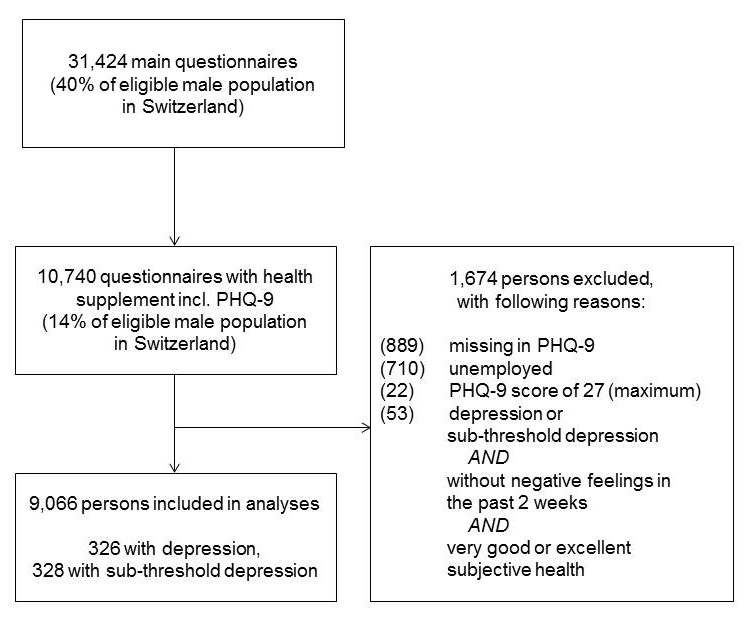
Figure 1
Flowchart of sample recruitment.
DOI: https://doi.org/10.4414/smw.2014.13945
Depression in adults is highly prevalent, and is one of the leading causes of disease burden and decreased work productivity worldwide [1, 2]; the numbers also hold true in Switzerland. One-year prevalence estimates of depression in Europe are reported to range from 3.1% to 10.1% [3]. According to the Swiss Health Survey, 3.1% of adults had a depressive syndrome, and 15.8% had some symptoms of a depressive syndrome during the last 2 weeks [4]. For Swiss adolescents and young adults aged between 16 and 20 years, the point prevalence is reported to be about 10% for females and about 6% for males [5]. In adolescents and young adults, depression accounts for one of the four leading causes of disease burden [6]. Repetitive health surveys on young Swiss adults showed worse mental health over time (between 1993 and 2003), but recent data are lacking [7]. Depression is also relevant in clinical settings of younger children such as paediatric practices [8], but in an earlier age the most prevalent diagnoses are externalising disorders like extensive aggression [9].
Measuring depression with population-based surveys is challenging [3] because, unlike clinical assessment [10], it does not allow a comprehensive assessment. In population surveys, however, self-reported information from standardised measurement instruments are common for the assessment ofdepressive symptoms, which afterwards can be used to predict a clinical diagnosis (depression) as described in classification systems (i.e., the International Classification of Disorders [ICD] or the Diagnostic and Statistical Manual for Mental Disorders [DSM-IV]). The term depression is ambiguous and can encompass a number of depressive symptoms, the severity of depressive symptoms and classification according to categories. An increasingly applied instrument to assess depression in the general population is the Patient Health Questionnaire (PHQ-9). Information from this inventory allows us to categorise persons into depressed versus non-depressed individuals by use of an algorithm of the combination of depressive symptoms [11]. Although such a classification is not a clinical diagnosis – which should only be made with a clinical interview (e.g., Structured Clinical Interview [SCID]) – the interrater reliability between self-reported depression inventories and a diagnosis by mental health professionals is high, with more than 80% accurate diagnoses [12, 13]. Among primary care patients, sensitivity and specificity of the PHQ-9 to detect a major depression ranged between 77% to 88% and 88% to 93% [14]. Comparative studies between the PHQ-9 and other self-reported measures (i.e., Hospital Anxiety and Depression Scale [HADS], Well Being Index [WBI)]) showed a slightly superior performance of the PHQ-9 [15].
Early adulthood is a transition phase consisting of new challenges, roles and tasks for individuals [16, 17]. Critical life events and low social or material resources are risk factors for the development of mental disorders during this phase [18]. In turn, mental disorders might complicate the transition from adolescence to adulthood. Depression is known to cause difficulties at school or at work [19] and in the formation of social relations.
