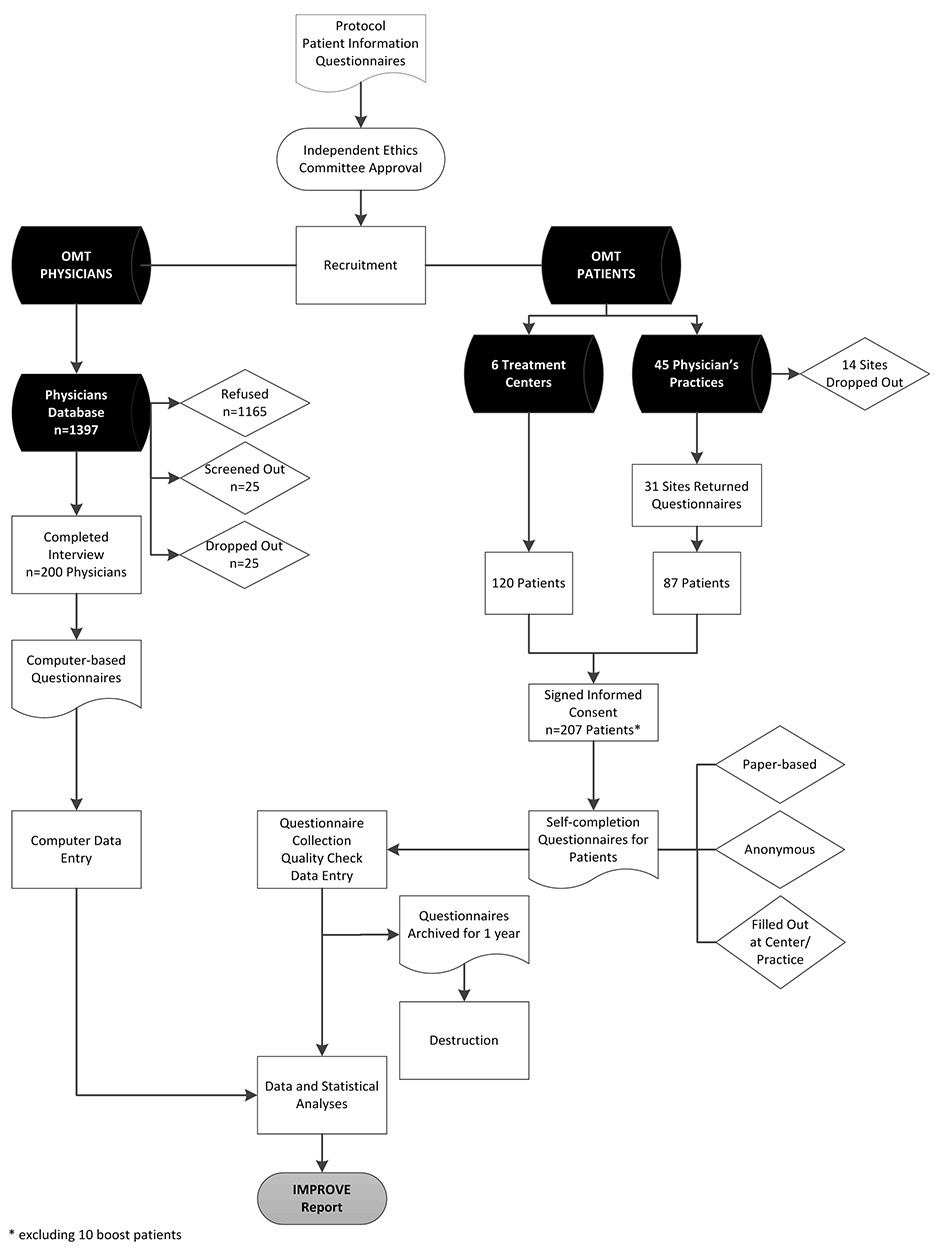
Figure 1
The Swiss IMPROVE study flow chart and disposition of subjects.
OMT = opioid maintenance therapy
DOI: https://doi.org/10.4414/smw.2014.13933
As estimated 25 million people worldwide are drug-dependent and a large majority of these (approximately 15.6 million) are illicit opioid users. Opioid dependence is a recognised chronic relapsing condition associated with high economic burden, not only in terms of direct healthcare costs, but also expenditures in social welfare, productivity loss, depression and law enforcement [1].
Switzerland’s drug policy model has always been unique and progressive and is based on “four pillars”, consisting of measures in the following four areas: prevention, therapy, harm reduction and law enforcement [2]. The first European supervised drug-consumption room was established in Bern in 1986. In the years that followed, more of these facilities were established all over the country, which gave status to medical institutions in Switzerland [3]. A great deal of the evidence base on opioid substitution treatment was collected from these settings [4–7].
A recent United Nations survey reported that about 0.6% of the Swiss population aged 15 to 64 years are opioid users [8]. Of the estimated 22,000 opioid-dependent individuals in Switzerland, more than 85% are in therapy [9]. Current clinical guidelines from the Swiss Society of Addiction Medicine (SSAM), the Swiss Association of the Medical Officers of the Cantons (VKS), and the Federal Office of Public Health (FOPH) fully support opioid maintenance therapy (OMT), with methadone and buprenorphine as the recommended first-line OMT medications [10]. Substitution-assisted treatment is covered by the Swiss obligatory health insurance system, but with certain limitations. Take-home medications on weekends and holidays are generally allowed, albeit with restrictions.
However, although the Swiss model at first glance seems to work smoothly, there is a need to reassess this system in a rapidly changing world. Over the years, new legislations, treatment options and drug-related problems have arisen. Regional differences across the country still abound.
In addition, the main players in OMT are changing. The demographics of the drug scene have been transformed as the drug addicts of the 1980s have aged and a new generation of drug users is emerging [6, 10]. In parallel, the profile of the treating physician may also be changing as the OMT pioneers of 30 years ago go into retirement and a younger generation of doctors take over treatment responsibilities.
It is important, now more than ever, to determine the “real-world” perspectives on OMT to help optimise decision making regarding treatment provisions.
The IMPROVE study aimed to gain understanding of the attitudes and beliefs towards OMT in Switzerland with regards to quality and access to treatment. To obtain a “real-world” view of OMT, the study approached its goals from two different angles, from the perspectives of the OMT patients and of the treating physicians.
The IMPROVE study collected a large body of data on OMT in Switzerland. This paper presents an overview of the IMPROVE study using a small subset of the dataset, focusing on the research design and methodology, as well as the demographic profile of the participants. In addition, the responses to several key questions are presented, including medication choices, therapy satisfaction, diversion and misuse. Other important data will be presented in subsequent publications.
IMPROVE was an observational, questionnaire-based, cross-sectional study on OMT conducted in Switzerland. Respondents consisted of OMT patients and treating physicians from various regions of the country. Recruitment was implemented through the Swiss drug treatment centres that offer help and support to patients and drug users, as well as through physicians who are active in the field of drug substitution research and practice.
