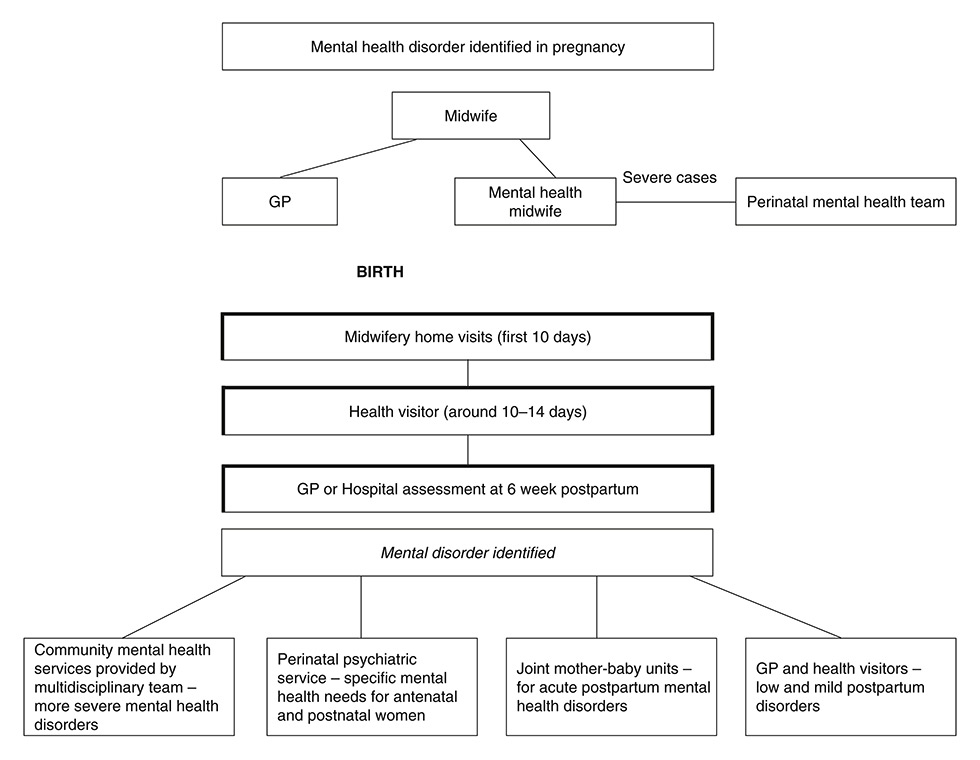
Figure 1
Care pathways offered to perinatal women with mental disorders in the UK.
DOI: https://doi.org/10.4414/smw.2015.14011
Perinatal mental health disorders are a major public health concern and affect a wide range of social, economic and health related outcomes [1]. The period around childbirth is often associated with psychiatric morbidity [2] and in the postpartum period, women face an increased risk of developing a bipolar or a post-traumatic stress disorder [3], or might have a recurrence of a pre-existing psychiatric condition [4]. The epidemiology of perinatal mental health illnesses is well recognised [4, 5]. Postpartum disorders vary in terms of diagnoses and severity and different types of treatment may be applied [5]. Once the right treatment is given, the outcome is usually positive for the woman, her partner, her family, and benefits the child's development [2].
Approximately 12% of women will suffer from depression during pregnancy [6, 7], which is a major risk factor for developing depression at postpartum, and 10–13% will develop postpartum depression [7]. Postpartum blues, the mildest and more common condition, affects about 40–70% of women a few days after birth and usually does not require any treatment [8]. The most severe disorder that may develop after birth is postpartum psychosis with an incidence of 0.1–0.2% [4]. The postpartum period is a time of important psychosocial changes [9, 10]. The new parental role [10], changes in the family relationships [11], altered self-perception and body image [9, 12] are some of the important modifications in a women’s life that may take longer than just the first weeks to resolve [11]. These social and psychological changes, the physical recovery from birth and the care of a new infant, make the first postpartum year a period of increased risk for physical and mental disorders [9, 11, 12]. Maternal mental health problems at this stage are associated with poor health outcomes for the child, early breastfeeding termination, potential negative perception of the infant, delayed child language acquisition, compromised mother-baby bonding, decreased rates of childhood immunisations and increased risk for child behavioural and emotional problems later in life [9, 13, 14].
For more than two decades, suicide was the leading cause of maternal deaths in the United Kingdom (UK) [4]. Its risk is estimated to be 70 times higher in women with psychiatric disorders during the first year after birth compared to the general female population [15]. There is evidence that specialised treatment can reduce duration and extent of maternal psychiatric morbidity, positively affect mother and baby bonding and empower women’s confidence as a mother [4, 16, 17].
