
Figure 1
Flow-chart of the students participating in the survey.
*Exact number of participating students (i.e., denominator) in lectures unknown
DOI: https://doi.org/10.4414/smw.2014.13932
Surgery will be confronted with a serious workforce shortage in the future [1]. In Switzerland, between 13% and 25% additional healthcare professionals will be needed by the year of 2020 [2], reflecting recent trends toward imminent physician and surgeon shortages in the United States [1, 3] and in the United Kingdom [4].

Figure 1
Flow-chart of the students participating in the survey.
*Exact number of participating students (i.e., denominator) in lectures unknown
Surgery, with its high social prestige and unique combination of intellectual and technical challenges, made generations of surgeons dedicate their lives to surgery. This power of attraction was lost in the recent decade. Surgery already has an image problem among potential candidates. Since the 1980s, the United States healthcare institutions and hospitals have been faced with a trend towards a declining interest in surgery, currently leaving almost 25% of positions in general surgery vacant [5]. Recent studies from Germany and Ireland indicate that only 5%‒18% of students decide on surgery as a career [6–8]. Career decision criteria are increasingly dominated by work-life balance aspects and not purely by personal interest [9, 10]. Concerns regarding antisocial working hours, unreliable career planning and inadequate remuneration are deterrents to surgery as a career option [11, 12]. Family issues and childbearing concerns are taken seriously by all residents [13]. Whilst currently about 50% of practicing doctors in Germany are woman [14], 70% of medical students are women, potentially leading to the rejection of a surgical career [12], enhancing the workforce shortage in surgery [15]. In Germany, only 5.6% of female students and 15.2% of male students started a surgical career, as suggested in a recent survey [14].
The number of practicing surgeons depends also on the number of surgeons who undergo career changes (attrition) over time, as well as retirement rates. By the year 2020, in Germany one third of current surgeons will be retired, creating a need for at least 20% of medical students opting for surgery as a career [7]. Reasons for attrition and career changes may be similar to the reasons for not starting a surgical career in the first place, namely the challenge to integrate professional and private lives [16, 17]. A recent survey of 549 trauma surgeons in Germany showed that most surgeons work significantly more than foreseen, leading to impaired life quality and dissatisfaction [18]. Twenty-two percent of surgeons would not select a medical profession again, and 15% would rather select another speciality. A recent evaluation of 215 American surgical education programmes showed attrition to be caused mostly by work-life balance issues and family concerns [19]. An increasing number of surgeons discontinue clinical work in favour of an industry career. An evaluation of 4,619 dropout-doctors in Germany [20] revealed inappropriate remuneration, incompatibility of family and job, and increasing administrative workload as main reasons to leave medicine.
Accentuated, but sustainable, motivation of students may be a key step to resolve the imminent shortage of surgeons. Medical school can be understood as a vulnerable phase, where early exposure to practical surgical procedures increases interest in surgery [21] and can help to overcome students’ negative perceptions [22]. The established role of virtual reality (VR) in surgical training [23–26] may be a useful tool in this setting. VR is safe, harmless, can be performed by students with minimal skills and anatomy expertise, and may be repeated at discretion.
To the best of our knowledge, a VR intervention has not yet been evaluated as a tool to increase student interest in surgery. Therefore, the aim of this study was (i.) to evaluate the current career expectations of Swiss medical students and their appraisal of surgery as a career choice and (ii.) to investigate the effect of a VR intervention on medical students’ ranking of future work environments.
This survey was conducted among medical students in study years Bachelor year 1, Master year 1 and Master year 2, referring to the European Bologna reform [27, 28], at three lectures in October and November 2012 at the Medical Faculty at the University Hospital Basel, Switzerland. The Bologna reform harmonised study curricula across Europe and divided medical training into a Bachelor and Master period [27]. Lectures were eligible for inclusion based on the following requirements. Firstly, in order to provide adequate time-slots for hands-on exercise, lectures had to be followed by a subsequent longer lunch break. Secondly, lecture rooms had to have overhead beamers, enough space and adequate IT equipment to demonstrate and use the VR simulator. Out of the few eligible lectures in the given time period, the respective academic professors holding the lecture were contacted at random to check their willingness to participate, until three lectures could be identified.