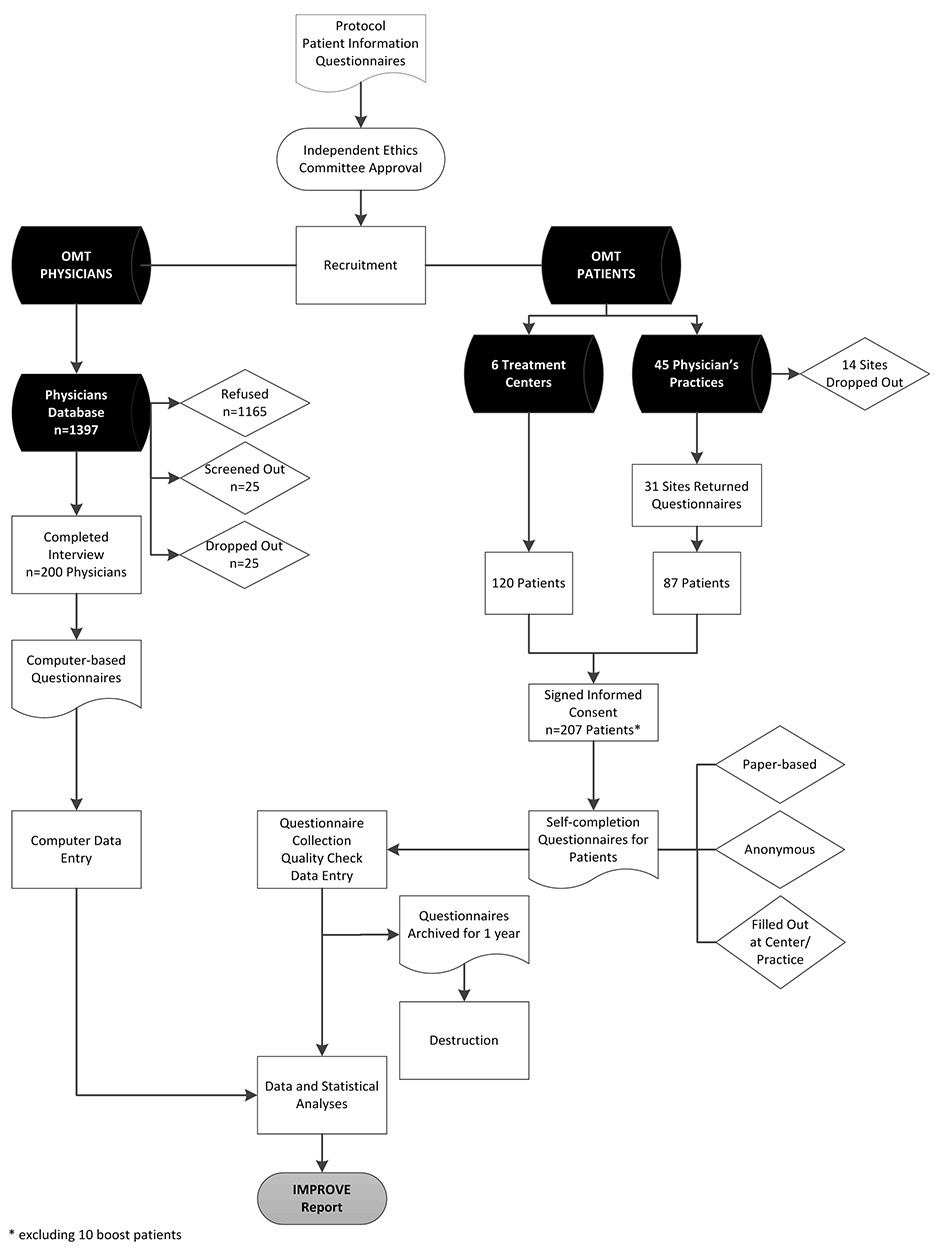
Figure 1
The Swiss IMPROVE study flow chart and disposition of subjects.
OMT = opioid maintenance therapy
The recruitment centres were selected on the basis of the size of the canton where the centre is located, the size and importance of the centre and membership of OMT-relevant networks (e.g., SSAM). On the basis of these considerations, sites from the biggest cities in Switzerland were identified. For political reasons, the city of Geneva could not be included, but other parts of French-speaking Switzerland were covered. Lugano was excluded for logistical reasons; thus the study did not cover the Italian-speaking region.
Data were collected using questionnaires in the local languages of German and French. The physician interviews were performed from 10 May to 15 June 2012. Patient data collection was conducted from 14 May to 07 September 2012.
The study protocol, patient information and questionnaires were approved by local independent ethics committees. Patients had to sign an informed consent form before study entry and study conduct followed Good Clinical Practice (GCP) guidelines. Confidentiality of the participants was observed at all times. The IMPROVE study flowchart is shown in figure 1.
The key inclusion criteria for physicians were active involvement in OMT and willingness to answer the questionnaire. Physicians’ data were collected through telephone interviews using a 54-item computer-based questionnaire. The questions addressed knowledge about and attitudes towards OMT, illicit drug use, guidelines and administrative requirements, and difficulties in treating patients. Responses were entered directly into the computer by the interviewer. On average, an interview lasted for 27 minutes.
A total of 250 opioid-dependent patients on OMT were planned to be recruited from seven sites in Switzerland, 50% of whom would come from physician’s offices, and 50% from substitution treatment support centres. The rationale behind this recruitment strategy was based on data from the methadone case register of canton Zurich, which indicated that 48.0% of OMTs are managed by general practitioners (GPs) and 47.6% by specialised treatment centres [11].
A total of 45 GPs agreed to distribute the patient questionnaires; 31 (69%) sent back completed questionnaires and 14 (31%) did not.
Six physicians from treatment centres in five cantons distributed questionnaires to OMT patients at their respective centres.
All recruiting physicians were instructed to recruit patients in a random manner.
Only opioid-dependent patients currently on OMT who signed the informed consent form and were willing to answer the questionnaire were included in the study.
A paper-based questionnaire consisting of 83 questions was used for patient data collection. The questionnaire covered sociodemographics, previous and current substitution therapy (type, access, satisfaction, scope for improvement, etc.), illicit drug use, drug diversion and the black market, and prison experience. The questionnaires were handed out at physician’s offices and centres and the patients had to complete (approximately 25–30 minutes) these on site. Data were collected anonymously, with no individually identifiable health information included in the questionnaires and datasets. The completed questionnaires were to be archived for 1 year and then destroyed.
The planned patient sample size (n = 250) was the maximum realistic number of patients that could be recruited. However, only 207 eligible patients could initially be included in the study. An additional 10 patients were later added to boost the sample size of buprenorphine users to n = 36. In order not to bias the total sample, the boost sample was not included in the overall analysis, but was used in specific analyses stratified by medication type.
