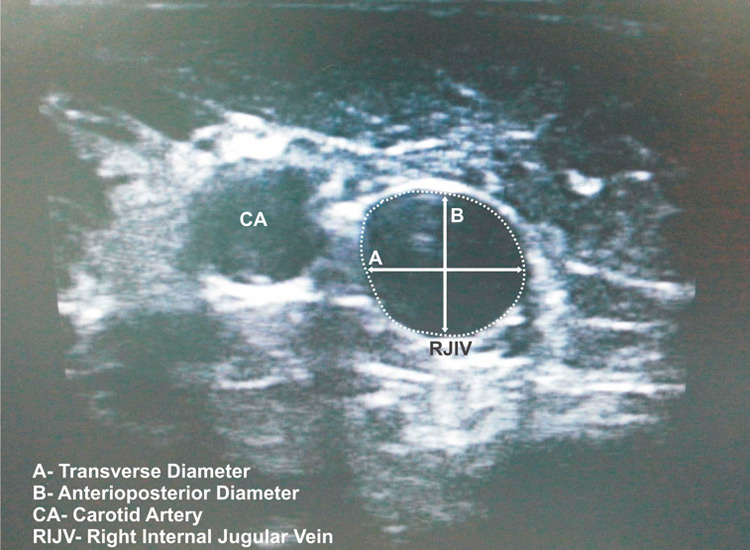
Figure 1
A still image of the RIJV, diameters and cross-sectional area.
DOI: https://doi.org/10.4414/smw.2014.13946
Central venous line placement is a common procedure used by anaesthetists in patients undergoing major surgery or in intensive care units [1, 2]. The right internal jugular vein (RIJV) is the most common route used in patients under general anaesthesia because of its easy access during the procedure and throughout the operation [1, 3]. Although the literature recommends the use of ultrasound, the blind surface anatomic landmark guided technique still predominates in clinical practice [2, 4]. However, using this method can lead to failure of puncture in 10% to 31% of attempts and arterial puncture in 5% to 9% of patients on the first attempt; thus, in total, one or more complications in 5% to 40% of all patients who have a catheterisation intervention [2, 5, 6].
Whether the ultrasound-guided or landmark-guided technique is used, the effective placement of an RIJV catheter is more challenging in patients with veins of shorter diameter or of smaller cross-sectional area (CSA) [7]. Many methods are used to increase the CSA of the RIJV such as rotation of the head, the “Valsalva” manoeuvre, hepatic compression, the Trendelenburg manoeuvre, humming, application of positive end-expiratory pressure (PEEP), or some combination of these methods [8, 9].
It is widely known that positive mechanical ventilation increases the positive intrathoracic pressure, which affects the pressure in the RIJV, resulting in an increase of the CSA [3]. Currently, there appears to be a lack of studies in the literature that assessed the effects of different modes of ventilation on this increase.
The aim of our study was to evaluate the changes in CSA and diameters of the RIJV during two different modes of mechanical ventilation (pressure-controlled ventilation [PCV] and volume-controlled ventilation [VCV]) and spontaneous ventilation with the head in a neutral position and a 30-degree rotated lateral position by use of ultrasonography, and to determine the ventilation mode that is most suitable for catheterisation.
Thirty American Society of Anesthesiologists (ASA) status I-II patients between 18 and 80 years old undergoing elective abdominal surgery under endotracheal intubation were included in this prospective, clinical study. Patients with a history of congestive heart failure, chronic obstructive pulmonary disease, pulmonary hypertension, chronic renal failure, diabetes mellitus, rheumatological diseases, neck surgery, valvular disease, body mass index over 40 or RIJV catheterisation or peak airway pressures above 20 cm H2O under mechanical ventilation were excluded from the study. Initially 45 patients were recruited for the study. Thirteen patients were excluded because of peak airway pressures above 20 cm H20. In two patients, unanticipated difficult airway was encountered and they were excluded from the study.
