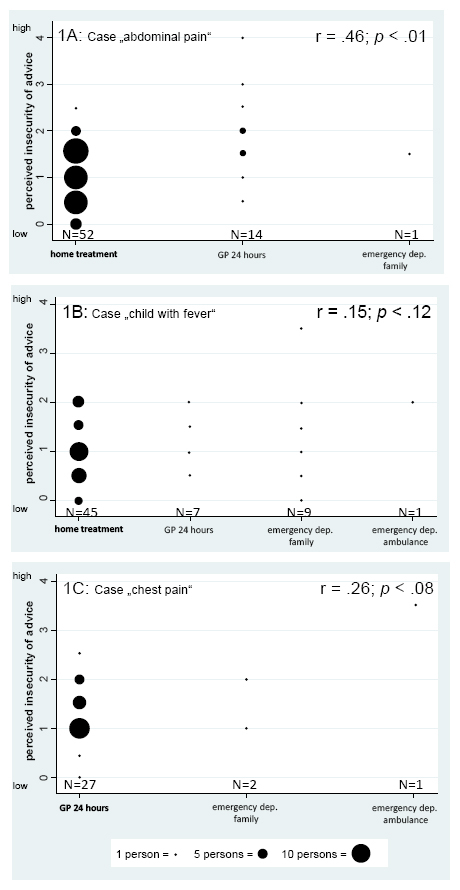
Figure 1
Association between type of recommendation and perceived insecurity (dot size represents the number of students).
Perceived insecurity graded from 0 = low insecurity to 5 = high insecurity. Bold text indicates the correct recommendation.
DOI: https://doi.org/10.4414/smw.2014.13919
Handling emergency telephone consultations (ETCs), and answering patients’ questions and providing information to them, are important everyday tasks for doctors. In the United States, about one quarter of all primary care consultations are by telephone [1]. Swiss general practitioners (GPs) handle 11% of their emergency consultations via telephone [2]. In the future, for economic and time-efficiency reasons, the importance of ETCs will increase in order to avoid unnecessary home visits and self-initiated emergency visits [3, 4].
GPs perceive ETCs as being challenging; they are obliged to make decisions based on limited information, without being able to see the patient and perform a physical examination [5]. In particular, when patients are unknown to the GPs, the number of incoming calls is high, and time pressure is high, GPs have low confidence in their handling of ETCs [6, 7]. Specific clinical situations increase insecurity about the correct management choice, such as calls from parents anxious about their ill children, patients with chronic diseases and patients with mental health problems. GPs also find it difficult when there is a discrepancy between their own views on the management needed and those of their patients [6].
Specific communication skills are required to enable clinicians to master ETCs, in addition to basic skills such as empathy, active listening and the ability to use different types of questions [5, 8]. More specific skills, such as actively advising and structuring the conversation (is there something missing here?), are fundamental in ETCs. A high quality consultation increases the likelihood of appropriate advice being given [9]. To achieve this, the patient’s history must be taken accurately and discriminating key questions, “red flags”, must be used [10]. The advice from a GP should include safety-net advice, a specific recommendation about when and how to re-consult if symptoms do not resolve in the expected time course and an explanation of specific warning signs of serious disease. Good clinical knowledge and expertise in the evaluation of patient information are required [11–13]. Ideally, an ETC consists of six phases [14, 15]: (1.) patient identification, (2.) history taking, (3.) analysis of information received, (4.) giving medical advice, (5.) checking the patient’s understanding of that advice and (6.) giving safety-net advice.
Unnecessary referrals to emergency departments should be avoided whenever possible. To be able to estimate the necessity of such referrals appropriately, the GP needs to have an accurate impression of the patient’s clinical situation.
The decision for more or less urgent advice may also be driven by the doctor’s perception of risk, feelings of insecurity, concerns about his or her own competence, and fears expressed by the patient [16, 17]. Thus, GPs with a similar performance in terms of asking relevant questions might give different treatment recommendations because of their level of insecurity [18]. Insecurity can be defined as a negative feeling about the appropriateness of a specific recommendation. One way to feel more comfortable in such a situation is to give more urgent advice in order to reduce insecurity.