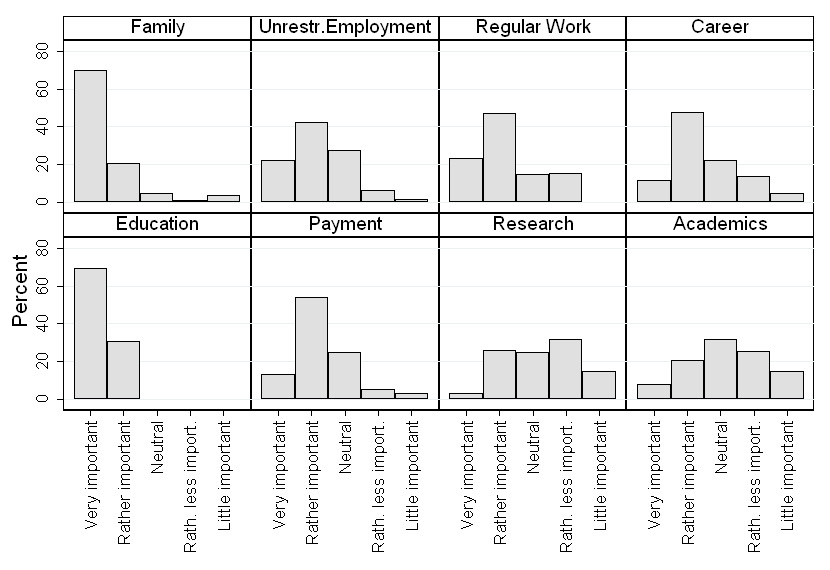
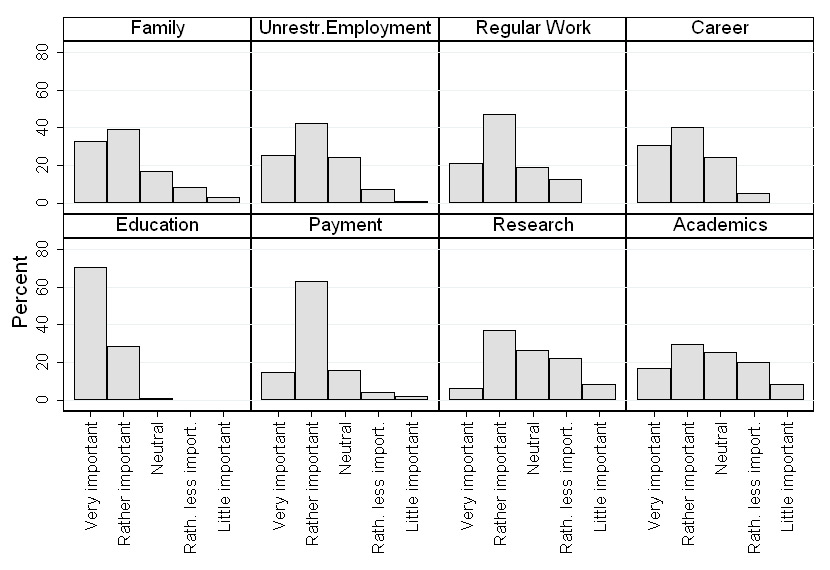
Figure 2
As a doctor, how important are the following aspects regarding future work environments to you: good work-life balance (family), unrestricted employment (unrest. employment), regular work, good career chances (career), optimal education (education), adequate payment (payment), possibility for research (research) and option for pursuing an academic career (academics)?
Please assign a value to each option. (Answering options with five descriptors: very important – rather important – neutral – rather less important- little important)
2a: Answers of female students
2b: Answers of male students
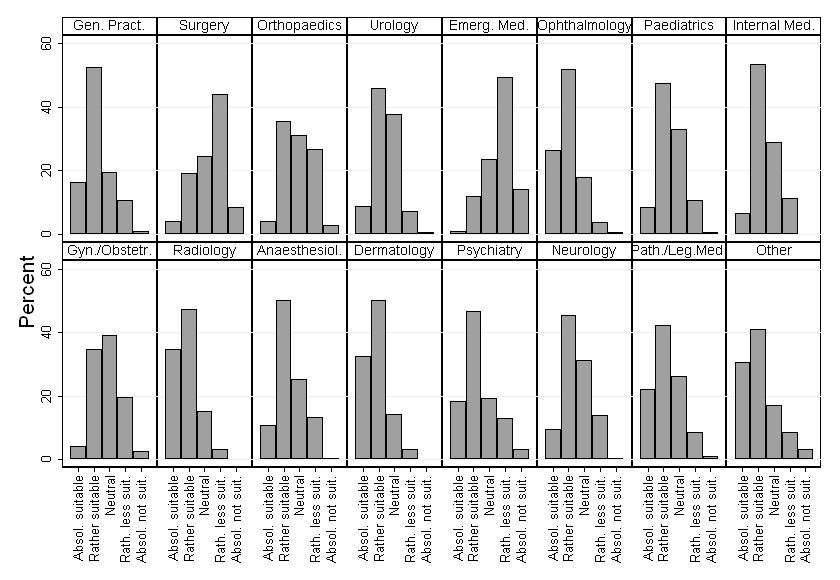
Figure 3
To what extent are different medical specialities suitable to satisfy your work environment expectations? Please assign a value to each option. (Answering options with five descriptors: absolutely suitable – rather suitable – neutral – rather less suitable – absolutely not suitable).
Anaesthesiol. = anaesthesiology; Emerg. Med. = emergency medicine; Gen. Pract = general practitioner; Gyn./Obstetr. = gynaecology/obstetrics; Internal Med. = internal medicine; Path./Leg.Med. = pathology/legal medicine
All students studying in these three academic years were eligible for this study. Every student could only take part once in the VR intervention. The total number of students subscribed to the lectures was obtained from the medical faculty secretary. The number of actually participating students per lecture could not be determined due to students being late or leaving lectures earlier hampering simple counting the participating students. All included students voluntarily participated in this study.