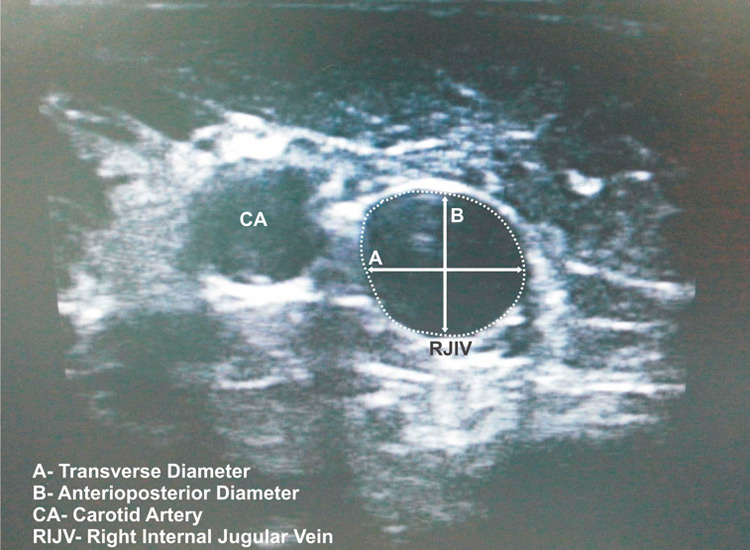
Figure 1
A still image of the RIJV, diameters and cross-sectional area.
Consent was obtained from every patient and the ethics committee approval (Ethics Committee No. 32488.9.9.2011) was provided by Istanbul University Cerrahpasa Medical School Ethics Committee, Istanbul, Turkey. The study was registered with Clinical Trials of the US National Institutes of Health (Clinicaltrials.gov NCT01790334) and conducted in accordance with the Helsinki Declaration.
All patients were given 0.02 mg/kg midazolam for (Dormicum, Deva, Turkey) for premedication intravenously in the preoperative room after a 20 G cannula was inserted on the dorsum of the left hand and an infusion of lactate ringer solution with a rate of 4 ml/kg/h was started. All patients were taken to the operating room and placed in a supine position on the operating table. The electrocardiogram (ECG) (3 leads), noninvasive blood pressure and peripheral oxygen saturation were monitored. In each patient, still ultrasound images of the vena jugularis interna were recorded in “neutral” and “neck rotated to 30 degrees to left” positions, first when under spontaneous ventilation (group S) before the induction, then after the induction of anaesthesia under volume-controlled ventilation (group V) and under pressure-controlled ventilation (group P). The six still images taken from the each patient were evaluated in terms of transverse and anteroposterior diameters and cross-sectional area.
Patients were asked to lie still in the supine position and breathe with a normal tidal volume and frequency. If any patient complained about the position or reported a problem in breathing or uneasiness before or during the measurements, the patient was excluded from the study. A single experienced anaesthetist examined the RIJV at the cricoid cartilage level with an Esaote My Lab 5 ultrasound (Esaote Europe B.V. Maastricht, Netherlands) with a LA523E probe and took still images both in a neutral position and with the neck rotated using a protractor 30 degrees to left from the midline without any pillow under the head. The neutral position is where the axis of the patient’s head is perpendicular to the plane the patient is on. The rotated position is where the axis of the head is at a 30 degree angle to the left of the plane that the patient is on. The probe was held with extreme care to minimise compression of the veins. When the best view of the RVJI was achieved with the subjective largest CSA, a still image was taken during the end of the expiration. The patients were given information about the concepts spontaneous ventilation, inspiration and expiration. They were asked to perform normal tidal volume ventilation during spontaneous ventilation. When patients fully understood the concept, they were asked to make a tidal volume inspiration and then expiration and hold breathing before inspiration.