The aim of this study was to estimate the recent prevalence of depression in a large cohort of young Swiss men. This study fills a gap between surveys in young children in clinical populations and surveys in adults in the general population by means of a standardised reliable assessment of depression. We explored the association of depression with education, material and social resources, and with problems experienced in daily life. By doing so, we highlight the psychosocial impact of depression in affected persons.
Data came from the Swiss Federal Surveys of Adolescents (ch-x) conducted in 2010 and 2011, and were collected during recruitment for compulsory military service at six national recruiting centres. Our sample included 10,740 Swiss male citizens aged 18 to 25 years (mean 19.7 years; standard deviation 1.1 years). All respondents filled out a paper-and-pencil questionnaire with a supplement focusing on health. Detailed information on the numbers of participants in the recruitment centres is not available; thus we calculated the proportion of the eligible population on the basis of data from the register survey of the Swiss census. The sample size corresponded to 14% of the eligible population in Switzerland. The survey design and translation process have been described elsewhere [20, 21]. The ch-x study was approved by the ch-x supervising board of nine members from the Swiss National Science Foundation, the Federal Statistical Office and scientists with various research backgrounds. Study procedures were also approved by the scientific advisory board of the ch-x, which has ten members from the humanities. Analyses depended on an already existing dataset, so approval from an additional ethics committee was unnecessary. Participants could refuse to fill in the questionnaire. Questionnaires were administered, collected and processed exclusively by trained nonmilitary staff to ensure confidentiality of participants’ answers. Data collection was anonymous.
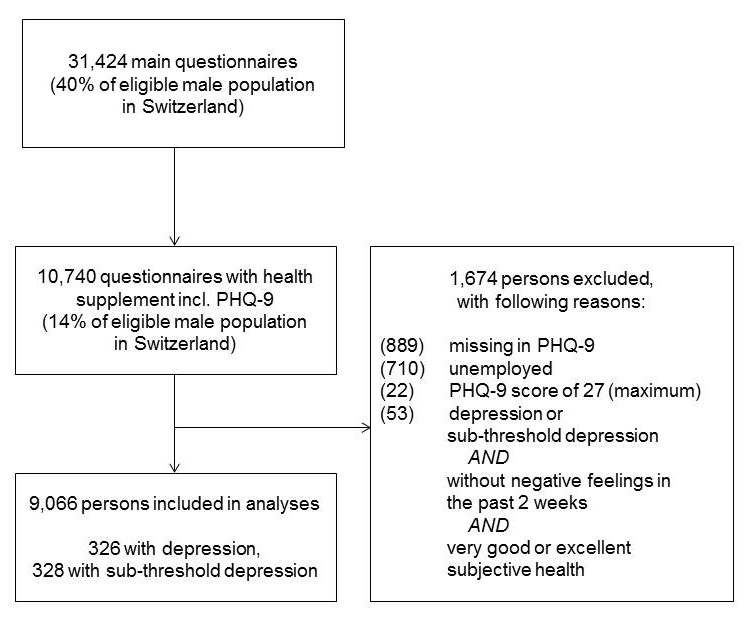
Figure 1
Flowchart of sample recruitment.
We excluded unemployed persons because one of our primary research questions referred to job-related circumstances. We also excluded from further analyses persons with one or more missing values in the variable of interest for analyses of associations. For persons with a valid depression score, we excluded those with the highest possible score. Persons with depression but without negative feelings in the past 2 weeks and a (at least) very good subjective health status were also excluded from further analyses since this pattern of answers is implausible. Overall, 0.75% of the sample was excluded for such reasons. We based all analyses on a sample of 9,066 persons. Figure 1 shows the sample recruitment.
Depression was measured using the PHQ-9 [22]. Persons indicated whether nine depressive symptoms – which correspond to the nine diagnostic criteria for major depressive disorder in the DSM-IV – had bothered them during the past 2 weeks. Persons could answer on a scale of 0–3 (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day). We assigned persons to three diagnostic groups according to the categorical PHQ office coding algorithm [22]:
A. Persons with depression: five or more of the nine depressive symptom criteria present on at least more than half of the days (i.e., ≥2) during the past 2 weeks (suicidal thoughts counted if present at all; i.e., ≥1); one of the symptoms had to be depressed mood or anhedonia, which was present more than half of the days.
