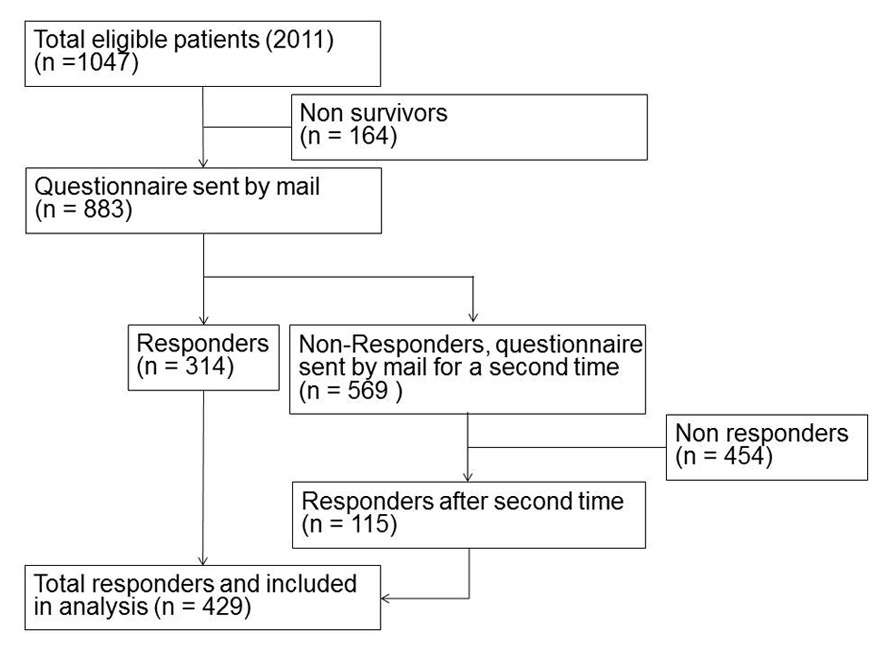
Figure 1
Patient inclusion flow chart 2011.
DOI: https://doi.org/10.4414/smw.2014.13972
An observational study in two tertiary university centres
On 1 January 2012 a new uniform case-based payment system for inpatients was introduced in Switzerland in order to decrease the costs for medical treatment mainly by shortening length of stay (LOS) and optimising efficiency [1–4]. Due to the consistently rising health care costs such a reform was strongly encouraged by politics [5, 6]. Another goal was better transparency regarding reimbursement to get a better comparability and thereby increases in efficiency [7]. The SwissDRG system is a flat rate system. DRG stands for diagnoses related groups. Several diagnoses are collected in preferably homogeneous groups containing patients with similar age, sex, diagnoses, co-morbidities, complications and treatment. For each of these groups a fixed remuneration for in-patients is defined [8].
Before 2012 various reimbursement systems were applied in different states (cantons) within Switzerland. Some cantons applied the fee-for-service (FFS) based system remunerating single medical services on top of a daily fee. Other cantons applied a precursor of the current Swiss DRG system, the all patient (AP-) DRG system.
The DRG system was developed at Yale University in the 1970’s. Since then many adaptations were developed in several countries all over the world. The SwissDRG is based on the German (G-) DRG, which has its roots in the Australian refined (AR-) DRG. The AR-DRG was derived from the AP-DRG [8].
Before the introduction of SwissDRG some concerns were raised among physicians regarding possible decreases in the quality of care [3, 9]. The main concerns were so-called “bloody exits”, the premature discharging of patients leading to a high re-hospitalisation rate. This concern was raised in literature mostly from the United States during the 1980’s, but also in newer reports from Germany [1, 2, 10]. Furthermore, patient satisfaction with the treatment and the discharge was expected to decrease.
To investigate these concerns we compared the clinical outcome and the patients’ satisfaction before and after the introduction of SwissDRG in two tertiary hospitals in Switzerland, the University Hospital Basel (USB) and the Cantonal Hospital Aarau (KSA). These two hospitals are located in different cantons, which initially (up to 2012) had two different reimbursement systems (FFS and AP-DRG, respectively).