Following the measurements under spontaneous ventilation, anaesthesia was induced with 2 mg/kg propofol (Propofol, Abbott, IL, USA) and following the start of hypnosis, 0.6 mg/kg rocuronium (Esmeron, Organon, Holland) was administered and endotracheal intubation was performed. Anaesthesia was maintained with 2% sevoflurane (Sevorane, Abbot, USA) in 40% oxygen / air mixture in 4 L fresh gas flow. Then each patient was ventilated in volume-controlled mode (VCV) (Datex Avence S5, Madison, Wisconsin, USA) to achieve tidal volumes of 8 ml/kg and end-tidal carbon dioxide (EtCO2) values between 32–36 mm Hg, under 6 cm H2O PEEP with a 1:2 inspiratory to expiratory ratio, respiratory rate between 10–12 and a flow rate of 4 l/min. Patients with peak airway pressures higher than 20 cm H2O were excluded from the study. Still images both in the neutral position and with the neck rotated were taken again using the ventilator expiratory pause function as for each patient. The pause time setting of the ventilator was used as still images were being taken. After the image was taken, the ventilation mode was changed to pressure-controlled mode (PCV) under 6 cm H2O PEEP with a 1:2 inspiratory to expiratory ratio, respiratory rate between 10–12 and a flow rate of 4 l/min and a pressure support of 12–14 cm H2O to achieve EtCO2 values between 32–36 mm Hg. In the 5th minute of the mode change, still images both in the neutral position and with the neck rotated were taken, again using the ventilator expiratory pause function as done under spontaneous and volume-controlled ventilation.
Three sets of images taken from every patient were evaluated by an anaesthetist who was not aware which group of ventilation mode the image belonged to. The CSA, transverse and anteroposterior diameters were measured using the built-in software of the ultrasound. Anteroposterior diameter is the distance between the anterior and the posterior wall of the RIJV. Transverse diameter is the distance between the medial and lateral wall of the RIJV (fig. 1).
The measurements achieved under spontaneous ventilation, VCM and PCV were grouped in group S, group V and group P, respectively.
No puncture or attempt of catheterisation was done before or after the measurements.
Statistical analysis was performed using the NCSS (Number Cruncher Statistical System) 2007 and PASS (Power Analysis and Sample Size) 2008 Statistical Software (Utah, USA). While evaluating our data, descriptive statistical methods (mean, standard deviation, median, frequency, ratio) were used, as well as a one-way analysis of variance (ANOVA) to compare quantitative parameters that display normal distribution and Tukey HSD as a post-hoc test. For parameters that did not display normal distribution, the Kruskal-Wallis test was applied. Finally, to determine which group caused the difference, the Mann-Whitney U’-test with Bonferroni correction was used. For the difference between the CSAs in different positions, the Wilcoxon test was used. The total sample of 90 subjects achieves 95% power to detect a difference of at least 10.00 using the Tukey-Kramer (Pairwise) multiple comparison test at a 0.05000 significance level. The common standard deviation within a group is assumed to be 5.00.
| Table 1:Demographic data. | |
| Age (years) | 47.6 ± 16.5 |
| Weight (kg) | 72.6 ± 13.4 |
| Height (cm) | 166.4 ± 9.0 |
| Sex (F/M) | 13/17 |
| ASA (I/II) | 23/7 |
| ASA = American Society of Anesthesiologists | |
Demographic data of the patients are shown in table 1.
In terms of transverse diameters in the head neutral position, the diameter measured in group S was significantly smaller than diameters in group P (p = 0.002) and group V (p = 0.01). No significant difference was observed between the transverse diameters in group P and group V measurements when the head was in the neutral position (table 2).
In terms of anteroposterior diameters in the head neutral position, the diameter measured in group S was significantly smaller than diameters in group P (p = 0.03) and group V (p = 0.02). No significant difference was observed between the transverse diameters in group V and group P when the head was in a neutral position (table 2).
In terms of transverse diameters in the 30 degree rotated position of the head, the diameter measured in group S was significantly smaller than those in group P (p = 0.001) and group V (p = 0.001). No significant difference was observed between the transverse diameters in group P and group V measurement when the head was in the 30 degree rotated to lateral position (table 3).
In terms of anteroposterior diameters in the 30 degree rotated to lateral position of the head, the diameter measured in group S was significantly smaller than those in group P (p = 0.006) and group V (p = 0.04). No significant difference was observed between the anteroposterior diameters in group P and group V measurements when the head was in the 30 degree rotated to lateral position (table 3).
