Comparison of clinical and angiographic prognostic risk scores in elderly patients presenting with acute coronary syndrome and referred for percutaneous coronary intervention
DOI: https://doi.org/10.4414/smw.2015.14049
Giuseppe
Vassalli, Ilaria
d’Angeli, Frank
Scherff, Daniel
Sürder, Antonio
Mantovani, Elena
Pasotti, Catherine
Klersy, Angelo
Auricchio, Tiziano
Moccetti, Giovanni B.
Pedrazzini
Summary
BACKGROUND: Multiple risk prediction models have been validated in all-age patients presenting with acute coronary syndrome (ACS) and treated with percutaneous coronary intervention (PCI); however, they have not been validated specifically in the elderly.
METHODS: We calculated the GRACE (Global Registry of Acute Coronary Events) score, the logistic EuroSCORE, the AMIS (Acute Myocardial Infarction Swiss registry) score, and the SYNTAX (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery) score in a consecutive series of 114 patients ≥75 years presenting with ACS and treated with PCI within 24 hours of hospital admission.
Patients were stratified according to score tertiles and analysed retrospectively by comparing the lower/mid tertiles as an aggregate group with the higher tertile group. The primary endpoint was 30-day mortality. Secondary endpoints were the composite of death and major adverse cardiovascular events (MACE) at 30 days, and 1-year MACE-free survival. Model discrimination ability was assessed using the area under receiver operating characteristic curve (AUC).
RESULTS: Thirty-day mortality was higher in the upper tertile compared with the aggregate lower/mid tertiles according to the logistic EuroSCORE (42% vs 5%; odds ratio [OR] = 14, 95% confidence interval [CI] = 4–48; p <0.001; AUC = 0.79), the GRACE score (40% vs 4%; OR = 17, 95% CI = 4–64; p <0.001; AUC = 0.80), the AMIS score (40% vs 4%; OR = 16, 95% CI = 4–63; p <0.001; AUC = 0.80), and the SYNTAX score (37% vs 5%; OR = 11, 95% CI = 3–37; p <0.001; AUC = 0.77).
CONCLUSIONS: In elderly patients presenting with ACS and referred to PCI within 24 hours of admission, the GRACE score, the EuroSCORE, the AMIS score, and the SYNTAX score predicted 30 day mortality. The predictive value of clinical scores was improved by using them in combination.
Introduction
Primary percutaneous coronary intervention (PCI) is commonly performed in patients presenting with ST-segment elevation myocardial infarction (STEMI). In addition, it is performed in a large subset of patients presenting with an acute coronary syndrome (ACS) other than STEMI, including non-ST-segment elevation myocardial infarction (NSTEMI) and unstable angina [1]. Identifying high-risk patients among those presenting with ACS has far reaching clinical consequences [2]. Thus, multiple patient-based risk prediction models have been validated in all-age populations of patients presenting with ACS and referred to PCI. Most of these models rely largely or entirely on clinical variables [3–6]. The GRACE (Global Registry of Acute Coronary Events) score was validated in more than 20,000 patients recruited between 1999 and 2003. This score predicted mortality at six months in patients discharged after an ACS episode [3]. Its use for risk stratification in ACS was recommended by clinical practice guidelines [7]. The logistic EuroSCORE (European System for Cardiac Operative Risk Evaluation) originally was validated as a method of predicting the mortality risk during, or shortly after, heart surgery [8]. Subsequently, this score was validated in patients referred for other cardiovascular interventions including PCI with unprotected left main disease [9–11] or multivessel coronary artery disease [12]. The AMIS (Acute Myocardial Infarction [AMI] in Switzerland) risk score was developed within the context of the AMIS Plus National Registry [13] and includes seven clinical variables. It accurately predicted intra-hospital mortality in AMI patients (C statistics = 0.842) [14].
