Figure 1
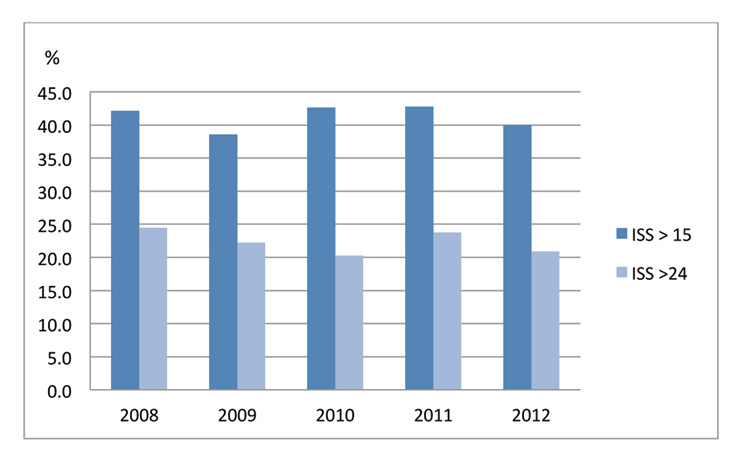
Annual incidence of severely (ISS >15) and seriously injured (ISS >24).
ISS = injury severity score
DOI: https://doi.org/10.4414/smw.2014.13958
Trauma is worldwide the leading cause of death amongst patients under 44 years of age and the fourth leading cause of death in high-income countries [1]. Many survivors face long rehabilitation and difficult reintegration into their previous life, leading to an important socioeconomic burden [2]. Switzerland is a small, densely populated high-income country of 8 million inhabitants, showing a wide range of differences in urbanisation and geographical settings. It has one of the longest life expectancies in the world and with 3.8 hospitals per 100,000 inhabitants it has numerous care providers [3]. This comes at a significant cost, with Switzerland’s spending on health being the highest worldwide. As of today, national data on incidence, epidemiology and outcome of injured patients are limited to reports from the federal office of statistics, the national insurance company for occupational accidents and the nongovernmental Swiss council for accident prevention. These publicly accessible data have several limitations for medical and epidemiological research, mainly because the classification of injury is not in line with internationally recognised definitions [8]. Furthermore, indications for hospital admission and length of stay are highly dependent on organisational and local conditions and can therefore not be compared internationally. As demonstrated in the United States since the mid-eighties and later in several European countries, a prospective collection of demographic, physiological and time-based parameters of consecutively admitted trauma patients is a key component in optimised efficiency and quality of trauma care [9].
Until recently, trauma care in Switzerland has been provided by numerous hospitals without an integrated and area-wide organised system. Specialist care for the severely injured is cost and resource consuming, with important planning needs in order to provide the required 24-hour availability of specific competences. In 2010, in an effort to improve efficiency, reduce costs and concentrate resources, the Swiss government included trauma care in the field of “highly specialised medicine”. Twelve of the biggest hospitals nationwide were designated to act as dedicated trauma centres. The chosen institutions had to sign a convention stating their ability and willingness to provide a defined number of trauma-specific facilities 24/7 and to develop a structure of trauma-specific education and research as well as to adhere to a future national trauma registry. Trauma centre designation will be reassessed by 2015 based on an analysis of registry data and compliance with the signed agreement.
In an effort to optimise resource allocation and with the aim to assess and consequently amend trauma care, the Lausanne University Hospital (CHUV), an academic tertiary centre, already designed in 2008, the first sustained trauma registry in Switzerland. The principal aim was to assess the incidence, pattern of injury and mortality rate of trauma patients admitted to our institution. The second aim was to conduct a gap analysis identifying potential deficiencies of the available resources in order to provide local and regional health authorities with data to support planning for system solutions.
As a prelude to the launching of the Swiss national trauma registry, this study provides an overview and analysis of demographics, injury patterns and outcome of trauma admissions over 5 years at the second largest university hospital in Switzerland. To our knowledge, this is the first comprehensive report about internationally comparable medical data on trauma admissions to a Swiss trauma centre.
Within the Lausanne Trauma Registry we analysed prospectively collected data consecutively over a 5-year period (1 January 2008 to 31December 2012) of admitted trauma patients. Ethical approval for collecting data based on patient’s hospital files was obtained from the Human Research Ethics Committee of Canton of Vaud (number of the approval: 66/13). Waiver of approval was granted since no prospective intervention was made.