The CSA of RIJV in head neutral position was significantly larger under both group V (p = 0.01) and group P (p = 0.001) measurements when compared with group S measurements (table 4).
The CSA of RIJV in head 30 degree lateral position were significantly higher in group V (p = 0.001) and group P (p = 0.001) measurements when compared with group S measurements (table 4).
In all three ventilation groups, no significant difference was observed in the diameters of RIJV when head was rotated to 30 degree lateral from neutral position.
The CSA of RIJV in group P measurements increased significantly (p = 0.002) when the head was rotated 30 degrees to lateral position from neutral position. No significant difference was observed in the CSA values of RIJV in group S or group V measurements when head is in a neutral or 30 degree rotated to lateral position within groups (table 4).
| Table 2: Evaluation of parameters according to study group. | |||
| Group P (n = 30) | Group S (n = 30) | Group V (n = 30) | |
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Neutral transverse (mm) | 10.5 ± 2.9 | 7.3 ± 3.5** | 10.0 ± 3.4## |
| Neutral anteroposterior (mm) | 16.2 ± 6.6 | 12.4 ± 4.5* | 15.4 ± 5.6# |
| * p <0.05, ** p <0.01 when group P compared with group S, # p <0.05, ## p <0.01 when group S compared with group V Group P: pressure-controlled ventilation Group S: spontaneous ventilation Group V: volume-controlled ventilation SD = standard deviation | |||
| Table 3: Evaluation of parameters in between group testing. | |||
| Group P (n = 30) | Group S (n = 30) | Group V (n = 30) | |
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Rotated transverse (mm) | 11.5 ± 3.7 | 7.4 ± 2.9*** | 11.0 ± 4.1### |
| Rotated anteroposterior (mm) | 16.5 ± 7.5 | 11.4 ± 3.3** | 15.3 ± 5.2# |
| ** p <0.01, *** p <0.001 when group P compared with group S, # p <0.05, ### p <0.001 when group S compared with group V Group P: pressure-controlled ventilation Group S: spontaneous ventilation Group V: volume-controlled ventilation SD = standard deviation | |||
| Table 4: Evaluation of CSA according to head position. | |||
| Group P (n = 30) | Group S (n = 30) | Group V (n = 30) | |
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Neutral CSA (mm2); | 148.9 ± 90.3 | 91.6 ± 115.5*** | 124.8 ± 83.1## |
| Rotated CSA (mm2); | 172.1 ± 115.4†† | 72.9 ± 40.2*** | 143.5 ± 79.2### |
| *** p <0.001 when group P compared with group S, ## p <0.01, ### p <0.001 when group S compared with Group V, †† p <0.01 within Group comparison Group P: pressure-controlled ventilation Group S: spontaneous ventilation Group V: volume-controlled ventilation CSA = cross-sectional area; SD = standard deviation | |||
Placement of central venous catheters with or without ultrasound has been evaluated by many studies [2, 3, 10]. Although it is well established that ultrasound-guided catheterisation decreases the complications and increases the success rate, using landmarks for catheterisation of the RIJV is still widely used, mainly in centres where an ultrasound device is not available.
In our literature search we were not able to find any studies assessing the effects of different ventilation modes on the CSA and diameters of RIJVs. It is not surprising to find that with positive pressure mechanical ventilation, the CSA and diameters increase. Although volume-controlled ventilation is the most common mode used on patients undergoing surgery, in recent years, pressure-controlled ventilation has been used increasingly in the operation rooms.
Lobato et al. [1] studied the effects of different manoeuvres such as the Trendelenburg and hepatic compression on the CSA of the RIJV during anaesthesia under a 20 cm H2O inspiratory hold and showed that all these manoeuvres increases the CSA of the RIJV.
Hollenbeck et al. [9] studied the effect of PEEP on the CSA of the RIJV in anaesthetised adults where they applied zero end-expiratory pressure (ZEEP) and a PEEP of 10 cm H20 to each patient in volume-controlled mode and found diameters and CSA increased significantly when PEEP is applied.
