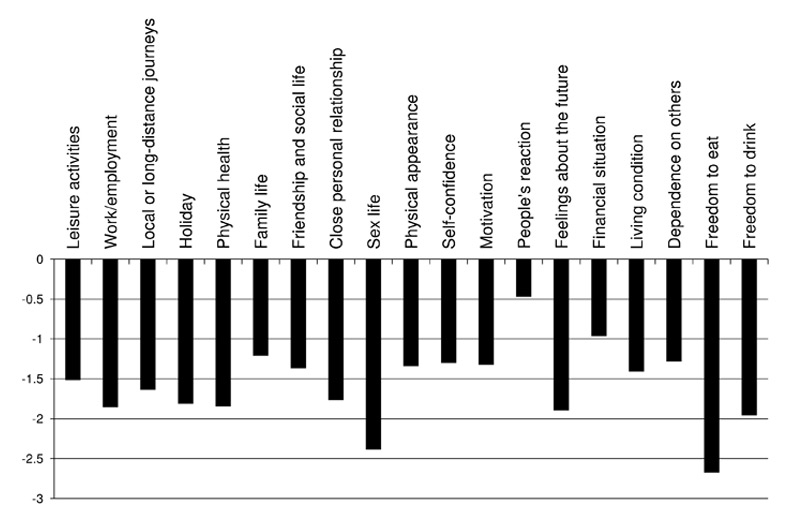
Figure 1
Average weighted impact score of the 19 domains of the ADDQoL.
ADDQoL = Audit of Diabetes-Dependent Quality of Life
DOI: https://doi.org/10.4414/smw.2014.13951
Worldwide more than 370 million people had diabetes in 2012 [1]. Its occurrence continues to increase, with debilitating clinical consequences [2, 3]. Despite a universal healthcare system, Switzerland is not protected against this upward trend. The overall prevalence of diabetes in Switzerland was reported to be 6.1% in 2010 [4] and 6.6% in 2006 in the canton of Vaud, Switzerland [5]. However, only scarce data are available regarding patient characteristics and the quality of their care [6]. Indeed, previous Swiss data showed that there was room for improvement regarding diabetes care and adherence to diabetes guidelines [7–9]. Although diabetes-specific processes-of-care were not so often performed by primary care physicians (two-thirds of patients had had annual eye and foot screening, 50% had had annual renal assessment) [8], this was somewhat better than initially measured [7].
Population-based studies are essential when studying chronic diseases, as they can offer an overall understanding about the trends in the prevalence of diabetes and the state of diabetes care in specific settings [10]. These studies help providers and public health advocates better to explain the current challenges of communities living with diabetes, and to tailor successfully supportive interventions [11]. In the past, population-based studies on diabetes had primarily focused on sociodemographic factors, medical outcomes, health services and quality-of-care indicators [12–14]. Now, there is a growing interest in using patient-reported outcome measures [15], with emphasis on patient-reported health status, health-related quality of life (HRQoL) and self-management [1, 16]. These latter measures are increasingly important as we now know that patients actively involved in their care are more engaged, better informed and benefit from improved health outcomes [17]. Indeed, patients who express higher HRQoL function better within the healthcare system and perform more health-promoting activities [18, 19]. Towards this goal, patient-reported outcomes, in combination with other quality-of-care indicators, are necessary for healthcare systems to better understand and meet the needs of patients [10].
In 2010, based on the Chronic Care Model, the Public Health department of the canton of Vaud created a pioneer programme in Switzerland, the “Programme cantonal Diabète”, to reduce the impact of diabetes on the population, specifically by (1.) acting on prevention, and (2.) improving care for people living with diabetes [20]. In this paper, we aimed to present a comprehensive picture of the health and care of a population-based sample of patients with diabetes. More specifically, we wanted to consider not only the self-report of usually considered primary processes and outcomes of care (e.g., HbA1c, HRQoL), but also of other daily life outcomes of importance to the patients such as health status, health behaviours, diabetes education, self-management support and self-efficacy. These data will represent the baseline measures of CoDiab-VD, a population-based cohort study on diabetes care in the canton of Vaud, Switzerland.