In an earlier study in 2011, we compared the FFS hospital USB and the AP-DRG hospital KSA regarding LOS and patients’ outcome before 2012 [11]. The investigation showed a shorter LOS in the AP-DRG hospital. However, this result did not remain significant after multivariate adjustment. The re-hospitalisation rate was significantly higher in the FFS hospital before and after adjustments, which may have resulted from the higher co-morbidity load in the FFS hospital (higher prevalence of diabetes and renal failure).
The aim of the current study was to investigate the influence of the implementation of the SwissDRG in 2012 regarding LOS, patients’ outcome and satisfaction. According to our knowledge and literature search, no newer studies have been performed addressing these goals after the introduction of SwissDRG.
This is a prospective, two centre observational cohort study using a survey with patients discharged from the University Hospital Basel and the Cantonal Hospital Aarau in northwestern Switzerland. The postal mail survey took place between January and June 2011 and January and June 2012. The University Hospital of Basel is a tertiary referral centre with 670 beds treating around 31,600 hospitalised patients a year. Until the end of 2011 a fee-for-service based reimbursement system was in place at this hospital. From 1 January 2012 onwards the reimbursement system was changed to SwissDRG in the whole of Switzerland. The Cantonal Hospital Aarau is also a tertiary university-affiliated hospital with 630 beds treating roughly 26,700 hospitalised patients per year. As opposed to Basel, this hospital used the AP-DRG reimbursement system up to the end of 2011 switching to the SwissDRG at the same time as the University Hospital Basel.
The two local ethical committees approved the study protocol.
All patients hospitalised between January and June 2011 and 2012 with the International Code of Disease (ICD-10) diagnosis of a community-acquired pneumonia (CAP; ICD-10 codes J10.0, J12–18), acute heart failure (AHF; ICD-10 code I50), exacerbation of chronic obstructive pulmonary disease (COPD; ICD-10 code J44.1) or hip fracture (ICD-10 codes S72.0–1) were included in our study. We chose these diagnostic groups because they represent important and well-defined patient cohorts within the medical and surgical spectrum. 2–4 months after hospital discharge they received a questionnaire by postal mail. A second mailing was sent to non-responders.
Patients who died during the hospitalisation or were under the age of 16 years were excluded. Patients hospitalised several times at the same study centre during the same study period in 2011 or 2012 were analysed on first admission and excluded in all further admissions because of potential recall bias.
Our primary endpoint was to analyse, whether the change in reimbursement systems between 2011 (pre-cohort) and 2012 (post-cohort) was associated with a change in LOS. LOS is defined as the time frame between the admission and the discharge from hospital. Secondary endpoints were patients’ satisfaction regarding care in general as well as the discharge process, the re-hospitalisation rate, the admission to a rehabilitation institution and health-related quality of life. Furthermore, visits to the general practitioner concerning the hospitalisation were of interest.
Overall satisfaction with the hospitalisation was determined by a scale from 0% (very bad) to 100% (very good). The definition of re-hospitalisation was the admission to a hospital in the first 3 months after the primary hospitalisation. Quality of life was using modified questions from the EQ-5D questionnaire with the dimensions mobility, self-care, usual activities, pain/discomfort and anxiety/depression (see questionnaire in Appendix 1).
We used mean and standard deviation or median and interquartile range as appropriate to describe the population. Because LOS is a heavily skewed outcome, simple linear regression models are not appropriate. We therefore compared differences between LOS by fitting a generalised linear model (GLM) using gamma distribution and log link function as recommended [12]. LOS was compared between the two cohorts overall, and within different subgroups (e.g., main medical diagnosis, study centre). To deal with potential confounding between the pre-cohort and post-cohort, we adjusted all models for the main predictors of LOS namely age, gender, diagnosis and the most important co-morbidities (anaemia, congestive heart failure, COPD, diabetes, hypertension, coronary heart disease, renal insufficiency, malignancy, history of trauma). For secondary endpoints, similar linear regression models were used for the continuous, normally distributed data and logistic models for binary data.
Reported confidence intervals are two-sided 95% intervals and tests were performed at the two-sided 5% significance level. All analyses were performed with STATA 12.1 (Stata Corp, College Station, Texas).