Perinatal mental health problems are a challenge for health services, particularly in terms of specific treatment, specialist knowledge, security and availability [1, 2]. The perinatal period is also a chance for health services to treat women, since in pregnancy and postpartum women are very open to advice and support [18, 19].
In general, perinatal mental health services should encompass prevention, detection and management of perinatal mental health disorders [4]. The treatments include medication, psychological care such as guided self-help or talking therapies (e.g., cognitive behavioural therapy, dynamic psychotherapy or interpersonal therapy), exercise and social care such as support and advice [2, 20]. In order to provide a satisfactory service, a good coordination between all health professionals involved in pregnant and postpartum women’s care is essential [4].
Depending on the severity of the disorder and the types of treatment required, perinatal mental health provision, like most services will apply different strategies of care [8]. In a primary care service, which is where people first contact the healthcare system and where the majority of health problems, including mental health care, are dealt with [21], a good and integrated perinatal service would be able to check and screen women antenatally, offering support to the ones in need and provide prevention to women at risk of developing a new disorder or recurrence of a past one [4, 6, 21]. The primary care service is responsible for the most common problems and it provides preventive, curative and rehabilitative services to increase health and well-being [21]. Secondary care consists of the provision of a specialised service by medical specialists or other health professionals on referral by a primary care physician [22]. Consequently, prevention and treatment of low risk and mild mental health disorders is carried out in primary and secondary care since the resources provided in these levels are sufficient to deal with the severity presented [23].
The most severe cases should be treated in tertiary care. This level provides inpatient care and more specialised treatments [4, 23]. Tertiary, specialised perinatal mental health care provides the possibility of hospitalising pregnant women and women with their babies during the postpartum period or during the first year after childbirth [24, 18]. All this requires expertise in treating women’s psychiatric problems as well as expertise in child care and development [24]. Care in a MBU may reduce the effects of maternal problems in the baby’s development [25]. Joint mother-baby treatments intend to treat the mother’s disorders and stimulate mother-baby interactions, secure attachment, promote child development and support parenting [25, 26].
The organisation and provision of perinatal mental health services may vary greatly from country to country [27]. In this paper, we aimed to compare the perinatal mental health services provided in the UK and in Switzerland. The UK has a longstanding tradition in providing perinatal-psychiatric services, and there is also a tradition of continuous surveys on service delivery. Perinatal psychiatry is recognised as a sub-discipline of psychiatry in the UK, therefore these services in the United Kingdom may be useful as “gold standard”.
We intended to detect differences and similarities between two countries with different traditions in psychiatry obtaining information regarding (1.) guidelines, (2.) structure of service provision from the government’s perspective, (3.) numbers of service users if known by the governments or supervising bodies and (4.) possible plans for future development of perinatal-psychiatric services. To the best of our knowledge, reports about the Swiss perinatal mental health provision with information provided by Swiss health authorities are still missing. Furthermore, there are no published comparisons on this topic and between these two countries.
Regarding access to mental health services, Chisholm et al (2004) in his cross sectional study [28] described a rate of 58 psychiatric beds and 11 psychiatrists per 100,000 people in the UK, while in Switzerland this rate was 132 psychiatric beds and 22 psychiatrists per 100,000 people. This shows that both countries are at the top end of intensity of psychiatric service provision. It remains to be investigated whether this is true for sub-sections of psychiatry like perinatal psychiatry as well.
The study was carried out using two different methods and ethical approval was obtained before commencing the study.
