Figure 1
Flow chart.
DOI: https://doi.org/10.4414/smw.2014.13978
Coronary artery bypass grafting using extracorporeal circulation (ECC) is the gold standard in the surgical treatment of coronary artery disease. Several studies have shown this to be a safe procedure with a low mortality rate and excellent outcomes [1, 2]. However, there is evidence, that ECC is associated with different adverse effects such as systemic inflammatory response syndrome (SIRS), renal insufficiency, alveolar damage or neurovascular complications [2–4].
Thus, efforts have been made to avoid conventional ECC: off-pump coronary artery bypass grafting (OBCABG) with myocardial revascularisation on the beating heart as well as the use of minimal extracorporeal circulation (MECC) have gained popularity within the last years and are well-proven procedures in coronary artery bypass grafting [3, 5]. It has been shown that perioperative morbidity of MECC and OPCABG is similar or even less compared to coronary artery bypass grafting (CABG) with ECC resulting in a reduction of postoperative ventilation time, release of creatinine kinase, catecholamine therapy, drainage loss and transfusion requirements.
In addition, using these techniques seems to have beneficial effects regarding kidney injury, neurovascular and pulmonary complications [2, 3, 5, 6].
Nonetheless, there are some concerns regarding long- term patency rates and completeness of revascularisation in OPCABG.
The aim of this retrospective study was to compare the prevailing potential benefits of the MECC- technique with OPCABG revascularisation. The primary endpoint was Troponin T level (TrT), as it is a sensitive marker for myocardial damage and an indicator for the clinical outcome following open heart surgery [7]. We performed a propensity weighted analysis in order to diminish allocation bias.
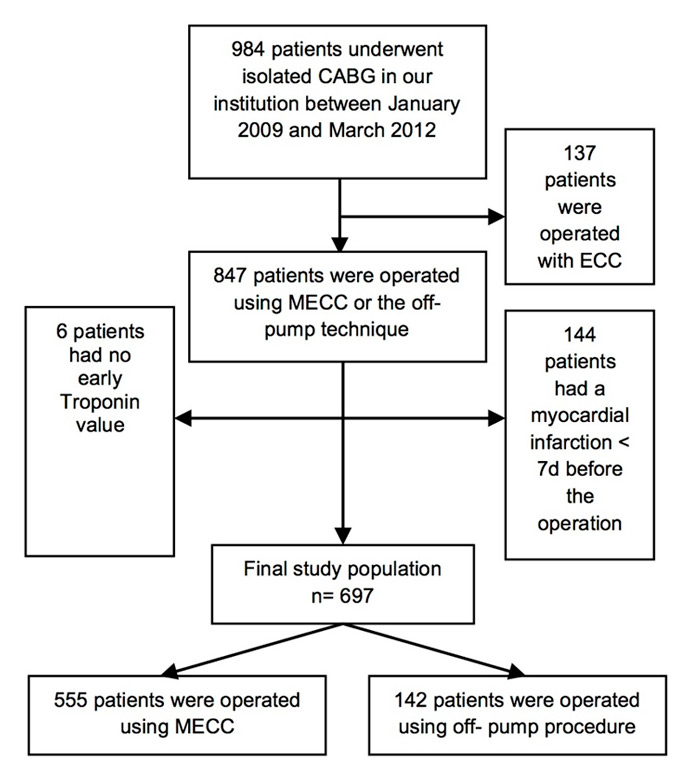
Between January 2009 and March 2012, 984 patients underwent isolated CABG in the clinic for cardiac surgery at the University Hospital Basel. A total of 137 (13.92%) patients were operated on using ECC; 685 (69.51%) with MECC and 163 (16.57%) off-pump. The indication for coronary surgery was based on currently published guidelines [8]. Standard procedure for isolated coronary artery bypass surgery in our institution is either off-pump revascularisation or MECC assisted surgery. Conventional ECC is now only used when open heart surgery is planned or suspected. The decision of whether to perform MECC or OPCABG was based on various parameters: renal insufficiency, age >80 years, ejection fraction <30%, extent of aortic calcifications as well as experience in off-pump surgery.