Ethical approval was not requested for this study. Our study was designed as a voluntary questionnaire based survey with a VR intervention integrated in the medical lectures with no violation of ethical standards.
The students received a short baseline questionnaire before the lecture. They were asked to rank five different future postgraduate working environments according to their preference: surgical sector, referring not only to surgery in the literal sense, but to all specialties with surgical interventions (e.g., general surgery, traumatology, orthopaedics, paediatric surgery, gynaecology, otorhinolaryngology, surgical ophthalmology), nonsurgical sector (e.g., internal medicine, general practitioner, paediatrics, neurology, psychiatry, dermatology, emergency medicine, nonoperative ophthalmology), cross-disciplinary specialties (e.g., anaesthesiology, radiology, pathology, legal medicine and laboratory medicine), nonclinical sector (e.g., controlling, medical coding, pharmaceutical industry, media), and research sector (e.g., basic research in a laboratory). The ranking for each of these sectors ranged from 1 (my first choice) to 5 (my last choice). Furthermore, e-mail addresses for the subsequent online survey were recorded with this questionnaire. All distributed questionnaires were collected at the end of the lecture before starting the VR intervention.
After the lecture, the laparoscopic virtual reality simulator (Simbionix, LAP MentorTM) was presented to the students, visualised on an overhead screen with a beamer. Steps of a laparoscopic cholecystectomy were presented to the students to provide brief impressions of this surgical intervention. During the presentation, students were briefed for indications for this operations and typical clinical patterns of gall bladder disease. Then, all participating students were invited to perform steps of this simulated operation on their own. For time reasons, participants worked in teams consisting of two students assisting each other. One student performed the dissection of the cystohepatic (Calot’s) triangle and the other student clipped the cystic duct and artery, followed by transection with scissors. On average every student spent 5 minutes on the simulator, but followed the clinical background information (whilst other students tested the simulator) through the overhead screen for up to 10 minutes.
Following the VR intervention, an online questionnaire was sent out (www.surveymonkey.com) on the same day to all students; this included 19 questions regarding baseline characteristics, their expectations concerning future working environments, surgical career aspects, and their feedback on the VR intervention. The students were asked to rank again the five working environments (final ranking). Most items in the online questionnaire were not evaluated in the baseline questionnaire, because their importance was thought not to be related to the VR intervention. To reduce bias, the order of the answering options was randomly generated for each student. In the case of rating scale questions, answering options were labelled with 5 descriptors (e.g., 1 = very important, 2 = rather important, 3 = neutral, 4 = rather less important, and 5 = little important). There was no “not applicable” answering option, in order to force students to provide an answer. It was mandatory to answer all questions in order to be able to send back the questionnaire. If the questionnaire was not answered within a week, a reminder was sent out by e-mail every 7 days, until the study was closed in November 2012. Response to the online questionnaire was kept anonymous in order to increase the response rate. Linking individuals to the preceding short baseline questionnaire was, therefore, not possible.
The results were downloaded from the online-survey tool as an Excel spreadsheet (Microsoft Excel 2010TM) and the answers of the initial ranking during the lecture were manually added into an Excel spread sheet. All data were handled anonymously. Therefore, the initial ranking during the lecture could not be assigned on an individual basis to the ranking in the online questionnaire. As a consequence, no hypothesis test could be carried out for this comparison, since any statistical test accounting for this paired design by definition requires the above-mentioned assignment. The answers to the question regarding expectations of future workplaces in terms of combining job and family were compared between male and female students. For this purpose, an overall Fisher’s exact test to investigate the association between gender and the five different categorical answer options was conducted. Additionally, we considered the answering options as equally spaced ranks with a Wilcoxon’s rank-sum test and calculated a generalised Hodges-Lehmann median difference with 95% confidence interval (CI) [29]. Since the focus of this research is not on comparing answers between different subgroups of students and we additionally did not want to carry out multiple hypothesis tests with the risk of committing a type I error, we refrained from other statistical analyses.
Descriptive analyses were conducted using Windows Excel (Microsoft Excel 2010TM). Statistical tests and graphs were performed using Intercooled Stata Version 12.1 (Stata Corp, college Station, TX, USA). Results are presented in numbers and percentages. A p-value below 0.05 was considered as statistically significant.
A total of 485 students were matriculated in the academic Bachelor year 1 (n = 138), Master year 1 (n = 174) and Master year 2 (n = 173) at the Medical Faculty of the University Basel between 1 October 2012 and 30 November 2012 (fig. 1). Out of these, 276 students participated in the lectures and returned the short questionnaire distributed beforehand. Out of the 485 students, 209 were missing because they did not participate in the lectures, left the auditorium early, or failed to return the short baseline questionnaire they received. The proportion of participants filling in the baseline questionnaire may thus not be calculated, given the unknown denominator. Had all 485 students participated in the three lectures from the beginning to the end, the response rate would have been 57% (276/485).