Physicians’ and patients’ datasets were analysed separately. Data summaries were provided using descriptive statistics for continuous variables, and frequency tables (absolute counts and percentages) for categorical variables. Significance testing at the 95% and 99% levels was applied where feasible (n >29). No comparison between the two datasets was performed.
Where appropriate, analyses took into account the multicultural and multilinguistic character of the population, and regional and demographic variations were indicated.
From a database of OMT physicians, 1,397 were considered for participation in the study. Of these, 1,165 (83%) refused participation, 25 (2%) did not meet all inclusion criteria, and 39 (3%) dropped out during the interview period (fig. 1).
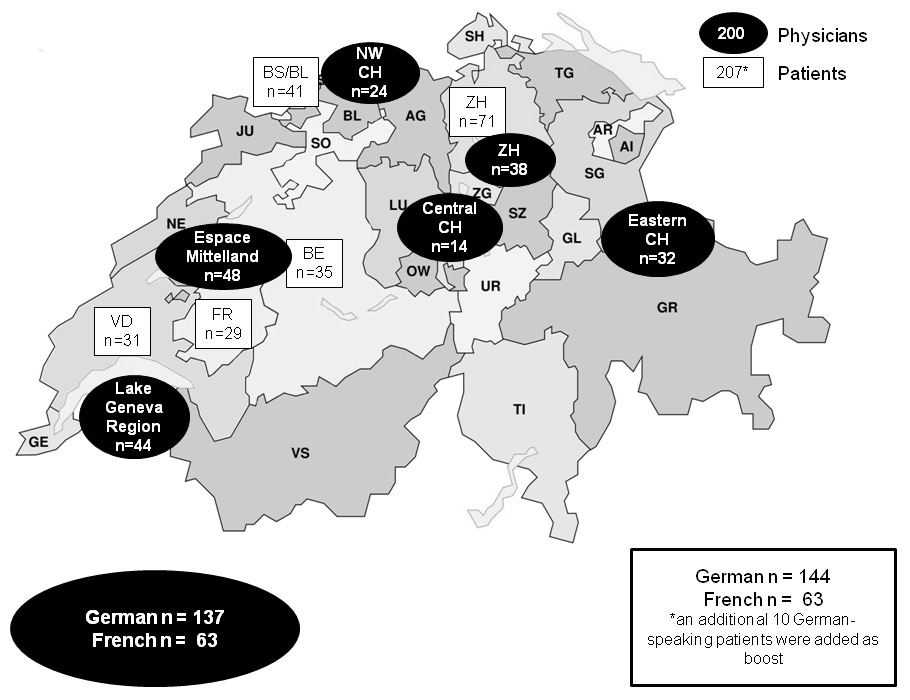
Figure 2
Regional distribution of study participants. Dark oval fields represent the physicians. White rectangular fields represent the patients. Abbreviations on the map represent the different cantons of Switzerland. Patients were recruited from Bern (BE), the Basel area (BS/BL), Fribourg (FR), Vaud (VD) and Zurich (ZH).
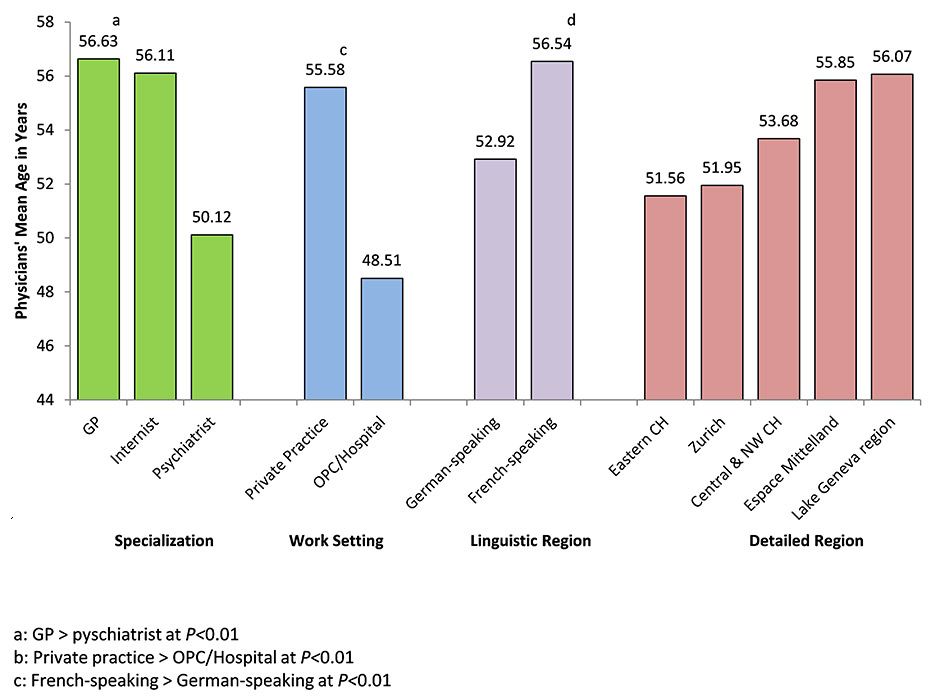
Figure 3
The age profile of the interviewed physicians by specialisation, work setting, linguistic region and detailed regional distribution.
GP = general practitioner; OPC = outpatient clinic
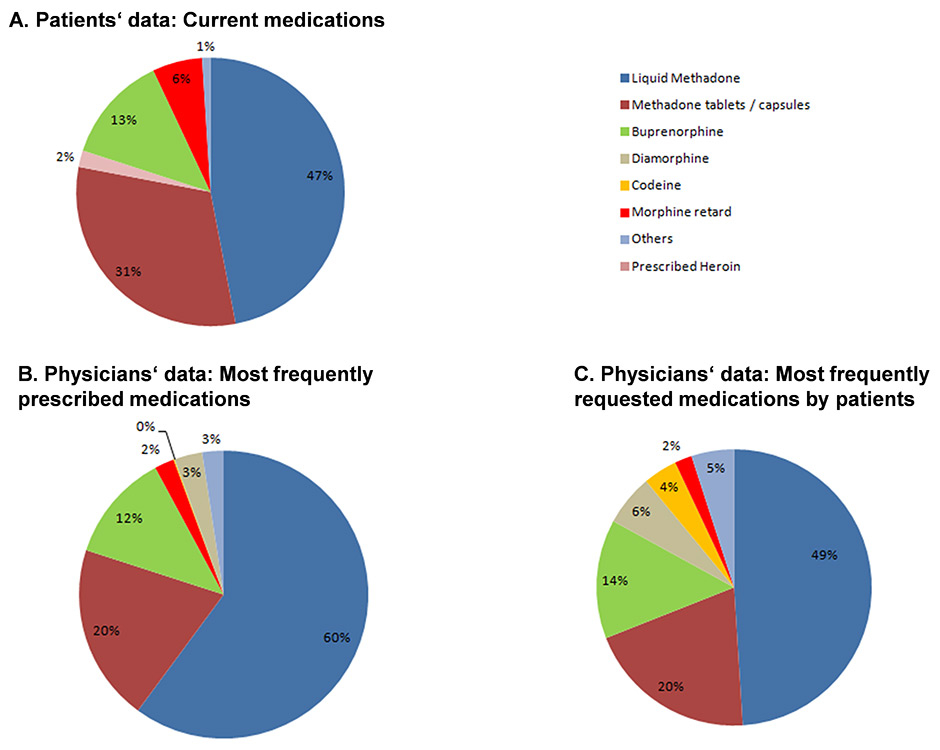
Figure 4
A summary of opioid maintenance therapy medication choices in Switzerland. A. Patients’ current medication. B. Most frequently prescribed medications. C. Medications most frequently requested by patients, as reported by physicians.