We conducted a paper-based survey with recruitment in two waves (autumn of 2011 and summer of 2012). Patients with diabetes, consecutively recruited through community-based pharmacies in the canton of Vaud, were invited to participate if they visited an included pharmacy with a prescription for diabetes-related treatment and/or equipment (oral antidiabetic medications, insulin, glycaemic strips or glucose meter). Eligible participants were noninstitutionalised adult (aged ≥18 years) patients with a diabetes diagnosis for at least 1 year and residing in that canton. Women with gestational diabetes, people with obvious cognitive impairment, or people not sufficiently fluent in French were excluded from the survey. Pharmacists checked patients’ eligibility and then briefly presented the study; patients who agreed to receive the questionnaire package (information letter, questionnaire, prepaid reply envelope) were asked to complete it at home and to send it back to the investigators. The total number of eligible participants and the characteristics of nonparticipating patients were not recorded by pharmacists because of time and organisation constraints. The recruitment was conducted without follow-up recall [21]. Sample size was based on estimates of good precision (i.e., confidence interval width) around the following primary outcomes: mean glycosylated haemoglobin (HbA1c), mean Physical and Mental component scores (PCS and MCS) of the Short Form-12 Health Survey (SF-12), Patient Assessment of Chronic Illness Care (PACIC) global score, and percentage of patients receiving recommended annual processes-of-care. Given pharmacy clusters (40 pharmacies, each recruiting 15 patients, intraclass correlation 0.05, alpha 0.05, beta 0.2), 600 participants were targeted.
The protocol of this study was approved by the Cantonal Ethics Committee of Research on Human Beings of the Canton of Vaud (Protocol N° 151/11). Written informed consent was obtained from all participants, and data were kept anonymous and confidential.
Participants completed a self-administered paper questionnaire. Primary outcomes of interest were recommended processes and outcomes of care indicators. The processes-of-care indicators considered were: HbA1c check among patients who were aware of what HbA1c is (“HbA1c-aware”), blood pressure measurement, weight measurement, lipid profile, annual diabetic foot examination, annual urine test for microalbuminuria, annual eye examination by ophthalmologist, seasonal influenza vaccination, physical activity and diet recommendations. Outcomes of care were: mean HbA1c among HbA1c-aware patients, generic and diabetes-specific HRQoL measures (SF-12 PCS and MCS, score range 0 = worst to 100 = best; Audit of Diabetes-Dependent Quality of Life 19 – ADDQoL, range –9 = maximum negative impact of diabetes to +3 = maximum positive impact of diabetes), and congruency of care with the Chronic Care Model (PACIC score, range 1 = lowest to 5 = highest congruency). We also considered the following diabetes education, self-management support and self-efficacy measures: glucose self-monitoring, HbA1c knowledge, participation in diabetes education course, membership in the local diabetes association (Association Vaudoise du Diabète – AVD), knowledge about the “Diabetes Passport” (a small booklet, kept by the patient, in which consultations and medical results are noted), easiness-difficulty with daily self-management of diabetes in general, with physical activity, medication and diet, as well as their level of information about diabetes and source of information, support and satisfaction with healthcare team and personal social network. Other data included age, gender, sociodemographics (relationship status, living situation, family income in Swiss franc (CHF/month), education, employment status, type of residence, nationality), and diabetes characteristics (type, duration, treatment, complications), health behaviours (smoking status, alcohol consumption, physical activity), and comorbidities.
Descriptive analyses were conducted, with data reported as means or percentages for continuous or categorical variables, respectively. For primary outcomes, confidence intervals were also calculated, taking into account the hierarchical structure of the data (clusters of pharmacies). All analyses were performed using Stata 12.1.