Figure 4
How compatible is surgery with the following aspects of the work environment: good work-life balance (family), unrestricted employment (unrest. employment), regular work, good career chances (career), optimal education (education), adequate payment (payment), possibility for research (research) and option for pursuing an academic career (academics)? Please assign a value to each option. (Answering options with five descriptors: well compatible – rather compatible – compatible – rather less compatible – poorly compatible.)
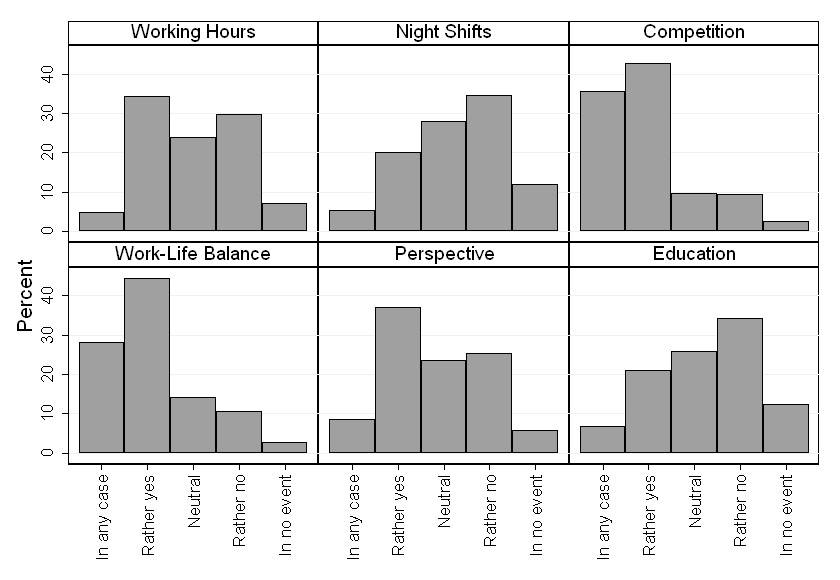
Figure 5
Which aspects of the work environment present a drawback to starting a surgical career: overtime hours (working hours), night shifts, strong competitive mentality inside the team (competition), apprehension of a bad work-life balance (work-life balance), unclear future perspectives (perspective), and lengthy and intensive education curriculum (education)? Please assign a value to each option. (Answering options with five descriptors: in any case – rather yes – neutral – rather no – in no event.)
Out of 276 questionnaires collected, 18 were incomplete, missing the e-mail addresses; therefore, the online follow-up questionnaire could not be sent out to these participants. Nevertheless, baseline-ranking data were available from the 18 incomplete questionnaires. Thereafter, the online questionnaire was sent to 258 students of whom 225 responded. Consequently, with the exception of the initial ranking of the postgraduate working environments (n = 276), the answers refer to a total of 225 out of 258 students, corresponding to an online-questionnaire response rate of 87%. Considering all matriculated students in the three academic years evaluated (n = 485), the returned questionnaires would represent 46% (225/485) of all students. Baseline characteristics are presented in table 1.
Most students (188/225, 84%) could imagine working both in medical and in nonmedical sectors. With regards to expectations of future workplaces, good education (n = 157, 70%) and combining job and family (n = 122, 54%) were considered to be very important by all students. Most items were similarly rated by female and male students, with the exception of combining job and family. This item was rated as very important in 70% (n = 91) and rather important in 21% (n = 27) of female students (fig. 2a) as compared to male students (fig. 2b), of whom 33% (n = 35) thought family to be very important and 39% (n = 41) rather important. The difference was statistically significant (Fisher’s exact test and Wilcoxon’s rank sum test: p <0.001, median difference and 95% CI –1 (–1, 0). Opportunities for an academic career and research were estimated to be slightly more important by male students (fig. 2b).
As shown in (fig. 3), different medical specialities seem to satisfy students’ expectations for optimal working environments to a different extent. The majority of students rated surgery (n = 99, 44%) and emergency medicine (n = 111, 49%) as a suboptimal working environment. Although radiology, dermatology and ophthalmology received the best overall rating, the remaining other specialties were rated ambiguously regarding their potential to satisfy working environment expectations.
The majority of students found that the work-life balance (n = 124, 55%) as well as the irregular working hours (n = 107, 48%) were low for surgery (fig. 4). Good career opportunities, education and remuneration were positive criteria that were assigned to surgery. As shown in figure 5, the main drawbacks to starting a surgical career were the apprehension of an impaired work-life balance, competitive mentality, unclear career perspectives, and longer working hours. Nightshifts and the long training, on the other hand, did not dissuade the majority of students from starting a surgical career.