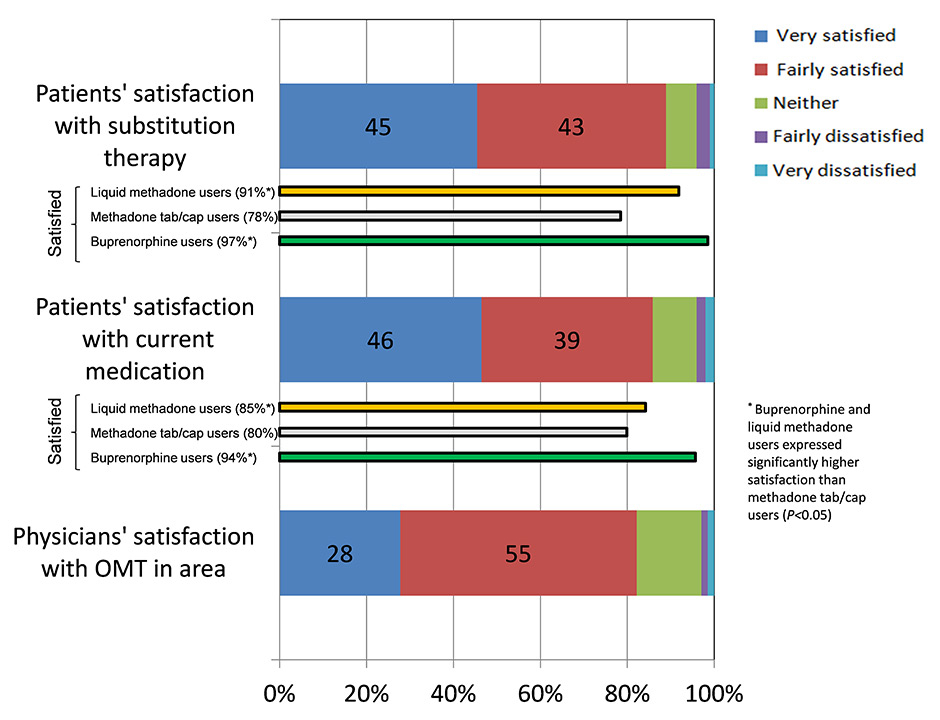
Figure 5
A summary of satisfaction with current medications and opioid maintenance therapy (OMT). The patients’ satisfaction was further stratified according to medications used.
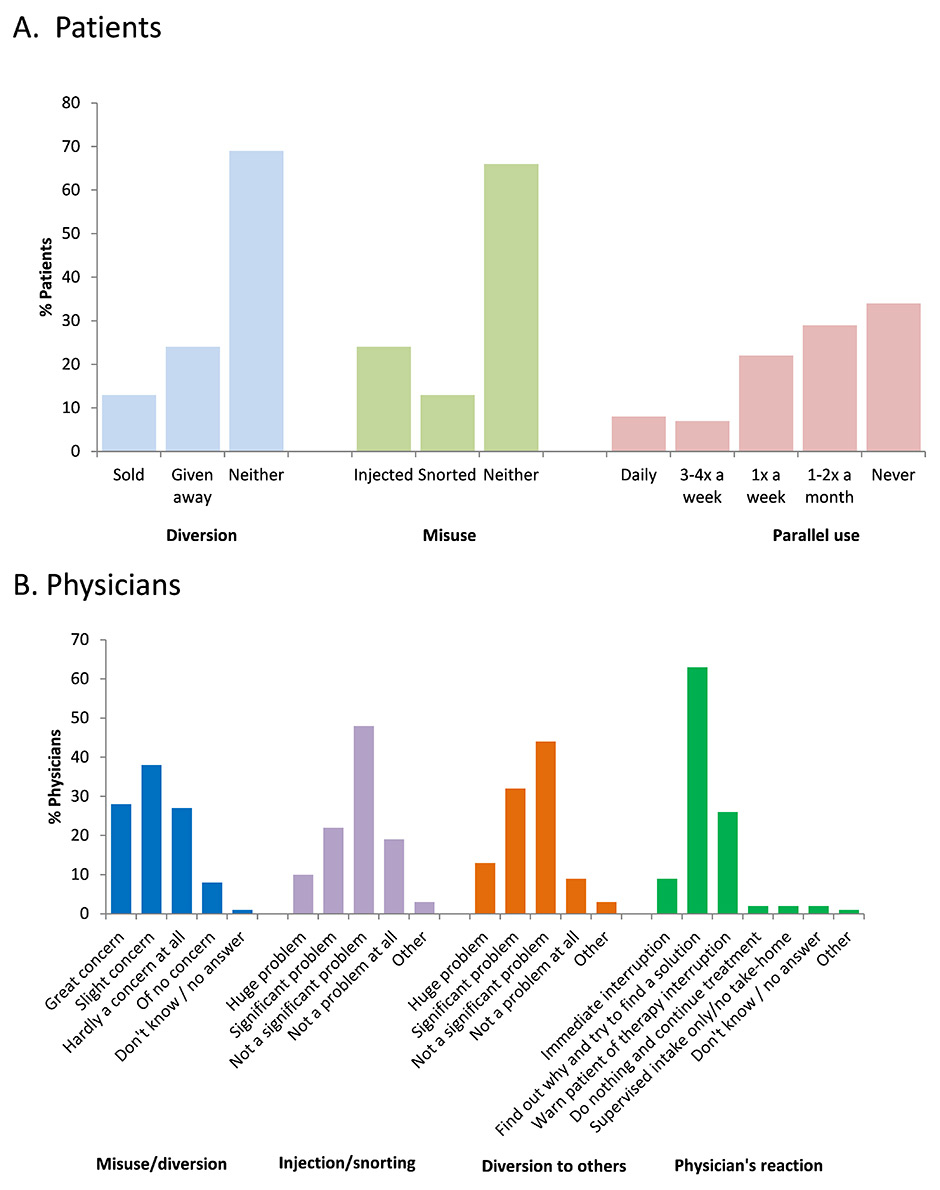
Figure 6
A summary of data on misuse, diversion and parallel use. A. Patient-reported data on the different ways of diversion, and misuse and the frequency of parallel consumption of illicit drugs. B. Physician-reported data on views about misuse and diversion and their reaction to these problems.