When mentioning a “trend” we refer to a p between >0.05 and <0.20.
| Table 1:Baseline characteristics of included patients according to time period. | ||||
| Overall | 2011 | 2012 | p-value | |
| (n = 841) | (n = 429) | (n = 412) | ||
| Sociodemographics | ||||
| Age, median (IQR)* | 76.7 (66, 83.1) | 77 (66.7, 83.6) | 76 (66, 83) | 0.250 |
| Male gender | 50.8% (n = 427) | 47.8% (n = 205) | 53.9% (n = 222) | 0.077 |
| Study centres | ||||
| (Former) AP-DRG | 32.8% (n = 276) | 36.1% (n = 155) | 29.4% (n = 121) | 0.037 |
| (Former) FFS | 67.2% (n = 565) | 63.9% (n = 274) | 70.6% (n = 291) | |
| Main diagnosis | ||||
| Acute heart failure | 32.22% (n = 271) | 33.80% (n = 145) | 30.58% (n = 126) | 0.177 |
| Community-acquired pneumonia | 34.48% (n = 290 ) | 34.03% (n = 146 ) | 34.95% (n = 144 ) | |
| Acute exacerbation of COPD** | 14.27% (n = 120 ) | 11.89% (n = 51) | 16.75% (n = 69) | |
| Hip fracture | 19.02% (n = 160 ) | 20.28% (n = 87) | 17.72% (n = 73 ) | |
| Co-morbidities | ||||
| Any co-morbidities | 45.5% (n = 383) | 45% (n = 193) | 46.1% (n = 190) | 0.743 |
| Renal failure | 10.3% (n = 87) | 9.1% (n = 39) | 11.7% (n = 48) | 0.223 |
| Malignancy | 2.7% (n = 23) | 2.8% (n = 12) | 2.7% (n = 11) | 0.910 |
| Gastrointestinal disease | 4.3% (n = 36) | 4.4% (n = 19) | 4.1% (n = 17) | 0.828 |
| COPD | 17.8% (n = 150) | 16.3% (n = 70) | 19.4% (n = 80) | 0.240 |
| Diabetes type II | 8.4% (n = 71) | 7.7% (n = 33) | 9.2% (n = 38) | 0.425 |
| Hypertension | 15.0% (n = 126) | 16.3% (n = 70) | 13.6% (n = 56) | 0.268 |
| Coronary heart disease | 16.1% (n = 135) | 16.6% (n = 71) | 15.5% (n = 64) | 0.688 |
| Congestive heart failure | 10.7% (n = 90) | 10.7% (n = 46) | 10.7% (n = 44) | 0.984 |
| Other cardiac diseases | 19.9% (n = 167) | 21.2% (n = 91) | 18.5% (n = 76) | 0.315 |
| History of stroke | 5.4% (n = 45) | 5.8% (n = 25) | 4.9% (n = 20) | 0.531 |
| Other neurological diseases | 4.6% (n = 39) | 3.7% (n = 16) | 5.6% (n = 23) | 0.201 |
| Anaemia | 4.8% (n = 40) | 5.6% (n = 24) | 3.9% (n = 16) | 0.244 |
| History of fracture or trauma | 7.3% (n = 61) | 9.3% (n = 40) | 5.1% (n = 21) | 0.018 |
| * p-value refer to Mann-Whitney-U and chi-square tests ** chronic obstructive pulmonary disease | ||||