B. Persons with subthreshold depression: two to four of the nine depressive symptom criteria present more than half of the days (i.e., ≥2) during the past two weeks (suicidal thoughts count if present at all; i.e., ≥1); one of these symptoms had to be depressed mood or anhedonia.
C. Persons without depression: the symptoms do not meet the diagnosis criteria of either group A or B.
Own education referred to the person’s highest completed educational degree. For students, education was based on the highest expected degree, assuming that the respondent would complete the ongoing education. Own education was categorised as mandatory, vocational training, and grammar school or higher.
Parents’ education was based on both maternal and paternal education. The parent with the higher educational level was chosen to indicate parents’ education. This was categorised as mandatory, secondary, or tertiary.
Household equivalent income was categorised as <2,500 CHF, 2,500–5,000 CHF, or >5,000 CHF per month. Ninety-two percent of the young men indicated that they currently still live with their parents. This suggests that the majority of our study population received material or monetary support from their families. Household income might therefore reflect the current financial situation of the parents rather than of the young men.
Social supportwas measured with three items: “number of friends” was measured as a count, and was categorised as having <3, 3–4, or >4 close friends; “perceived amount of emotional support” was measured on a four-point Likert scale including 1 = not sufficient at all, 2 = too little, 3 = sufficient, or 4 = much; “perceived amount of material support” was measured on a four-point Likert scale including 1 = not sufficient at all, 2 = too little, 3 = sufficient, or 4 = much. The last two items were merged into a single sum score, which we divided by the number of items (i.e., two) to match the scoring of the other variables used (resulting range: 1–4).
Satisfaction with social relations was measured with two items: “satisfaction with social relations with parents” and “satisfaction with social relations with friends”; both were measured on a five-point Likert scale. The lower category was 1 = feeling left alone, and the upper category 5 = being in good hands. Both items were combined to a sum score with a range from 1–5.
Self-efficacy was measured with a five-item short form of the general self-efficacy scale [23]. Persons answered all five items on a four-point Likert scale including 1 = not at all true, 2 = hardly true, 3 = moderately true, or 4 = exactly true. We calculated the recommended sum score, and divided it by the number of items (i.e., five) to match the scoring of the other variables used (resulting range: 1–5).
Satisfaction with job/training was measured on a four-point Likert scale including 1 = not satisfied at all, 2 = rather not satisfied, 3 = rather satisfied, or 4 = very satisfied.
We performed chi-square analyses to test the relationship between categorical variables and depression status. For continuous variables, we used one-way analyses of variance (ANOVA) with a Bonferroni correction as post-hoc procedure to compare the significance of differences in mean scores among persons on the basis of their depression status. Cohen’s d, as estimate of the effect size between subgroups, was calculated. According to Cohen’s definition, a d equal to 0.20 represents a small difference, 0.50 a moderate difference and 0.80 a large difference between groups [24]. A p-value below 0.005 was interpreted as meaningful, since the sample was large and multiple tests were performed. Next, we used crude and adjusted logistic regression analyses yielding (adjusted) odds ratios (AORs) with 99% confidence intervals (CIs). The AOR incorporated all social, material and educational variables to predict depression status (full diagnosis or subthreshold vs. no depression) in a multivariate model independent of their contribution in bivariate analyses. All analyses were performed using STATA (version 12 [25]).