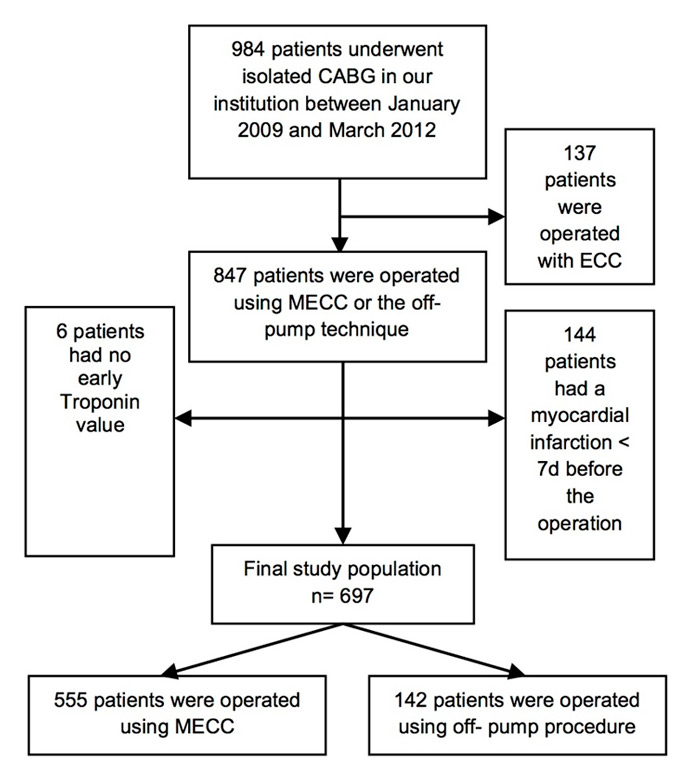
Figure 1
Flow chart.
Exclusion criteria for our study cohort were myocardial infarction within seven days before the operation (n = 144) and patients with no early Troponin T value (n = 6). Patients operated on with ECC (n = 137) were excluded, because usage of ECC does not comply with institutional standards. Finally, we observed a study population of 697 patients, of which 555 (79.63%) were operated using MECC and 142 (20.37%) using the off-pump technique (fig. 1).
The serological parameters were accrued according to the standard algorithm in our hospital, beginning on the first postoperative day (POD) and continuing during the following days until a normalisation of the values was observed.
The primary endpoint in our study was TrT serum levels, as they are an indicator for myocardial damage. As secondary endpoints we analysed the length of stay in the intensive care unit (ICU) and major cardiac or cerebrovascular events (MACCE) defined as in hospital mortality, myocardial ischemia or stroke and serological parameters. The latter included TrT, creatine kinase (CK) and creatine kinase- myocardial type (CK-MB). For each of these enzymes, we analysed the first postoperative value as well as the peak value during hospital stay.
In our clinic we used the closed Mini- ECC- system (MECC- System®,Minimal Extra Corporeal Circulation System, Maquet Rastatt, Germany) with a centrifugal pump and a Quadrox® oxygenator (Jostra Cardiopulmonary AG, Hirrlingen, Germany).
Revascularisation with MECC was performed through median sternotomy. After heparinisation the ascending aorta and the right atrium were cannulated. After cross-clamping, cardioplegic arrest was induced with Cardioplexol® (Fa. Bichsel, Interlaken, Switzerland) via the aortic root. Cardioplexol® is a colloid cardioplegia based on procaine, magnesium and potassium.
The internal mammary artery (IMA), radial artery or great saphenous vein were used as graft material.
A total of 15 (10.56%) of the 142 OPCABG operations were accomplished through an anterior lateral thoracotomy within a MIDCAB (minimal invasive direct coronary artery bypass) procedure, while the remaining 127 (89.44%) were performed through a median sternotomy.
All data were exported from our quality management database. Herein, data were regularly controlled for completeness and correctness.
Continuous variables are expressed as mean and standard deviation. Categorical variables are expressed as raw numbers and percentages. For the univariate statistical comparison of treatment groups, we used Fishers Exact Test or X2 for categorical and Mann-Whitney-U-Test for continuous variables. To investigate the treatment effect, we performed a multivariable regression analysis, including inverse propensity weights (IPTW). IPTWs were based on propensity scores derived from a logistic regression including all EuroSCORE items (age, gender, neurologic disease, chronic pulmonary disease, renal disease, pulmonary hypertension, ejection fraction, emergency, instable angina, recent myocardial infarction, extracardiac arteriopathy, critical preoperative state, reoperation, post-infarction ventricular septal defect, active endocarditis), together with the number of diseased vessels, main stem stenosis and body mass index. We checked for covariate imbalances by calculating p values after IPTW correction. We used Poisson regression with robust standard errors for the primary endpoint Troponin T and the secondary endpoints CK and CK-MB. We did not choose a linear regression model because the enzyme measurements were far away from being normally distributed. The log-linear Poisson model allows interpretation of effects in terms of Troponin T units or CK and CK-MB, respectively. We used a logistic regression for the secondary endpoint MACCE.
A p value of less than 0.05 was considered significant. All p values and confidence intervals are two-sided. Analyses were performed using SPSS (Statistical Package for Social Sciences), software release 17.0 for Windows (SPSS, Chicago, IL) and Stata 12.