| Table 1:Baseline characteristics of the participants (n = 519 patients with diabetes). | ||
| Sociodemographic and general health characteristics | ||
| Mean age (SD; range) (n = 519) | 64.5 (11.3; 19–91) | |
| Female (n = 519) | 40.3% | |
| Marital status (n = 516) | Single | 8.3% |
| Married or living with partner | 63.8% | |
| Separated, divorced, widowed | 27.9% | |
| Education (n = 504) | Primary | 18.9% |
| Secondary | 56.2% | |
| Tertiary | 25.0% | |
| Employment status (n = 503) | Employed (full time) | 23.7% |
| Employed (part time) | 8.4% | |
| Unemployed or disabled | 6.2% | |
| Not in labour force* | 61.8% | |
| Quartiles of family income (n = 486) | ≤3,499 CHF/month | 21.2% |
| 3,500–5,499 CHF/month | 26.5% | |
| 5,500–9,499 CHF/month | 27.8% | |
| ≥9,500 CHF/month | 17.3% | |
| Unknown | 7.2% | |
| Total number of people in household (n = 516) | 1 (lived alone) | 26.7% |
| 2 | 55.0% | |
| ≥3 | 18.2% | |
| Place of residence (n = 509) | Urban | 42.6% |
| Semiurban | 27.5% | |
| Rural | 29.9% | |
| Nationality (n = 515) | Swiss | 88.2% |
| Other | 11.9% | |
| Self-reported health (n = 509) | Excellent / very good | 14.2% |
| Good | 64.2% | |
| Medium/poor | 21.6% | |
| Diabetes | ||
| Type of diabetes (n = 519) | Type 1 | 12.7% |
| Type 2 | 66.9% | |
| Undetermined | 20.4% | |
| Duration of known diabetes (n = 511) | ≤10 years | 52.1% |
| >10 years | 47.9% | |
| Treatment for diabetes (n = 517) | Oral antidiabetic drugs (OAD) | 50.7% |
| Insulin | 21.7% | |
| OAD and insulin | 27.1% | |
| None/unknown | 0.6% | |
| Diabetes-related complication† (n = 505) | None | 52.5% |
| 1 | 30.7% | |
| ≥2 | 16.8% | |
| Comorbidity‡ (n = 505) | None | 17.4% |
| 1 | 26.9% | |
| ≥2 | 55.6% | |
| Current smoking (n = 509) | 17.3% | |
| High-risk drinking§ (n = 484) | 48.4% | |
| BMI (n = 481) | Overweight (BMI 25–29.9) | 35.3% |
| Obese (BMI ≥30) | 46.8% | |
| Physically inactive (n = 494) | 29.8% | |
| BMI = body mass index; CHF = Swiss franc; SD = standard deviation * Not in labour force encompassed retired, annuitant and stay-at-home. † List of diabetes related-complications: myocardial infarction/angina, stroke, retinopathy, nephropathy, neuropathy, severe hypo- or hyperglycaemia. ‡ List of co-morbidities: heart failure, valvulopathy, hypertension, hyperlipidaemia, chronic respiratory conditions, peptic ulcer, osteoporosis, osteoarthritis, Parkinson's disease, malignancy, depression, other chronic condition. § High risk drinking: AUDIT-C (Alcohol Use Disorders and Identification Test-Consumption) men ≥4, women ≥3. | ||
Out of 1,054 eligible people who accepted a questionnaire from pharmacists (809 in 2011, 245 in 2012), 519 patients completed and returned the questionnaire (406 in 2011, 113 in 2012, participation rate of 50.2% and 46.1%, respectively). Table 1 shows participants’ characteristics. The majority were male (59.7%) and mean age was 64.5 years. Most reported a diagnosis of type 2 diabetes (66.9%), and 48% of respondents had been diagnosed over 10 years ago. Although less than 20% of patients reported being current smokers, almost 50% presented high-risk drinking behaviour, more than 80% were either obese or overweight, and 30% were considered to be inactive physically.
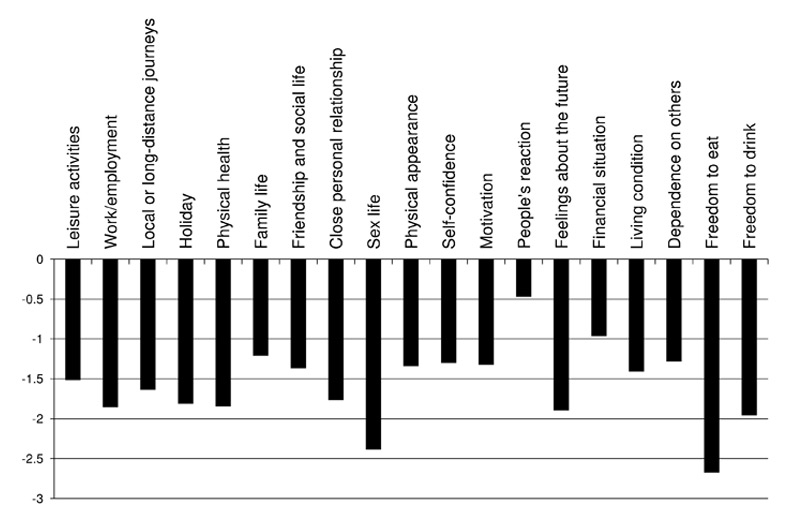
Figure 1
Average weighted impact score of the 19 domains of the ADDQoL.