The city of Lausanne is the fourth largest city in Switzerland with 138,000 citizens. The surrounding area is rural and confined by Lake Geneva, the Jura and the Alps. The CHUV is at the same time the local hospital for the city of Lausanne and the academic tertiary centre of referral for the 730,000 inhabitants of the canton of Vaud, the third largest state in Switzerland. With 1,200 beds, CHUV is the second largest hospital in Switzerland and one of the two national, major burn centres. It offers 24/7 a full range of surgical specialties and interventional radiology, two dedicated emergency operating rooms and one 34–bed medical-surgical intensive care unit. Admission criteria for the trauma shock room are all injuries with a potential immediate threat to survival, as well as neurological injuries. Shock room management follows a multidisciplinary surgeon-lead team approach, including anaesthetists, emergency physicians, radiologists and dedicated nurses. Treatment strategies follow advanced trauma life support (ATLS®) principles and standardised treatment algorithms. It is associated with a thoroughly organised prehospital system with a fast response car and a locally based rescue helicopter, both physician-staffed 24/7. This physician-based prehospital organisation acts as a triage tool, determining patient destination on the basis of pattern of injury, physiological and geographic components [10, 11].
The Lausanne Trauma Registry contains consecutive demographic, physiological and outcome data from all trauma patients admitted to the CHUV shock room. Burns, drowning and hanging are recorded as trauma and therefore included. Epidemiological data, vital signs, therapeutic measures, imaging and laboratory tests for every period throughout the chain of rescue, including prehospital phase, shock room, operating theatre, intensive and intermediate care unit are recorded.
Patient’s core data are automatically entered by the hospital admission database securing patient identification and traceability. Physiological data are entered by a specifically trained data manager based on electronic patient files. Severity of each sustained injury is coded in accordance with the international standard Abbreviatted injury scale / injury severity score (AIS/ISS), version AIS2005 (Update 2008) [8] by a certified coder according to the Association for the Advancement of Automotive Medicine (AAAM). Systematic quality assurance is undertaken on a predefined regular basis under the supervision of the first three authors. The registry respects the Utstein minimal dataset [12] and is structurally in line with the American National Trauma Data Bank (NTDB), the British (UK-TARN) and the German registry (DGU), allowing for comparative analysis. According to the international definition, severe injury is defined as an Injury Severity Score (ISS) >15 and critical injury is defined as an ISS >24 [8]. Seriously injured body regions were defined as an abbreviated injury severity score (AIS) ≥3 [8].
Nonparametric data were reported as medians with interquartile ranges (IQRs) and compared using the Mann-Whitney test. Chi-square test was used to compare proportions. Significance was assigned at the p <0.05 level. Data were analysed with JMP 10.0.0. statistical software (SAS Institute Inc.).
| Table 1:Demographics. | ||
| All patients | ISS >15 | |
| Gender (M/F) (%) | 74.6 / 25.4 | 74.5 / 25.5 |
| Age (median, IQR) | 38.8 (23–7–56.2) | 45.1 (25.1–62.9) |
| ISS (median, IQR) | 13 (5–22) | 25 (18–29) |
| Pre-injury ASA class (median, IQR) | 1 (1–2) | 2 (1–2) |
| Age over 65 years (%) | 15.4 | 22.6 |
| Mechanism of injury (%) | ||
| Fall | 34.3 | 39.6 |
| Motor vehicle accident | 30.9 | 34.2 |
| Pedestrian hit by vehicle | 5.4 | 7.5 |
| Pedal cyclist | 4.1 | 4.9 |
| Fire | 9.3 | 5.1 |
| Others | 15.9 | 8.7 |
| ASA = American Society of Anesthesiologists; IQR = interquartile range; ISS = injury severity score | ||
During the study period, a total of 1,599 patients were admitted to the shock room of CHUV for potentially life-threatening injuries. Patients were predominantly healthy males with a median age of 41.4 years (table 1). Over the 5 years, the rate of shock room admission did not vary significantly with a median of 323 (305–333.5) patients per year. Median injury severity score was 13 (5–22). Overall, 672 (42.0%) presented with severe injuries and 379 (24.8%) with critical injuries, corresponding to a median annual trauma intake of 134 (123.5–139) patients with ISS>15 (fig. 1). Elderly patients over 65 years represented 15.4% of the entire trauma workload. Principal mechanisms of injury were road traffic incidents (RTIs) (40.4%) followed by falls (34.3%). Although four-wheel vehicles were most frequently involved (19.1%), two-wheel vehicles (15.6%) were implicated in 38.6% of all RTIs. Pedal cyclists accounted for 4.1% of the annual trauma workload and 5.4% were pedestrians hit by vehicles (13.4% of all RTIs). Falls leading to shock room admission were mainly from an elevated level above 1 meter (20.3%), whereas falls from standing height accounted for 14% of admissions. Of these low-height falls, 42.4% presented with an ISS >15, compared with 51.2% for falls from levels higher than 1 metre. Accidents were predominant (85.9%) and 125 (7.8%) admissions were due to self-inflicted injuries and 101 (6.3%) due to assault.