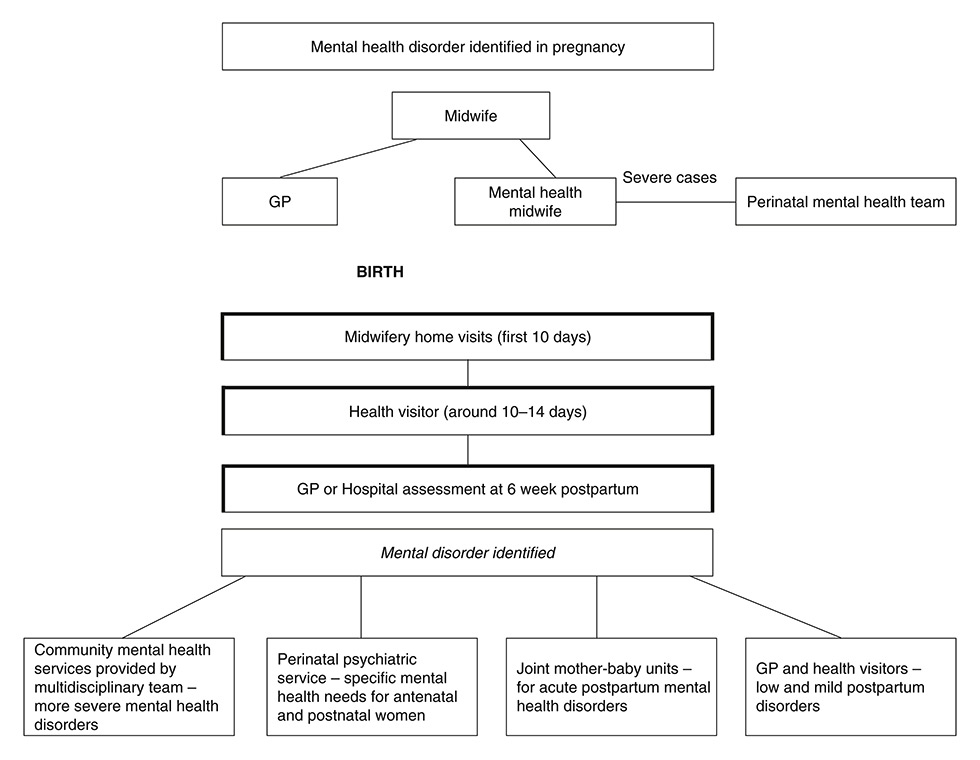
Figure 1
Care pathways offered to perinatal women with mental disorders in the UK.
Firstly, in Switzerland data were obtained from a European study in 2000, with a subsequent follow up survey in 2007. The European Study of Postnatal Depression, funded by the European Commission and the Swiss Federal Office for Sciences, aimed at testing research methods in the field of perinatal psychiatry and collecting relevant background information.
At both time points, in the years 2000 and 2007, health authorities from all 26 Swiss cantons were asked to fill in a postal questionnaire specifically created for this study. Information about mental health care in their canton, perinatal mental health care guidelines, numbers of service users and plans for the development of perinatal mental health care for the following year were asked. All the information given by the health authorities were regarding perinatal mental health services provided in their canton. No patients were interviewed for this purpose. Participation consent was given by the health authorities before taking part in the study. The responding personnel were selected by the government officials responsible for healthcare.
In the UK, information was accessed through a number of key reports commissioned by supervising bodies like the Royal College of Psychiatry, published from 2000 to 2012, [2, 4, 6, 23, 29, 30], providing information on the topic. In general, these studies aimed to give an overview of service provision in the UK across the years, pointing out limitations and needed improvements in mental health care. The data about accessed information can be seen in table 1.
| Table 1: Assessed information about perinatal mental health services in Switzerland and the UK. |
| Perinatal mental health guidelines (policies for antenatal and postnatal treatment) |
| Continuous assessment of perinatal psychiatric services |
| Plans for the future |
| Outpatient services |
| Perinatal psychiatric day hospital |
| Pregnant patients hospitalisation |
| Joint mother and baby hospitalisation on general psychiatric wards |
| Joint mother and baby hospitalisation on female psychiatric wards |
| Joint mother and baby hospitalisation on obstetric wards |
| Specialised inpatient perinatal psychiatric services (mother and baby units) and number of beds |
In Switzerland, mental health care is organised and provided by the department of health in each canton according to its own health guidelines.
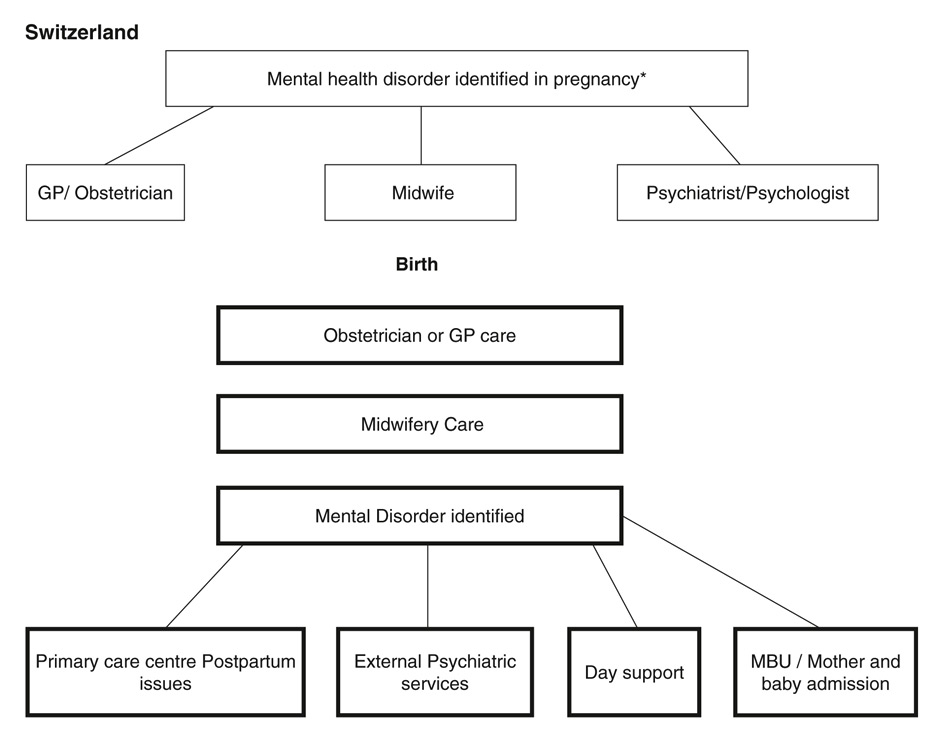
Figure 2
Care pathways offered to postpartum women with mental health disorders in Switzerland.