The SYNTAX (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery) score was developed as a comprehensive approach for the prospective quantification of coronary lesions with respect to their number, location, and anatomical complexity [15, 16]. This anatomical score was pioneered to aid in decision making in patients with complex coronary artery disease (CAD) allocated to PCI or coronary artery bypass graft (CABG) surgery in the landmark SYNTAX trial [16]. Subsequently, the SYNTAX score was validated for risk prediction in patients referred for PCI with multivessel disease [17–18] or unprotected left main disease [19–22], as well as in the general population undergoing PCI [23] and in patients with STEMI [24, 25] or NSTEMI undergoing PCI [26]. As such, the SYNTAX score is advocated in European and US guidelines as a tool to help clinicians decide the optimum revascularisation approach in patients with complex CAD.
Elderly patients presenting with ACS are a high risk group [27]. While most studies of risk prediction models in ACS patients have been carried out in all-age groups, elderly patients were under-represented in these studies. If not excluded by age, numerous elderly patients were excluded from these studies because of existing co-morbidities or other serious systemic illnesses.
Unfortunately, data on risk prediction in the elderly presenting with ACS and referred for PCI are scarce. We recently reported that the SYNTAX score predicted early mortality in elderly patients presenting with ACS and referred for PCI within 24 hours of admission to the hospital [28]. Here, we compared the predictive value of clinical scores including the GRACE score, the logistic EuroSCORE, and the AMIS score with the SYNTAX score in this group of patients.
Methods
Study population
All patients ≥75 years who were admitted to our institution with ACS during 2007 and 2008, had no exclusion criteria, and were treated by PCI within 24 hours of hospital admission were included in a retrospective analysis. ACS and STEMI were defined according to the guidelines of the European Society of Cardiology [29–31]. Exclusion criteria included previous CABG surgery or clinical indication for emergent CABG surgery; however, they did not include previous PCI. The decision to perform PCI, to treat additional coronary lesions beyond the infarct-related lesion, and to implant bare metal stents (BMS) or drug eluting stents (DES) was at the discretion of the operator. There was no restriction on the number of implanted stents.
Score systems
The logistic EuroSCOREincludes cardiac-related factors (unstable angina, LV function, recent myocardial infarction, pulmonary hypertension), other patient-related variables (age, gender, chronic pulmonary disease, peripheral artery disease, neurological disease, previous cardiac surgery, serum creatinine >200 microm/l, active endocarditis, critical preoperative state), and procedure-related variables (emergency other than isolated CABG, surgery on thoracic aorta, post-infarct septal rupture) [8]. The score was calculated using an online calculator (http://www.euroscore.org).
The GRACE score includes several conditions such as age, Killip-class, systolic blood pressure, heart rate, serum creatinine, cardiac arrest at admission, ST-segment deviation, and elevated serum levels of cardiac enzymes [3].
The AMIS risk scoreincludes seven clinical variables (age, gender, systolic blood pressure and heart rate on admission, Killip-class, pre-hospital resuscitation, history of heart failure, history of cerebrovascular disease/stroke) [13, 14]. This score was determined using an online calculator (http://www.amis-plus.ch/amis_risk_model.htm).
The SYNTAX scorewas calculated by scoring separately, from the baseline angiogram, each coronary lesion causing >50% diameter stenosis in vessels >1.5 mm in diameter, and then adding together the individual scores using the SYNTAX score online calculator (http://www.syntaxscore.com) [15]. For each patient, all angiographic variables involved in the calculation of the SYNTAX score were computed by two independent investigators who were blinded to all clinical data. Because patients with STEMI were excluded from the initial SYNTAX score algorithm [15, 16], there currently is no extensively validated method of calculating the score in STEMI patients. We therefore followed a method used for this purpose in recent studies in STEMI patients [24, 25]. If the infarct-related artery was occluded, it was scored as an occluded artery of <3 months’ duration.