ADDQoL = Audit of Diabetes-Dependent Quality of Life

Figure 2
Self-management support. A. Knowledge and information. B. “Self-efficacy” measures. C. Social support and satisfaction about it.
AVD = Association Vaudoise du Diabète; HbA1c = glycosylated haemoglobin
Blood pressure, weight, and lipid profile were measured in over 90% of participants in the prior 12 months (table 2). HbA1c was checked at least once in the last year in 98.3% of HbA1c-aware patients (n = 282). Other processes-of-care indicators were reported by less than 70% of the patients. Low percentages were also found for physical activity and diet recommendations. Among HbA1c-aware patients, mean patients-reported HbA1c was 7.3% (n = 177). Whereas generic health-related quality of life results showed worse physical than mental health (SF-12 PCS: 43.4, SF-12 MCS: 47.0), disease-specific HRQoL showed that patients reported being most affected by limitations in their daily life regarding “freedom to eat”, “sex life”, and “freedom to drink”, while “people’s reaction” and “financial situation” mattered least (fig. 1). Mean patient assessment of chronic illness care (PACIC) score was 2.8 (1 = lowest to 5 = highest congruency).
Home glucose self-monitoring was frequently used (81.6%) (fig. 2A), but HbA1c knowledge (58.3%) and participation in a diabetes education course (32.8%) were rather low. Only 14.3% were members of the local diabetes association and 18.4% knew about the “Diabetes Passport”. Measures of “self-efficacy” showed that diet posed a greater difficulty when compared with daily general diabetes management (fig. 2B). In addition, the majority of patients felt well- to very well-informed about their chronic disease (85.9%), with the major provider of information being their medical doctors (92%). Other sources of information were media (30.8%), other healthcare professionals (23.5%), social network (8.6%), association or healthcare network (5.7%), alternate sources (3.9%) and none (1.8%). Finally, 67% of the participants were well- or very-well satisfied about their care, and nearly 58% would definitely recommend the care received (fig. 2C). Most were satisfied by the support obtained from their healthcare team (72.6%) and members of their social network (72.3%).
| Table 2:Patient-reported primary outcomes. | |||
| Processes-of-care indicators within the prior 12 months: | Percentage | 95% CI | |
| HbA1c check among HbA1c aware patients | (n = 282) | ||
| 1x | 14.7% | 10.8%–19.8% | |
| ≥2x | 83.6% | 78.2%–87.9% | |
| None | 1.1% | 0.4%–3.1% | |
| Do not know | 0.8% | 0.2%–2.7% | |
| Blood pressure measurement | (n = 509) | ||
| 1x | 12.6% | 9.8%–16.1% | |
| 2–3x | 41.7% | 37.2%–46.3% | |
| ≥4x | 43.4% | 39.0%–47.9% | |
| None | 1.8% | 1.1%–3.1% | |
| Do not know | 0.9% | 0.4%–2.1% | |
| Weight measurement | (n = 507) | ||
| Yes | 93.4% | 90.5%–95.4% | |
| No | 6.2% | 4.3%–9.0% | |
| Do not know | 0.4% | 0.1%–1.5% | |
| Lipid profile | (n = 513) | ||
| Yes | 94.1% | 91.8%–95.7% | |
| No | 3.2% | 2.1%–5.1% | |
| Do not know | 2.4% | 1.3%–4.3% | |
| Diabetic foot examination by a physician | (n = 510) | ||
| Yes | 67.2% | 62.1%–71.9% | |
| No | 31.8% | 27.0%–37.0% | |
| Do not know | 0.8% | 0.3%–2.5% | |
| Urine test (for microalbuminuria) | (n = 512) | ||
| Yes | 64.5% | 59.1%–69.6% | |
| No | 21.6% | 18.0%–25.6% | |
| Do not know | 14.6% | 11.3%–18.6% | |
| Influenza vaccination | (n = 514) | ||
| Yes | 63.5% | 59.8%–66.9% | |
| No | 36.4% | 33.0%–40.0% | |
| Do not know | 0.2% | 0.0%–1.4% | |
| Eye assessment by ophthalmologist | (n = 511) | ||
| <1 year | 58.2% | 53.8%–62.5% | |
| 1–2 years | 17.9% | 15.1%–21.1% | |
| >2 years | 12.5% | 9.6%–16.1% | |
| Never | 9.5% | 7.3%–12.3% | |
| Do not know | 1.5% | 0.7%–3.3% | |
| Physical activity recommendations, written or verbal* | (n = 509) | ||
| Yes | 67.9% | 65.5%–70.2% | |
| No | 32.7% | 31.2%–34.3% | |
| Do not know | 0.4% | 0.1%–1.5% | |
| Diet recommendations, written or verbal* | (n = 510) | ||
| Yes | 49.0% | 44.2%–53.9% | |
| No | 50.6% | 45.8%–55.4% | |
| Do not know | 0.4% | 0.1%–1.5% | |