*Treatment option is chosen by the patient that is free to access any health professional.
At both survey time points (2000 and 2007), 100% of all 26 Swiss cantons contacted about this research returned the questionnaires. None of them reported to be in possession of numbers of service users of specialised in- and outpatient services. Likewise none of them reported current plans of future development of the structure of perinatal psychiatry in their cantons.
In the UK, the National Health Service (NHS) has a wide range of trusts that are responsible for providing and commissioning health (including mental health) and social care services on behalf of the National Health Service in a certain catchment area [6].
In the Swiss survey, the health authorities stated that according to the Swiss healthcare system patients are free to choose any general practitioner (GP), psychiatrist, child psychiatrist, gynaecologist and paediatrician for consultation. In addition, psychiatric hospitals and services of child psychiatry offer outpatient service. The patients can make an appointment with these practices and services directly. It may be useful to know that every citizen has a health insurance that will pay for these consultations. In case the citizen is unable to pay the fees for this insurance the local council will pay these fees [27].
In the year 2000 8% of the cantons and 19% of the cantons in 2007 reported that they provided a specialised perinatal-psychiatric service in their obstetric hospitals while another 15% mentioned cooperating with different cantons to supply this specific care. Swiss outpatient mental health care is delivered by psychiatric clinics, psychiatric practices, and child psychiatric services. Primary health care centres offer assistance in many topics, such as breastfeeding, that are important for mothers with babies.
In the year 2000 [4], in the UK, the Royal College of Psychiatry published a Council Report reviewing the importance of perinatal mental health together with strategies and existing service provision. At that time point, less than 50% of national health authorities offered perinatal specialist consultation or perinatal mental health community teams.
In 2005 [29], Oluwatayo and Friedman conducted a survey which aimed to investigate the specialist perinatal-psychiatric provision and opinions about these services in 78 mental health trusts in England. The final response rate was 73%; corresponding to 57 trusts out of the 78 initially contacted. The response personnel were mostly clinicians (65%). From the participating trusts, 35% had a multidisciplinary perinatal mental health team, 19% had one or more full time psychiatric nurses in their team and 10.5% had no community team at all.
In 2007, the National Institute for Health and Care Excellence (NICE) guidelines on clinical management and service guidance in the UK [6] showed that from 48% of primary care trusts responding to a survey (n = 144), which aimed to gain an understanding of service provision within primary care, 21% had a perinatal mental health team consisting of nurses, psychiatrists and mental health workers. From these 21%, 32% of mental health services given to postpartum women were provided via community teams.
The guidance for commissioners of perinatal mental health services [2] prepared by the Joint Commissioning Panel for Mental Health in the UK in 2012, discusses the commissioning of good quality perinatal mental health services. It states that in the country there are a total of 19 specialised perinatal community teams in place.
Regarding semi-outpatient perinatal mental health treatment (i.e., day hospitals), 23% of Swiss cantons offered this service in 2000, while in 2007 this offer was reduced to 8%.
In the UK, the 2005 survey [29] found that only3.5% of the respondent mental health trusts had a full time perinatal psychiatrist and in more than 90% of these, the consultants were liaison psychiatrists. Only 4% offered day hospital treatment while 9% offered intensive home treatment.
In the 2007 [6] survey, from the 21% of trusts that had a perinatal mental health team, the services of 42% were provided as part of comprehensive specialist services, including inpatient services, and a further 21% were provided via other services such as mental health centres or liaison psychiatrists.