The study obtained ethical approval by the responsible ethical committee (Ethikkommission beider Basel, EKBB), approval number 305/10.
| Table 1 | ||||
| MECC (n = 555) | Off-pump (n = 142) | p-value | p-value after IPTW | |
| Age (years) | 65.01 ± 9.5 | 69.39 ± 9.5 | <0.001 | 0.677 |
| Body mass index (kg m–2) | 28.50 ± 13.1 | 26.94 ± 4.1 | 0.004 | 0.595 |
| Ejection Fraction (%) | 52.41 ± 10.7 | 51.66 ± 11.1 | 0.671 | 0.508 |
| Logistic EuroSCORE I (%) | 4.92 ± 6.5 | 5.88 ± 6.8 | 0.017 | 0.773 |
| EuroSCORE II (%) | 2.09 ± 3.05 | 2.17 ± 2.06 | 0.749 | |
| Gender male (%) | 448 (80.6) | 115 (81.0) | 1.000 | |
| Dyslipidemia (%) | 465 (83.6) | 113 (79.6) | 0.013 | |
| Hypertension (%) | 499 (89.7) | 127 (89.4) | 0.874 | |
| Current or past nicotine intake (%) | 424 (76.3) | 104 (73.2) | 0.131 | |
| Angina pectoris CCS I (%) | 13 (2.3) | 16 (11.3) | <0.001 | |
| Angina pectoris CCS II (%) | 197 (35.4) | 73 (51.4) | ||
| Angina pectoris CCS III (%) | 304 (54.7) | 41 (28.9) | ||
| Angina pectoris CCS IV (%) | 25 (4.5) | 6 (4.2) | ||
| NYHA I (%) | 64 (11.5) | 61 (43.0) | <0.001 | |
| NYHA II (%) | 271 (48.7) | 41 (28.9) | ||
| NYHA III (%) | 81 (14.6) | 8 (5.6) | ||
| NYHA IV (%) | 2 (0.4) | 2 (1.4) | ||
| Emergency classification (<12 hours) (%) | 11 (2.0) | 1 (0.7) | 0.204 | 0.696 |
| Very urgent classification (<24 hours) (%) | 14 (2.5) | 1 (0.7) | ||
| Urgent classification (<48 hours) (%) | 39 (7.0) | 6 (4.2) | ||
| Elective classification (%) | 492 (88.5) | 134 (94.4) | ||
| Sinus rhythm (%) | 543 (97.7) | 138 (97.2) | 0.716 | |
| Atrial fibrillation (%) | 11 (2.0) | 3 (2.1) | 0.716 | |
| Myocardial infarction before operation (%) | 272 (48.9) | 51 (35.9) | 0.006 | 0.512 |
| Previous CABG (%) | 7 (1.3) | 2 (1.4) | 1.000 | |
| Previous cardiovascular surgery (%) | 39 (7.0) | 9 (6.3) | 0.844 | 0.719 |
| Previous PCI (%) | 131 (23.6) | 16 (21.1) | <0.001 | |
| lnstable Angina pectoris (%) | 64 (11.5) | 5 (3.5) | 0.003 | 0.829 |
| Number of diseased vessels | 2.89 ± 0.4 | 2.67 ± 0.7 | <0.001 | 0.923 |
| Main stem stenosis (%) | 148 (26.6) | 13 (9.2) | <0.001 | 0.800 |
| Chronic obstructive pulmonary disease (%) | 85 (15.3) | 11 (7.7) | 0.239 | 0.658 |
| Dialysis- chronic renal failure (%) | 4 (0.7) | 2 (1.4) | 0.58 | 0.928 |
| Carotid stenosis more than 50% (%) | 50 (9.0) | 15 (10.6) | 0.627 | |
| ASA IV or V (%) | 8 (1.4) | 3 (2.1) | 0.474 | |
| Plus–minus values are means ± Standard Deviation IPTW = inverse propensity weights | ||||
Between January 2009 and March 2012, 555 patients underwent CABG with MECC, whereas 142 patients were operated on using the off-pump technique. Patients undergoing OPCABG were significantly older (69.39 years ± 9.5 vs. 65.01 years ± 9.5; p value <0.001) with a higher logistic EuroSCORE I (5.88% ± 6.8 vs. 4.92% ± 6.5 ; p value = 0.017). Apart from that, demographic data (table 1) were not significantly different including EuroSCORE II (MECC: 2.09% ± 3.05; OPCABG: 2.17% ± 2.06; p value = 0.749). In both groups the majority of the patients were men (MECC 80.6%, off-pump 81.0%, p = 1.000), and the ejection fraction was virtually identical (MECC 52.41% ± 10.7, off-pump 51.66% ± 11.1, p = 0.671).