| Table 1: Association of mental health with education and income in young men (n = 9,066). | ||||||
| Number | No depression | Subthreshold depression | Depression | χ2 | p-value | |
| Own education, % | ||||||
| Mandatory | 550 | 84.18 | 4.91 | 10.91 | ||
| Vocational | 5,314 | 93.81 | 3.03 | 3.16 | ||
| Grammar school or higher | 3,073 | 92.71 | 4.36 | 2.93 | 106.63 | 0.001 |
| Parents’ education, % | ||||||
| Mandatory | 185 | 88.65 | 4.32 | 7.03 | ||
| Upper secondary | 4,130 | 93.37 | 3.17 | 3.46 | ||
| Tertiary | 3,993 | 92.96 | 3.86 | 3.18 | 11.23 | 0.024 |
| Household equivalent income, % | ||||||
| <2,500 CHF | 896 | 90.29 | 4.46 | 5.25 | ||
| 2,500–5,000 CHF | 2,731 | 93.08 | 3.55 | 3.37 | ||
| >5,000 CHF | 3,692 | 93.93 | 3.36 | 2.71 | 17.86 | 0.001 |
| χ2 = chi-square test for categorical variables | ||||||
| Table 2: Association of mental health with social resources, self-efficacy and satisfaction in young men (n = 9,066). | ||||||
| Number | No depression | Subthreshold depression | Depression | χ2 a / Fb | p-value a / b | |
| Number of friends, % | ||||||
| <3 | 605 | 84.13 | 6.28 | 9.59 | ||
| 3–4 | 1,370 | 90.80 | 4.60 | 4.60 | ||
| >4 | 6,120 | 94.56 | 3.01 | 2.43 | 121.93 | 0.001 |
| Perceived amount of emotional support, % | ||||||
| Not at all sufficient | 85 | 58.82 | 18.82 | 22.35 | ||
| Too little | 379 | 77.57 | 18.83 | 12.66 | ||
| Sufficient | 5,309 | 92.79 | 3.82 | 12.67 | ||
| Much | 3,206 | 95.51 | 2.15 | 2.34 | 321.11 | 0.001 |
| Perceived amount of material support, % | ||||||
| Not sufficient at all | 74 | 63.51 | 17.57 | 18.92 | ||
| Too little | 410 | 79.27 | 7.56 | 13.17 | ||
| Sufficient | 5,689 | 92.90 | 3.71 | 3.39 | ||
| Much | 2,828 | 95.30 | 2.51 | 2.19 | 253.24 | 0.001 |
| Perceived amount of support, mean (SD) | 8,957 | 3.30 (0.51) | 3.02 (0.65)c | 2.95 (0.70)c | 104.27 | 0.001 |
| Satisfaction with social relations with parents, % | ||||||
| (1) Left alone | 120 | 71.67 | 11.67 | 16.67 | ||
| (2) | 217 | 80.65 | 9.22 | 16.66 | ||
| (3) Middle category | 693 | 86.29 | 6.35 | 10.13 | ||
| (4) | 1,729 | 91.96 | 4.57 | 3.47 | ||
| (5) In good hands | 6,149 | 94.73 | 2.67 | 2.60 | 219.44 | 0.001 |
| Satisfaction with social relations with friends, % | ||||||
| (1) Left alone | 40 | 77.50 | 5.00 | 17.50 | ||
| (2) | 164 | 77.44 | 10.98 | 11.59 | ||
| (3) Middle category | 870 | 77.43 | 7.70 | 7.24 | ||
| (4) | 3,083 | 93.12 | 3.80 | 3.08 | ||
| (5) In good hands | 4,716 | 95.02 | 2.50 | 2.48 | 200.71 | 0.001 |
| Satisfaction with social relations, mean (SD) | 8,789 | 4.49 (0.60) | 4.07 (0.79)d | 4.00 (0.92)d | 149.85 | 0.001 |
| Self-efficacy, mean (SD) | 8,851 | 3.20 (0.46) | 2.99 (0.50) | 2.82 (0.59) | 131.33 | 0.001 |
| Satisfaction with job/training/school, % | ||||||
| Not satisfied at all | 121 | 63.64 | 16.53 | 19.83 | ||
| Rather dissatisfied | 532 | 83.27 | 7.89 | 8.83 | ||
| Rather satisfied | 2,938 | 91.70 | 4.22 | 8.84 | ||
| Very satisfied | 4,441 | 95.23 | 2.50 | 2.27 | 269.31 | 0.001 |
| SD = standard deviation a χ2–test for categorical variables; b F-test for continuous variables (analysis of variance); c/d Differences between groups in mean scores are not significant at p<0.005 using a Bonferroni correction as post-hoc test | ||||||
In the total sample (n = 9,066), the point prevalence of depression was 3.60% (99% CI 3.10%–4.10%); 3.62% (99% CI 3.11%–4.13%) suffered from subthreshold depression. Persons with depression had a mean PHQ-9 score of 15.71 (median 15; interquartile range [IQR] 4), subthreshold depression was also associated with elevated scores (mean 9.24; median 9; IQR 3). The mean score of persons without depression was much lower (mean 3.04; median 2; IQR 5). Depression was associated with a respondent’s own educational status and household equivalent income (table 1; both p <0.005). However, parents’ education was associated with the prevalence of depression only in trend (p = 0.024). The prevalence rates for depression were about three times as high in young adults with mandatory education than in those with the highest educational level. Persons in the group with the lowest household equivalent income had about twice as much risk of suffering from depression as compared with the highest income group. An important finding is the rather invariant prevalence of subthreshold depression over social strata.