Although the handling of such difficult clinical situations requires training [1, 6, 19, 20], for GPs this has been restricted to postgraduate training [5]. Even though the use of ETCs has become increasingly frequent, training in it as part of undergraduate medical education has not yet been established [13, 21]. As a result, the Institute of Family Medicine at the University of Bern provided a training programme on ETCs for fifth-year medical students, using simulated patients (SPs) [22]. The teaching aim was to prepare students for the seven-month clerkship in their final year by providing them with guidelines on handling ETCs.
The objective of this study was to identify the reasons for feeling insecure in handling ETCs. Since medical students have limited clinical knowledge and experience, we hypothesised that this would be the most frequently cited reasons for feeling insecure. In addition, we hypothesised that a higher level of insecurity would lead to more urgent medical advice than would be expected given the clinical situation, such as immediate transfer to hospital by ambulance. The link between perceived insecurity and less urgent medical advice remains unclear; the latter can be driven by emotional triggers (e.g. anticipating patients’ fear) or by a misunderstanding of the clinical case (which may be due to a lack of clinical knowledge). We therefore restricted our analysis of the association of insecurity and urgency of advice to students with adequate or more urgent advice, since a clear theoretical prediction on the association of less urgent medical advice and insecurity cannot be made.
From December 2010 to January 2011, 137 fifth-year medical students participated in the mandatory ETC training. They were given a manual with guidelines for ETCs before the training. During the training, each student performed two different ETCs with two different SPs. The allocation of cases to students was made randomly by an external administrator from the University of Bern, who was only involved in this procedure and responsible for the smooth management of the whole course.
Based on the most common reasons for ETCs [2, 23], four case studies were developed with the support of clinical experts. The ETC topics were disclosed to the students in advance, along with advice on how to prepare for the exercise.
The four cases, with the recommended management shown in brackets, were as follows:
– a call from a parent of a child with fever: a five-year-old child who had had a fever of 39 °C for two hours but no other symptoms or signs. (Appropriate advice: home treatment.)
– a patient with a headache phoning: a 25-year-old with a headache and symptoms that should suggest the possibility of a cerebral haemorrhage. (Appropriate advice: immediate transport to an emergency department by ambulance.)
– a call from a woman whose husband has chest pain: a 45-year-old man with chest pain described as “stinging”, occurring only with certain movements and located at the right lateral lower chest. (Appropriate advice: consultation with a general practitioner within 24 hours.)
– a patient with abdominal pain phoning: a 24-year-old with abdominal pain, on a background of chronic constipation, which has worsened owing to taking an iron medication. (Appropriate advice: home treatment.)
SPs were hidden behind a screen and presented their cases verbally. Students were not able to see the SPs or perform a physical examination.
The students were asked whether they had felt any insecurity. If they answered “yes”, they were asked to write down the reasons for their insecurity during five specific phases of the ETC: history taking, analysis of information, giving medical advice, checking the patient's understanding and giving safety net advice.
The level of perceived insecurity was measured by two items indicating how insecure they felt about (1.) the appropriateness of their clinical decision based on their assessment of the case’s urgency and (2.) the appropriateness of their advice (6–point Likert scale: 0 = no insecurity, 5 = high insecurity). A mean value for both items was used in the analysis.
The urgency of their advice was documented by the SPs, with four options: (1.) home treatment, (2.) consultation with a general practitioner within 24 hours, (3.) transport to an emergency department by a family member within a short period of time, (4.) immediate transport to an emergency department by ambulance. If no advice on this was given, this was coded as zero. A score from 0 to 4 (from no advice to transport to the emergency department by ambulance) reflects the urgency of the advice.