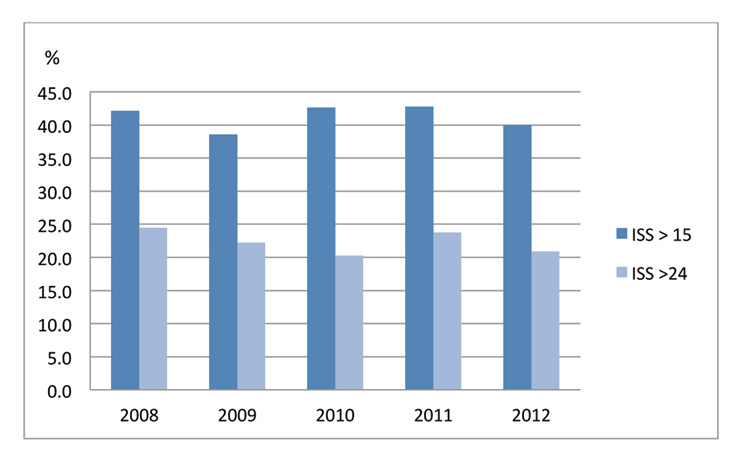
Figure 1
Annual incidence of severely (ISS >15) and seriously injured (ISS >24).
ISS = injury severity score
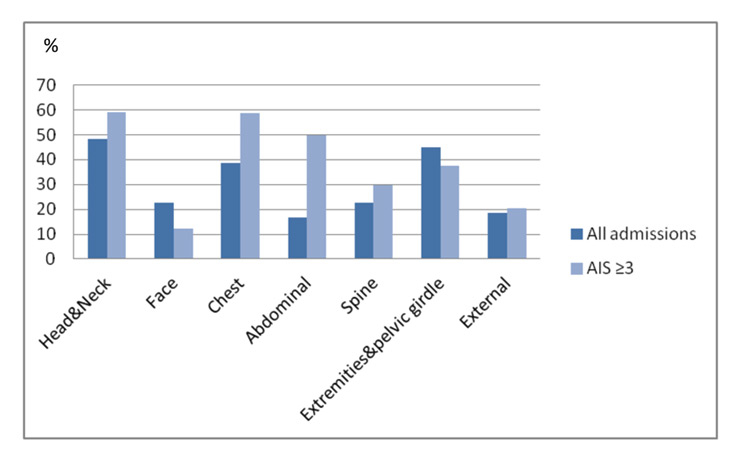
Figure 2
Incidence of injury in each body region, overall and severe (AIS score ≥3).
AIS = abbreviated injury scale.
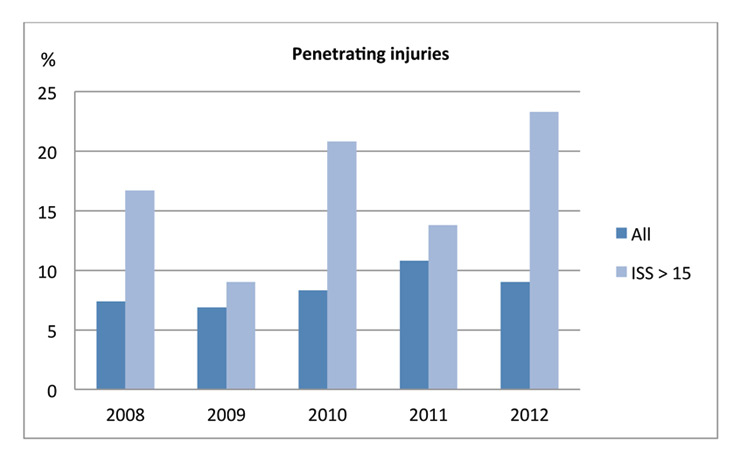
Figure 3
Annual incidence of penetrating injuries, overall and amongst severely injured patients.
ISS = injury severity score
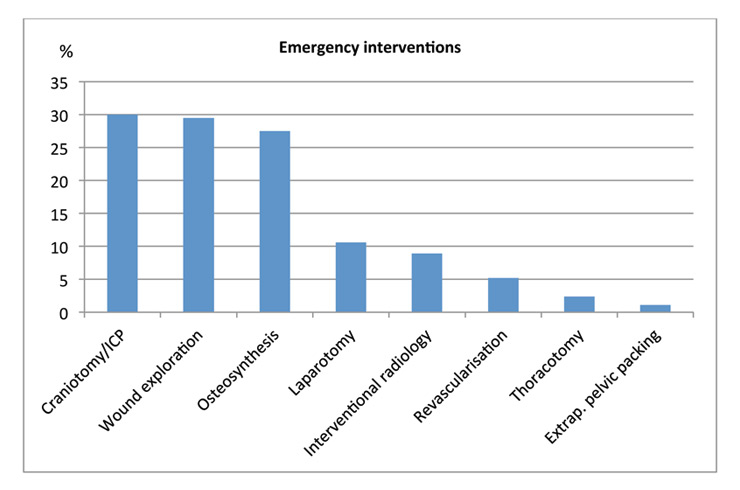
Figure 4
Incidence of operative emergency interventions.