Data collection
Baseline data were assessed retrospectively. Patients were invited to a 12 month follow-up interview, which was performed using a standardised protocol. They agreed to participate in the interview, and to have their clinical data collected and used for statistical analyses within the scope of the study. No ethical approval was required for this observational study. The patients’ out-hospital caring physicians were contacted by phone. Hospital admissions and major adverse cardiovascular events (MACE), defined as the composite of death, target vessel revascularisation, AMI and stroke after baseline PCI were monitored. All documents regarding hospital admissions, out-hospital medical examinations, and fatal events were collected.
Statistical methods
Data were described as mean and standard deviation (SD) if continuous, and as counts and % if categorical (tables 1 and 2). They were compared between score groups by means of the test for trend.
Analyses of death or MACE at 30 days:The predictive role of the logistic EuroSCORE, the GRACE score, the AMIS score, and the SYNTAX score with respect to mortality at 30 days, the study’s primary end point, or rates of MACE at 30 days, one of the two secondary end points of the study, was assessed with the logistic model, both with scores on a continuous scale and categorised as the aggregate lower/mid vs upper tertile (defined as the "high-risk" tertile). Tertile categorisation reflects the clinical practice of identifying high risk patients. Aggregating lower and mid tertiles into a single group was used in order improve the statistical power of the analysis. In addition, a combined score was computed by adding up the number of score models according to which a patient was classified in the “highrisk” tertile. To assess the predictive accuracy (discrimination ability) of scores, we computed the areas under the receiver operator characteristic (ROC) curves (and 95% confidence intervals; CI) and compared them between models. Because combinations of models are of interest when the individual models do not significantly overlap, we computed the Kappa statistic (and standard error) and the Lin’s concordance correlation coefficient (with 95% CI) to measure the agreement of any two scores.