1983 patients (2011 n = 1,047, 2012 n = 936) of the two study centres met the inclusion requirements. A letter and questionnaire were sent to 1,657 patients (83.6%) after exclusion of non-survivors. 29.2% (n = 578) returned the complete questionnaire and after a second send-out the number of responders rose to 42.41% (n = 841). These 841 patients (= 100%; 429 (41%) in 2011 and 412 in 2012 (44%) were included in the study (see inclusion flow charts in figures 1 and 2). 78.6% (n = 661) of the questionnaires were fully completed; in 13.4% (n = 113) one question and in 8.0% (n = 67) two or more questions were missing. The most common main diagnosis was CAP with 34.5% (n = 290) followed by AHF in 32.2% (n = 271; see table 1). Hip fracture was present in a smaller group of 19.0% (n = 160) and acute exacerbation of COPD was the least frequent main diagnosis with 14.3% (n = 120). The overall median patient age was 76.7 years, which was similar in both time periods (p = 0.25). 50.8% (n = 427) of patients were male with a higher proportion in the second time period (47.8%, n = 205 in 2011 vs. 53.9%, n = 222 in 2012; p = 0.077). The occurrence of the four main diagnoses did not show a statistical significant difference between 2011 and 2012. Almost half (45.5%, n = 383) of patients were suffering from at least one comorbidity. Taken both years together, the most frequently represented co-morbidities were coronary heart disease with 16.1% (n = 135), hypertension (15%, n = 126), congestive heart failure with 10.7% (n = 90) and renal insufficiency (10.3%, n = 87). The four co-morbidities hypertension, coronary heart disease, congestive heart failure and history of stroke were similarly represented in both time periods. Congestive heart failure showed by far the smallest difference between 2011 and 2012 (p = 0.984). These above mentioned four co-morbidities belong to the group of cardiovascular diseases, the main cause of death in Switzerland according to Swiss Federal Statistical Office (BFS) [13]. Also, the second most common cause of death, namely malignancy showed an almost identical prevalence within the two time periods (p = 0.910). The mentioned similarities between the two cohorts of 2011 and 2012 regarding co-morbidities point to the comparability of the two data sets. The largest difference between 2011 and 2012 was found regarding the prevalence of the co-morbidity “history of fracture or trauma”, which was higher in 2011 than in 2012 (p = 0.018). Co-morbidities occurring in less than 20 patients are not listed in the tables.
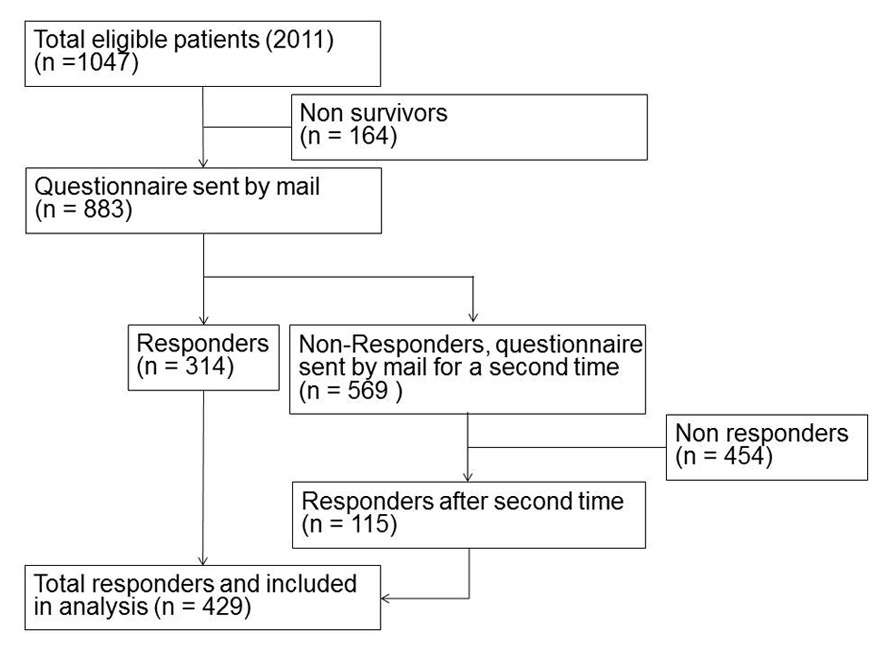
Figure 1
Patient inclusion flow chart 2011.