The standardised forms were scanned and transferred to a data file. The free-text answers were coded by two authors in duplicate (MS, RA). First, each coded the reasons for insecurity separately in 20 of the questionnaires. Differences in coding were resolved by discussion and the coding system was adapted (table 1). Then, all 274 questionnaires were coded by both authors separately, using the revised coding system. The two raters agreed in over 95% of their codings; kappa values for the five reasons for insecurity ranged from 0.66 to 0.96, suggesting good to excellent inter-rater reliability (see table 1). Finally, any differences in coding were resolved by discussion. Only codes which were present in more than 5% of the questionnaires were analysed.
For the descriptive analysis of the reasons for insecurity for all cases and across the cases, we calculated percentages of the respective reasons with their 95% confidence intervals (CIs). The comparison of the mean values of the level of insecurity between cases was made using the t-test for independent samples.
The association between the level of insecurity about the appropriateness of the advice and the urgency of the advice given was calculated with the Spearman rank correlation test, with a one-tailed test of statistical significance, for three cases. A positive coefficient reflects an association of higher insecurity with more urgent advice. As stated above, no clear theoretical assumption about the association of perceived insecurity and less urgent advice was possible. We therefore excluded the headache case from this part of the analysis, since the correct option was the most intense advice. In addition, we excluded answers recommending less urgent action (i.e. home treatment) in one case (chest pain) (n = 1) so that we could make valid conclusions on the association of more urgent advice with perceived insecurity. All analyses were performed with STATA release 12.
| Table 1:Reasons given for insecurity (definitions and kappa values). | |
| Categories | Definition |
| Lack of clinical knowledge and experience kappa = 0.86 | The student did not know all the symptoms or complications of a certain disease or was not familiar with the therapy. The student lacked a clinical routine to handle the problem. |
| Low quality/quantity of questions asked kappa = 0.90 | The student forgot to ask one or several questions relevant to the history, such as “red flag” questions or questions about the patient’s current medication. |
| Doubts about reliability of information kappa = 0.66 | The student had the impression that the information given by the caller could not be trusted. |
| History taken from a third party kappa = 0.96 | The student felt insecure because he/she could not talk to the patient him- or her-self. |
| Lack of visual impression and physical examination kappa = 0.88 | The student felt insecure because he/she could not get a visual impression of the patient’s condition and/or because he/she could not do a physical examination. |
The questionnaire response rate was 100%, corresponding to 274 questionnaires (68 or 69 questionnaires per case). Table 2 shows the number and percentages of students who reported insecurity in their free text answers. Their responses were allocated to the five phases of an ETC. History taking was the ETC phase in which the most students had some insecurity (63.1%), ranging from 54.4% (headache) to 81.2% (child with fever), while 44.9% experienced insecurity during the analysis of the information given (ranging from 33.8% for the patient with abdominal pain to 68.1% for the child with fever). More than half of the students felt insecure when giving their advice (53.6% overall), ranging from 42.6% (abdominal pain) to 69.1% (headache).
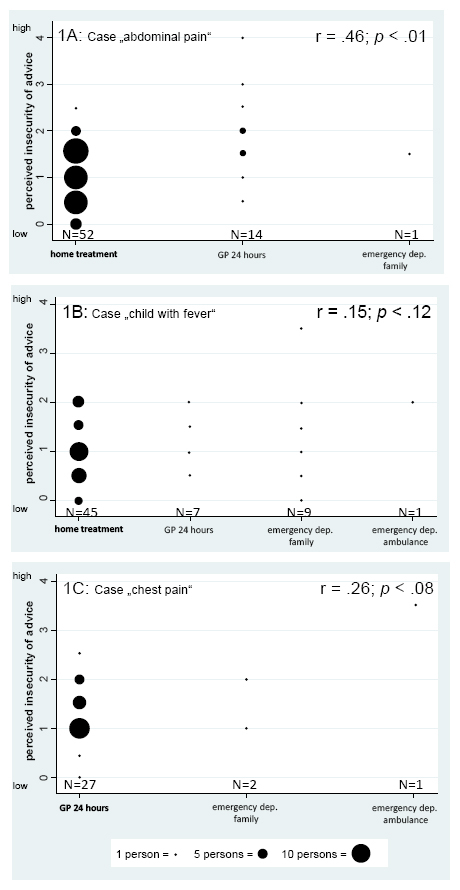
Figure 1
Association between type of recommendation and perceived insecurity (dot size represents the number of students).