A total of 200 (14%) physicians (44% GPs, 33% psychiatrists and 19% internists) completed the survey, with a mean age of 54.1 ± 8.2 (range 33‒70) years.
The majority of the respondents were male (87%), and the largest proportion (79%) worked in a private practice; 16% worked in an outpatient clinic and 6% in a hospital. More than half (59%) reported a caseload of ≤9 OMT patients, 19% treated 10 to 19 patients, and 22% had ≥20 patients. The demographic characteristics of the interviewed physicians by specialty, work setting and years of experience in OMT are given in table 1.
The majority of the respondent physicians (68.5%) were based in the German-speaking part of Switzerland, and 31.5% in the French-speaking regions. The regions of Espace Mittelland (n = 48), Lake Geneva (n = 44) and Zurich (n = 38) accounted for the majority of participants. The regional distribution of the interviewees is shown in figure 2.
Participating physicians from the French-speaking region were significantly older than their counterparts in German-speaking Switzerland (56.5 vs 52.9 years; p <0.01). On average, GPs were significantly older than psychiatrists (56.6 vs 50.1 years; p <0.01); those working in a private practice were significantly older than hospital-based physicians (55.6 vs 48.5 years; p <0.01). The age profile of the participating physicians is summarised in figure 3.
A random sample of 207 patients was included in the study, 87 of whom were recruited from 31 physicians’ practices, and 120 from six support centres (fig. 1). No data on screening failures or drop-out rates among OMT patients were available.
A total of 144 German questionnaires (69.6%) were completed and 63 (30.4%) were in French. An additional 10 patients (all German-speaking) were added to boost the subsample of buprenorphine patients, to be used in specific analyses only.
The canton Zurich and the combined Basel area accounted for 34% and 20% of patients recruited, respectively. The geographic distribution of the patient respondents is shown in figure 2.
The majority of the patients were male (66%) and single (60%). More than half (51%) were unemployed and >92% had finished obligatory schooling or attained secondary and tertiary education
The mean patient age was 39.8 ± 9.3 (range 20‒61) years. On average, patients rated their physical and mental health statuses as mediocre, with little variation between regions. The sociodemographic data of the IMPROVE patients are summarised in table 1.
Nearly half of the physicians (46%) cited social commitment as the main reason for treating patients with OMT, and 24% cited therapeutic efficacy. Social stabilisation of the patient, and reduction of health risks, illegal activities and criminality were the top three most important goals of OMT, reported by 9%, 8.8% and 8.6% of respondents, respectively. Stopping all illegal drug use and achieving a drug-free state were rated as the least important goals.
The majority of patients (79%) started OMT on their own decision. Approximately 34% cited their main motivations for initiating OMT as the desire to improve general health and 30% wanted to end their drug dependence for good. Less than a third (29%) considered the high expense of drug consumption as another important reason for OMT.
In terms of medication choices, data on OMT prescription volume (expressed in % patient load) showed that, on average, physicians prescribed liquid methadone (oral) to 60% of their patients. Methadone tablets and capsules accounted for almost 20% and buprenorphine for over 12% of prescribed volume. Buprenorphine was more likely to be prescribed by psychiatrists and internists (19% and 13% of patient load, respectively) than by GPs (6%; p<0.05). It was also prescribed more often by physicians in hospitals and outpatient clinics (18% of patient load) than in private practice (11%; p<0.05).
Liquid methadone was generally the preferred medication in all regions. Physicians in French-speaking Switzerland prescribed liquid methadone to more than 78% of their patients, significantly higher than physicians in the German-speaking regions (52%; p<0.05). Prescription volume per region indicated a high preference for liquid methadone in the Lake Geneva and Espace Mittelland regions (82% and 70% of patient load, respectively). Buprenorphine had a higher following in the German-speaking (14% of patient load) than in the French-speaking region (8%; p<0.05), and accounted for up to 18% of prescription volume in central and northwest Switzerland. Table 2 summarises physician data on prescription volume of different OMT drugs, broken down by specialisation, work setting and regional distribution.
The reasons cited by physicians for their preference for liquid methadone were personal experience (30% of respondents), safety (21%) and recommendations in guidelines (16%). For methadone tablets and capsules, compliance (35%), usage (30%) and personal experience (21%) were the main grounds for preference. Efficacy (41%), personal experience (41%) and safety (24%) were the top reasons for preferential prescription of buprenorphine by the physicians interviewed.
Physicians were also asked to rate the importance of drug attributes in influencing their prescription choice. Effectiveness in controlling cravings was ranked the most important attribute (8.4%), closely followed by safety and tolerability (8.1%), whereas therapy cost was ranked as the least important (5.5%).
Overall, 39% of physicians stated that patients always or often request a specific substitution medication. This frequency was highest among psychiatrists (53%) and among physicians in outpatient clinics/hospitals (53%), and lowest among GPs (25%; p<0.05). The medication most often requested was liquid methadone (49%), with the highest proportion of requests coming from the Lake Geneva region (79%). The highest frequency of patient requests for buprenorphine was reported in Espace Mittelland (22% of physicians). Of the physicians who received specific requests from their patients, 61% granted the requests ≥70% of the time.
Of the 207 patients interviewed, 47% were on liquid methadone, 31% on methadone tablets or capsules, and 13% on buprenorphine (fig. 4). Other substitution medications used were morphine retard and codeine. Generally, patients had a major influence on the choice of medication, with 48% of patients reporting they were given the option to choose, and 54% given the drug of their choice.
Detailed data on medication use presented by age, gender, employment status and geographic region are presented in table 2. In terms of demographics (including 10 boost patients), methadone tablets were the preferred OMT medication among women (p<0.05). A significantly higher proportion of buprenorphine users were employed (47.2%) compared with methadone liquid and tablet users (28.6% and 21.5%, respectively; p<0.05).
Excluding boost patients, regional differences were noted in terms of OMT medication use. Methadone was generally the drug of choice in all cantons surveyed, with liquid methadone use significantly higher in Vaud (81% of patients) and Bern (77%; p <0.01) compared with other cantons surveyed.
Out of the 200 physicians interviewed, 77% were of the opinion that OMT is easy for patients to access in their geographic area, whereas 11% considered it difficult. The difficulty was attributed mainly to imbalance between therapy supply and demand, as well as the personal problems of the patients.
On a 10–point satisfaction scale, 83% of physicians were satisfied (score 7‒10) with the treatment programmes in their area, and only 2% were dissatisfied (score 1–4). The satisfaction ratings of physicians are shown in figure 5.