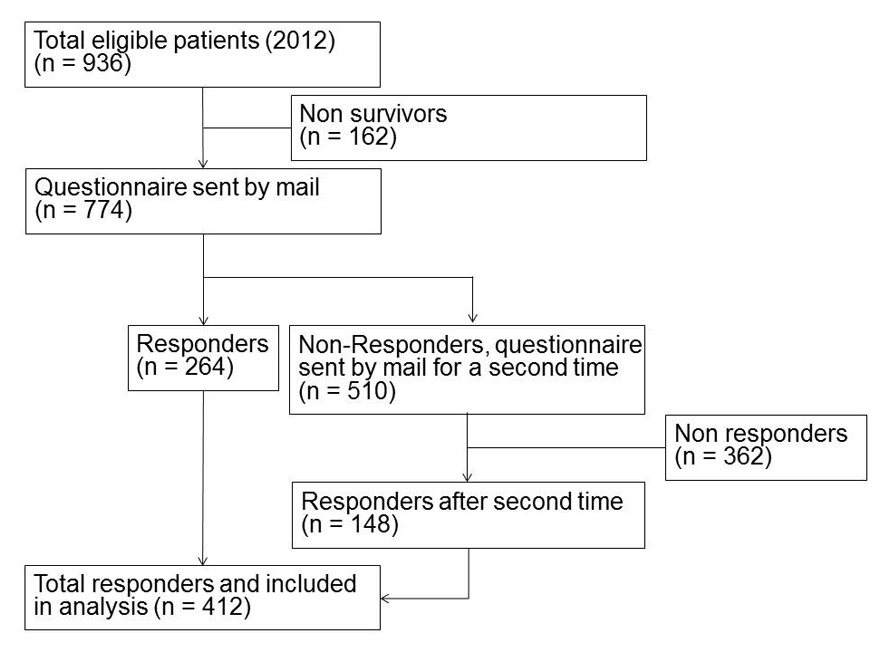
Figure 2
Patient inclusion flow chart 2012.
Mean LOS in the overall patient population was 10.0 days (95%CI 9.4, 10.6). Overall, LOS was not different between the 2011 and the 2012 cohorts (9.7 days vs 10.3 days, p = 0.43). This was also true for the subgroups of patients with CAP, AHF and hip fracture, where no differences in LOS was observed after the introduction of SwissDRG. In patients with acute exacerbation of COPD there was a trend towards longer LOS without reaching statistical significance (p = 0.118). Table 2 shows detailed results for the overall cohort and the four main diagnoses. The longest LOS was found in hip fracture patients (11.5 days, 95%CI 9.7, 13.2) followed by acute exacerbation of COPD patients (10.9 days, 95%CI 8.8, 12.9), AHF patients (9.8 days, 95%CI 9.0, 10.6). CAP patients had the shortest LOS of 9.0 days (95%CI 8.2, 9.8).
Patients who were discharged to a post-acute care facility had a significantly longer LOS compared to patients discharged home in the 2011 cohort (12.0 vs 8.9 days, p <0.01) and the 2012 cohort (12.4 vs 9.2 days, p <0.01). However, there was no difference in the frequency of post-acute care facility relocation between the two time cohorts (30.0% vs 32.4%, respectively, p = 0.40), which is a potential confounder for our results. Also, there was no effect modification on LOS difference between 2011 and 2012 by post-acute care facility relocation of our main statistical model (p interaction term = 0.45).
The re-hospitalisation rate was similar in the two cohorts (9.3%, n = 37) in 2011 and 11.6% in 2012 (n = 46, p = 0.317). Furthermore, similar rates of follow-ups were observed at the general practitioners’ (GP, 60.6%, n = 260 in 2011 vs 62.4%, n = 257 in 2012; p = 0.392).
Overall satisfaction with care did not change much after the introduction of SwissDRG and remained high (89.0% in 2011 vs 87.8% in 2012; p = 0.429). The number of patients satisfied with the date of discharge was also similar in 2011 and 2012 (88.6%, n = 380 vs 91.3%, n = 376; p = 0.299). However, there was a trend with more patients feeling insecure on discharge in 2012 (23.1%, n = 99 vs 26.7%, n = 110; p = 0.141).