Perceived insecurity graded from 0 = low insecurity to 5 = high insecurity. Bold text indicates the correct recommendation.
Students were advised to check patients’ understanding of the advice given. Almost a quarter (23.4%) felt insecure during this phase. Students who had to respond to the patient with a headache showed the least insecurity about checking patients’ understanding of the advice given (14.7%). With regards to giving safety-net advice, 20.1% felt insecure about the task, ranging from 13.2% (abdominal pain) to 29.0% (husband with chest pain).
In all cases except the one with the headache patient, insecurity was most prevalent during history taking. Those answering the call of the headache patient, were more often insecure about their provision of medical advice. Of 274 ETCs, there were only 13 ETCs (4.7%) in which the students felt no insecurity at any stage.
The reason for students' insecurity (table 3) was most frequently cited as being their lack of clinical knowledge and experience (47% overall), ranging from 34.8% (husband with chest pain) to 69.1% (abdominal pain). Approximately the same percentage of students (46.7% overall) felt insecure about whether they had asked all the necessary questions, ranging from 31.9% (husband with chest pain) to 59.4% (headache). In addition, 23.0% of the students had doubts about the reliability of the information that they had been given by the SP: in particular, students doubted the quality of the information in the cases of the child with fever and the husband with chest pain (27.9% and 40.6%, respectively). In the cases of abdominal pain and headache, there was more confidence in the presented information, with doubt in only 8.8% and 14.5% consultations respectively. In total, 75.4% of all students experienced insecurity in their history taking from the spouse (husband with chest pain), but only 2.9% felt such insecurity when the history was taken from the parent of the child with fever.
Lack of visual information contributed to insecurity in only 10.6% of the students overall, ranging from 5.8% (husband with chest pain) to 16.2% (child with fever). Further reasons for insecurity described by the students were fear of misunderstandings (5.8% overall), avoidance of particular questions because they were concerned about offending the caller (4.0% overall) and the fact that the patient was unknown to them (1.1% overall).
The students felt most insecure in their advice after the ETC on abdominal pain (mean = 1.54, standard deviation [SD] = 0.92) and the ETC on chest pain (mean = 1.35, SD = 0.82). Students felt less insecure in their advice for the child with fever (mean = 1.13, SD = 0.62) and the patient with a headache (mean = 1.09, SD = 0.93). The mean perceived insecurity of students differed significantly between the abdominal pain case and the headache case (p < .02) and between the abdominal pain case and the child with fever case (p <0.04).
The percentage of students giving correct advice differed between the four cases. For the headache case, 88% of the students gave the correct advice. The case involving the patient with abdominal pain received the correct advice from 76% of the students, and the advice for the case of a child with fever was correct in 66% of consultations. The case of the patient with chest pain was most difficult, with only 39% of students giving the correct advice. About 50% of the students incorrectly advised home treatment or gave no advice at all.
As hypothesised, perceived insecurity was correlated with more urgent advice given for the case with abdominal pain (r = 0.46, p <0.01; fig. 1A). In the case of the child with fever (r = 0.15, p <0.12; fig. 1B) and in the case of the husband with chest pain (r = 0.26, p <0.08), there was a trend to more urgent advice being associated with a higher level of insecurity (fig. 1C).
