeping the priority of meeting patients’ needs in mind. This aspect refers to the need for concrete mandatory treatment goals. Such goals were not set explicitly so far, but they might better support the impact of a new remuneration system (e.g., reduction of the LOS by a specified amount). Further, one could consider how the earnings of the hospital could be reinvested in order to improve quality of care or to motivate the staff to work more efficiently.
As for structural aspects, improving the remuneration system itself might improve efficiency of care. Due to its preliminary development and due to the widely unknown indicators for homogenous cost groups in psychiatry, the Swiss system has not yet considered the case-mix. The consideration of the latter might allow to provide standards for resource allocation with respect to individual treatment needs. The Canton of Zurich intends to implement severity, psychiatric diagnosis and resource use to generate homogenous performance-based groups. As a measure of symptom and social handicap severity the canton uses the Health of the Nations Outcome Scales (HoNOS) [37], which is since 2012 continuously assessed. The question is whether payment depends on current changes in HoNOS ratings. However, its financial impact is not yet clear and needs to be evaluated. Correspondingly, in the UK the HoNOS is the most popular outcome measure in adult mental secondary health services [38]. The intention is to combine outcome measurement with a stricter finance-driven policy: Payment by Results (PbR). It is a case-mix-approach to health funding that consists of varying tariffs for defined groups of procedures or patients and depends on the recorded activity level. The more one does, the more one earns. It has been in operation in UK acute services for several years with the aim of being incorporated into mental health care.
A corresponding new approach is pay for performance (P4P). It is based on variable compensation depending on the quality of care. The quality goal of pay for performance may include benchmarks in health care structure, qualification level of therapists, processes of care, or medical outcomes [39]. The incentive of a pay for performance programme may either take the form of a financial bonus or a financial disadvantage, depending on whether quality thresholds are achieved or not, for instance the qualification level of the therapeutic team. The aims are long-term improvements in performance and structural changes as well as increasing efficiency and cost savings [39]. The effects of such programmes might be promising but their appropriateness in mental health care has not yet been systematically examined [40].
In summary, linking financing and service quality is essential. It also implies that the physician’s judgment on the patient’s clinical condition and need for treatment should have highest priority, even though it might be guided by corresponding financial incentives. Accordingly, a reduction in LOS without taking treatment quality into account is certainly not desirable and from an ethical perspective even unfeasible.
This is one of a few studies [21, 22, 30] delivering an insight into implemented new remuneration systems in psychiatry in a European country. The study could contribute to the understanding of aspects that have to be taken into account while implementing a new financing system. Limitations are related to the observation period which might be too short. Further, we only considered one specific hospital where the remuneration system was implemented. It would be interesting to compare outcomes of several hospitals and different hospital types (e.g., private vs public ones) using the respective remuneration system. Further research on HoNOS-data and resource use (e.g., LOS or costs) would increase understanding of the association between efficiency of treatment and patient outcome.
In conclusion, results revealed a slight increase in the proportion of the LOS-category 6–10 days and a slight decrease in the proportion of early readmissions associated with the NRS. Further, we found a decrease in hospital stays in the LOS-category of more than 28 days and an increase in the LOS-category 11–28 days. However, these changes were observed in both hospital types since 2005 and may therefore be unrelated to the NRS. Methodological considerations suggest a further evaluation of the NRS over a longer time period. Future developments of the NRS might lead to more comprehensive insights. The implementation of the new remuneration system remains an important step towards more appropriate mental health care financing.
Acknowledgement:We thank Heather Murray for language editing on a freelance basis.
1 OECD. Health at a Glance 2013: OECD Indicators [Internet]. Paris: The Organisation for Economic Co-operation and Development (OECD); 2013 [cited 2013 Dec 12]. Available from: http://dx.doi.org/10.1787/health_glance-2013–en.
2 WHO. Mental health policy and practice across Europe [Internet]. Kopenhagen: World Health Organization; 2007 [cited 2013 Dec 12]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0007/96451/E89814.pdf.