Prehospital transport was mostly done by a physician-staffed team (84.2%), either by helicopter (56.8%) or by car (27.4%); 158 patients (9.9%) were admitted by paramedics without medical bystander. two hundred and seventy-eight (17.5%) admissions were secondary referrals, with 28.3% being burn patients. A total of 926 (57.9%) admissions occurred outside standard working hours, either between 7 pm and 7 am (39.1%) or on Saturday or Sunday (33.7%).
Prevalent patterns of injury were traumatic brain injuries (64.4%), thoracic trauma (59.8%) and injuries to extremities and the pelvic girdle (52.9%). Within each injured body region, severe injuries were observed in 59.3% in the head and neck area, in 58.7% in the chest and in 49.9% in the abdomen. Severe orthopaedic injuries, taking spine and pelvic/extremity injuries together, accounted for 67.1% of all serious injuries (fig. 2).
Blunt injuries accounted for 91.5% of admissions. Amongst the 136 (8.5%) penetrating injuries, 18.4% were due to gunshots, which equal a 1.6% rate of firearm-related cases of severe trauma. In 60%, self-harm was the intent for gunshot-related injuries. Overall median severity of penetrating injury was 4.5 (1–10) (fig. 3).
Overall, 466 patients (29.1%) underwent an emergency intervention (defined as an immediate transfer from shock room to the operating room or the angiographic facility; fig. 4). Main specialties involved were orthopaedic surgery (27.3%) and neurosurgery (26.3 %), followed by plastic surgery for burn care (15.4%) and visceral surgery (13.9%). Emergency angiography and embolisation was performed in 8.8% of patients as part of the initial haemostatic procedure. Overall, 700 (43.8%) had a surgical/radiological intervention within the first 24 hours after admission and 59.1% of patients had at least one surgical intervention during their hospital stay.
A total of 708 (44.3%) patients required admission to the intensive care unit (ICU) for a median length of stay (LOS) of 4 days (2–11) and 575 (81.2%) needed invasive mechanical ventilation. In-hospital LOS overall was 7 days (2–17), and 8 days (2–19) if considering survivors only.;18.2% of survivors were hospitalised for less than 24 hours and 12.5% of these were discharged home. Overall readmission rate within 48 hours was 3.2%. Over the 5 years, in-hospital mortality for severely and critically injured patients was 26.2% and 39.1%, respectively.
| Table 2: Outcome. | ||
| All patients | ISS>15 | |
| LOS in hospital (d) | 7 (2–17) | 11 (4–23) |
| LOS in ICU (d) | 4 (2–11) | 5 (2–12) |
| LOS in hospital (survivors) (d) | 8 (2–19) | 15 (8–29) |
| In-hospital mortality | 12.6% | 26.2% |
| ICU = intensive care unit; LOS = length of stay; ISS = injury severity scale | ||
This first registry-based analysis of 5 years of trauma care in a Swiss University hospital demonstrates that our institution annually treats 320 trauma patients with potentially severe injuries. Our demographic findings are typical for those of an urban area in a western first-world country, with trauma patients being mainly males in their early forties [5, 13]. Although the actual rate of “elderly” trauma patients is similar to the reports from high-volume American trauma centres [14], rising numbers have to be expected. A recent study has revealed an 18% increase of injury rates amongst patients older than 65 years over the last 15 years [15]. Although we have not seen a similar trend over the study period, with increasing life expectancy and sustained independence, we need to be prepared to see a growing geriatric trauma population over the coming years, often with more complex medical histories and treatments, requiring prolonged hospital stays, and which are more prone to complications as multiorgan failure and death [16].
As observed in the majority of the surrounding European countries, blunt trauma represented the predominant type of injury, commonly resulting either from fall or from motor vehicle accidents. Interestingly, at 40.4% Lausanne University Hospital sees a higher rate of road traffic related trauma admissions than for example the United Kingdom (33%) [13] or the United States (35.2%) [6]. This might be related to the proximity to one of the busiest highways in Switzerland and is further supported by a comparative report indicating that rates of road traffic related deaths are higher in Switzerland (47 per million inhabitants) than in Great Britain (43 per million inhabitants) [7] but lower than in Germany (55 per million inhabitants), which reported a road traffic related trauma workload of 55.9% [5].