When we looked at resources for mental health, social support was closely linked to depression in young adults (upper part table 2; all p-values <0.001). A low number of friends was associated with a four-fold risk of depression. Low perceived emotional support and low material support were also strongly associated with depression, and persons without sufficient resources had an especially pronounced risk of depression (22.35% and 18.92% respectively). The link between social resources and subthreshold depression was also supported by our data. Fewer friends, lower perceived emotional support or lower perceived material support increased the risk of subthreshold depression. Therefore, the perceived social support (score) did not differ significantly between young adults with subthreshold depression and those with depression. However, both diagnostic groups differed from persons with no depression (d = 0.66 and 0.53, respectively).
The satisfaction with social relationships mirrored the initial findings from social support, and showed the same pattern (lower part table 2; p <0.001). However, the association between satisfaction measures and depression was less pronounced than for social support measures. The satisfaction with social relationships (score) did not differ between persons with subthreshold and full depression, but both subgroups differed from persons without depression (d = 0.79 and 0.68, respectively).
As a more general resource for mental health, the amount of self-efficacy differed between the three subgroups. As expected, persons with depression reported a lower self-efficacy than persons without depression (d = 0.82). Subthreshold depression was also associated with a lower self-efficacy as compared with persons without depression (d = 0.46). Self-efficacy also differed between depressed persons and those with subthreshold depression, but with a smaller effect size (d = 0.31).
An important facet of young adults’ life was the satisfaction with their current situation at school or at work. Persons with depression and subthreshold depression reported a substantial loss of their satisfaction in school or at work (19.83% and 16.53%, respectively; see table 2).
Table 3 shows univariate and multivariate associations of all sociodemographic and social variables with the presence of (subthreshold) depression. In the univariate unadjusted model, the respondent’s own education, household income, number of friends, self-efficacy and all measures of satisfaction (friends and job/school) showed significant associations in the expected direction. Parents’ education was not associated with depression in Swiss young men. In the multivariate model, respondent’s own education and household income were no longer associated with (subthreshold) depression. A low satisfaction with job/school and a low self-efficacy were the most important correlates with (subthreshold) depression with an AOR of 2.5 and above. A low satisfaction with social relations and a low number of friends contributed independently to the risk for (subthreshold) depression with an AOR of about 1.8. Taken together, low social resources, a low satisfaction with job/school, and a low self-efficacy had a unique negative impact on the chance for (subthreshold) depression.
| Table 3:Logistic parameter estimates for young men with full or subthreshold depression (n = 9,066). Estimates as unadjusted and adjusted odds ratios with 99% confidence intervals. | ||||
| OR | 99% CI | AOR | 99% CI | |
| Own education | ||||
| Mandatory | 2.39 | 1.68‒3.39 | 1.80 | 0.97‒3.36 |
| Vocational | 0.84 | 0.67‒1.06 | 0.91 | 0.65‒1.27 |
| Grammar school or higher | 1.00 | 1.00 | ||
| Parents’ education | ||||
| Mandatory | 1.69 | 0.91‒3.14 | 0.64 | 0.23‒1.78 |
| Upper secondary | 0.94 | 0.75‒1.18 | 0.91 | 0.66‒1.26 |
| Tertiary | 1.00 | 1.00 | ||
| Household equivalent income | ||||
| <2,500 CHF | 1.66 | 1.18‒2.34 | 1.45 | 0.93‒2.27 |
| 2,500–5,000 CHF | 1.15 | 0.88‒1.50 | 0.91 | 0.64‒1.29 |
| >5,000 CHF | 1.00 | 1.00 | ||
| Number of friends | ||||
| <3 | 3.28 | 2.38‒4.52 | 1.88 | 1.16‒3.06 |
| 3–4 | 1.76 | 1.33‒2.33 | 1.27 | 0.86‒1.88 |
| >4 | 1.00 | 1.00 | ||
| Low perceived amount of supporta | 2.74 | 2.27‒3.30 | 1.28 | 0.94‒1.76 |
| Low satisfaction with social relationsa | 2.35 | 2.05‒2.70 | 1.85 | 1.47‒2.34 |
| Low self-efficacya | 3.51 | 2.83‒4.36 | 2.53 | 1.80‒3.56 |
| Satisfaction with job/training/school | ||||
| Not satisfied at all | 11.40 | 6.78‒19.16 | 7.37 | 3.18‒17.06 |
| Rather not satisfied | 4.01 | 2.82‒5.69 | 2.64 | 1.61‒4.33 |
| Rather satisfied | 1.81 | 1.41‒2.32 | 1.44 | 1.01‒2.03 |
| Very satisfied | 1.00 | 1.00 | ||
| AOR = adjusted odds ratio with n = 5,236; CI = confidence interval; OR = odds ratio Bold type indicates association is significant at 99% CI a We reversed the direction of the sum score, indicated by the prefix “low”, to make the comparability of OR and AOR easier | ||||
Depression and subthreshold depression was prevalent in about 7% of young male adults in Switzerland. The point prevalence of depression in our sample corresponds well with other studies: in the German Early Developmental Stages of Psychopathology Study sample, the lifetime prevalence of depression in men aged 14 to 24 years was 7.7% [26]. Our findings are in line with earlier studies on the point prevalence of depression in Switzerland, where it was reported that about 6% of young men had depression [5, 7]. The most recent data of the German health survey also assessed depression with the PHQ-9, and found a 12-month prevalence of 8% in this age group [11].