The majority of all students (n = 143, 64%) agreed that surgery should be introduced in the first 3 years at medical school, as is the current practice. In contrast, 36% (n = 82) of all students think that surgery should be introduced later in the Master years. Among Bachelor students only, 83% (n = 85) would like surgery to be introduced sin the first 3 years, whereas 17% (n = 18) preferred introduction in the last 3 years. Among Master students only, 48% (n = 58) preferred introduction during the first 3 years, whereas 48% (n = 58) favoured introduction in the fourth year, 5% (n = 6) in the fifth year, and none in the last year.
Forty-seven percent (n = 105) of students had never heard about VR simulation in surgery prior to the current study (table 1). The majority of students (n = 132, 59%) chose the option “absolutely or rather correct” concerning whether the VR intervention had increased their interest in surgery, and these two options were chosen in 98% (n = 212) concerning whether the VR demonstration was helpful in providing more insight into surgery (fig. 6). A total of 75% (n = 170) answered the question whether VR sessions should be integrated into the university curriculum at medical school as absolutely or rather correct and 94% (n = 213) that these sessions should be integrated into the practical year (practical year of stages at different specialties during medical school, (fig. 6). Most students (n = 191, 85%) expressed a wish to participate in further, intensive VR practice sessions. In answer to the direct question as to whether the VR intervention had an impact on their decision-making in their aspired medical speciality, 70% (n = 158) denied and 4% (n = 10) confirmed a positive influence.
The ranking of postgraduate working environments (n = 276) retrieved from the initial short questionnaire, from 1 (highest rank) to 5 (lowest rank), showed the nonsurgical sector to be the most attractive area with a median ranking of 1 (Interquartile range [IQR] 1–2), followed by the surgical sector (median 2, IQR 1–3), cross-disciplinary specialties (median 3, IQR 2-3), the research sector (median 4, IQR 4–5) and finally the nonclinical sector (median 5, IQR 4–5) (fig. 7, upper row). The impact of the VR intervention on re-evaluation of the ranking of the five sectors with the online follow-up questionnaire was limited (fig. 7). Rank 1 was given by 33% of students for surgical disciplines in the baseline evaluation, rank 1 for surgical disciplines increased after VR intervention to 35%. However, the majority of the students still preferred the nonsurgical sector, 60% (n = 166/276) rated the nonsurgical sector before VR intervention rank 1, although this percentage decreased to 55% (n = 123/225) after VR intervention.
| Table 1: Baseline characteristics of participants. Baseline characteristics of participants who responded to the online-questionnaire (n = 225, 87%) *One student from Bachelor 2 and one from Bachelor 3 participated in the Bachelor 1 lecture and were allocated to the Bachelor 1 year in this study. | ||
| Total, n (%) | 225 (100) | |
| Female, n (%) | 130 (58) | |
| Age, median (IQR) | 23 (20‒24) | |
| Medical school, n (%)* | Bachelor 1 | 103 (46) |
| Master 1 | 60 (27) | |
| Master 2 | 62 (28) | |
| Civil status, n (%) | Unmarried | 223 (99) |
| Married | 1 (<1) | |
| Divorced | ||
| Widowed | 1 (<1) | |
| Living situation, n (%) | Living alone | 43 (19) |
| Shared house | 132 (59) | |
| Close-partnered | 50 (22) | |
| Children, n (%) | None | 225 (100) |
| Participation in operations, n (%) | No | 56 (25) |
| Watching | 120 (53) | |
| Assisting | 49 (22) | |
| Aware of VR in surgery, n (%) | Yes | 120 (53) |
| No | 105 (47) | |
| IQR = interquartile range: VR = virtual reality | ||
The present investigation shows that (i.) surgery seems to be of considerable interest among students, but they fear incompatibility of family and surgical work, overtime work and competitive mentality; and (ii.) a short VR intervention increases students’ interest in surgery, however with limited impact on the overall ranking of surgery.
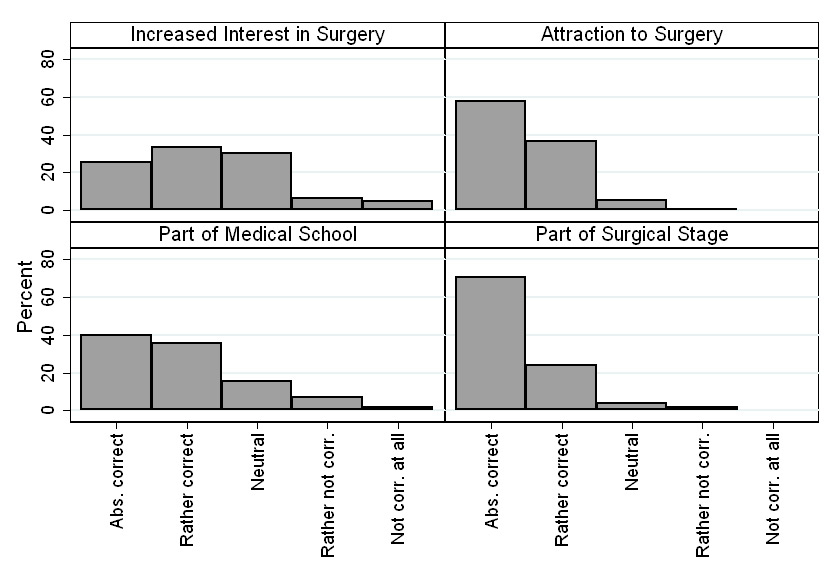
Figure 6
The following aspects apply to the virtual reality (VR) intervention in this study: The VR demonstration has increased my interest in surgery, the VR demonstration increased the attraction of surgery as a career choice, VR demonstrations and exercises should be a formal part of medical school, and the VR demonstrations and exercises should be integrated as formal part of the surgical stage. (Answering options with five descriptors: absolutely correct – rather correct – neutral – rather not correct – not correct at all.)