Quality of life was assessed with a standardised questionnaire across five dimensions (EQ-5D, mobility, self-care, usual activities, pain and depression). A high proportion of patients reported problems with their mobility (48.2%, n = 405), during usual activities (49.8%, n = 419) and with pain or discomfort respectively (50.1%, n = 421). The number of patients experiencing problems with mobility, usual activities and anxiety/depression stayed the same. Regarding self-care as well as pain or discomfort there was no difference between 2011 to 2012, although there was a trend towards more problems with self-care (p = 0.100) and more pain or discomfort (p = 0.186).
| Table 2:Primary and secondary endpoints with regard to time period. | |||||
| Overall | 2011 | 2012 | Adjusted regression coefficient or odds ratio† | p-value | |
| (n = 841) | (n = 429) | (n = 412) | |||
| LOS**, [days], mean (CI) | |||||
| All patients | 9.99 (9.41, 10.58) | 9.72 (9.00, 10.45) | 10.27 (9.35, 11.20) | Coefficient 0.05 (–0.07, 0.16) | 0.430 |
| Acute heart failure | 9.81 (8.98, 10.64) | 10.28 (9.03, 11.54) | 9.26 (8.21, 10.31) | Coefficient -0.12 (–0.28, 0.05) | 0.171 |
| Community-acquired pneumonia | 8.99 (8.19, 9.79) | 8.58 (7.32, 9.84) | 9.40 (8.42, 10.38) | Coefficient 0.07 (–0.11, 0.24) | 0.463 |
| Acute exacerbation of COPD*** | 10.86 (8.83, 12.89) | 9.22 (7.49, 10.94) | 12.07 (8.76, 15.38) | Coefficient 0.29 (–0.07, 0.65) | 0.118 |
| Hip fracture | 11.48 (9.72, 13.24) | 11.01 (9.29, 12.73) | 12.04 (8.71, 15.37) | Coefficient 0.03 (–0.25, 0.32) | 0.822 |
| (Former) AP-DRG | 8.42 (7.77, 9.06) | 8.46 (7.62, 9.29) | 8.36 (7.33, 9.40) | Coefficient 0.00 (–0.15, 0.15) | 0.979 |
| (Former) FFS | 10.76 (9.96, 11.57) | 10.44 (9.42, 11.47) | 11.07 (9.84, 12.30) | Coefficient 0.05 (–0.10, 0.20) | 0.545 |
| Re-hospitalisation rate | 10.4% (n = 83) | 9.3% (n = 37) | 11.6% (n = 46) | OR 1.27 (0.80, 2.03) | 0.317 |
| Rehabilitation after discharge | 31.0% (n = 250) | 29.7% (n = 121) | 32.4% (n = 129) | OR 1.24 (0.89, 1.72) | 0.198 |
| Follow-up by general practitioner | 61.5% (n = 517) | 60.6% (n = 260) | 62.4% (n = 257) | OR 1.13 (0.85, 1.51) | 0.392 |
| Overall satisfaction with care (100%-0%), mean (SD) | 88.4% (±15.92) | 89.0% (±15.43) | 87.8% (±16.43) | Coefficient –0.90 (–3.13, 1.33) | 0.429 |
| Satisfaction with discharge procedure | |||||
| Not satisfied with date of discharge | 10.1% (n = 85) | 11.4% (n = 49) | 8.7% (n = 36) | OR 0.78 (0.49, 1.24) | 0.299 |
| Too early | 8.4% (n = 71) | 9.6% (n = 41) | 7.3% (n = 30) | OR 0.79 (0.48, 1.30) | 0.351 |
| Too late | 1.7% (n = 14) | 1.9% (n = 8) | 1.5% (n = 6) | OR 0.75 (0.25, 2.25) | 0.609 |
| Feeling of insecurity at discharge | 24.9% (n = 209) | 23.1% (n = 99) | 26.7% (n = 110) | OR 1.27 (0.92, 1.76) | 0.141 |
| Insufficient informed about discharge | 10.9% (n = 83) | 12.8% (n = 49) | 9.0% (n = 34) | OR 0.67 (0.42, 1.08) | 0.101 |
| Not satisfied with date of information about discharge | 7.7% (n = 65) | 8.9% (n = 38) | 6.6% (n = 27) | OR 0.73 (0.43, 1.23) | 0.232 |
| Too early | 1.0% (n = 8) | 1.2% (n = 5) | 0.7% (n = 3) | OR 0.59 (0.13, 2.67) | 0.496 |
| Too late | 6.8% (n = 57) | 7.7% (n = 33) | 5.8% (n = 24) | OR 0.74 (0.42, 1.29) | 0.291 |
| Insufficient informed about procedures at home after discharge | 6.5% (n = 55) | 6.8% (n = 29) | 6.3% (n = 26) | OR 0.91 (0.52, 1.59) | 0.735 |
| Quality of life (QoL according to EQ-5D) today | |||||
| Any problems with mobility | 48.2% (n = 405) | 46.9% (n = 201) | 49.5% (n = 204) | OR 1.18 (0.89, 1.57) | 0.254 |
| Any problems with self-care | 27.7% (n = 233) | 25.2% (n = 108) | 30.3% (n = 125) | OR 1.30 (0.95, 1.79) | 0.100 |
| Any problems with usual activities | 49.8% (n = 419) | 50.8% (n = 218) | 48.8% (n = 201) | OR 0.92 (0.69, 1.22) | 0.569 |