Depression was associated with lower social, economic and educational resources. Social support was associated with better mental health, and represents an important protective factor in this age group [27]. Poor mental health was also associated with a substantial loss of satisfaction in school or at work. In consequence, this might result in noncompletion of school- or job-related training, which is likely to lead to additional difficulties during the transition to adulthood [2, 19, 28]. The reported associations of depression with resources and job/school satisfaction might lead to an overall poor quality-of-life prognosis, since these young men have to cope with limitations in mental health and limitations in resources.
Our findings in young adults with subthreshold depression were similar to those with depression, with similar patterns but less pronounced associations. This raises the question whether subthreshold depression should be considered a relevant health impairment: the answer is yes [29]. Subthreshold depression is a risk factor for the development of full depression in later life [30], and recent quality of life is considerably reduced in such adolescents and young adults [31].
From a gender perspective, the results have additional implications for the prevalence estimates of depression in young adults in Switzerland and for healthcare [32]. First, males might under-report symptoms of depression [18], and may have a rather “externalising” coping style [33]. Therefore, prevalence estimates for females might be higher. Second, males utilise mental health services less often [34], which might have negative consequences in the long run. Third, a gender paradox is present, since young males have a suicide rate that is three times higher than females [35], which contradicts the lower depression rates in males.
Taken together, our findings emphasise the need to target young Swiss men with prevention and intervention measures to reduce initial symptoms and to improve long-term prognosis. Some primary prevention programmes have been found to be effective in the short-term [36, 37], but concerns about the efficacy of such interventions are also present [38]. The broad application of prevention programmes to the general population often results in lower effects than indicated programmes with distressed individuals [39, 40]. The early detection of depression in young adults is crucial to reach better treatment outcomes and to improve the long-term prognosis of initially affected persons. Low self-efficacy and low social resources were found to be very important for the trajectory from poor mental health to depression in young adults [41].
For the treatment of patients with depression in adults, a variety of effective psychotherapeutic treatments are available [42]; pharmacological interventions are also beneficial. For children and adolescents, cognitive behavioural therapy and pharmacological interventions were effective in the treatment of depression [43]. However, the underutilisation of treatments for mental disorders in adolescents and young adults is very common [44]. From the perspective of healthcare providers in Switzerland, there are still urgent training needs for communication about, and treatment of, depression in this age group [45].
The study population and those excluded owing to missing or implausible data differed in some material, social and educational variables. Our study population had better education, a higher household income, more emotional and material support, and reported a higher level of self-efficacy. The definition of young adults with depression was based on self-reports. There was no clinical diagnosis from expert interviews. Thus, we cannot rule out the possibility of an over-reporting of symptoms as a result of the context of the assessment (i.e., military conscription). From the opposite perspective, we excluded unemployed young men who have a higher risk of poor mental health, and who are known to be more difficult to reach with preventive programmes. Additionally, young men with a history of severe depression are less likely to have participated in the study, since they do not need to attend the conscription examination. Thus, our results may underestimate the prevalence of depression and need for care in this population. The cross-sectional survey design did not allow judgments about the direction of causality of the associations and, furthermore, we do not want to imply any causality.