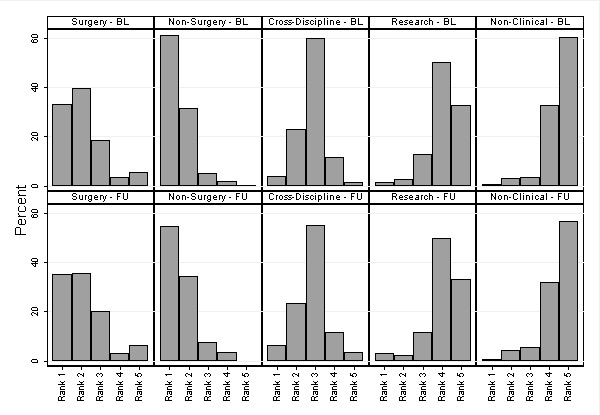
Figure 7
Please rank the following working sectors according to your preference (BL: baseline evaluation, FU: follow-up evaluation after virtual reality intervention)
Surgical sector (general surgery, trauma surgery, orthopaedics, paediatric surgery, gynaecology, otorhinolaryngology, surgical ophthalmology)
Nonsurgical sector (medicine, general practitioner, paediatrics, neurology, psychiatry, dermatology, emergency medicine, nonsurgical ophthalmology)
Cross-disciplinary sector (anaesthesiology, radiology, pathology, legal medicine, laboratory medicine)
Research sector (work in laboratory)
Nonmedical sector (controlling, coding, pharmaceutical industry, media)
To our knowledge this is the first study investigating interest in surgery as well as the impact of a VR intervention on students’ decision-making regarding their future medical specialisation. Several studies have investigated trends in students’ career expectations and underlined surgery’s image problem [5, 8, 11, 15, 17, 30]. Our study combined a survey with a VR intervention in order to highlight the importance of actively interacting with students to attract them to surgery, by breaching preformed attitudes and expectations in medical students’ minds.
This study contributes to the important problem of students deciding against a surgical career, which results in the imminent loss of surgical workforce in the future. It investigates the students’ expectations and VR as a tool to counteract this trend. The challenge for surgical societies and faculties will consist of increasing students’ interest in surgery and providing alternative working modalities to ensuring adequate work-life balance, good teaching and clear career pathways. Focussed mentoring and exposure to positive role models in surgical clerkship can help to increase the number of students deciding on a surgery career [22]. This is all the more important because the majority of medical students in our study were female (58%), reflecting findings of other studies and investigations. In contrast to male students, the majority of female students (70%) rated compatibility of work and family as very important. Thereby, family matters will become even more eminent in the next generation of surgeons, enhancing the emerging work-life challenge in the future for all students, trainees and employers. In our study surgery has, however, been rated as less compatible with most students’ work environment expectations, which reflects the need for a change in surgery as a career option. Working hours, competitive mentality, unclear career perspectives, concerns about family compatibility and inadequate work-life balance were the main drawbacks to starting a surgical career in our study. Some of these apprehensions may, however, be addressed with flexible working conditions and mentorships. Surgical societies have recently started creating mentoring programmes for postgraduates, which may also be successful in influencing undergraduates’ choice of surgery as a career [31]. Hospitals and employers need to find solutions such as part time jobs and adjusted surgical education programmes. Indeed, initial data suggest that mentorship and flexible working conditions can help to prevent trainees from quitting their surgical training programme [31, 32]. The impact of these strategies on surgical training attrition and surgical career decision should be further investigated. Since most students can also envisage working in industry, their work environment expectations need to be taken seriously in order to prevent a further decline of surgical trainees. This applies all the more to surgery with its time-consuming work in operating theatres. Otherwise trends, such as those found in a recent survey [20] involving over 4,000 doctors who dropped out from medical working sector, will continue.