Analysis of MACE at one year: Rates of MACE at one year, one of the study’s secondary end points, was described by means of the Kaplan-Meier method (in terms of event-free survival) and compared between groups with a Cox model. Follow-up was computed from the time point of PCI. The Harrell’C statistic (with 95% CI) was computed to measure model discrimination ability (highest discrimination ability, Harrell’C value = 1) and compare models. Stata 13 (College Station, TX, USA) was used for computation. A two-sided p<0.05 value was considered statistically significant.
|
Table 1: Baseline clinical characteristics of the study population either non-stratified or stratified in the higher and the aggregate lower/mid tertiles according to the clinical scores (log EuroSCORE, GRACE score, AMIS score). |
|
|
Overall population n = 114
|
Log EuroSCORE
Overall population (34.9 ± 17.9)
n = 113
|
GRACE Score
Overall population (19.5 ± 22.4)
n = 114
|
AMIS Score
Overall population (19.9 ± 26.9)
n = 112
|
|
|
|
Lower/mid tertiles(24.5 ± 7.1)
|
Higher tertile
(56.2 ± 14.0)
|
p
|
Lower/mid tertiles(7.3 ± 3.6)
|
Higher tertile
(45.2 ± 23.8)
|
p
|
Lower/mid tertiles(4.5 ± 2.8)
|
Higher tertile
(50.5 ± 27.8)
|
p
|
|
|
|
n = 82
|
n = 31
|
|
n = 79
|
n = 35
|
|
n = 77
|
n = 35
|
|
| Age, mean (SD) |
79.6 ± 4.1 |
79.1 ± 3.8 |
80.7 ± 4.3 |
0.028 |
79.0 ± 3.8 |
80.9 ± 4.3 |
0.07 |
79.2 ± 4.0 |
80.5 ± 4.1 |
0.12 |
| Male sex, n (%) |
76 (66.7) |
55 (67.0) |
20 (64.5) |
0.798 |
54 (67.5) |
22 (64.7) |
0.773 |
51 (65.3) |
24 (68.5) |
0.74 |
| Diabetes, n (%) |
23 (22.3) |
14 (19.1) |
8 (27.5) |
0.354 |
12 (17.1) |
11 (33.3) |
0.067 |
10 (14.2) |
13 (40.6) |
0.003 |
| Hypertension, n (%) |
80 (72.0) |
61 (76.2) |
18 (60.0) |
0.093 |
57 (73.0) |
23 (69.7) |
0.718 |
54 (71.5) |
25 (73.5) |
0.791 |
| Current smoking, n (%) |
11 (9.8) |
8 (9.8) |
3 (10.0) |
0.899 |
9 (11.3) |
2 (6.0) |
0.438 |
9 (11.6) |
1 (2.9) |
0.531 |
| Hyperlipidaemia, n (%) |
48 (46.6) |
36 (49.2) |
12 (41.8) |
0.471 |
36 (51.4) |
12 (36.3) |
0.155 |
31 (44.9) |
17 (51.5) |
0.535 |
| Family history of CAD, n (%) |
16 (16.3) |
14 (20.0) |
2 (7.1) |
0.122 |
13 (19.4) |
3 (9.6) |
0.228 |
12 (17.9) |
4 (13.3) |
0.577 |
| Previous myocardial infarction, n (%) |
6 (12.5) |
5 (15.1) |
1 (7.1) |
0.457 |
5 (13.9) |
1 (8.3) |
0.618 |
4 (11.4) |
2 (15.3) |
0.716 |
| Previous PCI, n (%) |
11 (9.7) |
10 (12.2) |
1 (3.2) |
0.153 |
7 (8.7) |
4 (11.7) |
0.62 |
7 (8.9) |
4 (11.4) |
0.685 |
| Renal insufficiency, n (%) |
15 (13.2) |
4 (4.8) |
11 (35.5) |
0.001 |
7 (8.7) |
8 (23.5) |
0.033 |
5 (6.4) |
10 (28.5) |
0.001 |
| Peripheral vascular disease, n (%) |
5 (4.4) |
3 (3.6) |
2 (6.4) |
0.521 |
5 (6.2) |
0 (0) |
0.138 |
5 (6.4) |
0 (0) |
0.127 |
| Previous stroke, n (%) |
4 (8.3) |
1 (3.2) |
3 (18.7) |
0.074 |