| Outcomes of care: | Mean | 95% CI | |
| HbA1c value among HbA1c -aware patients (%) | (n = 177) | 7.3 | 7.1–7.5 |
| Health-related quality of life | |||
| SF-12 PCS | (n = 498) | 43.4 | 42.3–44.4 |
| SF-12 MCS | (n = 496) | 47.0 | 46.0–48.0 |
| ADDQoL global score | (n = 512) | –1.6 | –1.7 – –1.4 |
| PACIC global score | (n = 503) | 2.8 | 2.7–2.9 |
| ADDQoL = Audit of Diabetes Dependent Quality of Life questionnaire; CI = confidence interval; MCS = Mental Component Score; PACIC = Patient Assessment of Chronic Illness Care questionnaire; PCS = Physical Component Scor; SF-12 = Short Form-12. * Without time frame | |||
In this survey, we comprehensively described the care of a cohort of 519 patients with diabetes in the canton of Vaud, Switzerland. Our results signalled that quality gaps remained, especially for certain diabetes-specific quality indicators. We also noted a disconnection between patients’ perceptions and their actual disease knowledge and care; indeed, patients felt satisfyingly informed about diabetes, but yet many reported not even knowing what HbA1c meant. Although satisfaction with and support from healthcare providers were rated high and the majority of participants would recommend their healthcare, recommendations about physical activity and diet were well below goal. This is doubly significant as patients expressed their greatest management difficulties in these areas.
The percentage of patients reporting uncontrolled diabetes (5.7%), defined by a HbA1c over 9%, as well as the percentage of patients with HbA1c level below 8% (73%), were below and above, respectively, the 15% and 60% cut-off recommended by the Swiss society of endocrinology and diabetology (E. Christ, personal communication). The mean self-reported HbA1c value was good (7.3%), but only available for the 177 HbA1c-aware patients. Mean HbA1c levels for the whole sample would probably be less satisfactory.
Generic HRQoL results showed that patients reported better MCS than PCS scores; this is similar to previous population-based studies on diabetes using the SF-12 scoring [22, 23]. Diabetes-specific HRQoL measures (ADDQoL) showed that “freedom to eat” was a quality-of-life domain where patients felt particularly affected. This difficulty, also reported by Collins et al. [24], echoed the fact that patients reported more difficulties when it came to the management not only of diet but also of physical activity. These findings point to the need for more emphasis on guiding patients on these topics since patients reported few recommendations regarding both diet and physical activity. Increased participation in diabetes education programmes and diabetes association could be a targeted way to address these needs since higher levels of self-management and self-efficacy have been shown to have a positive impact on diabetes-related outcomes such as HbA1c [25]. Another way to improve patient’ knowledge, attitudes and behaviour about nutrition could be to increase physicians’ referral to dieticians and specialised nurses. This would be particularly appropriate since our participants reported unsatisfactory health behaviours (i.e., smoking, drinking and physical activity status), and under-utilisation of such resources was previously described in that population [26].
Even though both satisfaction and support from healthcare providers were globally well ranked, and about 60% of the patients would definitely recommend their healthcare, few participants were informed about the canton’s diabetes association, programme or activities that could help improve their empowerment. This should be improved since we know that patients who receive more support from their social network or healthcare providers possess more self-management skills and self-efficacy regarding their diabetes, and feel more confident about their ability to complete health-promoting activities [27, 28]. Planning activities for patients with diabetes is important. All healthcare providers should be involved in promoting these resources to patients.