Future work should include a longitudinal youth cohort in Switzerland with standardised measures of depression to assess the stability of depressive symptoms over time, as well as to identify causal relations between depression and education, and social and economic resources across different stages of life. Given the negative consequences associated with depression in adolescence and early adulthood, intervention studies targeting prevention, as well as health services research, are of critical importance. School-based strategies outside of paediatric care may help to detect depressive symptoms at an early stage. Finally, data on healthcare utilisation in this age group are urgently needed in the Swiss context in order to identify potential barriers to care, and those adolescents and young adults with unmet mental health needs.
Depression and subthreshold depression are a major burden on health in young Swiss men. This study updates earlier epidemiological findings from Switzerland and shows that, from a public health perspective, (subthreshold) depression in early adulthood is an important issue. Since (subthreshold) depression was associated with a pronounced risk of insufficient job and school satisfaction and lower self-efficacy, there is a need to detect and treat young men with (subthreshold) depression from early on in order to improve the long term prognosis. This seems especially important for a successful trajectory from adolescence to adulthood. Intervention strategies should especially target the lack of social resources of these young adults, which is also a risk factor in the aetiology of depression.
Acknowledgement: The study used data from the Swiss Federal Surveys of Adolescents (ch-x) collected by the ch-x research consortium ch-x cc. Project management: Institute for the Management and Economics of Education, University of Teacher Education Central Switzerland Zug: Stephan Huber. Research partners: Institute for Education Evaluation, Associated Institute of the University of Zurich: Urs Moser; Institute of Social and Preventive Medicine, University of Bern: Thomas Abel; and the Department of Sociology, University of Geneva: Sandro Cattacin.
1 Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
2 Kessler R. The costs of depression. Psychiatr Clin North Am. 2012;35(1):1–14.
3 Wittchen HU, Jacobi F. Size and burden of mental disorders in Europe – a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol. 2005;15(4):357–76.
4 Schuler D, Burla L. Psychische Gesundheit in der Schweiz: Monitoring 2012 [Mental Health in Switzerland: Monitoring 2012]. Neuchâtel: Schweizersiches Gesundheitsobservatorium; 2012.
5 Narring F, Tschumper A, Inderwildi Bonivento A, Jeannin A, Addor V, Bütikofer A, et al. SMASH-02: Swiss multicenter adolescent survey on health 2002. Lausanne: Institut Universitaire de Médecine Sociale et Préventive; 2004.
6 Estimates of DALYs by sex, cause and WHO region for 2002 [database on the Internet]. World Health Organization; 2002 [cited June 12, 2013]. Available from: http://www.who.int/entity/healthinfo/statistics/gbdwhoregiondaly2002.xls.
7 Mohler-Kuo M, Wydler H, Zellweger U, Gutzwiller F. Differences in health status and health behaviour among young Swiss adults between 1993 and 2003. Swiss Med Wkly. 2006;134(29–30):464–72.
8 In-Albon T, Zumsteg U, Müller D, Scheider S. Mental disorders in the paediatric setting – results of a Swiss survey. Swiss Med Wkly. 2010;140:1–5.
9 Michaud PA, Fombonne E. Common mental health problems. BMJ. 2005;330:835–8.
10 Compas BE, Ey S, Grant KE. Taxonomy, assessment, and diagnosis of depression during adolescence. Psychol Bull. 1993;114(2):323–44.
11 Busch MA, Maske UE, Ryl L, Schlack R, Hapke U. Prävalenz von depressiver Symptomatik und diagnostizierter Depression bei Erwachsenen in Deutschland [Prevalence of depressive symptoms and the diagnosis of depression in adults in Germany]. Bundesgesundhbl Gesundheitsforsch Gesundheitsschutz. 2013;56:733–9.
12 Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001;16(9):606–13.
13 Löwe B, Gräfe K, Zipfel S, Witte S, Loerch B, Herzog W. Diagnosing ICD-10 depressive episodes: Superior criterion validity of the Patient Health Questionnaire. Psychother Psychosom. 2004;73(6):386–90.
14 Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen Hosp Psychiatry. 2010;32(4):345–59.
15 Löwe B, Spitzer RL, Gräfe K, Kroenke K, Quenter A, Zipfel S, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004;78(2):131–40.
16 Roisman GI, Masten AS, Coatsworth JD, Tellegen A. Salient and emerging developmental tasks in the transition to adulthood. Child Dev. 2004;75(1):123–33.