3 McDaid D. Psychiatric remuneration systems in Europe: an overview. Die Psychiatrie. 2011;8(1):9–15.
4 OECD. StatExtracts. Health expenditure and financing: % gross domestic product [Internet]. Paris: The Organisation for Economic Co-operation and Development (OECD); 2012 [updated 2013 May 2; cited 2013 Dec 12]. Available from: http://stats.oecd.org.
5 OECD. StatExtracts. Health Care Resources: Hospital beds [Internet]. Paris: The Organisation for Economic Co-operation and Development (OECD); 2012 [updated 2013 May 2; cited 2013 Dec 12]. Available from: http://stats.oecd.org.
6 FSO. Kosten und Finanzierung des Gesundheitswesens. Neuchatel: Swiss Federal Statistical Office (FSO); 2010.
7 OECD. StatExtracts. Health Care Utilisation: Average length of stay by diagnostic categories 2012 [Available from: http://stats.oecd.org.
8 Obsan. Stationäre Psychiatrie in der Schweiz 2000–2006. Neuchatel: Swiss Health Observatory; 2008.
9 GDKtZH. Psychiatrieplanung 2012. 1.Teil Versorgungsbericht Psychiatrie [Internet]. Zürich: Gesundheitsdirektion Kanton Zürich; 2011 [cited 2013 Dec 12]. Available from: http://www.gd.zh.ch/internet/gesundheitsdirektion/de/themen/behoerden/spitalplanung_spitallisten/psychiatrie/archiv_projekt_psychiatrieplanung_2012.html.
10 Thornicroft G, Tansella M. Components of a modern mental health service: a pragmatic balance of community and hospital care: overview of systematic evidence. Br J Psychiatry. 2004;185:283–90.
11 Knapp M, McDaid D, Ammadeo F, Constantopoulos A, Oliveira MD, Salvador-Carulla L, et al. Financing mental health care in Europe. J Ment Health. 2007;16(2):167–80.
12 Lave R, Frank G. Effect of the structure of hospital payment on length of stay. Health Serv Res 1990;25(2):327–47.
13 Schuhmacher DN, Namerow MJ, Parker B, Fox P, Kofie V. Prospective payment for psychiatry – feasability and impact. N Engl J Med. 1986;315(21):1331–6.
14 Taube CA, Goldman HH, Lee ES. Use of specialty settings in constructing DRGs. Arch Gen Psychiatry. 1988;45(11):1037–40.
15 Taube C, Lee ES, Forthofer RN. DRGs in psychiatry: An empirical evaluation. Med Care. 1984;22(7):597–610.
16 Rupp A, Steinwachs DM, Salkever DS. Hospital payment effects on acute inpatient care for mental disorders. Arch Gen Psychiatry. 1985;42(6):552–5.
17 Frank RG, Lave JR. A comparison of hospital responses to reimbursement policies for Medicaid psychiatric patients. Rand J Econ. 1989;20(4):588–600.
18 Lave JR, Frank RG, Taube C, Goldman H, Rupp A. The early effects of Medicare’s prospective payment system on psychiatry. Inquiry. 1988;25(3):354–63.
19 Rupp A, Steinwachs D, Salkever D. The effect of hospital payment method on the pattern and cost of mental health. Hosp Community Psych. 1984;35(5):456–9.
20 Lave J. Developing a Medicare prospective payment system for inpatient psychiatric care. Health Affair. 2003;22(5):97–109.
21 De Agostini P, Bomizzato P, Ammadeo F, Bisoffi G, Perali F, Tansella M. For a more rational funding system of mental health services. Analyses of costs for service supplied by community mental health services during a 7–year period. Epidemiol Psychiatr Soc. 2001;10(3):163–79. Italian.
22 Salvador-Garulla L, Garrido M, McDaid D, Haro JM. Financing mental health care in Spain. Context and critical issues. Eur J Psychiat. 2006;20(1):29–44.
23 Zechmeister I, Oesterle A, Denk P, Katschnig H. Incentives in financing mental health care in Austria. J Ment Health Policy Econ. 2002;5(3):121–9.
24 Frank RG, Lave JR. Per case prospective payment for psychiatric inpatients: an assessment and alternatives. J Health Polit Policy Law. 1986;11(1):83–96.