The majority (85%) of OMT patients were very (46%) or fairly (39%) satisfied with their current medication. Satisfaction was significantly higher among buprenorphine (94%) and liquid methadone users (85%) compared with users of methadone tablets or capsules (80%; p<0.05). In terms of the overall success of OMT, 88% were very (45%) and fairly (43%) satisfied. Buprenorphine (97%) and liquid methadone (91%) users were significantly more satisfied (p<0.05) with their therapy than users of methadone tablets or capsules (78%). Patient satisfaction is graphically presented in figure 5.
Regional differences in therapy satisfaction were not significant, with a trend towards lower satisfaction in Zurich and Fribourg.
With regards to diversion and misuse, 45% of all physicians interviewed reported that diversion of substances was a significant or huge problem. This perception was similar between German- and French-speaking regions, but was considered most problematic in Eastern Switzerland (63%) and least in Zurich (29%).
About a third (32%) of all doctors considered medication misuse (e.g., injecting, snorting) a huge or significant problem, with a higher problematic rating in the French-speaking region (rated 38% of physicians), especially in the Lake Geneva area (34%).
As reaction to misuse or diversion, 63% of physicians would try to find out the reason for the patient’s action and find a solution; 26% would warn patients of therapy interruption if misuse or diversion persists. Only 9% would resort to immediate therapy cessation. A summary of misuse and diversion data is given in figure 6.
Of the 207 patients interviewed, 66% admitted to using illicit drugs at least one to two times a month; daily use was reported by 8% of respondents. Parallel use of illicit drugs was highest among liquid methadone users (71%) and lowest (53%) among buprenorphine users (p <0.05).
The main reasons for misuse cited were the need to get high occasionally (41%) and the inability of the current therapy to control cravings (20%). There was great variation in availability of medications on the street, with benzodiazepines (69%) and methadone (59%) reported as the easiest to access. It is important to note that 19% of patients declined to answer this question.
About a third (37%) of respondents admitted to having diverted their prescribed medications, with 13% admitting to having sold their drugs and 24% to having given theirs away without financial compensation. Thirty-seven percent admitted to deviating from the officially prescribed use of their OMT drug, with 24% admitting to injecting and 13% to snorting their medications.
| Table 1. Demographic characteristics of study participants. | |||
| Physicians n = 200 | Demographic data | Patients n = 207* | |
| Gender, n (%) | |||
| 173 (86.5) | Male | 137 (66.2) | |
| 27 (13.5) | Female | 69 (33.3) | |
| – | No response | 1 (0.5) | |
| Age (years) | |||
| 33‒70 | Range (min‒max) | 20–61 | |
| 54.06 ± 8.15 | Mean ± standard deviation | 39.77 ± 9.29 | |
| 55 | Median | 41 | |
| Age groups, n (%) | |||
| – | ≤19 years | 1 (0.5) | |
| – | 20–29 years | 33 (15.9) | |
| 8 (4.0) | 30–39 years | 58 (28.0) | |
| 50 (25.0) | 40–49 years | 85 (41.1) | |
| 82 (41.0) | 50–59 years | 25 (12.1) | |
| 57 (28.5) | 60–69 years | 3 (1.4) | |
| 3 (1.5) | >70 years | ||
| – | No response | 2 (1.0) | |
| Specialisation, n (%) | Level of education, [n (%) | ||
| General practitioner | 87 (43.5) | Did not finish school | 16 (7.7) |
| Psychiatrist/psychologist | 66 (33.0) | Finished obligatory school only | 58 (28.0) |
| Internist | 37 (18.5) | ||
| Other | 10 (5.0) | Apprenticeship | 110 (53.1) |
| Matura | 16 (7.7) | ||
| University degree | 7 (3.4) | ||
| Work setting, n (%) | Employment status, n (%) | ||
| Private practice | 144 (72.0) | Unemployed | 106 (51.2) |
| Outpatient clinic | 32 (16.0) | Employed | 62 (30.0) |
| Private practice specialised in addiction medicine | 13 (6.5) | Full time | 23 (11.1) |
| Part time | 39 (18.8) | ||
| Job seeker | 34 (16.4) | ||
| Hospital | 11 (5.5) | Student / job training | 3 (1.4) |
| Don’t know | 2 (1.0) | ||
| Involvement in substitution therapy, n (%) (Mean 16.3 ± 6.7 years) | Relationship status, n (%) | ||
| 1–4 years | 10 (5.0) | Single | 125 (60.4) |
| 5–9 years | 31 (15.5) | Divorced | 41 (19.8) |
| 10–14 years | 41 (20.5) | Living with someone | 23 11.1) |
| 15–19 years | 37 (18.5) | Married | 14 (6.8) |
| 20–24 years | 41 (20.5) | Widowed | 3 (1.4) |
| 25–29 years | 23 (11.5) | No response | 1 (0.5) |
| ≥30 years | 17 (8.5) | ||
| * excluding boost | |||
| Table 2: Medication choices by demographics and by regions – physician- and patient-reported data | |||||||||||||
| Physician-reported data: volume of prescribed OMT medications expressed in mean percentage (%) of patient load by specialisation, work setting and linguistic and regional distribution§ | |||||||||||||
| Medication prescribed | Mean % patient load | Specialisation (%) | Work setting (%) | Linguistic region (%) | Detailed regional distribution (%) | ||||||||
| GP n = 87 | Internist n = 37 | Psychiatrist n = 76 | Private practice n = 157 | OPC/hospital n = 43 | German-speakingCH n = 137 | French-speaking CH n = 63 | Eastern CH n = 32 | Zurich n = 38 | Central & NW CH n = 38 | Espace Mittelland n = 38 | Lake Geneva region n = 44 | ||
| Liquid methadone | 60.1 | 64.3 | 59.0 | 56.0 | 62.7* | 50.7° | 51.8° | 78.3** | 52.7° | 44.1° | 44.6° | 70.1** | 81.9** |
| Methadone tablets/capsules | 19.9 | 23.2 | 25.9 | 13.2 | 19.8 | 20.2 | 24.7 | 9.4 | 23.6 | 32.8 | 29.9 | 11.0 | 7.0 |
| Buprenorphine | 12.2 | 5.9° | 12.8* | 19.0** | 10.6 | 18.0* | 14.3* | 7.5 | 14.5 | 11.2 | 17.9 | 13.2 | 5.2 |
| Patient-reported data: OMT medication by demographics and regional distribution§ | |||||||||||||
| Medication prescribed | Total n = 207 (+10 boost) | Age groups, with boost (%) | Gender, with boost (%) | Employment, with boost (%) | Detailed regional distribution (%), excluding boost | ||||||||
| ≤29 years | 30‒39 years | ≥40 years | Female | Male | Employed | Unemployed + other | BS/BL n = 41 | BE n = 35 | ZH n = 71 | FR n = 29 | VD n = 31 | ||
| Liquid methadone | 98 | 18.4 | 25.5 | 55.1 | 27.6° | 72.4 | 28.6° | 71.4 | 39° | 77** | 37° | 14° | 81** |
| Methadone tablets/capsules | 65 | 12.3 | 32.3 | 55.4 | 43.1* | 56.9 | 21.5° | 78.5 | 41 | 0.0 | 35 | 52 | 26 |
| Buprenorphine | 26 (+10) | 27.8 | 25 | 47.2 | 30.6° | 69.4 | 47.2* | 52.8 | 7 | 17 | 10 | 34 | 0.0 |
| */** Values were tested and found to be significantly different at (**) p <0.01 and (*) p <0.05 compared with number(s) marked ° in the same category. § Percentages may not add up to 100% owing to data on other medications not reported in the table. “Others” included, but were not limited to, morphine, diamorphine, codeine and prescribed heroin. Boost: 10 patients who were buprenorphine users added to boost the sample size to n = 36. Regional distribution excluded boost patients as these only consisted of participants from German-speaking CH. BE = Bern; BS/BL = Basel area; CH = Switzerland; FR = Fribourg; GP = general practitioner; NW = northwest; OPC = outpatient clinic; VD = Vaud; ZH = Zurich | |||||||||||||
The most frequent reason, cited by 70% of physicians, for not treating OMT patients was the difficulty in handling opioid-dependent patients, followed by the current political conditions (15%).