2 (5.5) |
2 (16.7) |
0.233 |
1 (3.1) |
3 (18.7) |
0.068 |
| COPD, n (%) |
15 (13.2) |
7 (8.5) |
8 (25.8) |
0.016 |
13 (16.2) |
2 (5.8) |
0.136 |
11 (14.1) |
4 (11.4) |
0.7 |
| Sinus rhythm, n (%) |
103 (92.0) |
78 (96.3) |
24 (80.0) |
0.005 |
75 (94.9) |
28 (84.8) |
0.075 |
74 (94.8) |
28 (84.8) |
0.078 |
| STEMI, n (%) |
87 (76.3) |
59 (71.9) |
27 (87.1) |
0.094 |
58 (72.5) |
29 (85.2) |
0.143 |
60 (76.9) |
26 (74.3) |
0.762 |
| Cardiogenic shock, n (%) |
19 (16.7) |
3 (3.6) |
16 (51.1) |
<0.001 |
0 (0) |
19 (55.8) |
<0.001 |
2 (2.5) |
17 (48.5) |
<0.001 |
| Cardiac arrest, n (%) |
14 (12.3) |
2 (2.4) |
12 (38.7) |
0.001 |
1 (1.2) |
13 (38.2) |
0.001 |
2 (2.5) |
12 (34.3) |
<0.001 |
| SYNTAX score, mean (SD) |
20.2 ± 10.8 |
18.5 ± 9.7 |
24.5 ± 12.4 |
0.017 |
17.9 ± 8.8 |
25.3 ± 12.9 |
0.001 |
18.2 ± 9.4 |
24.2 ± 12.5 |
0.01 |
|
Table 2: Angiographic and PCI-related data in the study population either non-stratified or stratified in the higher and the aggregate lower/mid tertiles according to the SYNTAX score. Lesions include both treated and untreated lesions (≥50% stenosis). Chronic total occlusions (CTO) were not treated with PCI in the acute setting. “Patients and number of stents” refers to numbers of patients receiving different numbers of stents. “Stent type” refers to numbers of patients receiving either DES or BMS (in brackets, percentages of patients receiving a given stent type within the lower/mid or higher SYNTAX tertile groups). |
|
|
Total
N = 114
|
SX low + intermediate
N = 79
|
SX high
N = 35
|
p
|
|
Infarct localisation
|
|
|
|
|
| Anterior and antero-septal, n (%) |
44 |
31 (40) |
16 (43) |
0.12 |
| Inferior, n (%) |
39 |
26 (34) |
13 (35) |
0.69 |
| Posterior, n (%) |
9 |
5 (6) |
4 (11) |
0.15 |
| Lateral, n (%) |
19 |
15 (20) |
4 (11) |
0.46 |
|
1, 2 or 3 vessel disease
|
|
|
|
|
| 1 vessel, n (%) |
57 |
46 (59) |
11 (32) |
<0.001 |
| 2 vessels, n (%) |
34 |
25 (32) |
9 (26) |
<0.001 |
| 3 vessels, n (%) |
23 |
7 (9) |
15 (42) |
<0.001 |
| Chronic total occlusion (CTO), n (%) |
12 (10.5) |
5 (6.3) |
7 (20.0) |
0.12 |
|
Lesion localisation
|
|
|
|
|
| Left main, n (%) |
2 |
|
2 (3) |
0.35 |
| LAD, n (%) |
79 |
53 (45) |
26 (34) |
0.44 |
| RCX n, n (%) |
53 |
31 (27) |
22 (29) |
0.02 |
| RCA, n (%) |
59 |
33 (28) |
26 (34) |
<0.001 |
|
Patients and number of stents
|
|
|
|
|
| 0 stents, n (%) |
7 |
6 (8) |
1 (3) |
|
| 1 stent, n (%) |
69 |
50 (63) |
19 (54) |
|
| 2 stents, n (%) |
30 |
21 (27) |
9 (25) |
|
| 3 stents, n (%) |
5 |
2 (2) |
3 (9) |
|
| 4 stents, n (%) |
3 |