Trautner et al. [11] showed similar results in paediatric patients and stated that the Trendelenburg position and PEEP administration increases the CSA of IJA under volume-controlled ventilation.
Marcus et al. [8] compared the CSA of the RIJV in different PEEP levels in the Trendelenburg position. They found that the Trendelenburg position is more effective in increasing the CSA when compared with PEEP administration and stated that high PEEP levels are useless as they also have a negative impact on haemodynamics.We used a neutral supine position instead of the Trendelenburg position to evaluate the effects of mechanical ventilation on the RIJV without the effect of any position that increases the intrathoracic pressure. We have applied a PEEP level of 6 cm H20, which is considered to be physiological. Hence, we have observed PEEP as an effect that increases the CSA, not lessening it.
In their study, Bellazzini et al. [7] evaluated the effects of the “Valsalva” manoeuvre and hepatic compression, both individually and combined, during a stimulated venipuncture. They showed that in the absence of venipuncture compression, the CSA increased significantly with both manoeuvres, combined or separate. “Valsalva” manoeuvre increases the intrathoracic pressure especially during expiration, which results in an increase in the blood volume in the pulmonary bed.
In our study, no difference was observed in terms of anteroposterior and transverse diameters and CSA when two mechanical ventilation modes were compared, but these were significantly greater under PCV and VCV modes when compared with spontaneous ventilation. As the levels of PEEP used in both mechanical ventilation groups are the same, we cannot talk about a difference on the effect of PEEP in these two groups. Our results show that both ventilation modes have a similar effect on the CSA of the RIJV and can be used during catheterisation effectively both in neutral and head 30 degree rotated. The CSA measurements under spontaneous ventilation are lower when compared with the measurements under mechanical ventilation modes. This is not surprising, for when compared with spontaneous breathing, positive-pressure ventilation increases both peak and mean intrathoracic pressure. The increase in CSA under pressure control is higher although not significant and this can be explained with higher peak airway pressures (pressure support level and PEEP) observed in pressure-controlled ventilation when compared with volume-controlled ventilation.
Suarez et al. [12] evaluated the effect of head rotation and position on the CSA of the RIJV in patients under spontaneous ventilation. They measured the CSA of the RIJV in the supine and Trendelenburg positions with neck positions of neutral, 20 degrees and maximal rotation (58–71 degrees) and concluded that, although head rotation in the Trendelenburg position had no effect on the CSA, maximal rotation in a supine position caused an increase in the CSA. No difference was observed in the supine position when rotation was none or only 20 degrees. In our study, the head rotation was 30 degrees, whereas Suarez et al. [12] employed additional rotations. Hence, the increase in the CSA with the rotation under volume controlled or spontaneous ventilation in those studies depended on the high degree rotations. In another study, Wang et al. [4] showed that head rotation increases the overlapping of the RIJV and carotid artery, especially in high degree rotations. Although a rotation over 30 degrees can increase the CSA, overlapping of the vessels also increases the likelihood of unwanted arterial punctures. The only significant increase of the CSA with a 30 degree head rotation was in patients under PCV.
In their study, Lamperti et al. [4] showed that neutral head position is as safe as 45 degree lateral rotation during ultrasound guided RIJV cannulation and complications are higher in veins with smaller diameter.
In our study, no difference was observed when the CSA values were compared in terms of mechanical ventilation modes (PCV and VCV) with the head either in a neutral or 30 degree rotated position when body is in supine position. However, as an interesting result, only when under pressure-controlled ventilation the CSA of RIJV increased significantly with the rotation of the head to 30 degree lateral from neutral position. Although the increase when under volume-controlled was not statistically significant, it was clinically significant as it also enables a larger target for the venipuncture. In contrast to all these, although not statistically significant, a clinical significant finding was the decreasing of the CSA with a 30 degree rotation under spontaneous ventilation. The rotation of the head causes the lateral head of the sternocleidomastoid muscle to compress the RIJV when under spontaneous ventilation resulting with a decrease in CSA, whereas the rotation under positive mechanical ventilation increases the CSA as the positive intrathoracic pressure helps overcome the compression of sternocleidomastoid muscle. This finding leads us to believe that the catheterisation can be achieved with a larger CSA when the head is in neutral position in patients under spontaneous ventilation.