According to the 2000 survey in Switzerland, inpatient mental health treatment for pregnant women on general psychiatric wards was offered in 100% of Swiss cantons. In 2007, 92% of the cantons reported to be offering the same type of inpatient treatment. Joint postpartum mother with baby admission on general psychiatric wards was provided by 19 cantons (73%) in 2000 rising to 24 cantons (92%) offering this service in 2007. Adult psychiatrists and child psychiatrists were described to be responsible for service delivery in these facilities within medicine.
In the seven-year gap between the first survey and the follow up, three (11.5%) cantons implemented specialised perinatal-psychiatric units (1 unit per 2.5 million people), which more specifically were perinatal-psychiatric mother-baby units, offering from 3–8 beds in each one.
According to the Royal College of Psychiatrists Council Report, in 2000 [4] there were 10 specialist psychiatric mother-baby units in the UK offering 6 or more beds. Inpatient joint mother-baby admissions were offered by a large number of psychiatric units, but less than 50% of national health authorities had mother-baby units.
In the UK survey conducted in 2005 [29], 37% (n = 21) of the respondent trusts had specialised perinatal psychiatric units, but one third of these facilities were placed in a general psychiatric unit. Two of them were mother-baby units with 2 beds, 3 units with 5–8 beds, 6 units with 3–4 beds and the rest had only 2 beds. From the 57 respondent trusts, 23% provided the whole range of services from inpatient care, intensive home treatment to obstetrics wards and liaison clinical services, while 46% had either inpatient or intensive home treatment. The remaining trusts had no perinatal facilities and half of them arranged beds with neighbouring trusts when necessary.
In a report done in 2006 [30], describing the situation of maternal mental health care in the UK, among other related topics, it was found that less than 50% of mental health trusts had some kind of perinatal mental health services. At that time point, 12% of inpatient mother-baby admissions were carried out on general psychiatric wards and 31.1% of pregnant women diagnosed with a mental illness were put on a waiting list to receive treatment. Despite this, since 2006, joint mother-baby admissions were advised to be done in specialized mother-baby units only, where mothers and babies can receive adequate care [2].
In the 2007 report [6], 31% of respondents had a perinatal-psychiatric unit or beds specifically for perinatal women, 40% used perinatal-psychiatric units outside the trust and 52% used general psychiatric beds for mothers without admitting their babies. At that time point, there were 19 specialised perinatal-psychiatric units with 126 available beds in the UK.
In the most recent report, [2] 22 perinatal-psychiatric units were in place in the UK (1 unit per 2.8 million people). A total of 19 units were in England, 2 in Scotland, 1 in Wales, offering a total of 168 beds. No perinatal-psychiatric unit was in place in Northern Ireland. This report suggested that there is a national deficit of about 50 beds for inpatient mother-baby treatment. 50% of the UK perinatal-psychiatric units work closely with 11 specialised perinatal community teams, less than 50% of all mental health trusts in the UK provide perinatal mental health services and large areas of the country have no specialised facilities. Due to this fact, women need to travel long distances to the next available perinatal-psychiatric unit or are admitted to psychiatric general wards without their babies.
The current structure of perinatal mental health services provided in both countries is shown in table 2, where the range of services provided for outpatient and inpatient care is described.
In 2000, no canton in Switzerland had guidelines or development policies for perinatal mental health provision. In 2007, only one canton had developed specific guidelines for the provision of perinatal mental health care.
Data regarding the number of treatments offered per year in each level of care by each canton is missing at both time points in the Swiss survey. Although all cantons returned the questionnaires, this specific item was never filled in. The same happened to the topic plans for future development, since no canton reported plans for future implementation of perinatal mental health services.
In the 2005 UK research [29], documents and protocols with guidelines for management of perinatal disorders as well as mother-baby admission policies and strategies of perinatal mental health care were described as being in place by the respondent trusts, but were considered inadequate or outdated in 48% of them.
In 2007, the National Institute for Health and Care Excellence (NICE) guidelines on clinical management and service guidance [6] showed that around 25% of primary care trusts responding to its survey in the UK had developed and implemented policy for antenatal and postnatal mental health provision.