VR may be a useful tool to increase the interest in surgery among students by simulating laparoscopy as one of the standard procedures. However, the impact on ranking of surgery in our study was limited and may decline, since the VR intervention was limited in time to 5 minutes. On this account, longer and repeated VR sessions accompanied by theoretical background and hands-on lessons in the operating room may be necessary to transform students’ general interest in surgery into actual decision-making for a surgical career. Resources in education of medical undergraduates are however limited and most surgical trainees have limited access to VR simulators. Therefore, brief “taster-sessions” on a voluntary base may be an option for surgically interested medical students. Once students have decided on a surgical career, surgical societies and medical directors should take the responsibility to reduce the attrition of surgical trainees by using transparent training programmes, mentorships and providing support regarding family matters.
Although the total number of students and respondents included in this study is exceeded by other national database driven studies [5, 30], our response rate of 87% from all participating students who performed the hands-on VR intervention and received the online questionnaire, is higher than in recent similar cross-sectional studies [8, 11, 16], thus minimising response bias. Taking into account the 209 students who did not take part in these lectures at all or who left early and subsequently did not receive the online questionnaire, the 225 returned online questionnaires would represent 46% of all students in the three academic years investigated (n = 487). However, our response rate is in line with recent findings of other studies [5, 11, 17], although the exact content of the questionnaires used in these studies has frequently not been reported.
When designing this research project, we attempted to address specifically the risk of systematic errors, i.e., biases. We tried to include as many students as possible in three lectures from different academic years in order to reduce selection bias and to reflect the attitude of students at different ages, degrees of life experience and medical knowledge. Using a weekly e-mail reminder, we achieved a high response rate yielding a reduced risk of attrition bias. We randomly ordered the sequence of answering options in order to reduce the possibility that answering was influenced by previous responses. As a result of the time-limited intervention and the web-based questionnaire system, the research question could be answered in a relatively short time period. Although the design of this survey does not allow the attainment of a higher level of evidence, results may be understood as an up-to-date snapshot of students’ work environment expectations in Europe. For the VR intervention, we chose the LAP Mentor from SimbionixTM because of its qualities as a realistic VR tool. Its face validity has been tested [33], enhancing its informative and motivating character to generate enthusiasm among students. Furthermore, VR laparoscopy simulation was chosen in this study to address the increasing importance of minimally invasive surgical techniques in surgery.
Like all questionnaire-based surveys, our results may have some limitations. We reported data from 225 out of 276 participating students. Therefore, results may be influenced by a selection bias. Since the initial short questionnaire during the lecture did not include any questions about baseline characteristics, in order to keep it as short as possible, we are unable to compare baseline characteristics of responders and nonresponders. The response rate of participating students was high, thus lowering the risk of systematic differences. However, out of 485 matriculated medical students in the three academic years evaluated, 209 students did not take part in the visited lectures or left early, which hampers generalisability and may contribute to a selection bias. However, we estimate that the number of students who attended the entire lecture, but did not participate in the study, is fairly low. Introduction of VR was brief and students’ hands-on VR practice was limited owing to the tight lecture schedule. This may contribute to diminishing the effect of the VR intervention on decision-making in the online questionnaire.
Some questions however remain unanswered. It would be interesting to evaluate in more depth the effect of repeated VR interventions on surgical career choice among medical students, for which the optimal design would be a randomised controlled trial (RCT). An RCT might, however, lack acceptability and thus could be replaced by a comparative prospective study with before-after design, which may be more feasible. A prospective comparative study seems necessary because other important issues (such as work-life balance or family concerns) may dissuade students from starting a surgical career, independent of whether VR intervention increased their interest in surgery or not. Of note, should students having undergone such a VR intervention opt for a surgical career, their repeated VR training may positively impact their learning curve and finally contribute to the enhancement of patient safety, especially in their first years of surgical training.
In summary, socioeconomic developments with restrictive budgetary policies in the health system and epidemiological tendencies will generate a lack of surgical workforce in the future. Medical faculties and surgical societies should generate increasing interest in surgery among medical students and provide well-planned training programmes that adhere to compatibility of family life with structured training curricula. VR already is an important adjunct to surgical training programmes, and brief VR hands-on “taster” sessions could be a helpful tool to increase sustainably interest in surgery among medical students, thus balancing the imminent lack of surgeons in the future. In parallel, prospective comparative studies should be conducted to further explore the impact of VR sessions on choice of a surgical career.
1 Terhune KP, Zaydfudim V, Abumrad NN. International medical graduates in general surgery: increasing needs, decreasing numbers. J Am Coll Surg. 2010;210(6):990–6.
2 Ruedin H, Weaver F, Roth M, Widmer M. Gesundheitspersonal in der Schweiz – Bestandesaufnahme und Perspektiven bis 2020;2010.
3 Cooper RA, Getzen TE, McKee HJ, Laud P. Economic and demographic trends signal an impending physician shortage. Heal. Aff. 2002;21(1):140–54.
4 Kmietowicz Z. Shortage of surgeons might threaten NHS targets. BMJ. 2005;330:379.
5 Bland KI, Isaacs G. Contemporary Trends in Student Selection of Medical Specialties. Arch Surg. 2002;137:259–67.
6 Sauer J, Dommisch K. Chirurg – Ein Wunschberuf? Der Chir. BDC. 2006;5:145–148.
7 Ansorg J, Krones C, Schroeder W, Leschber G, Ochel U. Be courageous! No average job: Being a surgeon. Chirurg. 2009:52–3.