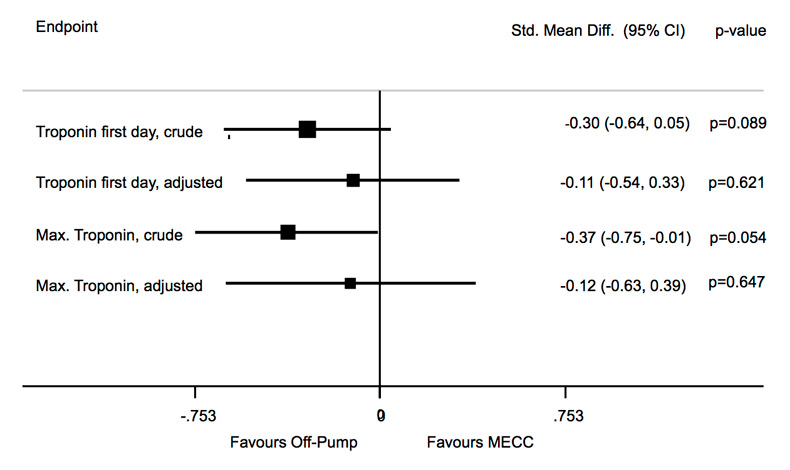
Figure 2
Forest plot regarding the values of TrT on the first postoperative day and the highest values of TrT.
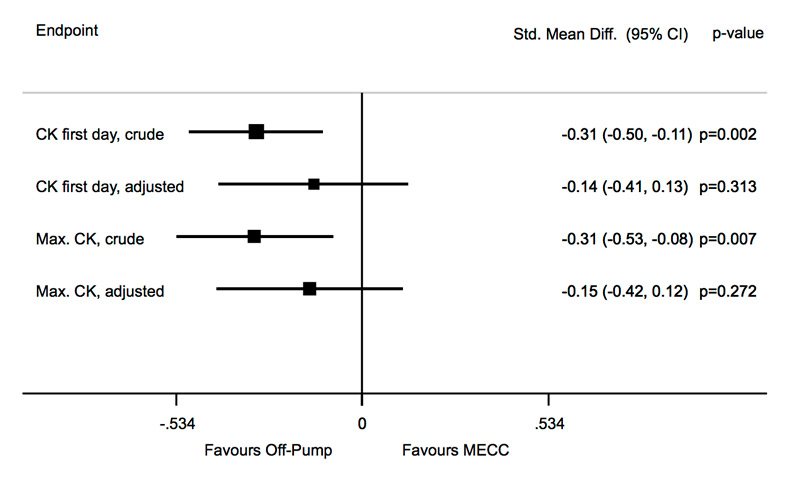
Figure 3
Forest plot regarding the values of CK on the first postoperative day and the peak value of CK.
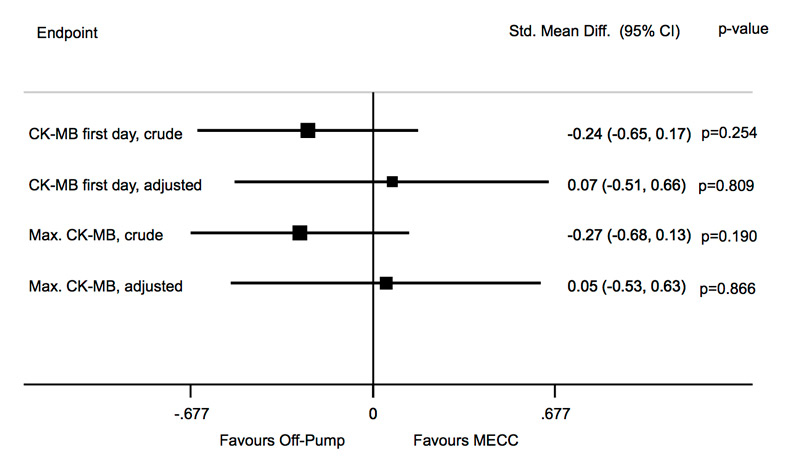
Figure 4
Forest plot regarding the values of CK-MB on the first postoperative day as well as peak level.
MECC and off-pump procedures were mostly elective (MECC 88.5% vs. off-pump 94.4%). In the MECC group 7% of the patients were operated urgently compared to only 4.2% of the patients in the off-pump group. Also very urgent and emergency indications were slightly more frequent in the MECC group (very urgent 2.5%, emergency 2.0%) compared to off-pump patients (very urgent 0.7%, emergency 0.7%). Atrial fibrillation occurred similarly in both groups (MECC 2.0% vs. off-pump 2.1%, p = 0.716), but myocardial infarction before the operation was seen significantly more often in the MECC group (48.9% vs. 35.9%, p = 0.009). Previous coronary artery bypass grafting was observed equally in both groups (MECC 1.3% vs. off-pump 1.4%, p = 1.000).