25 Frank RG, Lave JR. The effect of benfit design on the length of stay of medicaid psychiatric patients. JHR. 1986;21(3):321–37.
26 OFR. Federal Register, Medicare Program; Inpatient Psychiatric Facilities Prospective Payment System – Update for Fiscal Year Beginning October 1, 2013 (FY 2014) [Internet]: Office of the Federal Register (OFR); 2013 [cited 2013 Dec 12]. Available from: https://www.federalregister.gov/articles/2013/08/01/2013–18445/medicare-program-inpatient-psychiatric-facilities-prospective-payment-system-update-for-fiscal-year.
27 Klose P, Dirschedl P, Mohrmann M. Fallpauschalen in der Krankenhaus-Psychiatrie der USA. Das Inpatient Psychiatric Facility Prospective Payment System (IPF PPS). Gesundheitswesen. 2010;72(8–9):487–91.
28 InEK. PEPP-Entgeltsystem 2013 [Internet]: Institut für das Entgeltsystem im Krankenhaus (InEK); 2013 [cited 2013 Dec 12]. Available from: http://www.g-drg.de/cms/PEPP-Entgeltsystem_2013.
29 GDKtZH. PSYREC-KTR-Handbuch [Internet]. Zurich: Department of Health Canton of Zurich; 2007 [cited 2013 Dec 12]. Available from: http://www.gd.zh.ch/internet/gesundheitsdirektion/de/themen/institutionen/spitaeler_kliniken/handbuecher_vorgaben_erhebung.html.
30 Frick U, Winfried B, Binder H. Hospital financing in inpatient psychiatry via DRG-based prospective payment – The Salzburg experience. Psychiatr Prax. 2001;28(Suppl 1):55–62.
31 Warnke I, Rössler W. Length of stay by ICD-based diagnostic groups as basis for the remuneration of psychiatric inpatient care in Switzerland. Swiss Med Wkly. 2008;138(35–36):520–7.
32 Warnke I, Rössler W, Herwig U. Does psychopathology at admission predict the length of stay of inpatient stay in psychiatry? Implications for financing psychiatric services. BMC Psychiatry. Epub 2011 Jul 29; 11: 120. DOI: 10.1186/1471–244X-11–120.
33 Becker T, Kilian R. Psychiatric services for perople with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care? Acta Psychiatr Scand. 2006;Suppl(429):9–16.
34 Long MJ, Fleming ST, Chesney JD. The impact of diagnosis related group profitability on the skimming and dumping of pschiatric diagnosis related groups. Int J Soc Psychiatry. 1993;39(2):108–20.
35 IOM. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academic Press: Institute of Medicine; 2001.
36 GDKtZH. Zürcher Psychiatrieplanung 2012. 2.Teil: Strukturbericht Psychiatrie [Internet]. Zürich: Gesundheitsdirektion Kanton Zürich; 2011 [cited 2013 Dec 12]. Available from: http://www.gd.zh.ch/internet/gesundheitsdirektion/de/themen/behoerden/spitalplanung_spitallisten/psychiatrie.html http://www.gd.zh.ch/internet/gesundheitsdirektion/de/themen/behoerden/spitalplanung_spitallisten/psychiatrie.htm .
37 RCPSYCH. Health of the Nation Outcome Scales [Internet]. London: Royal College of Psychiatrists; 2013 [cited 2013 Dec 12]. Available from: http://www.rcpsych.ac.uk/crtu/healthofthenation.aspx.
38 MacDonald AJ, Elphick M. Combining routine outcomes measurement and “Payment by Results”: will it work and is it worth it? Br J Psychiat. 2011;199(3):178–9.
39 Sikka R. Pay for performance in emergency medicine. Ann Emerg Med. 2007;49(6):756–61.
40 Bremer RW, Scholle SH, Keyser D, Houtsinger JV, Pincus HA. Pay for performance in behavioral health. Psychiat Serv. 2008;59(12):1419–29.
Funding / potential competing interests:The authors have no competing interests to declare. There was no extra funding related to the study and the manuscript preparation. Accordingly, no funding body was involved in the study design, analysis, or interpretation of the data, in writing the manuscript and in the decision to submit the manuscript for publication.