The majority of our trauma patients presented with traumatic brain injuries and thoracic and extremity injuries. The rate of 38% of severe brain injuries accounted for an annual incidence of approximately 120 patients. This exceeded previous estimates based on a national cohort study of severe brain trauma in Switzerland [17]. In comparison with data from the 10-year report of the German trauma registry [5], in CHUV, we observed more severe head injuries (68% vs 54.4%) and pelvic/extremity injuries (40% vs 31.3%) in severely injured patients. This finding might be related to the high rate of two-wheel trauma. Recreational biking is frequent in alpine Switzerland and motorbikes are amongst the preferred means of transport. Motorbike-related injuries therefore accounted for 28.5% of all road traffic incidents, which is above reported rates (22.2%) [5]. A study including 13 trauma centres in California reported a motorbike related trauma workload of only 4.3% [18]. Also, the incidence of severely injured pedal cyclists was comparable to that in major European cities [19].
Rates of penetrating injuries vary widely across Europe. An overview of penetrating trauma in England and Wales reported rates of 3.7% [20], a Scandinavian study 9%–12% [21] and major European cities such as London report up to 21% [22] of penetrating trauma. Our rate of 8.5% remained unchanged over the observed period and the overall median severity of injury was low. However, we observed a trend towards more severe injuries over the years. The rate of assault-related injuries approached rates seen in major European cities such as Lyon, France’s third largest city (9%) [23]. Although Switzerland is known to be amongst the countries with the highest militia gun ownership rates in the world, gunshot related trauma admissions were rare and in the majority self-inflicted injuries. The rate of 7.8% self-inflicted injuries was higher than in German reports (4.7%) [5] and in studies from the United States and Australia [24, 25].
An essential component of a regionalised trauma system is the concept of trauma bypass, in which severely injured patients are transported directly to designated competence centres, bypassing local hospitals. This process has been demonstrated to lead to reduced mortality and morbidity [26–28].
Our rate of secondary referrals of 17.4% was high, as compared with a report from a Dutch Level I trauma centre (7.1%) [29]. Inclusion criteria in the Dutch paper were limited to adults older than 18 years, whereas our registry includes children, which limits the number of attending hospitals and potentially leads to more secondary transfers. Further, the fact that CHUV serves as one of the two major burn centres in Switzerland might contribute to the high referral rate. Secondary referrals of trauma patients initially managed at a smaller hospital are an important indicator for prehospital triage process and in-depth analysis of these data will be crucial for further system planning.
Approximately 30% of all shock room patients underwent an immediate emergency intervention. This rate was almost 20% above those reported from the United States [6] and Sweden (11.4%) [30], and higher than rates in a level I centre in Sydney (18.2%) [31]. If subdivided into the different surgical specialities involved, the operative emergency interventions per speciality were scarce. This finding constitutes an important organisational issue and may affect the possibility and motivation to provide prompt readiness of a multidisciplinary surgical team. Subspecialisation in what has formerly been called “general surgery” made planning for 24-hour presence of broad band surgical competence difficult, although this trend has led in many, mainly American, centres to the creation of “acute care surgeons” [32, 33],CHUV plans to enhance specific competence with the support of fellowships in high volume trauma centres and specific training courses for trauma-interested doctors. Overall, the number of surgical interventions during the hospital stay was lower (59.1%) than in the German population (73.1%) [5] or as reported in a study on blunt trauma in England and Wales (69 %) [13], but higher than the rate of 28.8% in an urban Australian centre [31]. Analysis of both differences in rate of emergency intervention and delayed surgical approach will need a prospective comparative analysis in order to be interpretable in terms of indications and timings.
Trauma care is cost- and resource-intensive. In the United States, care for the severely injured ranked second after heart diseases in the list of US healthcare spending, accounting for approximately 10% of the entire US medical expense [34, 35]. The rate of 12.5% of patients being discharged home within 24 hours might be considered as over-triage to shock room care; 77.3% of the over-triaged patients were admitted by medicalised prehospital team. Overall quality of triage to trauma centres will be an important part of the analysis from a cost containment perspective. A recent US study showed that over-triage to a trauma centre for patients who did not meet field triage criteria were responsible for 40% of costs for acute injury care [36]. Reappraisal of key words may be a valuable first step towards optimised triage. Although the nonelective readmission rate has been identified as a quality indicator for trauma care [37], published data is scarce. Battistella et al. reported a rate of 1.4% of overall nonelective readmission after trauma [38], and a recent report indicates a 4.2% rate of unplanned readmission within 30 days after orthopaedic surgery [39]. The pathway of care of the 47 patients who required readmission within 48 hours in our institution will need to be analysed in depth in order to evaluate whether post-hospitalisation complications might have been prevented if the patients had remained longer in the hospital.
The majority of patients with potentially severe injuries arrived outside working hours, underlining the need for a 24-hour readiness of trauma specialists in all major trauma centres – another cost- and resource-intensive issue. However, although the cost of trauma care provided in a major trauma centre is higher than at nonspecialised hospitals [40, 41] trauma centres have proven to be cost effective, particularly for younger patients with more severe injuries [40].
