Controversies in the mammography screening programme in Switzerland
DOI: https://doi.org/10.4414/smw.2014.13969
Pierre
Vassilakos, Rosa
Catarino, Michel
Boulvain, Patrick
Petignat
Recently, the Swiss Medical Board [1] issued a report stating that systematic mammography screening programmes for early detection of breast cancer are no longer reasonable for women to attend. A systematic review of the existing literature allowed the Board to conclude that the effectiveness of mammography is still uncertain, over-diagnosis and false positive tests cause harm, and the screening programmes have an unfavourable cost-effectiveness ratio.
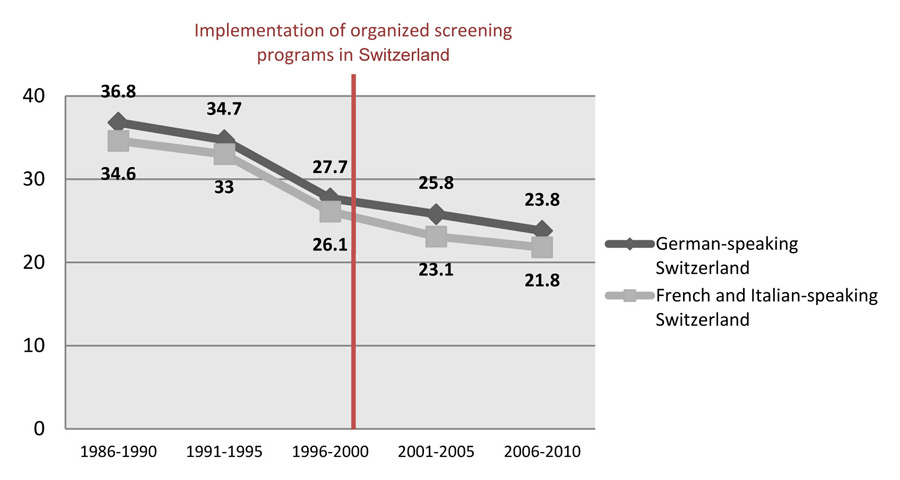
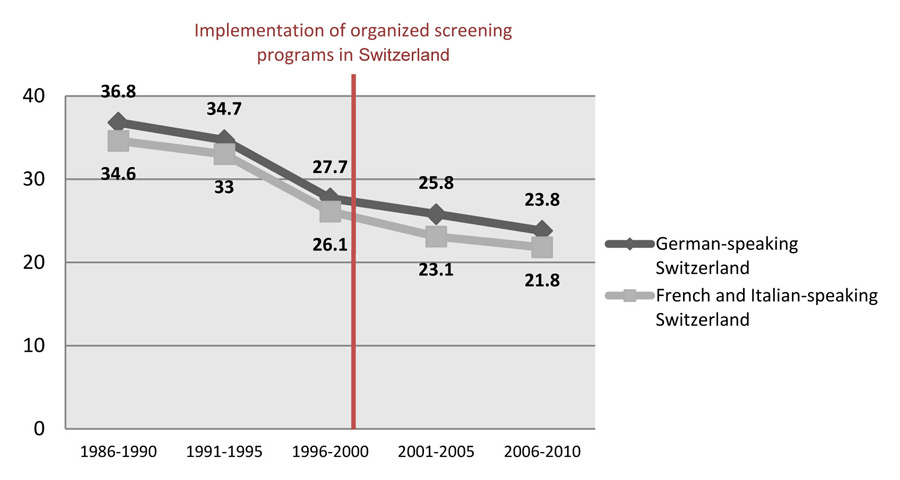
Figure 1
Breast cancer mortality rates by region over time (all women). Death rates per 100'000 are age standardised using the European Standard Population. The introduction of the mammography screening programme does not seem to modify the mortality rate, which had been progressively declining since 1990.
Source: Swiss Federal Statistical Office.
In response to these new recommendations, prominent Swiss personalities, experts and organisations have expressed their opinion, considering the report as “flawed and misleading” and that it could confuse women and cost their lives. Moreover, a review [2], published simultaneously with the report of the Swiss Medical Board, presented a completely opposite view of routine breast cancer screening by declaring that its benefits outweighed its harms.
This is not the first time that in Switzerland, as in other countries, controversy over the effectiveness of mammograms and other cancer screening method (prostate cancer) has been debated. Only a few cancer screening tests have proven to be effective by reducing mortality (Pap smears or human papillomavirus testing for cervical cancer and endoscopy for colorectal cancer).
Mammography can be effective, but the magnitude of mortality benefit is still unclear. An important issue related to breast cancer screening is over-diagnosis, which is a “side effect” of screening. Over-diagnosis corresponds to “disease” that will be identified by the test, but would never have caused symptoms or death in the absence of screening. Therefore, the detection of these “nonlife-threatening cancers” leads to high cure rates, and an artifactual increase in survival, exaggerating the apparent benefits of screening. Another separate issue is false positive results that cause anxiety and physical discomfort to women and generate additional testing or interventions to rule out cancer. Together, over-diagnosis and false positive results lead to unnecessary procedures that bring harm to women who attend screening programmes.