| Table 2:Presence of insecurity noted by the students during the five phases of the emergency telephone consultation (number, percentage and 95% confidence interval). | ||||||||||
| Husband with chest pain (n = 69) | Child with fever (n = 69) | Abdominal pain (n = 68) | Headache (n = 68) | Total (n = 274) | ||||||
| Phase of ETC | n | % (CI) | n | % (CI) | n | % (CI) | n | % (CI) | n | % (CI) |
| History taking | 38 | 55.1 (43.38–64.55) | 56 | 81.2 (70.25–88.78) | 42 | 61.8 (49.86–72.41) | 37 | 54.4 (42.65–65.70) | 173 | 63.1 (57.28–68.64) |
| Analysis of information | 24 | 34.8 (24.59–46.58) | 47 | 68.1 (56.38–77.95) | 23 | 33.8 (23.68–45.69) | 29 | 42.6 (31.59–54.49) | 123 | 44.9 (39.11–50.81) |
| Giving medical advice | 31 | 44.9 (33.77–56.62) | 40 | 58.0 (46.20–68.90) | 29 | 42.6 (31.59–54.49) | 47 | 69.1 (57.32–78.87) | 147 | 53.6 (47.74–59.46) |
| Checking the understanding | 19 | 27.5 (18.33–39.11) | 18 | 26.1 (17.11–37.58) | 17 | 25.0 (16.15–36.52) | 10 | 14.7 (7.99–25.20) | 64 | 23.4 (18.72–28.73) |
| Giving safety-net advice | 20 | 29.0 (19.56–40.63) | 11 | 15.9 (8.97–26.51) | 9 | 13.2 (6.90–23.50) | 15 | 22.1 (13.74–33.36) | 55 | 20.1 (15.74–25.23) |
| CI = confidence interval; ETC = emergency telephone consultation | ||||||||||
| Table 3:Reasons for insecurity obtained from free text answers (number, percentage and 95% confidence interval). | ||||||||||
| Husband with chest pain (n = 69) | Child with fever (n = 68) | Abdominal pain (n = 68) | Headache (n = 69) | Total (n = 274) | ||||||
| n | % (CI) | n | % (CI) | n | % (CI) | n | % (CI) | n | % (CI) | |
| Lack of clinical knowledge and experience | 24 | 34.8 (24.59–46.58) | 31 | 45.6 (34.30–57.35) | 47 | 69.1 (57.32–78.87) | 28 | 40.6 (29.78–52.37) | 130 | 47.4 (41.61–53.35) |
| Low quality/quantity of questions | 22 | 31.9 (22.05–43.62) | 35 | 51.5 (39.83–62.95) | 30 | 44.1 (32.94–55.92) | 41 | 59.4 (47.63–70.22) | 128 | 46.7 (40.89–52.63) |
| Doubts about reliability of information | 28 | 40.6 (29.78–52.37) | 19 | 27.9 (18.62–39.63) | 6 | 8.8 (3.78–18.27) | 10 | 14.5 (7.87–24.86) | 63 | 23.0 (18.39–28.34) |
| History taken from a third party | 52 | 75.4 (63.95–84.09) | 2 | 2.9 (0.20–10.71) | 54 | 19.7 (15.41–24.84) | ||||
| Lack of visual impression and physical examination | 4 | 5.8 (1.85–14.40) | 11 | 16.2 (9.1–26.87) | 9 | 13.2 (6.9–23.5) | 5 | 7.2 (2.77–16.23) | 29 | 10.6 (7.43–14.83) |
This study reveals that specific parts of ETCs are challenging for medical students, despite prior provision of guidelines and safety-net advice. Overall, 95% of the students felt insecure in at least one of the five phases of their ETC with a simulated patient, which confirms studies in qualified doctors [5, 6].
Calls from a third person are frequent, occurring in 30% to 57% of ETCs [23, 24], and these may cause considerable insecurity for both health professionals and medical students [25]. Surprisingly, our results suggest that taking a history from a spouse was much more challenging than taking a history from a parent. This finding may be explained by health professionals’ belief that parents give more reliable information than other parties.
Surprisingly, our results did not show that either lack of a visual impression or lack of a physical examination were important reasons for insecurity. This is in contrast to findings from studies with GPs and triage nurses [6, 25]. Our finding might be explained by the fact that in our study setting a visual exploration was impossible, so students did not expect to get a visual impression of the patient. Another possibility is that today’s students might assign less importance to physical examination than they do to laboratory or radiological diagnostic procedures [26–28]. If this is indeed the case, then the teaching of physical examination skills should be emphasised during medical education.