The duration of operation was slightly shorter in off-pump procedures (MECC 200.19 min ± 42.5, off-pump 191.39 min ± 42.1, p = 0.229). A significant difference was observed in the requirement of intra-operative blood. 8.6% (n = 48) of the patients undergoing CABG with MECC required intra-operative blood products while in the off-pump group only 0.7% (n = 1) were in the need of intra-operative blood products (p <0.001).
The number of distal anastomoses differed significantly with higher values in the MECC group (MECC 3.79 ± 0.9 vs. off-pump 3.24 ± 1.2; p <0.001).
In 100% of the patients who underwent OPCABG the internal mammary artery (IMA) was used whereas in the MECC group 98.6% of the patients received an IMA graft. The use of BIMA was more frequent in the OPCABG group. The radial artery was taken in 27.2% in the MECC group, and in 12% in the off-pump group (p <0.001). The great saphenous vein was used more often in the MECC group (89.4% vs. 74.6%, p <0.001).
Post-infarction ventricular septal defect and active endocarditis dropped out of the propensity modelling because of co-linearity. All other p values turned out to be >0.5 after IPTW correction (given in the 4th column of table 1). Propensity weighting eliminated imbalances of the preoperative risk factors.
In the evaluation of our primary endpoints we could not find a significant advantage of either treatment. Primary as well as peak TrT was slightly lower in the off-pump group in the crude comparison (reduction of primary TrT by using off-pump strategy was –0.30, 95% confidence interval [CI] –0.64 to 0.05, p = 0.089; reduction for peak TrT –0.37, CI –0.75 to 0.01, p = 0.054), but the difference almost disappeared in the multivariable analysis (reduction for primary TrT –0.11, CI –0.54 to 0.33, p = 0.621; for peak TrT –0.12, CI –0.63 to 0.39, p = 0.647) (fig. 2).
CK on the primary postoperative day showed a significant difference in the crude comparison (reduction of first CK by using off-pump strategy was –0.31, 95% confidence interval [CI] –0.50 to –0.11, p = 0.002) but was not significant anymore in the multivariable analysis (reduction of primary CK by using off-pump strategy was –0.14, 95% CI –0.41 to 0.13, p = 0.313). Nevertheless it still showed lower values in the off-pump group. Also peak CK showed significant lower values in the off-pump group in the crude analysis (reduction of peak CK by using off-pump strategy was –0.31, 95% CI –0.53 to –0.08, p = 0.007) which were not significant anymore in the multivariable analysis (reduction of peak CK by using off-pump strategy is –0.15, 95% CI –0.42 to 0.12, p = 0.272) (fig. 3).
Values of primary CK-MB as well as peak CK-MB showed no significant differences in the crude calculations (reduction of primary CK-MB by using off-pump strategy was –0.24, 95% confidence interval [CI] –0.65 to 0.17, p = 0.254; reduction for peak CK-MB –0.27, [CI] –0.68 to 0.13, p = 0.190). In the multivariable analysis primary CK-MB as well as peak CK-MB were slightly lower in the MECC group, but neither were significant (reduction of primary CK-MB by using off-pump strategy was 0.07, 95% CI –0.51 to 0.66, p = 0.809; reduction for peak CK-MB 0.05, CI –0.53 to 0.63, p = 0.866) (fig. 4).
Regarding the length of stay on the ICU there was a significant benefit using the off-pump procedure in the crude as well as in the multivariable analysis (crude: reduction of length of stay on the ICU by using the off-pump strategy was –0.30 95% CI –0.53 to –0.07, p = 0.010; multivariable: reduction for length of stay on the ICU –0.32, CI –0.56 to –0.07, p = 0.011) (fig. 5).
Comparing the occurrence of MACCE there was no significant difference to be observed in both calculations but a trend favouring OPCABG in the multivariable calculations was observed (crude: 1.09 95% CI 0.67 to 1.77, p = 0.730; multivariable: 0.82, 95% CI 0.61 to 1.09, p = 0.177) (fig. 6).
Atrial fibrillation or atrial flutter occurred similarly frequently in both groups (MECC 19.8%, off-pump 18.3%, p = 0.812). The need for re-exploration due to graft failure was low in both groups (MECC n = 8, 1.4%; off-pump n = 0, 0.05, p = 0.37). Re-exploration for bleeding was very rare in both groups (MECC n = 3, 0.5%; off-pump n = 1, 0.7%, p = 1.000). Occurrence of renal complications was comparably low in both groups. Postoperative renal insufficiency (defined as a doubling value of the preoperative creatinin value and a postoperative creatinin value >172 micromol/l or new onset of need for dialysis) was observed in 4.3% (n = 24) of the patients operated on with MECC and in 3.5% (n = 5) of the patients in the OPCAB group (p value = 0.816).