A limitation of our study is the lack of the actual puncture. During the puncture, compression can occur, changing the diameters and the CSA of the RIJV. Although the probe of the ultrasound mimics the pressure of the puncture, it is advisable also to study the effect of ventilation modes with actual punctures. This also is the strength of the study as we have observed the diameters and CSA of RIJV without any outer impact except ventilation, as it is harder to standardise the pressure done during catheterisation.
We conclude that both pressure-controlled and volume-controlled mechanical ventilation modes have similar effects on the CSA and diameters of the RIJV. Positioning of the head with a 30 degree rotation to lateral increases the CSA when under both mechanical ventilation modes, but decreases the CSA under spontaneous ventilation. Neutral position should be preferred under spontaneous ventilation whereas 30 degree rotation should be preferred in patients under pressure-controlled ventilation and volume-controlled ventilation.
Acknowledgment:The authors would like to thank native speaker, Ward Ryder for the English editing and to Bulent Sakaoglu for the statistical analysis.
1 Lobato EB, Florete OG Jr, Paige GB, Morey TE. Cross-sectional area and intravascular pressure of the right internal jugular vein during anesthesia: effects of trendelenburg position, positive intrathoracic pressure, and hepatic compression. J Clin Anesth. 1998;10(1):1–5.
2 Chittoodan S, Breen D, O’Donnell BD, Iohom G. Long versus short axis ultrasound guided approach for internal jugular vein cannulation: a prospective randomised controlled trial. Med Ultrasound. 2011;13(1):21–5.
3 Hayashi H, Ootaki C, Tsuzuku M, Amano M. Respiratory jugular venodilation: a new landmark for right internal jugular vein punctures in ventilated patients. J Cardiothorac Vasc Anesth. 2000;14(1):40–4.
4 Lamperti M, Subert M, Cortellazzi P, Vailati D, Borrelli P, Montomoli C, et al. Is a neutral head position safer than 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation? Results of a randomized controlled clinical trial. Anesth Analg. 2012;114(4):777–84
5 Wang R, Snoey ER, Clements RC, Hern HG, Price D. Effect of head rotation on vascular anatomy of the neck: an ultrasound study. J Emerg Med. 2006;31(3):283–6.
6 Mey U, Glasmacher A, Hahn C, Gorschlüter M, Ziske C, Mergelsberg M, et al. Evaluation of an ultrasound-guided technique for central venous access via the internal jugular vein in 493 patients. Support Care Cancer. 2003;11(3):148–55.
7 Bellazzini MA, Rankin PM, Gangnon RE, Bjoernsen LP. Ultrasound validation of maneuvers to increase internal jugular vein cross-sectional area and decrease compressibility. Am J Emerg Med. 2009;27(4):454–9.
8 Marcus HE, Bonkat E, Dagtekin O, Schier R, Petzke F, Wippermann J, et al. The impact of trendelenburg position and positive end-expiratory pressure on the internal jugular cross-sectional area. Anesth Analg. 2010;111(2):432–6.
9 Hollenbeck KJ, Vander Schuur BM, Tulis MR, Mecklenburg BW, Gaconnet CP, Wallace SC, et al. Brief report: effects of positive end-expiratory pressure on internal jugular vein cross-sectional area in anesthetized adults. Anesth Analg. 2010;110(6):1669–73.
10 Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J, et al. A. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10(6):R162.
11 Trautner H, Greim CA, Arzet H, Schwemmer U, Roewer N. Ultrasound-guided central venous cannulation in neuropaediatric patients to avoid measures causing potential increase in brain pressure. Anaesthesist. 2003;52(2):115–9.
12 Suarez T, Baerwald JP, Kraus C. Central venous access: the effects of approach, position, and head rotation on internal jugular vein cross-sectional area. Anesth Analg. 2002;95(6):1519–24.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.