Our study showed that perceived insecurity was associated with a greater urgency of advice in ETCs. However, unnecessary hospital referral is costly. As the quality of an ETC is positively associated with the appropriateness of the advice [9], specific training in systematic history taking and asking discriminating questions might reduce insecurity and, as a consequence, reduce unnecessary hospital referrals. More research on ETC training within the healthcare system and on the training of students is needed to acquire information on the long-term effects of such a new curriculum [29].
History taking was the phase of ETCs during which most students felt insecure. This finding is related to their second most common concern, which was whether or not they had asked all the necessary questions. This result was somewhat unexpected as students had been trained in history taking from the beginning of their studies and had the opportunity to prepare discriminatory questions for these particular cases. The current training in history taking seems to be insufficient for ETCs and standardised teaching on choosing discriminatory questions has so far not been implemented.
The strengths of this study were its variety of clinical cases and the moderately large sample. However, some weaknesses might limit the interpretation of our findings. First, the presentation of cases may have been influenced by the individuals who simulated the patients. The perceived challenge of a case might have reflected the way the SP presented the case (e.g. the clarity of their language) as well as the difficulty of the case itself. A second limitation is that only four cases were presented, limiting the generalisability of the findings to other clinical conditions and to other countries with different systems of healthcare and medical education. A third limitation is the rather low level of clinical knowledge of the study participants. Studies to replicate this work with experienced clinicians are needed; these would also give an insight into their strategies for dealing with insecurity in ETCs.
Poor history taking, a low number of discriminating questions, and the lack of clinical knowledge and experience are the main problems for fifth-year medical students in ETCs. As a consequence, medical schools should stress the importance of history taking and clinical examination in medical education. Training of medical students in ETCs in Swiss medical schools should help prepare the next generation of doctors for the adequate management of this important day-to-day task.
In accordance with other studies, the insecurity that students report affects the quality of the advice that they give. Our results have two implications. Firstly, insecurity and ambiguity were present in these consultations, but the self-concept of doctors is founded in rationality and evidence. Some clinical situations induce insecurity and dealing with this should be part of the curriculum. Secondly, interventions to reduce insecurity within clinical scenarios might help clinicians to handle them. Such interventions might include new electronic tools (e.g. risk score calculator apps) or come within undergrauduate and postgraduate training.
1 Car J, Freeman GK, Partridge MR, Sheikh A. Improving quality and safety of telephone based delivery of care: teaching telephone consultation skills. Qual Saf Health Care. 2004;13:2–3.
2 Marty F, Meyer R, Lüscher S, Gnädinger M, Kissling B. Urgent consultations/emergencies to a general practitioner – a pilot study. Prim Care. 2006;6:345–7.
3 Christensen MB, Olesen F. Out of hours service in Denmark: evaluation five years after reform. BMJ. 1998;316:1502–6.
4 Leibowitz R, Day S, Dunt D. A systematic review of the effect of different models of after-hours primary medical care services on clinical outcome, medical workload, and patient and GP satisfaction. Fam Pract. 2003;20:311–7.
5 Larsen J-H, Risor O. Telephone consultations at the emergency service, Copenhagen County: analysis of doctor-patient communication patterns. Fam Pract. 1997;14:387–97.
6 Foster J, Jessopp L, Dale J. Concerns and confidence of general practitioners in providing telephone consultations. Br J Gen Pract. 1999;49:111–3.
7 O’Donnell CA. Variation in GP referral rates: what can we learn from the literature? Fam Pract. 2000;17:462–71.
8 Innes M, Skelton J, Greenfield S. A profile of communication in primary care physician telephone consultations: application of the Roter Interaction Analysis System. Br J Gen Pract. 2006;56:363–8.