In CHUV, the mortality rate for severely injured patients with ISS >15 was 26%, which is higher than rates from trauma centres in the United States or Europe [42, 43]. A major trauma centre in London reported a mortality rate of 17.5%, with a steep drop after important restructuring of their system of trauma care [42]. A Dutch study reported a mortality rate of 18.8% [44] and an Italian centre reported a rate of 21% [43]. The 10–year report of the German Society of Emergency Surgery DGU described a mortality rate of 11.6%, which underscores our rate even when we consider only DGU-eligible patients (24.2%) [5]. Looking only at severely injured patients, median injury severity of our population (25) was higher than that described in the English paper (13) and above the those cited in the German (19.3) and Dutch (22) populations. In addition, we observed up to 30% higher prevalence of severe head injuries in our population, which might further contribute to these differences. The higher rate of self-inflicted injuries might also contribute, as intentional injuries have been linked to higher mortality [25].
Nevertheless, crude mortality rates must be used carefully for benchmarking between trauma centres. Without checking for case mix adjustment and systematic preventability assessment, these numbers alone are insufficient to make any judgement about the quality of the care provided. Assessment of preventable deaths rates by in-depth analysis of the entire pathway of care by a panel of specialists is an internationally used benchmarking tool and the only evidence-based performance indicator in trauma care [45]. Based on the aforementioned data we started a performance improvement programme assessing all trauma deaths by a panel peer-review in order to check and assess potential preventability. Our mortality rate of 26% is actually lower than that reported by hospitals before the introduction of systematic efforts for trauma care and regional planning [42]. With the implementation of a specialist trauma service and the institution of a solid clinical governance programme, in addition to nationwide improvements in system planning, the authors of this landmark paper reported a reduction of 48% of their mortality rates within 5 years. Further, they showed significantly reduced LOS and rates of preventable deaths [42]. With the creation of a national trauma registry, allowing for system planning and concentration of severely injured patients to specialised competence centres, similar reductions in mortality rates over the coming years are a realistic perspective.
The newly created Swiss trauma registry is planned to be launched in 2014. The steering committee of this national project chose to be compatible with the German Trauma registry DGU. CHUV will therefore have to enlarge the inclusion criteria to encompass all hospital admissions for trauma with ISS >15 and/or those with serious head injuries. With these changes, the actual number of around 134 severely injured patients per year is estimated to rise above 200 patients annually. Therefore, our trauma workload will be close to fulfilling the workload requirement of the American College of Surgeons Committee on Trauma for Level-1 trauma centre certification (minimal requirement of 240 severely injured patients per year) and be comparable to major trauma centres in Europe such as the Amsterdam Academic Medical Center with around 230 severely injured per year [46], or the Rigshospitalet in Copenhagen with 250 severely injured patients per year (http://www.rigshospitalet.dk/). Regionalised trauma care and designation of trauma centres have shown to improve survival among seriously injured adults and children [27, 47, 48]. With data provided by the future national trauma registry, authorities will hopefully be able to further concentrate the care of severely injured in high competency centres, ensuring a sufficient exposition of dedicated teams and systems.
A trauma centre in Switzerland sees a fair amount of severe trauma, justifying the implementation of important structural and clinical measures necessary to provide a systematic approach. Trauma admissions to the Lausanne University Hospital CHUV are comparable to other first-world European countries in terms of demographic data and injury patterns. Overall, injury severity and incidence of severe head injuries were higher than reported from nearby systems. Further, rates of assault and self-inflicted injures showed equally a higher incidence. Mortality rates are higher than reported from other European systems. Prospective comparative studies, within Switzerland and beyond, are needed for case-mix adjusted comparison, gap-analysis and the definition of strategies allowing for optimisation of the care pathway.
The principal aim of a regionalised trauma system is to minimize preventable trauma deaths and there is a large body of evidence showing the positive impact of trauma centre designation on outcomes and reduction of preventable mortality. Although later than other European countries, Switzerland has now started to address trauma care in a systematic manner. With the implementation of a nationwide benchmarking tool, initial results of the assessment of the currently provided care are expected by 2015 and will guide further organisational steps. It is hoped that this process will be guided by a needs assessment exempt of political interests allowing for concentration of care of the severely injured in a limited number of highly specialised facilities. Switzerland will hopefully take advantage of the experience of our predecessors and integrate the need for a solid performance improvement programme, including systematic assessment of preventable deaths into the basic requirements for trauma centre certification. Following our neighbouring countries, we need to recognise severe trauma as a generalised disease and move away from a multiple speciality approach to an integrative multidisciplinary strategy. As demonstrated by Davenport et al. [42], with regionalised system planning and trauma centre designation, including designated leadership of a multidisciplinary trauma service and a formal performance improvement programme, we should aim at significant reduction of mortality rates and improved recovery within the coming 5 years.