The 2012 [2] report reinforces the importance of guidelines for the provision of perinatal mental health care, not only citing the NICE guidelines, but a number of other documents developed by Health authorities in the UK .
| Table 2: Perinatal mental health service structure in all levels of care in the UK and in Switzerland. | |
| Swiss perinatal mental health service | UK perinatal mental health service |
| Specialised inpatient perinatal psychiatric units (for pregnant women and mothers with babies) | Specialised inpatient perinatal psychiatric units (for pregnant women and mothers with babies) |
| Joint mother and baby hospitalisation on general psychiatric wards | Not advised |
| Joint mother and baby hospitalisation on female psychiatric wards | Not advised |
| Joint mother and baby hospitalisation on obstetric wards | Not advised |
| Day hospital | Day hospital |
| Psychiatric clinics / practices | Psychiatric clinics / practices |
| Clinical psychology/psychiatry services linked to maternity hospitals | Clinical psychology/psychiatry services linked to maternity hospitals |
| Not reported, however possible. | Perinatal specialist professionals in / in cooperation with: – Maternity services – General adult services – GP practices – Health visitors |
| Child psychiatric services | Parenting and infant mental health services |
| Specialised community mental health teams | Specialised community mental health teams |
| – | Guidelines and continuous evaluation of services |
Failing to deal with perinatal mental health problems at any level has adverse consequences for the woman, her partner and her baby. Pregnant women are in frequent contact with health services and consequently there are many opportunities for prevention, early detection and adequate treatment [4, 18]. Without adequate care, 30% of women with postpartum depression are still ill at one year postpartum [4, 5, 6]. Prolonged mental disorders in women can contribute to marriage disruption, and negative effects on families and older children [4, 10].
In general, the human resources needed to organise a perinatal metal health service can be calculated from the country’s annual birth rate and information about the epidemiology of perinatal disorders in the area [4]. This was discussed in the UK 2000 report. The number of live births in the UK was 690,000 in 2007 and 729,000 in 2012 [31]. In Switzerland in 2007 the number was 74,494 and 82,164 in 2012 [32].
The data collected for this report suggest that Switzerland and the UK share the same principles of service provision for pregnant women and women in the first postpartum year. A chain of services is offered ranging from mental health teams in primary care to outpatient and inpatient specialised services (see diagrams 1 and 2 below).
The proportion of specialised perinatal mental health teams varied across the years in the UK. In 2000, the Royal College of Psychiatry report stated that less than 50% of all trusts in the UK had a perinatal mental health community team, while in 2005, [29] 35% of the mental health trusts had a specialised team. In 2007, 21% of the primary care trusts reported to have a perinatal-psychiatric team, including a community team. The mental health teams are one of the key tools in perinatal mental health care since they have a close link to the mother before and after birth, are aware of women’s medical history, alert to the possibility of development or recurrence of mental health problems, can effectively detect such problems and refer women to more specialised services if required [2]. Not providing this essential aspect of care means that women will take longer to be detected and treated by a specialised service, potentially compromising maternal care which brings short and long-term effects on the child development [9, 11, 13, 14].
With less than 50% of the country (UK) having specialised perinatal mental health care and large areas with no specialised facilities at all [2, 4, 23], appropriate service alternatives should be in place. The data showed that mental health teams are insufficient in number and perinatal home treatment and day hospitals are hardly mentioned or provided by trusts despite reported as being part of the structure of services as seen in table 2. According to the NICE report [6], the majority of women with mental disorders only need to be treated by the primary care level.
In Switzerland, specialised outpatient’s treatment provided in the cantons more than doubled between the two time points of the survey. Switzerland has a strong network of free primary care centres, providing assistance to women antenatally and postnatally on topics such as nutrition, sleep problems, breastfeeding and maternal as well as paternal psychological problems [27]. This might be a possible explanation for the high rate of usage of these Swiss services instead of a direct contact with mental health specialists. Specialists from the primary care centres can also refer their patients to psychiatrists and arrange individual counselling and day support [26]. However, the day hospital offer (semi outpatient) decreased between the two time points with only 2 cantons offering this type of treatment in 2007.
With the increasing number of perinatal-psychiatric units in the UK from 10 in 2000 [4] to 22 units in 2012 [2] – also increasing the bed offer from around 80 to 168 – service provision is more concentrated in the tertiary care. It is possible that more specialised mental health teams available would diminish hospital admissions and provide adequate care in the community [28]. Meanwhile, with more mother-baby units it is possible to accomplish the national health regulation of not admitting mother and babies in a non-specialised psychiatric ward. Nevertheless, according to the Mind report [30] in 2006, 12% of women were still admitted with their babies to non-specialised adult psychiatric wards. Despite improvement of the bed offer in mother-baby units, there is still a national shortfall that would correspond to 5–8 perinatal-psychiatric units [2]. Care in a specialised unit may reduce the effects of maternal problems on the baby’s development while treating the mother’s disorder [24].
Before 2007, there were no specialised perinatal-psychiatric units in Switzerland, so mothers with babies and pregnant women in need of psychiatric care were admitted to non-specialised wards providing psychiatric treatment. In 2007, three Swiss cantons implemented perinatal-psychiatric units and all of them focused on postpartum care. None of the cantons where the specialised perinatal-psychiatric units were implemented developed perinatal mental health guidelines.