Stay on the ICU was significantly shorter among patients undergoing OPCAB (2.04 days ± 2.63) compared to the patients operated with MECC (2.76 days ± 2.79, p <0.001).
Neurovascular complications, defined as stroke and/or prolonged reversible ischemic neurologic deficit (PRIND) (MECC 1.6% vs. off-pump 0.7%, p = 0.696), and mortality (MECC 2.2% vs. off-pump 2.1%, p = 1.000) were comparable in both groups.
| Table 2 | |||
| MECC ( n = 555) | Off-pump (n = 142) | p-value | |
| Duration of operation (min) | 200.19 ± 42.5 | 191.39 ± 42.1 | 0.229 |
| Intraoperative blood products (%) | 48 (8.6) | 1 (0.7) | <0.001 |
| Number of distal anastomoses | 3.79 ± 0.9 | 3.24 ± 1.2 | <0.001 |
| Internal mammary artery use (%) | 547 (98.6) | 142 (100) | 0.370 |
| Left or right internal mammary artery use | 0.023 | ||
| Left internal mammary artery use (%) | 489 (88.1) | 116 (81.7) | |
| Right internal mammary artery use (%) | 6 (1.1) | 2 (1.4) | |
| Left and right mammary artery use (%) | 52 (9.4) | 24 (16.9) | |
| Radial artery use (%) | 151 (27.2) | 17 (12.0) | <0.001 |
| Great saphenous vein use (%) | 497 (89.4) | 106 (74.6) | <0.001 |
| Plus–minus values are means ± Standard Deviation | |||
| Table 3 | |||
| MECC (n = 555) | Off-pump (n = 142) | p-value | |
| Atrial fibrillation or Atrial flatter (%) | 110 (19.8) | 26 (18.3) | 0.812 |
| Postoperative renal insufficiency (%) | 24 (4.3) | 5 (3.5) | 0.816 |
| Stay an ICU (days) | 2.76 ± 2.79 | 2.04 ± 2.63 | <0.001 |
| Stroke (included PRIND) (%) | 9 (1.6) | 1 (0.7) | 0.696 |
| Mortality 30 days (%) | 12 (2.2) | 3 (2.1) | 1.000 |
| Plus–minus values are means ± Standard Deviation | |||
Avoiding ECC in coronary surgery is an ongoing process based on studies underlying potential side-effects of this technique [9]. Though Berdajs et al. could show acceptable results even in octogenarians with impaired left ventricular function, alternative methods have been developed to minimise trauma to the patient [10]. The most radical approach is the beating heart OPCABG revascularisation which provides a more physiologic state during surgery with convincing outcome. However, this technique has its impediments and thus a widespread use could not been accomplished during the last two decades. The introduction of MECC it was thought to combine the advantages of both pre-existing techniques: to reduce the negative impact of extensive extracorporeal circulation and to safely and entirely sustain the ischemic heart.
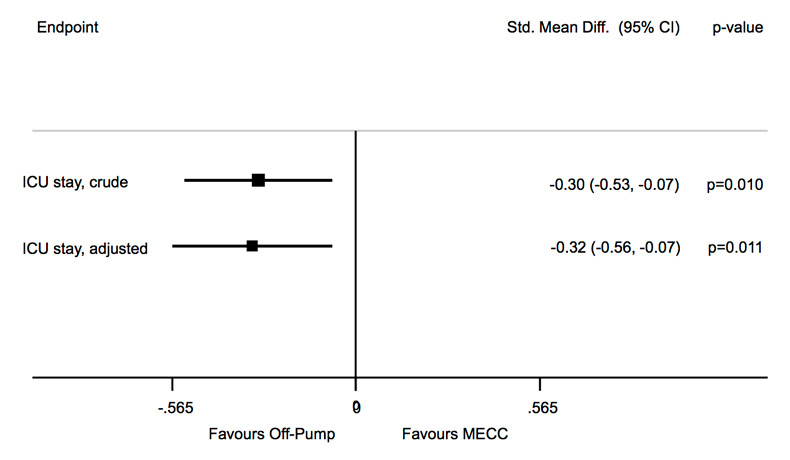
Figure 5
Forest plot comparing length of stay on the ICU.