The best indicator to assess effectiveness of mammography in Switzerland is breast cancer mortality. However, several years have to elapse between the start of screening and the reduction in mortality.
In Switzerland, systematic screening programmes and opportunistic screening coexist in different regions of the country. It is, therefore, useful to compare mortality rates, and estimate over-diagnosis and false positivity between regions with different screening approaches. In the French-speaking region of Switzerland, screening programmes were implemented in 1999. The analysis of the data provided by the Swiss Federal Statistical Office shows that there is no difference in mortality between the two major regions of Switzerland (German-speaking vs French- and Italian-speaking), despite the increased incidence of diagnosed breast cancer in the French- and Italian-speaking regions that could be secondary to the higher screening coverage (table 1). Moreover, the introduction of the mammography screening programme does not seem to modify the mortality rate, which had been progressively declining since 1990 (fig. 1). Other reasons for mortality reduction besides screening, such as tamoxifen therapy and changes in cause-of-death coding, may act as confounders when evaluating screening benefits [3].
The recent controversy over the effectiveness of mammography highlights the urgent need for a clear regulation of the mammography screening programmes, which will permit clinicians to give confident recommendations to their patients, and public health decision-makers to make more global recommendations. Today, many clinicians and patients have the impression that a mammogram is simply an innocuous test able to detect a breast cancer sooner, with a better prognosis for cure and less invasive surgery. But the report of Swiss Medical Board demonstrated that this screening may end up harming more women than it helps. It is therefore essential to give balanced information that will ensure a good understanding of the benefits and harms of mammography. Balancing harms and benefits becomes a question that relies not only on scientific evidence but also on our values and how much our society is willing to pay to save one life.
Finally, we believe that it is now imperative to verify the accomplishment of the expected objectives that have been announced along with the implementation of breast cancer screening programmes in Switzerland. In order to do so, we think that a prospective study should be performed in our population by considering also the effect of diagnostic and treatment advances, taking as example the ongoing case-control study in England [4]. In the meantime, systematic screening programmes should be maintained until the benefits of mammography are clarified. Specialists should continue to standardise their practice by focusing on the improvement of the quality and safety of care provided to patients. The debate about the benefits of mammography should be centred on the balance of risks and benefits by age and the frequency of screening. Women should be encouraged to discuss with their clinicians their personal risk, and the real harms associated with over-diagnosis and false positive results. Each woman has the right to make medical decisions according to her values and obtain at the same time the possibility to maximise the benefits and minimize the harms.
|
Table 1:Breast cancer mortality rates in women aged between 50 and 69 years (recommended ages for screening). The periods from 1986 to 1990 and from 2006 to 2010 represent, respectively, the periods before and after the establishment of organised screening programmes in Switzerland.
Rate ratios and their respective 95% CIs have been calculated in order to compare mortality rates of two major regions of Switzerland (German-speaking vs French and Italian-speaking).
There is no difference in mortality between the two major regions of Switzerland despite the increased incidence of diagnosed breast cancer in the French and Italian-speaking regions that could be secondary to the higher screening coverage. |
|
|
|
German-speaking Switzerland
|
French- and Italian-speaking Switzerland
|
Rate ratio (95% CI, p-value)
|
| Screening (%) |
At least once |
43.5 |
F: 52.8
I: 57.3 |
– |
| |
In the last 12 months |
10.6 |
F: 19.4
I: 19.5 |
– |
| Incidence of breast cancer (100,000 women-year) |
1986–1990 |
211.0 |
229.1 |
1.085 (0.97–1.21; p = 0.14) |
| 2006–2010 |
254.1 |
316.2 |
1.244 (1.15–1.35; p <0.001) |
| Mortality from breast cancer (100,000 women-year) |
1986–1990 |
80.4 |
80.1 |
0.997 (0.83–1.120; p = 0.97 |
| 2006–2010 |
54.4 |
50.5 |
0.929 (0.76–1.13; p = 0.25) |
| C = Confidence Interval; F = French-speaking region; I = Italian-speaking region
Sources: Swiss Federal Statistical Office; National Cancer Programme for Switzerland 2011–2015, Bern. |
References
1 Board SM. Dépistage systématique par mammographie – 15 décembre 2013. 2013.
2 Duffy SW, Hsiu-Hsi Chen T, Smith RA, Xing-Fang Yen A, Tabar L, et al. Real and artificial controversies in breast cancer screening. Breast Cancer Manag. 2013;2(6):519–28.
3 Lutz J, Pury P, Fioretta G, Raymond L. The impact of coding process on observed cancer mortality trends in Switzerland. Eur J Cancer Prev. 2004;13(1):77–81.
4 Massat NJ, Sasieni PD, Parmar D, Duffy SW. An ongoing case-control study to evaluate the NHS breast screening programme. BMC cancer. 2013;13(1):596.