The collection of a broad range of outcomes and measures is an added value of this study. However, some limitations must be taken into consideration. First, these results are based on patients’ self-report which may be prone to recall bias. However, supplementary analyses demonstrated good correlation between patient-reported data and physician records for simple processes-of-care, when data was supplied by the treating physician for a fraction of the cohort (H. Collet, personal communication); in addition, these results were similar to those of other population-based studies [29]. Also, despite the possibility of under- or over-estimation of self-report indicators of care, patient-reported outcomes are important measures to consider when evaluating the health status of a population and its needs regarding healthcare [15]. Second, 519 patients were recruited in the study instead of the 600 targeted. As we had more clusters (pharmacies) than expected, and because of our conservative sample size calculations, the precision around point estimates was nevertheless acceptable. Finally, our results may not be generalisable to the whole population of patients with diabetes in the canton of Vaud, as only patients fluent enough in French to fill in a questionnaire, and with a diagnosis of diabetes for over a year and visiting a pharmacy, were recruited. We cannot exclude that results might have been different with the inclusion of patients speaking foreign languages such as migrants or highly-skilled and educated English-speaking expatriate workers. However, the direction and size of the effect of a broader inclusion of patients may not be so straightforward to apprehend. Also, participants showed similar characteristics in terms of age, gender, education and BMI than those from prior studies in the same canton [6, 30]. In addition, they represent a population-based sample of patients with diabetes more closely than participants recruited in hospitals [9].
These findings will be useful for the further development and evaluation of the “Programme cantonal Diabète”. They are particularly interesting since they constitute the baseline data of the cohort of patients with diabetes in the canton of Vaud (CoDiab-VD). On a more global level, these results shall support institutional strategies to close knowledge gaps for patients with diabetes. More specifically, they should ensure that all processes-of-care are received by patients – especially those specific to diabetes care, and that diabetes education programmes are promoted and made accessible to all patients. A special emphasis should be given to diet and physical activity education and support. As this study covered a wide spectrum of quality of care indicators, these results should be of interest to healthcare stakeholders seeking to improve care for patients with diabetes both in Switzerland and elsewhere.
Acknowledgments: We would like to thank all pharmacies, patients with diabetes and practicing physicians who participated in the study. We also thank the partners and members of the working groups for their collaboration.
1 Smith KJ, Page V, Gariepy G, Beland M, Badawi G, Schmitz N. Self-rated diabetes control in a Canadian population with type 2 diabetes: associations with health behaviours and outcomes. Diabetes Res Clin Pract. 2012;95(1):162–8.
2 Grandy S, Fox KM. Change in health status (EQ-5D) over 5 years among individuals with and without type 2 diabetes mellitus in the SHIELD longitudinal study. Health Qual Life Outcomes. 2012;10(1):99.
3 Glasgow RE. Tackling the hard problems: long-term maintenance. Curr Diab Rep. 2005;5(2):113.
4 Rey A, Thoenes M, Fimmers R, Meier CA, Bramlage P. Diabetes prevalence and metabolic risk profile in an unselected population visiting pharmacies in Switzerland. Vasc Health Risk Manag. 2012;8:541–7.
5 Firmann M, Mayor V, Vidal PM, Bochud M, Pecoud A, Hayoz D, et al. The CoLaus study: a population-based study to investigate the epidemiology and genetic determinants of cardiovascular risk factors and metabolic syndrome. BMC cardiovascular disorders. 2008;8:6.
6 Sebo P, Abetel G, Stalder H, Bovier PA. Importance of lifestyle counselling by primary care physicians for diabetic patients. Swiss Med Wkly. 2006;136(35–36):566–73.
7 Groupe de travail de la Fondation de l’Association Suisse du Diabète: La déclaration de St. Vincent: une enquête sur la prise en charge des diabétiques en Suisse. Bull Med Suisse. 1996;15:628–35.
8 Bovier PA, Sebo P, Abetel G, George F, Stalder H. Adherence to recommended standards of diabetes care by Swiss primary care physicians. Swiss Med Wkly. 2007;137(11–12):173–81.
9 Burgmann K, Fatio SA, Jordi B, Rutishauser J. Medical care of type 2 diabetes mellitus in light of international and national recommendations: a retrospective analysis. Swiss Med Wkly. 2013;143:w13871.
10 Donald M, Dower J, Ware R, Mukandi B, Parekh S, Bain C. Living with diabetes: rationale, study design and baseline characteristics for an Australian prospective cohort study. BMC Public Health. 2012;12:8.
11 Griffiths F, Anto N, Chow E, Manazar U, Van Royen P, Bastiaens H. Understanding the diversity and dynamics of living with diabetes: a feasibility study focusing on the case. Chronic Illn. 2007;3(1):29–45.