Approximately 64% of physicians agreed that the necessity of attending all appointments was the most important, yet also the most difficult, rule for patients to abide by, thus presenting a major barrier for OMT participation. In corollary to this, the most commonly reported barriers that led to therapy interruption were the inability of patients to adhere to the treatment rules (cited by 79% of physicians), patients changing place of residence (50%) and imprisonment (29%).
In the physicians’ opinion, changes were needed to motivate medical practitioners to engage in OMT. The top two factors that needed to be changed were the lack of training and/or information (cited by 33%) and the financial barriers in relation to doctors’ compensation (20%). In connection with the information gap, only 83% of physician respondents were familiar with the clinical guidelines and joint OMT recommendations of SSAM, VKS and FOPH. Of those who were aware of these Swiss practice guidelines, 83% found them useful in their daily practice.
Current political conditions and framework were also considered by 15% of respondents as a barrier, with changes desired in terms of less bureaucracy, less complicated obligations and more support for OMT physicians.
Regarding quality of patient care, the need for change in the Swiss political framework was cited as most important by 13% of respondents. Other areas for improvement identified were increasing access by patients to OMT (reported by 12%), and enhancing the attractiveness of treating opioid-dependent patients to physicians (10%).
The majority of patients (75%) informed themselves of the different treatment options before initiating OMT and 76% felt they were very well-informed (33%) or well-informed (43%) about OMT. The main sources of information were other drug users, reported by 52% of respondents, followed by counselling or drug support centres (47%), friends and acquaintances (43%) and the OMT physician (41%). However, 21% of respondents felt insufficiently or poorly informed about OMT.
A total of 153 respondents knew of current users who were not in OMT. The reasons reported for not starting therapy were the user’s feeling of being able to cope effectively with the situation (cited by 24%) and not feeling addicted at all (23%). Other reasons included lack of flexibility in therapy appointments (22%) and the long duration until a maintenance dose could be achieved (15%).
Several prerequisites to starting OMT were considered as difficult to meet, especially daily supervised consumption (cited by 70% of respondents), the necessity of attending all appointments (63%) and psychosocial counselling (41%), the long-term goal of a drug-free state (39%) and cessation of all illicit drug use (38%).
Despite Switzerland’s seemingly progressive approach to OMT, the system is far from perfect. Treatment barriers and unmet needs that were identified by the IMPROVE study included political, financial and social problems discussed below. These present opportunities for improving the Swiss OMT model.
The IMPROVE data showed that liquid methadone remained the most common OMT medication preferred by patients and prescribed by physicians in Switzerland. The number of buprenorphine users in Switzerland remains low.
Despite different pharmacological properties, methadone and buprenorphine are both considered to be effective and safe medications in OMT and are given equal merit by the SSAM and the FOPH guidelines [10, 9]. Several clinical trials and systematic reviews have compared the two medications [12–15]. Advantages associated with methadone are higher retention rates, and better patient control and dosage adaptation. Buprenorphine, on the other hand, has the safety advantage of being less proarrhythmic than methadone and allowing faster achievement of steady-state dose without the risk of serious overdose with respiratory depression. In addition, dispensing in intervals of 2 to 3 days is possible for the latter [10], supporting the practice of allowing take-home medications. A main disadvantage of buprenorphine is its higher cost in comparison with methadone.
Some European countries have reported potential shortages in OMT healthcare providers as ageing physicians retire and are not replaced by younger doctors [16, 17]. This trend was reflected in the IMPROVE data, with 31% of physician respondents being 60 years and above. Participating GPs and internists were generally older than psychiatrists, and a similar trend in age difference was also evident between practice-based and clinic/hospital-based physicians. The ageing GPs and the practice-based physicians represented a considerable bulk of the IMPROVE respondents and could well correspond to the real-life demographics of Swiss OMT providers. Even though the number of OMT patients in Switzerland is not necessarily increasing [9, 10], the IMPROVE data on OMT physician demographics indicate a potential imbalance in OMT supply and demand that needs to be addressed before a bottleneck is reached.
Patients’ satisfaction with their treatments is not often analysed. The IMPROVE data showed that, in general, satisfaction with OMT therapy and medications in Switzerland was high. However, although substantial improvements have been made since the open drug scenes in the 1980s, a number of opioid-dependent individuals have not been integrated into OMT. In addition, OMT still generally follows a revolving door pattern of initiation and dropping out. Certain clinical practices were found by IMPROVE patients to be too restrictive and presented as barriers to therapy entry and retention.
Physicians were also generally satisfied with the availability of OMT in their area. However, several factors were identified by the medical professionals as areas for improvement. Based on the respondent physicians’ views, the Swiss political framework, the accompanying bureaucracy, as well as financial issues were identified as barriers that deter physicians from providing OMT. Lack of information and training and the negative perception of OMT patients as being difficult were also cited as hindrances.
In general, high satisfaction with OMT in the Swiss setting was consistent for both OMT patients and treating physicians, although this was not statistically tested.
As an indication of abovementioned information gap, a significant proportion of the treating physicians (17%, unpublished data IMPROVE) were not aware of the current SSAM/VKS/FOPH clinical guidelines on OMT [10], including the existence of effective treatments other than methadone, and the importance of diversification of OMT to optimise and individualise therapy to the needs of the patients. Recently, morphine retard was also approved by Swissmedic for the indication of OMT, providing another treatment option.
The abovementioned shortcomings and other barriers identified by the IMPROVE study need to be addressed in order to increase the willingness of physicians to engage in OMT (and thus address the supply and demand imbalance previously mentioned), optimise treatment outcomes, and improve further the Swiss OMT model.