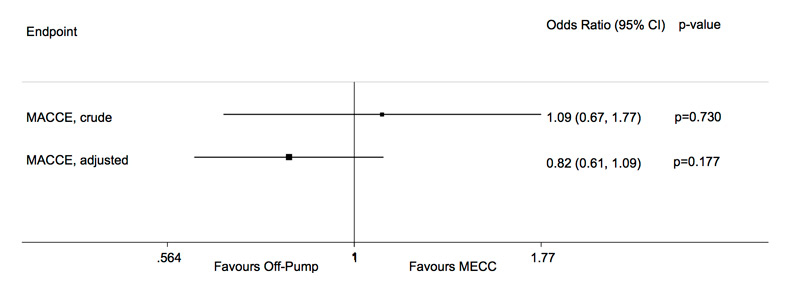
Figure 6
Forest plot regarding secondary endpoint MACCE.
At our institution, OPCABG and MECC revascularisation are routine procedures for bypass surgery. To gain a better understanding of the clinical impact of both techniques, we analysed our data including 697 patients. To our surprise, both techniques show comparable outcome data except for need for blood transfusion and length of stay on the intensive care unit.
Concerning our primary endpoint TrT as well as secondary serological endpoints CK and CK-MB, there was no significant difference between the two groups neither in the crude nor in the multivariate analysis. As depicted in figures 2–4 a mere trend towards limited myocardial damage in OPCABG revascularisation could be shown. This was in accordance to previously published data indicating less myocardial trauma in beating heart surgery [3].
Perioperative blood transfusion was significantly higher in the MECC cohort despite the fact that the inflammatory response is minimised in MECC and haemodilution is low due to the reduced priming volume with crystalloid solutions [5, 11]. There is an ongoing effort to further decrease interactions between blood and artificial surfaces resulting in less activation [12]. However, since there are no blood- material or blood-air interactions in OPCABG, mechanical trauma to blood cells as well as the activation of the inflammatory cascade is close to nil and SIRS is rarely caused [13].
Reduced blood transfusion may result in lower transfusion accidents, lower infection rate and reduced costs [14]. Re-exploration for bleeding was rare in both groups. Length of stay on the ICU was significantly shorter in patients operated off-pump, mainly because of faster transfer to the ward due to higher vigilance after extubation. Indeed there are several publications indicating reduced cognitive limitations after OPCABG [15]. A lower rate of HITS (High Intensity Transcranial Doppler Signals), expressing less microemboli, is supposed to be causative.
However, severe neurological complications, such as stroke or PRIND, did not differ significantly between the two groups. There was a mere trend towards less neurological events in OPCABG. Though there is no aortic cannulation in OPCABG, proximal vein-to-aorta anastomoses are performed with either side-clamping or the use of devices (e.g. Heart String, Maquet, Rastatt, Germany). In a recent review Polomsky pointed out that these aortic manipulations in off-pump surgery appear to be causal for apparent neurological complications [16]. Beside this, intraoperative haemodynamic stability, often compromised during tilting of the heart to graft the circumflex area, is mandatory for good neurological outcome [17].
There is an ongoing debate concerning completeness of revascularisation in OPCAB surgery. The number of grafts differed significantly between the two groups with higher numbers in the MECC group. However, completeness of revascularisation is not dependent on number of grafts performed but the number of grafts needed. This fact has been pointed out in a recently published analysis by Magee et al. [18]. The authors could show in 945 patients that the amount of grafts needed was significantly less in OPCABG compared to conventional ECC. A total of 2.95 grafts in OPCAB and 3.36 grafts in conventional CABG were performed. We grafted 3.24 coronaries in OPCAB and 3.79 in MECC, significantly more than indicated. Furthermore it has to be considered, that 15 (10.56%) of the 142 patients undergoing OPCABG were operated via thoracotomy (MIDCAB) with a mere LIMA graft to the LAD. Calculation excluding these 15 patients increases the number of distal grafts in OPCAB from 3.24 to 3.5. Compared to 3.79 in the MECC group it remains statistically significant however with a questionable effect on clinical outcome. Concerning the need for repeated revascularisation Hannan and co-workers stated a significantly higher risk for redo in OPCABG. However our data showed that re-exploration for graft failure was 1.4% (n = 8) in MECC and 0% (n = 0) in OPCABG [19].
We retrospectively analysed 697 patients undergoing CABG off-pump or MECC assisted. We could not show a significant benefit of the off-pump procedure compared to MECC in terms of the primary endpoints. However, patients undergoing OPCABG had less need for intra-operative blood products and a shorter length of stay on the ICU. Thus we conclude that both techniques have their eligibility in the surgical treatment of coronary artery disease. CABG with MECC seems to be applicable for a wider range of patients, whereas OPCAB probably has its advantages in high-risk subgroups. Further investigations are ongoing to define these subgroups and to show the significance of the MECC-system in the stratification of surgical treatment of coronary heart disease.
This was a retrospective study from a single centre. Due to its design it is at risk of bias compared to a more robust design such as a randomised controlled trial. Therapy allocation was not randomised but based on clinical assessment. A total of 144 patients were excluded due to myocardial infarction less than 7 days prior to the operation.