9 Huibers L, Keizer E, Giesen P, Grol R, Wensing M. Nurse telephone triage: good quality associated with appropriate decisions. Fam Pract. 2012;29:547–52.
10 Derkx HP, Rethans J-JE, Maiburg BH, Winkens RA, Muijtjens AM, van Rooij HG, et al. Quality of communication during telephone triage at Dutch out-of-hours centres. Patient Educ Couns. 2008;74:174–8.
11 Huibers L, Giesena P, Smitsa M, Mokkinkb H, Grola R, Wensinga M. Nurse telephone triage in Dutch out-of-hours primary care: the relation between history taking and urgency estimation. Eur J Emerg Med. 2011;19:309–15.
12 Rutenberg CD. Telephone Triage. Am J Nurs. 2000;100:77–81.
13 Patel A, Dale J, Crouch R. Satisfaction with telephone advice from an accident and emergency department: identifying areas for service improvement. Qual Health Care. 1997;6:140–5.
14 Derkx HP, Rethans J-JE, Knottnerus JA, Ram PM. Assessing communication skills of clinical call handlers working at an out-of-hours centre: development of the RICE rating scale. Br J Gen Pract. 2007;57:383–7.
15 McKinstry B, Watson P, Pinnock H, Heaney D, Sheikh A. Confidentiality and the telephone in family practice: a qualitative study of the views of patients, clinicians and administrative staff. Fam Pract. 2009;26:344–50.
16 Donner-Banzhoff N. Umgang mit Unsicherheit in der Allgemeinmedizin. Z Evid Fortbild Qual Gesundhwes (ZEFQ). 2008;102:13–8.
17 Morgan M, Jenkis L, Ridsdale L. Patient pressure for referral for headache: a qualitive study of GP’s referral behaviour. Br J Gen Pract. 2007;57:29–35.
18 Wayne S, Dellmore D, Serna L, Jerabek R, Timm C, Kalishman S. The association between intolerance of ambiguity and decline in medical students’ attitudes toward the underserved. Acad Med. 2011;86:877–82.
19 Car J, Sheikh A. Telephone consultations. BMJ. 2003;326:966–9.
20 Giesen P, Ferwerda R, Tijssen R, Mokkink H, Drijver R, van den Bosch W, et al. Safety of telephone triage in general practitioner cooperatives: do triage nurses correctly estimate urgency? Qual Saf Health Care. 2007;16:181–4.
21 Cykert S, Flannery MT, Huber EC, Keyserling T, Moses GA, Elnicki MD, et al. Telephone medical care administered by internal medicine residents: concerns of program directors and implications for residency training. Am J Med Sci. 1997;314:198–202.
22 Schaufelberger M, Harris M, Frey P. Emergency telephone consultations: a new course for medical students. Clin Teach. 2012;9:373–5.
23 Crouch R, Patel A, Williams S, Dale J. An analysis of telephone calls to an inner-city accident an emergency departement. J R Soc Med. 1996;89:324–8.
24 Marklund B, Bengtsson C. Medical advice by telephone at Swedish Health Centres: who calls and what are the problems? Fam Pract. 1989;6:42–6.
25 Wahlberg AC, Cedersund E, Wredling R. Telephone nurses’ experience of problems with telephone advice in Sweden. J Clin Nurs. 2003;12:37–45.
26 Young MJ, Poses RM. Medical student perceptions of the value of the history and physical examination. J Med Educ. 1983;58:738–9.
27 Holmboe ES. Faculty and the observation of trainees’ clinical skills: problems and opportunities. Acad Med. 2004;79:16–22.
28 Goodwin J. The importance of clinical skills. BMJ. 1995;310:1281–2.
29 Adler RH, Minder CE. Clinical competence of biopsychosocially trained physicians and controls. SMW. 2012;142:w13649.
Acknowledgement: We thank all participants in this study for completing the comprehensive set of questionnaires. The support of Petra Büchler and Anna Hirsbrunner in preparing this manuscript is very much appreciated.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.