Unsupervised and take-home doses of substitution medications on weekends and holidays is common practice in Switzerland (unpublished data, IMPROVE) but could present an opportunity for misuse and diversion of OMT medications. Indeed, many OMT patients admitted to snorting or injecting their medications, or giving them away. However, the main motivation for diversion was not necessarily financial gain but rather sharing with other users, indicating minimal involvement of patients in selling prescribed OMT in the black market.
Many physicians were concerned about misuse and diversion although surprisingly many of the IMPROVE respondents did not consider either as a huge problem in their geographic area. As response to the problems, the majority of physicians took a proactive approach, in keeping with the Swiss harm reduction drug policy, by trying to find out reasons for misuse and possible solutions; only very few took the hardline position of immediate OMT interruption.
There were some limitations in the IMPROVE study. The canton of Tessin, which comprise the Italian-speaking part of Switzerland, could not be included in the study because of resource and logistical constraints. However, the largest Italian-speaking city of Lugano ranks only 9th in Switzerland in terms of population size. The number of Italian-speaking participants would have been small and did not justify the additional costs of documentation (e.g., translation of questionnaires and other study documents) and logistics.
Although physicians were instructed to randomly select participating patients, this could not be fully ensured and documented. In addition, only a small number of buprenorphine users could participate in the study, which could have been a source for bias. However, appropriate measures during the analysis were taken to avoid this.
Limitations related to questionnaire-based research also need to be considered. The questionnaires used in this study were not validated instruments, but modelled on those used in previous studies, in order to facilitate comparison, as discussed below.
Finally, limitations inherent to observational cross-sectional studies should be kept in mind when interpreting the results of the IMPROVE study. The representativeness of the IMPROVE populations and their generalisability to other populations could not be confirmed. Owing to the uncontrolled study design, data and comparisons could only be interpreted in a descriptive manner.
Switzerland is not alone in addressing present-day OMT problems. The pan-European project European Quality Audit of Opioid Treatment (EQUATOR) is assessing the current state of opioid-dependence treatment in ten countries across Europe [18]. The questionnaires used in the IMPROVE study were similar but not identical to those used in the EQUATOR study. This is a result of several differences between the Swiss OMT landscape and other European countries. EQUATOR surveyed both OMT patients and out-of-treatment users, whereas IMPROVE only included OMT patients. With the majority of Swiss users in treatment [9], it was not feasible for IMPROVE to enrol enough opioid users not in treatment. Despite these differences, the research design of IMPROVE was comparable enough to that of the EQUATOR survey to allow comparison with data from other countries in future publications.
The subset of IMPROVE data presented here gives a present-day, real-life overview of the OMT landscape in Switzerland which has not been previously assessed and published in any scientific journal. It gives a glimpse into the profile of the present-day OMT Swiss patients as well as those of the current OMT healthcare providers. It also addressed many knowledge gaps in the field of addiction medicine, including treatment satisfaction, unmet needs, the prevalence of misuse and diversion and the common barriers to therapy.
The dataset represents a valuable resource for policy makers, key opinion leaders and drug addiction researchers and will be a useful basis for improving the current Swiss OMT model. Further publications on other important aspects of the IMPROVE study is planned.
Acknowledgement: The authors would like to acknowledge Dr. med. Johannes Strasser, Dr. med. Marc Vogel, and Dr. phil. Ken Dürsteler-MacFarland of the Centre for Substance Use Disorders, Psychiatric Hospital of the University of Basel for their invaluable support in the study conduct.
1 World Health Organization. Guidelines for the Psychosocially Assisted Pharmacological Treatment of Opioid Dependence. 2009.
2 Federal Office of Public Health (FOPH). Switzerland’s National Drugs Policy: The federal government’s third package of measures to reduce drug-related problems (MaPaDro III). 2006−2011.2006.
3 Hedrich D. European report on drug consumption rooms. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA. 2004.
4 Klingemann HK. Drug treatment in Switzerland: harm reduction, decentralization and community response. Addiction. 1996;91(5):723–36.
5 Huissoud T, Rousson V, Dubois-Arber F. Methadone treatments in a Swiss Region, 2001-2008: a registry-based analysis. BMC Psychiatry. 2012;12:238.
6 Dürsteler-MacFarland KM, Vogel M, Wiesbeck GA, Petitjean SA. There is no age limit for methadone: a retrospective cohort study. Subst Abuse Treat Prev Policy. 2011;6:9.
7 Nordt C, Landolt K, Stohler R. Estimating incidence trends in regular heroin use in 26 regions of Switzerland using methadone treatment data. Subst Abuse Treat Prev Policy. 2009;4:14.
8 United Nations Office on Drugs and Crome (UNODC). World Drug Report. 2011.
9 Vogel M, Petitjean S, Borgwardt S, Wlesbeck GA, Walter M. Therapie der Opioidabhängigkeit: Ein Update. Schweizer Archiv für Neurologie und Psychiatrie. 2010;161(1):5–13.
10 Federal Office of Public Health (FOPH). Substitution-assisted treatment in opioid dependence. October 2009.
11 Stohler R, Nordt C, Falcato L, Dürsteler-MacFarland KM, Rössler W. Wie effektiv sind Methadonbehandlungen in Privatpraxen? Soz.- Präventivmed. 2004;49:276–80.
12 Petitjean S, Stohler R, Déglon JJ, Livoti S, Waldvogel D, Uehlinger C, et al. Double-blind randomized trial of buprenorphine and methadone in opiate dependence. Drug Alcohol Depend. 2001;62(1):97–104.
13 Uehlinger C, Déglon J, Livoti S, Petitjean S, Waldvogel D, Ladewig D. Comparison of buprenorphine and methadone in the treatment of opioid dependence. Swiss multicentre study. Eur Addict Res. 1998;4(Suppl 1):13–8.
14 Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2008;(2):CD002207.
15 Ducharme S, Fraser R, Gill K. Update on the clinical use of buprenorphine: in opioid-related disorders. Can Fam Physician. 2012;58(1):37–41.
16 Stöver H. Barriers to opioid substitution treatment access, entry and retention: a survey of opioid users, patients in treatment, and treating and non-treating physicians. Eur Addict Res. 2011;17(1):44–54.
17 Goulão J, Stöver H. The profile of patients, out-of-treatment users and treating physicians involved in opioid maintenance treatment in Europe. Heroin Addict Relat Clin Probl. 2012;14(4):7–22.
18 Fischer G, Stöver H. Assessing the current state of opioid-dependence treatment in Europe: methodology of the European Quality Audit of Opioid Treatment (EQUATOR) project. Heroin Addict Relat Clin Probl. 2012;14(3):5–70.
Funding / potential competing interests: The IMPROVE study was funded by Reckitt-Benckiser (Switzerland) AG. The study conduct, data collection and data analyses were implemented by Ipsos Healthcare (formerly Synovate) of Hamburg, Germany. Medical writing support was provided by Clinipace Worldwide AG (Switzerland).