Although the number of perinatal-psychiatric units has increased in the UK in the last years, primary care services are insufficient in number or non-existent [2, 4, 6], unlike Switzerland which has a strong network of primary mental health services offered to women and their partners. On the other hand, the late implementation of perinatal-psychiatric units in Switzerland meant that pregnant women and mothers with babies were admitted to non-specialised obstetric or psychiatric wards, a practice not considered advisable in the UK. However, since there are large areas in the UK without any kind of perinatal service provision, it can be assumed that many women in need of more acute care were admitted to general psychiatric wards without their babies [23, 30].
Many efforts have been made in order to provide excellent guidelines for organisation and clinical management of perinatal mental health services in the UK. A commission panel for mental health is in place in order to help and support the delivery of the UK government health strategy [2]. The NICE clinical guidelines [6] provide guidance on clinical and service management, giving clear information about perinatal service implementation as well as recommendations and advice to professionals, in order to ensure a uniform national approach in the three levels of care. In Switzerland, each canton is responsible for developing, implementing and commissioning its own health service guideline. During the seven-year gap between the first survey and the follow up, only one canton developed perinatal mental health care guidelines, despite the fact that all of them provided mental health services antenatally and at postpartum. This suggests there is no agreed minimum standard in service provision in each level of care and also no clear approach about how the service should be delivered. This is even more concerning in cantons that now provide perinatal-psychiatric units. Guidelines, including recommendations for treatment, management, advice and types of appropriate care based on the best available evidence [6] are essential and would benefit practitioners, guarantee a common standard of services and provide the best treatment to patients.
Women are in constant contact with medical services during pregnancy and at postpartum and this is an important opportunity to anticipate and prevent the occurrence of psychiatric disorders and to carry out rapid and appropriate intervention [4, 5, 7]. All women experiencing a perinatal disorder should have access to suitable treatment at the level of care appropriate for their needs. Thus, services should seek to provide the most effective and accessible care with the lowest degree of intrusion and disruption to the new mother’s life [6].
Our study is limited by its design and data. The data recording in both countries is not as comprehensive as needed to obtain complete information about services provided, since there is not enough information about community teams or main components of mental health teams. In the Swiss survey, the questionnaire was sent to the departments of health only. Therefore, efforts made by other departments of the Swiss canton (state) governments for pregnant and postpartum women and their families – in the fields of child protection for example – have not been assessed. The data regarding the number of treatments offered per year in each level of care by each canton are missing at both time points and the most recent Swiss data was collected in 2007. Also, we were unable to access information about main psychiatric diagnoses that led to the design of the current Swiss service structure. In the UK, data are based on national reports done by different health authorities in the country using different data collection methodologies. The data could be biased since the respondent trusts from all studies were likely to be most interested in the area.
In conclusion, this comparison study shows that despite improvements in the last years, perinatal mental health services remain uneven, and concentrated in few areas in the UK. It remains unclear to what extent the three Swiss perinatal-psychiatric units are in charge of the most severely ill perinatal patients. With the exception of one canton, guidelines are missing in Switzerland.
Acknowledgement:The authors would like to thank Professor Vivette Glover, Imperial College London, and Dr Alyx Taylor, King’s College London, for their valuable comments to this paper.
1 The World Health Report: 2005: make every mother and child count. World Health Organization, 2005.
2 Joint Commissioning Panel for Mental Health. Guidance for commissioners of perinatal mental health services. London: JCP-MH; 2012.
3 Munk-Olsen T, Jones I, Laursen TM. Birth order and postpartum psychiatric disorders. Bipolar Disord. 2014;16(3):300–7.
4 Royal College of Psychiatrists. Perinatal Maternal Mental Health Services. London; 2000.
5 O’Hara MW, Swain AM. Rates and risk of postpartum depression – a meta-analysis. International Review of Psychiatry. 1996;8(1):37–54.
6 Antenatal and Postnatal Mental Health: The NICE Clinical Management and Service Guidance. Nice Clinical Guidelines N45. National Collaborating Centre for Mental Health (UK). 2007.
7 Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews 2013, Issue 2. Art. No.: CD001134. DOI: 10.1002/14651858.CD001134.pub3.
8 Hedegaard M, Henriksen TB, Sabroe S, Secher NJ. Psychological distress in pregnancy and preterm delivery. British Medical Journal. 1993;307:234–9.
9 Nappi RE, Petraglia F, Luisi S, Polatti F, Farina C, Genazzani AR. Serum Allopregnanolone in Women With Postpartum Blues. Obstetrics & Gynecology. Volume 97, Issue. 2001;1:77–80.