8 Boyle E, Healy D, Hill ADK, O'Connell PR, Kerin M, McHug S, et al. Career choices of today’s medical students: where does surgery rank? Ir J Med Sci. 2013;182(3):337–43.
9 Nüssler NC. Surgical graduate education in crisis. Chirurg. 2008;Suppl:86–88.
10 Tolhurst HM, Stewart SM, Medical T. Balancing work, family and other lifestyle aspects: a qualitative study of Australian medical students’ attitudes. MJA. 2004;181(7):361–4.
11 Azizzadeh A, Mccollum C, Charles C, Holliday K, Shilstone H, Lucci A. Medical Students Interested in Surgery. Curr Surg. 2003:210–3.
12 Thiele K, Matziolis D, Perka C. Lack of new trainees in trauma surgery and orthopedics. An approach to a solution. Unfallchirurg. 2010;113(12):1053–6.
13 Saalwachter AR, Freischlag JA, Sawyer RG, Sanfey HA. The training needs and priorities of male and female surgeons and their trainees. J Am Coll Surg. 2005;201(2):199–205.
14 Gensch K. Occupational decisions of young physicians and possible future consequences for the provision of medical care. Results of an anonymous questionnaire. Gesundheitswesen. 2007;69(6):359–70.
15 Baxter N, Cohen R, McLeod R. The impact of gender on the choice of surgery as a career. Am J Surg. 1996;172(4):373–6.
16 Dyrbye LN, Freischlag J, Kaups KL, Oreskovich MR, Satele DV, Hanks JB, et al. Work-home conflicts have a substantial impact on career decisions that affect the adequacy of the surgical workforce. Arch Surg. 2012;147(10):933–9.
17 Businger A, Villiger P, Sommer C, Furrer M. Arguments for and against a career in surgery: a qualitative analysis. Ann Surg. 2010;252(2):390–6.
18 Matthes G, Rixen D, Tempka A, Schmidmaier G, Wölfl C, Ottersbach C, et al. Physicians in traumatology. Critically endangered? Results of an inquiry. Unfallchirurg. 2009;112(2):218–22.
19 Leibrandt TJ, Pezzi CM, Fassler SA, Reilly EF, Morris JB. Has the 80-hour work week had an impact on voluntary attrition in general surgery residency programs? J Am Coll Surg. 2006;202(2):340–4.
20 Spinner G. Gutachten zum “Ausstieg aus der kurativen ärztlichen Berufstätigkeit in Deutschland.”; 2004:1–71.
21 O’Herrin JK, Lewis BJ, Rikkers LF, Chen H. Why do students choose careers in surgery? J Surg Res. 2004;119(2):124–9.
22 Makama JG, Ameh EA. Does general surgery clerkship make a future career in surgery more appealing to medical students? Afr Heal. Sci. 2010;10(3):292–6.
23 Al-Kadi AS, Donnon T, Oddone Paolucci E, Mitchell P, Debru E, Church N. The effect of simulation in improving students’ performance in laparoscopic surgery: a meta-analysis. Surg Endosc. 2012;26(11):3215–24.
24 Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg. 2004;91(2):146–50.
25 Lucas S, Tuncel A, Bensalah K, Zeltser I, Jenkins A, Pearle M, et al. Virtual reality training improves simulated laparoscopic surgery performance in laparoscopy naïve medical students. J Endourol. 2008;22(5):1047–51.
26 Miskovic D, Wyles SM, Ni M, Darzi AW, Hanna GB. Systematic review on mentoring and simulation in laparoscopic colorectal surgery. Ann Surg. 2010;252(6):943–51.
27 Patrício M, Harden RM. The Bologna Process - A global vision for the future of medical education. Med Teach. 2010;32(4):305–15.
28 Michaud PA. Reforms of the pre-graduate curriculum for medical students: the Bologna process and beyond. Swiss Med Wkly. 2012;142:w13738.
29 Newson R. Confidence intervals for rank statistics: Percentile slopes, differences, and ratios. Stata J. 2006;6(4):497–520.
30 Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003;290(9):1173–8.
31 Drolet BC, Sangisetty S, Mulvaney PM, Ryder BA, Cioffi WG. A mentorship-based preclinical elective increases exposure, confidence, and interest in surgery. Am J Surg. 2013.
32 Mayer KL, Perez R V, Ho HS. Factors affecting choice of surgical residency training program. J Surg Res. 2001;98(2):71–5.
33 Ayodeji ID, Schijven M, Jakimowicz J, Greve JW. Face validation of the Simbionix LAP Mentor virtual reality training module and its applicability in the surgical curriculum. Surg Endosc. 2007;21(9):1641–9.
Funding / potential competing interests: This study was supported by the Swiss National Science Foundation grant Nr 3200B0-120722/1.