OPCABG is a more demanding technique and consequently more often performed by an experienced surgeon. On the other hand MECC assisted revascularisation is the first choice for training purposes and thus more often performed by inexperienced surgeons.
Despite the relatively large number of patients in this study the statistical power might not be sufficient overall. Thus for certain variables (e.g. neurologic complications) only propensities could be calculated and observed.
1 Gundry SR, Romano MA, Shattuck OH, Razzouk AJ, Bailey LL. Seven-year follow-up of coronary artery bypasses performed with and without cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1998;115(6):1273–7.
2 Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med. 2012;366(16):1489–97.
3 Puehler T, Haneya A, Philipp A, Wiebe K, Keyser A, Rupprecht L, et al. Minimal extracorporeal circulation: an alternative for on-pump and off-pump coronary revascularization. Ann Thorac Surg. 2009;87(3):766–72.
4 van Boven WJ, Gerritsen WB, Waanders FG, Haas FJ, Aarts LP. Mini extracorporeal circuit for coronary artery bypass grafting: initial clinical and biochemical results: a comparison with conventional and off-pump coronary artery bypass grafts concerning global oxidative stress and alveolar function. Perfusion. 2004;19(4):239–46.
5 Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El SN, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832–6.
6 Puehler T, Haneya A, Philipp A, Zausig YA, Kobuch R, Diez C, et al. Minimized extracorporeal circulation system in coronary artery bypass surgery: a 10-year single-center experience with 2243 patients. Eur J Cardiothorac Surg. 2011;39(4):459–64.
7 Fromm RE, Jr. Cardiac troponins in the intensive care unit: common causes of increased levels and interpretation. Crit Care Med. 2007;35(2):584–8.
8 Kolh P, Wijns W, Danchin N, Di MC, Falk V, Folliguet T, et al. Guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2010;38(Suppl):S1–S52.
9 Yuruk K, Bezemer R, Euser M, Milstein DM, de Geus HH, Scholten EW, et al. The effects of conventional extracorporeal circulation versus miniaturized extracorporeal circulation on microcirculation during cardiopulmonary bypass-assisted coronary artery bypass graft surgery. Interact Cardiovasc Thorac Surg. 2012;15(3):364–70.
10 Berdajs D, Marinakis S, Kessler U, Muradbegovic M, Ferrari E, von Segesser LK. Impaired left ventricular function as a predictive factor for mid-term survival in octogenarians after primary coronary artery bypass surgery. Swiss Med Wkly. 2012;142:w13704.
11 Immer FF, Ackermann A, Gygax E, Stalder M, Englberger L, Eckstein FS, et al. Minimal extracorporeal circulation is a promising technique for coronary artery bypass grafting. Ann Thorac Surg. 2007;84(5):1515–20.
12 Wiesenack C, Liebold A, Philipp A, Ritzka M, Koppenberg J, Birnbaum DE, et al. Four years' experience with a miniaturized extracorporeal circulation system and its influence on clinical outcome. Artif Organs. 2004;28(12):1082–8.
13 Hsu RB, Lin CH. Surgical Proficiency and Quality Indicators in Off-Pump Coronary Artery Bypass. Ann Thorac Surg. 2013 Sep 12.
14 Puskas JD, Thourani VH, Kilgo P, Cooper W, Vassiliades T, Vega JD, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann Thorac Surg. 2009;88(4):1142–7.
15 Diegeler A, Hirsch R, Schneider F, Schilling LO, Falk V, Rauch T, et al. Neuromonitoring and neurocognitive outcome in off-pump versus conventional coronary bypass operation. Ann Thorac Surg. 2000;69(4):1162–6.
16 Polomsky M, Puskas JD. Off-pump coronary artery bypass grafting – the current state. Circ J. 2012;76(4):784–90.
17 Lemma MG, Coscioni E, Tritto FP, Centofanti P, Fondacone C, Salica A, et al. On-pump versus off-pump coronary artery bypass surgery in high-risk patients: operative results of a prospective randomized trial (on-off study). J Thorac Cardiovasc Surg. 2012;143(3):625–31.
18 Magee MJ, Hebert E, Herbert MA, Prince SL, Dewey TM, Culica DV, et al. Fewer grafts performed in off-pump bypass surgery: patient selection or incomplete revascularization? Ann Thorac Surg. 2009;87(4):1113–8.
19 Hannan EL, Wu C, Smith CR, Higgins RS, Carlson RE, Culliford AT, et al. Off-pump versus on-pump coronary artery bypass graft surgery: differences in short-term outcomes and in long-term mortality and need for subsequent revascularization. Circulation. 2007;116(10):1145–52.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.