|
3 (9) |
|
| Mean (SD) |
1.4 ± 0.8 |
1.2 ± 0.6 |
1.7 ± 1.0 |
0.053 |
|
Stent type
|
|
|
|
|
| Bare metal stents, n (%) |
40 |
25 (34) |
15 (42) |
0.07 |
| Drug eluting stents, n (%) |
69 |
48 (66) |
21 (58) |
0.71 |
Results
Risk scores
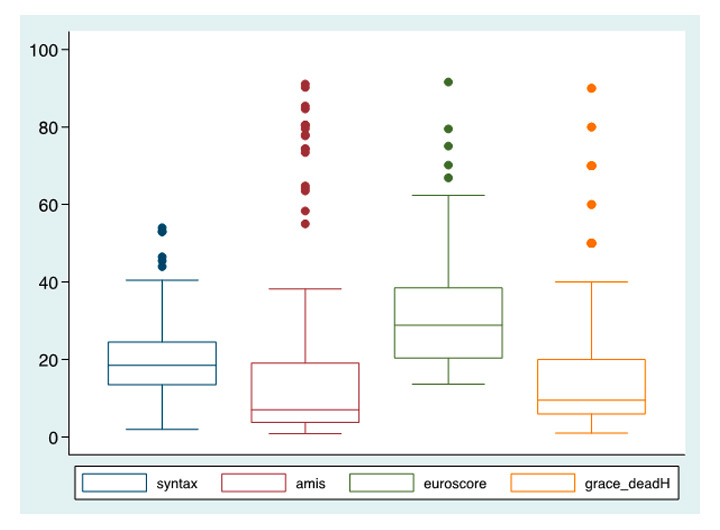
Clinical scores were calculated in a series of 114 consecutive patients aged ≥75 (mean age, 79.6 ± 4.1) who presented with ACS during 2007 and 2008, had no exclusion criteria, and were treated with PCI within 24 hours of hospital admission. No patient was lost during follow-up. Clinical characteristics of the study population as a whole or stratified according to each clinical score are shown in table 1. STEMI was diagnosed in 76.3% of patients. Cardiogenic shock and cardiac arrest were diagnosed in 16.7% and 12.3% of patients, respectively. The logistic EuroSCORE (mean ± SD) was 34.9 ± 17.9 in the overall population, 56.2 ± 14.0 in the higher tertile, and 24.5 ± 7.1 in the aggregate lower/mid tertiles. The GRACE score was 19.5 ± 22.4 in the overall population, 45.2 ± 23.8 in the higher tertile, and 7.3 ± 3.6 in the lower/mid tertiles. The AMIS score was 19.9 ± 26.9 in the overall population, 50.5 ± 27.8 in the higher tertile, and 4.5 ± 2.8 in the lower/mid tertiles. The SYNTAX score was 20.2 ± 10.8 in the overall population, 32.8 ± 9.1 in the higher tertile, and 14.7 ± 5.6 in the lower/mid tertiles. A boxplot showing the distribution of each score in the study population is shown in figure 1. Cardiogenic shock and cardiac arrest, but not STEMI, were significantly more frequent in the higher tertile compared to the lower/mid tertiles according to each score. Angiographic data and PCI-related variables are shown in table 2. Three-vessel disease was significantly more frequent in the higher tertile compared to lower/mid tertiles according to the SYNTAX score (p<0.01). In patients with CTO, the vessel treated with PCI was another vessel than the chronically occluded one. Agreement between any two scores was slight to fair on both the categorical and the continuous scale, with the exception of the AMIS and GRACE scores showing good agreement on both scales (table 5).
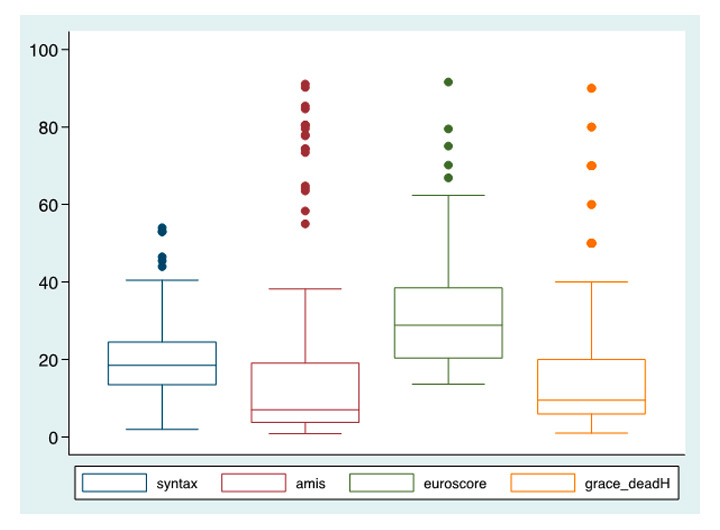
Figure 1
Boxplot showing the distribution of the log EuroSCORE, the GRACE score, the AMIS score, and the SYNTAX score in the study population; boxes represent the 25th and 75th percentile and midlines represent the median; whiskers represent the range excluding the extreme outliers (±3D), which are shown as dots.