This 5-year review of trauma admissions and care in a Swiss University Hospital provides an important first step for the engaged effort for local trauma centre planning and the setup of an area-wide trauma system in Western Switzerland. It may also help to extrapolate and anticipate the organisational needs for other trauma centres in Switzerland in anticipation of the first results from the future national trauma registry.
Acknowledgment:Thanks goes to the collaborative and participating departments of acute trauma care, notably the departments of Anaesthesiology (Pr. Chr. Kern), Emergency medicine (Prof. B. Yersin), General Surgery (Prof. N. Demartines), Intensive care medicine (Prof. P. Jolliet), Interventional Radiology (Prof. A. Denys), Neurosurgery (Prof. Levivier), Orthopaedic and trauma surgery (Prof. A. Farron).
1 National Confidential Enquiry into Patient Outcomes and Death: Trauma: who cares? [http://www.ncepod.org.uk/2007t.htm],
2 Atlanta (GA): Centers for Disease Control and Prevention 2006. The incidence and economic burden of injury in the United States. Available from: http://www.cdc.gov/ncipc/factsheets/CostBook/Economic_Burden_of_Injury.htm. [Last accessed on 2013 Jan 12]
3 http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/03/01/key/01.html, [Last accessed on 2013 November 8].
4 http://www.bfs.admin.ch/bfs/portal/en/index.html [Last accessed on 2013 October 10].
5 DGU Annual report. Available at: http://www.traumaregister.de/images/stories/downloads/englisch/TR-DGU_annual_report_2013.pdf [Last accessed on 2013 October 16]
6 NTDB Annual Report 2012. Available at: http://www.facs.org/trauma/ntdb/ntdbannualreport2010.pdf. [Last accessed on 2013 May 12]
7 Annual report 2012 of the Swiss Council of Accident Prevention. Available at: http://www.bfu.ch/PDFLib/1415_75.pdf
8 Rating the severity of tissue damage. I. The abbreviated scale. JAMA: the journal of the American Medical Association 1971;215:277–80.
9 Moore L, Clark DE. The value of trauma registries. Injury. 2008;39:686–95.
10 Carron PN, Taffe P, Ribordy V, Schoettker P, Fishman D, Yersin B. Accuracy of prehospital triage of trauma patients by emergency physicians: a retrospective study in western Switzerland. European journal of emergency medicine: official journal of the European Society for Emergency Medicine 2011;18:86–93.
11 Schoettker P, Ravussin P, Moeschler O. Ejection as a key word for the dispatch of a physician staffed helicopter: the Swiss experience. Resuscitation. 2001;49:169–73.
12 Ringdal KG, Coats TJ, Lefering R, Di Bartolomeo S, Steen PA, Roise O, et al. The Utstein template for uniform reporting of data following major trauma: a joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008;16:7.
13 Christensen MC, Ridley S, Lecky FE, Munro V, Morris S. Outcomes and costs of blunt trauma in England and Wales. Critical care. 2008;12:R23.
14 Adams SD, Cotton BA, McGuire MF, Dipasupil E, Podbielski JM, Zaharia A, et al. Unique pattern of complications in elderly trauma patients at a Level I trauma center. J Trauma Acute Care Surg. 2012;72:112–8.
15 Ciesla DJ, Pracht EE, Tepas JJ, 3rd, Cha JY, Langland-Orban B, Flint LM. The injured elderly: a rising tide. Surgery. 2013;154:291–8.
16 Kruger AJ, Soreide K. Trimodal temporal distribution of fatal trauma – fact or fiction? Injury. 2008;39:960–1; author reply 1–2.
17 Walder B, Haller G, Rebetez MM, Delhumeau C, Bottequin E, Schoettker P, et al. Severe Traumatic Brain Injury in a High-Income Country: An Epidemiological Study. J Neurotrauma. 2013.
18 Talving P, Teixeira PG, Barmparas G, Dubose J, Preston C, et al. Motorcycle-related injuries: effect of age on type and severity of injuries and mortality. J Trauma. 2010;68:441–6.
19 Manson J, Cooper S, West A, Foster E, Cole E, Tai NR. Major trauma and urban cyclists: physiological status and injury profile. Emergency medicine journal: EMJ. 2013;30:32–7.
20 Christensen MC, Nielsen TG, Ridley S, Lecky FE, Morris S. Outcomes and costs of penetrating trauma injury in England and Wales. Injury. 2008;39:1013–25.
21 Kristiansen T, Soreide K, Ringdal KG, Rehn M, Kruger AJ, Reite A, et al. Trauma systems and early management of severe injuries in Scandinavia: review of the current state. Injury. 2010;41:444–52.