17 Adam A, Faouzi M, Gaume J, Gmel G, Daeppen J-B, Bertholet N. Age of first alcohol intoxication: Association with risky drinking and other substance use at the age of 20. Swiss Med Wkly. 2011;141:w13226.
18 Fiis RH, Wittchen HU, Pfister H, Lieb R. Live events and changes in the course of depression in young adults. Eur Psychiatry. 2002;17:241–53.
19 Fergusson D, Woodward L. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59(3):225–31.
20 Hofmann K, Schori D, Abel T. Self-reported capabilities among young male adults in Switzerland: Translation and psychometric evaluation of a German, French and Italian version of a closed survey instrument. Soc Ind Res. 2013;114(2):723–38.
21 Abel T, Hofmann K, Schori D. Social and regional variations in health status and health behaviours among Swiss young adults. Swiss Med Wkly. 2013;143:w13901.
22 Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD. JAMA. 1999;282(18):1737–44.
23 Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: A user’s portfolio causal and control beliefs. Windsor: NFER-NELSON; 1995. p. 35–7.
24 Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988.
25 StataCorp. Stata data analysis statistical software: Release 12. StataCorp LP, College Station, TX; 2011.
26 Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med. 1998;28:109–26.
27 Khatib Y, Bhui K, Stansfeld SA. Does social support protect against depression and psychological distress? Findings from the RELACHS study of east London adolescents. J Adolesc. 2013;36(2):393–402.
28 Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: Educational attainment. Am J Psychiatry. 1995;152(7):1026–32.
29 Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: The relevance of thresholds. Br J Psychiatry. 2010;196(5):365–71.
30 Fergusson D, Horwood L, Ridder E, Beautrais A. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62(1):66–72.
31 Bertha EA, Balázs J. Subthreshold depression in adolescence: A systematic review. Eur Child Adolesc Psychiatry. 2013:1–15.
32 Gutzwiller F, Hurrelmann K, Kolip P, Schaeffer D. Männergesundheitsbericht 2013. Psychische Erkrankung des Mannes [Men’s health report 2013. Mental health in men]. Bern: Hans Huber; 2013.
33 Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994;115(3):424.
34 Mauerhofer A, Berchtold A, Michaud PA, Suris JC. GP’s role in the detection of psychological problems of young people: A population-based study. Br J Gen Pract. 2009:e308–e14.
35 Federal Statistical Office. Cause of death statistics 2009. Assisted suicide and suicide in Switzerland. Neuchâtel: Federal Statistical Office; 2010.
36 Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry. 2001;58:1127–34.
37 Pössel P, Horn AB, Groen G, Hautzinger M. School-based prevention of depressive symptoms in adolescents: A 6–month follow up. J Am Acad Child Adolesc Psychiatry. 2004;43:1003–10.
38 Spence SH, Shortt AL. Research review: Can we justify the widespread dissemination of universal, school-based interventions for the prevention of depression among children and adolescents? J Child Psychol Psychiatry. 2007;48(6):526–42.
39 Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. J Consult Clin Psychol. 2006;74(3):401.
40 Calear AL, Christensen H. Systematic review of school-based prevention and early intervention programs for depression. J Adolesc. 2010;33(3):429–38.
41 Costello DM, Swendsen J, Rose JS, Dierker LC. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J Consult Clin Psychol. 2008;76(2):173.
42 Barth J, Munder T, Gerger H, Nüesch E, Trelle S, Znoj H, et al. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: A network meta-analysis. PLoS Med. 2013;10(5):e1001454.
43 Thapar A, Collishaw S, Potter R, Thapar AK. Managing and preventing depression in adolescents. BMJ. 2010;340.
44 Jeannin A, Narring F, Tschumper A, Inderwildi Bonivento A, Addor V, Bütikofer A, et al. Self-reported health needs and use of primary health care services by adolescents enrolled in post-mandatory schools or vocational training programms in Switzerland. Swiss Med Wkly. 2005;135:11–8.
45 Kraus B, Stronski S, Michaud PA. Training needs in adolescent medicine of practising doctors: A Swiss national survey of six disciplines. Med Educ. 2003;37(8):709–14.
Funding / potential competing interests: This study was supported by a grant from the Swiss National Science Foundation (No. 105313_130068_/1). No other potential conflict of interest relevant to this article was reported.