12 McClain MR, Wennberg DE, Sherwin RW, Steinmann WC, Rice JC. Trends in the diabetes quality improvement project measures in Maine from 1994 to 1999. Diabetes care. 2003;26(3):597–601.
13 Price JF, Reynolds RM, Mitchell RJ, Williamson RM, Fowkes FGR, Deary IJ, et al. The Edinburgh Type 2 Diabetes Study: study protocol. BMC Endocr Disord. 2008;8:18.
14 Thompson W, Wang H, Xie M, Kolassa J, Rajan M, Tseng CL, et al. Assessing quality of diabetes care by measuring longitudinal changes in hemoglobin A1c in the Veterans Health Administration. Health services research. 2005;40(6 Pt 1):1818–35.
15 Gibbons E, Fitzpatrick R. A structured review of patient-reported outcome measures for people with diabetes: an update 2009. Oxford; 2009.
16 Rubin RR, Peyrot M, Siminerio LM. Health care and patient-reported outcomes: results of the cross-national Diabetes Attitudes, Wishes and Needs (DAWN) study. Diabetes care. 2006;29(6):1249–55.
17 Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health affairs. 2013;32(2):207–14.
18 Rubin RR, Peyrot M. Quality of Life and Diabetes. Diabetes Metab Res Rev. 1999;15:205–18.
19 Wexler DJ, Grant RW, Wittenberg E, Bosch JL, Cagliero E, Delahanty L, et al. Correlates of health-related quality of life in type 2 diabetes. Diabetologia. 2006;49(7):1489–97.
20 Programme cantonal Diabète. 2013 [cited; Available from: http://www.vd.ch/themes/sante-social/prevention/le-diabete/programme-cantonal/
21 Peytremann-Bridevaux I, Bordet J, Santschi V, Collet TH, Eggli M, Burnand B. Community-based pharmacies: an opportunity to recruit patients? Int J Public Health. 2012 Jul 1.
22 Bourdel-Marchasson I, Druet C, Helmer C, Eschwege E, Lecomte P, Le-Goff M, et al. Correlates of health-related quality of life in French people with type 2 diabetes. Diabetes Res Clin Pract. 2013 Jul 4.
23 Grandy S, Chapman RH, Fox KM, Group SS. Quality of life and depression of people living with type 2 diabetes mellitus and those at low and high risk for type 2 diabetes: findings from the Study to Help Improve Early evaluation and management of risk factors Leading to Diabetes (SHIELD). Int J Clin Pract. 2008;62(4):562–8.
24 Collins M. Quality of life and quality of care in patients with diabetes experiencing different models of care. Diabetes Care. 2009;32(4):603–5.
25 Strychar I, Elisha B, Schmitz N. Type 2 Diabetes Self-Management: Role of Diet Self-Efficacy. Can J Diabetes. 2012;36(6):337–44.
26 Peytremann-Bridevaux I, Bordet J, Burnand B. Diabetes care in Switzerland: good, but perfectible: a population-based cross-sectional survey. BMC Health Serv Res. 2013;13:232.
27 Kadirvelu A, Sadasivan S, Ng SH. Social support in type II diabetes care: a case of too little, too late. Diabetes, metabolic syndrome and obesity: targets and therapy. 2012;5:407–17.
28 Schiøtz ML, Bøgelund M, Almdal T, Jensen BB, Willaing I. Social support and self-management behaviour among patients with Type 2 diabetes. Diabetic Medicine. 2012;29(5):654–61.
29 Stone MA, Charpentier G, Doggen K, Kuss O, Lindblad U, Kellner C, et al. Quality of Care of People With Type 2 Diabetes in Eight European Countries: Findings from the Guideline Adherence to Enhance Care (GUIDANCE) study. Diabetes Care. 2013;36(9):2628–38.
30 Kaiser A, Vollenweider P, Waeber G, Marques-Vidal P. Prevalence, awareness and treatment of type 2 diabetes mellitus in Switzerland: the CoLaus study. Diabetic medicine: a journal of the British Diabetic Association. 2012;29(2):190–7.
Funding / potential competing interests: This project was funded by the Department of Public Health of the canton of Vaud (“Programme cantonal Diabète”). Prof. I. Peytremann-Bridevaux is supported by a grant from the Swiss National Science Foundation [PROSPER N° 32333B-123817 and N° 32333B-139789] and by the Swiss School of Public Health+ [Assistant Professorship grant].
Authors’ contribution: EZ and AC contributed equally to this work.