22 Chalkley D, Cheung G, Walsh M, Tai N. Deaths from trauma in London – a single centre experience. Emergency medicine journal: EMJ. 2011;28:305–9.
23 David JS, Gelas-Dore B, Inaba K, Levrat A, Riou B, et al. Are patients with self-inflicted injuries more likely to die? J Trauma. 2007;62:1495–500.
24 Niemcryk SJ, Hines R, Brawley M, Yount SI. Intentional and unintentional injury in the State of Nevada: 1989–1992. Am J Prev Med. 1998;14:43–53.
25 Varley J, Pilcher D, Butt W, Cameron P. Self harm is an independent predictor of mortality in trauma and burns patients admitted to ICU. Injury. 2012;43:1562–5.
26 Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34:252–61.
27 Sampalis JS, Denis R, Lavoie A, Frechette P, Boukas S, Nikolis A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46:565–79; discussion 79–81.
28 Sampalis JS, Denis R, Frechette P, Brown R, Fleiszer D, Mulder D. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma. 1997;43:288–95; discussion 95–6.
29 Lansink KW, Gunning AC, Spijkers AT, Leenen LP. Evaluation of Trauma Care in a Mature Level I Trauma Center in The Netherlands: Outcomes in a Dutch Mature Level I Trauma Center. World journal of surgery 2013.
30 al-Ayoubi F, Eriksson H, Myrelid P, Wallon C, Andersson P. Distribution of emergency operations and trauma in a Swedish hospital: need for reorganisation of acute surgical care? Scand J Trauma Resusc Emerg Med. 2012;20:66.
31 Macken L, Manovel A. Trauma bypass in south-eastern Sydney: an 8-year review. Emergency medicine Australasia: EMA. 2005;17:137–42.
32 Hoyt DB, Kim HD, Barrios C. Acute care surgery: a new training and practice model in the United States. World J Surg. 2008;32:1630–5.
33 Kashuk JL, Klein Y, Bacchus H, Kluger YS. Acute care surgery: what’s in a name? A new specialty comes of age. The Israel Medical Association journal: IMAJ 2013;15:147–51.
34 Thorpe KE, Florence CS, Joski P. Which medical conditions account for the rise in health care spending? Health affairs 2004;Suppl Web Exclusives:W4–437–45.
35 Centers for Disease C, Prevention. Medical expenditures attributable to injuries – United States, 2000. MMWR Morbidity and mortality weekly report 2004;53:1–4.
36 Newgard CD, Staudenmayer K, Hsia RY, Mann NC, Bulger EM, Holmes JF, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health affairs. 2013;32:1591–9.
37 Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Medical care. 1997;35:1044–59.
38 Battistella FD, Torabian SZ, Siadatan KM. Hospital readmission after trauma: an analysis of outpatient complications. J Trauma. 1997;42:1012–6; discussion 6–7.
39 Dailey EA, Cizik A, Kasten J, Chapman JR, Lee MJ. Risk factors for readmission of orthopaedic surgical patients. J Bone Joint Surg Am. volume 2013;95:1012–9.
40 MacKenzie EJ, Weir S, Rivara FP, Jurkovic GJ, Nathens AB, Wang W, et al. The value of trauma center care. J Trauma 2010;69:1–10.
41 Durham R, Pracht E, Orban B, Lottenburg L, Tepas J, Flint L. Evaluation of a mature trauma system. Ann Surg. 2006;243:775–83; discussion 83–5.
42 Davenport RA, Tai N, West A, Bouamra O, Aylwin C, Woodford M, et al. A major trauma centre is a specialty hospital not a hospital of specialties. Br J Surg. 2010;97:109–17.
43 Chiara O, Cimbanassi S, Andreani S, Sammartano F, Pizzilli G, Girotti P, et al. The model of the Niguarda Hospital Trauma Team in Milan. Chirurgia italiana. 2008;60:627–40.
44 Saltzherr TP, Visser A, Ponsen KJ, Luitse JS, Goslings JC. Complications in multitrauma patients in a Dutch level 1 trauma center. J Trauma. 2010;69:1143–6.
45 Stelfox HT, Straus SE, Nathens A, Bobranska-Artiuch B. Evidence for quality indicators to evaluate adult trauma care: a systematic review. Crit Care Med. 2011;39:846–59.
46 Fung Kon Jin PH, Penning N, Joosse P, Hijdra AH, Bouma GJ, et al. The effect of the introduction of the Amsterdam Trauma Workflow Concept on mortality and functional outcome of patients with severe traumatic brain injury. J Neurotrauma. 2008;25:1003–9.
47 MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78.
48 Hulka F, Mullins RJ, Mann NC, Hedges JR, Rowland D, Worrall WH, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma. 1997;42:514–9.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.