| Any problems with pain/discomfort | 50.1% (n = 421) | 48.0% (n = 206) | 52.2% (n = 215) | OR 1.21 (0.91, 1.59) | 0.186 |
| Any problems with anxiety/depression | 34.4% (n = 289) | 34.7% (n = 149) | 34.0% (n = 140) | OR 0.96 (0.72, 1.29) | 0.794 |
| * Results are derived from generalised linear model (GLM) with a gamma distribution for LOS, logistic regression for binary outcomes and linear models for continuous outcomes. **length of stay [days] ***chronic obstructive pulmonary disease † models adjusted for the main predictors of LOS, namely age, gender, study centre, diagnosis and co-morbidities (anaemia, congestive heart failure, COPD, diabetes type II, hypertension, coronary heart disease, renal insufficiency, malignancy, trauma). | |||||
Overall, there were only few if any relevant changes, as was to be expected due to the short time interval of one year between the two cohorts. Nevertheless there were some important early trends, which may forecast changes in the future.
The two time cohorts were rather similar regarding co-morbidities and therefore well balanced. Regarding baseline characteristics only two significant differences were apparent: There were significantly less patients with history of fracture and trauma and a higher proportion of men in 2012. These differences may be explained by a changing patient flow pattern due to the implementation of SwissDRG and possibly changing demographics. To confirm this assumption another study investigating the admission flows to hospitals should follow.
The expectation was that LOS would decrease with the implementation of the SwissDRG. The data in this study show that LOS remains stable or even tends to increase shortly after implementation of SwissDRG. The reason for this trend can only be assumed and may be due to changes in the patient transfer processes from acute to post-acute care hospitals. This assumption is based on the fact that the process of coverage confirmation by the insurer for post-acute care facilities was changed with the implementation of SwissDRG. The change of remuneration systems to SwissDRG allows the insurer now to use eight working-days’ time to decide regarding provision of cost coverage for post-acute care institutions. However, further studies are necessary to identify the reasons for this development.
In 2003 the G-DRG was introduced in Germany [8]. Bartkowski et al. analysed the development of LOS in Germany between 1994 and 2010. They observed a continuously decreasing LOS. Particularly no significant change in this trend after the implementation of the G-DRG was observed [10]. However, as mentioned previously, the study period after the DRG implementation was only six months. Follow-up –studies are needed to verify a decrease in LOS of hospitalised patients as would be expected in accordance with the data from Germany.
The concerns about “bloody exits” meaning too early discharge from hospitals did not become evident in this study. Patients did not feel that they were discharged too early. Furthermore, there was no significant increase in the number of visits to the GP’s office after DRG implementation.
However, although patients agreed with the time point of discharge, there was still a noteworthy trend for these same patients to feel more insecure, to have more problems with self-care and more pain or discomfort. This may lead to the assumption of too early discharge. Another explanation may be that by the implementation of DRG sicker patients with more co-morbidities are directed rather towards tertiary care hospitals and less sick patients to peripheral institutions. To verify these assumptions and trends, further research in this area and a longer follow-up of our cohort should be conducted.