10 Staehelin K, Kurth E, Schindler C, Schmid M, Stutz EZ. Predictors of early postpartum mental distress in mother with midwifery home care – results from a nested case-control study. Swiss Med Wkly. 2013;143:w13862 http://www.smw.ch/content/smw-2013-13862/
11 Fahey, JO, Shenassa, E. Understanding the needs of women in the postpartum period: The perinatal mental health promotion model. Journal of midwifery and women’s health. 2013; 613–21.
12 Mercer, RT. Becoming a mother versus maternal role attainment. J Nurs Scholarsh. 2004;36(3):226–32.
13 Hill, PD, Aldag, JC.Maternal perceived quality of life following childbirth. J Obstet Gynecol Neonatal Nurs. 2007;36:328–34.
14 Rallis S, Skouteris H, Wertheim EJ, Paxton SJ. Predictors of body image during the first year postpartum: A prospective study. Women Health. 2007;45(1):87–104.
15 Mendez-Bustos P, Lopez-Castroman J, Boca-Garcia E, Ceverino A. Life cycle and suicidal behaviour among women.The Scientific World Journal. 2013;1–9.
16 Kahn RS, Zuckerman B, Bauchner H, Homer CG, Wise, P. Women’s health after pregnancy and child outcomes at age 3 years: A prospective cohort study. Am J Public Health. 2002;92(8):1312–8.
17 Minkovitz CS, Strobino D, Scharfstein D, How W, Miller T. Maternal depressive symptoms and children’s receipt of healthcare in the first 3 years of life.Pediatrics. 2005;115(2):306–3012.
18 Goodman J. Women’s Attitudes, Preferences, and Perceived Barriers to Treatment for Perinatal Depression. Birth. 2009;36:1,60–9.
19 Blöchlinger P, Kurth E, Kammerer M, Frei IA. What women want: a qualitative study about postnatal midwifery care at home. Pflege. 2014;27(2):81–91.
20 National Health System (NHS) Choices: postnatal depression treatment. Retrieved online on April, 15th, 2014 from http://www.nhs.uk/Conditions/Postnataldepression/Pages/Treatment.aspx
21 WHO Regional Office for Europe’s Evidence Network (HEN). What are the advantages and disadvantages of restructuring a health care system to be more focused on primary care services? WHO, 2004.
22 Mosby’s Medical Dictionary. Mosby, 2009, 8th Edition.
23 Centre for Mental Health, Department of Health, Mind, NHS Confederation Mental Health Network, Rethink Mental Illness, Turning Point. No Health without Mental Health: Implementation Framework. 2012.
24 Glangeaud-Freudenthal, NMC, Howard, L, Sutter-Dallay, AL. Treatment – Mother-infant inpatient units. Best practice and Research Clinical Obstetrics and Gynaecology. 2014;147–57.
25 Kumar R, Hipwell AE. Development of a clinical rating scale to assess mother-infant interaction in a psychiatric mother-baby unit.BR J Psychiatry. 1996;169:18–26.
26 Seneviratne G, Sue C, Marks M. Parenting assessment in a psychiatric mother and baby unit.Br J Work 2003;33:535–55.
27 Asten P, Marks MN, Oates M. Aims, measures, study sites and participant samples of the Transcultural Study of Postnatal Depression. The British Journal of Psychiatry. 2004;184:s3–s9.
28 Chisholm D, Conroy S, Glangeaud-Freudenthal NMC, Oates MR, Asten P, et al., TCS-PND Group. Health Services research into postnatal depression: results from a preliminary cross-cultural study. Br J Psychiatry Suppl. 2004 Feb;46:s45–52.
29 Oluwatayo O, Friedman T. A survey of specialist perinatal mental health services in England. Psychiatric Bulletin 2005;29:177–9.
30 Mind Week Report. Out of the blue? Motherhood and Depression. Mind (National Association for Mental Health); 2006.
31 Office for National Statistics. Statistical Bulletin: Births in England Wales. Retrieved online on March, 31st, 2014 from http://www.ons.gov.uk/ons/rel/vsob1/birth-summary-tables--england-and-wales/2012/stb-births-in-england-and-wales-2012.html
32 Swiss Federal Statistical Office. Retrieved online on April 10th, 2014 from http://www.bfs.admin.ch/bfs/portal/en/index/themen/01/06/blank/key/02/05.html
Authors’ contribution: RT Amiel Castro and K Schroeder contributed equally
Funding / potential competing interests: European Commission and Swiss Federal Office for Sciences, Bern, Switzerland (Grant Nr. BBW 07.0034). Fondation Quality of Life, Geneva, Switzerland