Our study has several limitations. First, it was a short study period of six months after the nation-wide DRG-implementation. The time point chosen for the analysis is still relevant in order not to miss early effects. It allowed us to identify some important trends but may be too short to draw final conclusions. Second, our study comprised two centres in the northwestern part of Switzerland. Therefore, the results may not be generalisable to other parts of the country or other regions of the world the same is true for the diagnoses used where our findings may not be the same for other illnesses than the ones studied here. Interestingly however, like in our study, the Swiss Federal Statistical Office (BFS) observed the same stable or even slightly increasing LOS for all Swiss hospitals from 2011 to 2012 [14]. Third, patients with four defined main diagnoses were included; other diagnoses may show different patterns regarding LOS and quality of care. However, we believe that these four diagnoses represent an important part of patients in tertiary referral centres. Fourth, the sample size of patients may have been too low and trends may differ looking at larger patient samples. Fifth, several circumstances may have created a selection bias. We included inpatients exclusively during the first six months of 2011 und 2012 seeking to exclude seasonal confounders. However, we cannot exclude that the second half of the years 2011 and 2012 may show different results. Furthermore, our study population was selected in two study centres only. Also, the questionnaire was written in German which might have excluded patients not fluent enough in this language. Sixth, the questionnaires were sent to the patients two to four months after discharge and may therefore be subject to recall bias. Also, some patients were hospitalised more than once in other hospitals during the observation period and may therefore have referred to the wrong hospitalisation. Seventh, we cannot exclude confounding by the fact that the AP-DRG remuneration system was in place at one study site in 2011 which might have mitigated the difference between the two study periods.
In conclusion the nation-wide implementation of SwissDRG took place without major problems. Although our study shows some limitations we observed some noteworthy trends. We suggest further studies in order to monitor these developments.
Please download here the questionnaire in PDF format.
Acknowledgement:Rakesh Padiyath, Ursula Althaus and Thomas Gaida were very helpful and swift in retrieving the patient data at Basel University Hospital. Nadine Binda and Sabina Roth were of great help for the printing of envelopes.
1 Donaldson C, Magnussen J. DRGs: the road to hospital efficiency. Health Policy. 1992;21(1):47–64.
2 Davis C, Rhodes DJ. The impact of DRGs on the cost and quality of health care in the United States. Health Policy. 1988;9(2):117–31.
3 Busato A, von Below G. The implementation of DRG-based hospital reimbursement in Switzerland: A population-based perspective. Health Res Policy Syst. 2010;8:31.
4 Schuetz P, Albrich WC, Suter I,Hug BL,Christ-Crain M, Holler T, et al. Quality of care delivered by fee-for-service and DRG hospitals in Switzerland in patients with community-acquired pneumonia. Swiss Med Wkly. 2011;141:w13228.
5 Rosenthal MB. Beyond pay for performance – emerging models of provider-payment reform. N Engl J Med. 2008;359(12):1197–200.
6 Rosenthal MB. What works in market-oriented health policy? N Engl J Med. 2009;360(21):2157–60.
7 SwissDRG-AG. Fallpauschalen in Schweizer Spitälern: Basisinformationen für Gesundheitsfachleute. Available from: http://www.swissdrg.org/assets/pdf/de/Broschuere_SwissDRG_d_A4.pdf.
8 Fischer Wolfram. Die DRG Familie. 2008; Available from: http://www.fischer-zim.ch/textk-pcs-pdf/DRG-Familie-0801.pdf.
9 Busse R, Geissler A, Aaviksoo A, Cots F, Hakkinen U, Kobel C, et al. Diagnosis related groups in Europe: moving towards transparency, efficiency, and quality in hospitals? BMJ. 2013;346:f3197.
10 Bartkowski R. Length of hospital stay due to DRG reimbursement. Ther Umsch. 2012;69(1):15–21.
11 Weissenberger N, Thommen D, Schuetz P, Mueller B, Reemts C, Holler T, et al. Head-to-head comparison of fee-for-service and diagnosis related groups in two tertiary referral hospitals in Switzerland: an observational study. Swiss Med Wkly. 2013;143:w13790.
12 Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465–88.
13 BFS, B.f.S. Todesfälle: Anzahl, Entwicklung und Ursachen. 2013; Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/02/04/key/01.html.
14 BFS, B.f.S. Durchschnittliche Spitalaufenthaltsdauer. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/01/keyw.html.
Authors’ contribution: NW, DT and PS contributed equally.
Funding / potential competing interests: The University Hospital Basel, Switzerland, provided an unconditional research grant for this study. All authors declare that they have no competing interests.