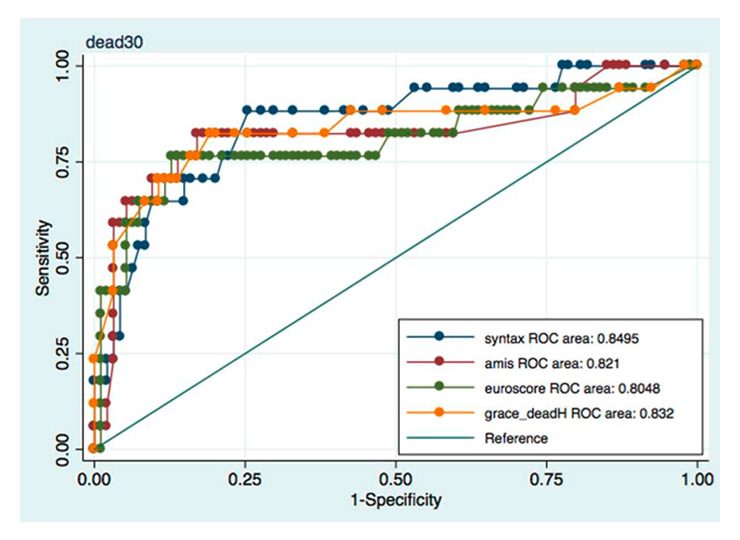
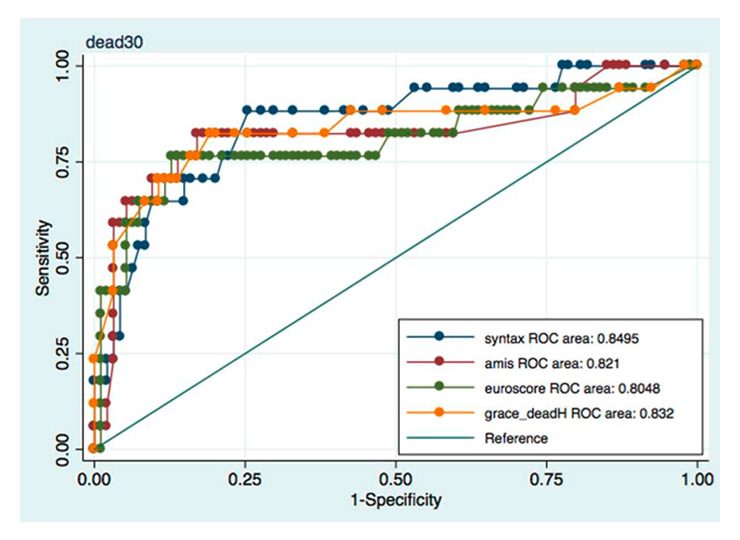
Figure 2
Sensitivity vs specificity curves for the logEuroSCORE, the GRACE score, the AMIS score, and the SYNTAX score with respect to the study’s primary end point (30-day mortality). ROC areas for all scores are indicated.
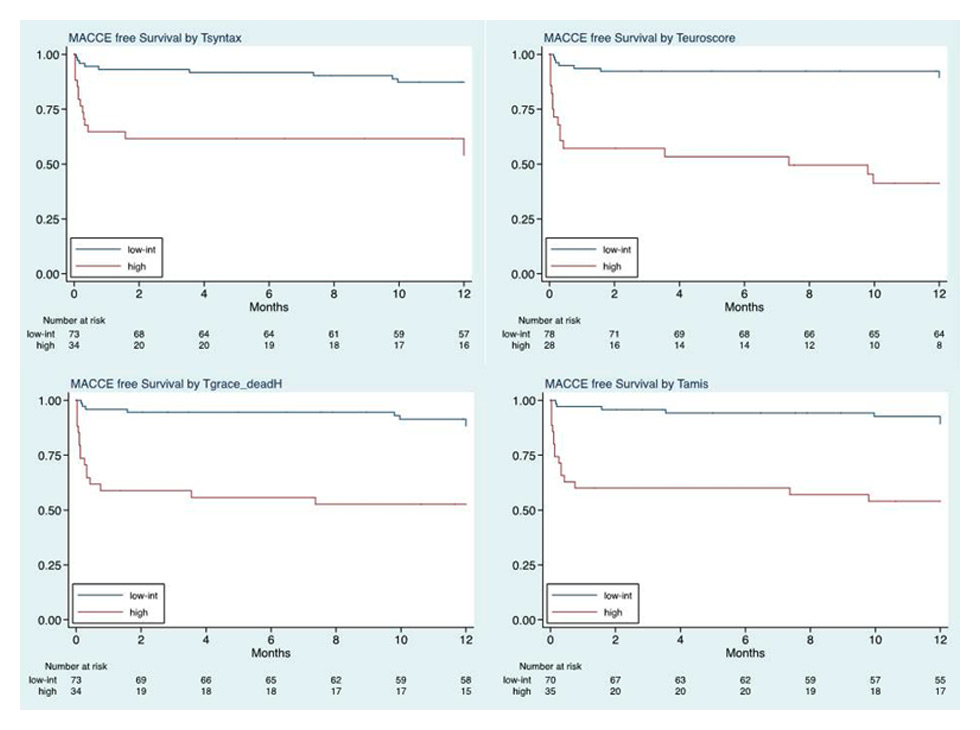
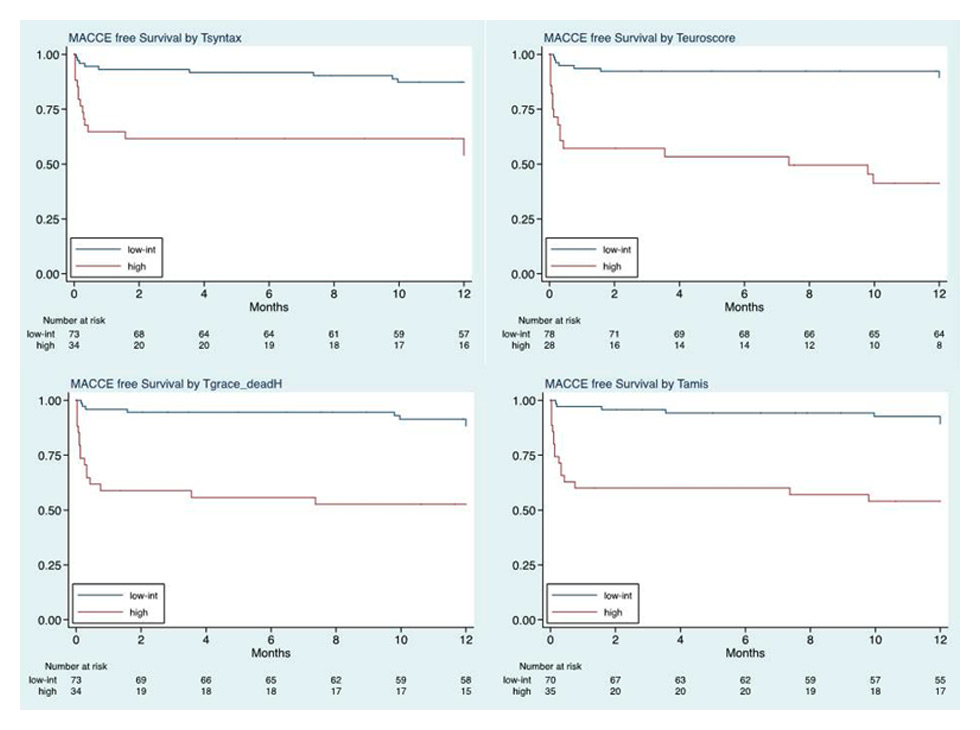
Figure 3
One-year MACE-free survival curves in patients stratified in the higher and lower/mid tertiles according to log EuroSCORE (upper right panel), the GRACE score (lower left panel), the AMIS score (lower right panel), and the SYNTAX score (upper left panel).
Risk scores and 30 day mortality
The study’s primary end point was mortality 30 days after baseline PCI. Results in patients stratified according to individual risk scores are shown in table 3. Seventeen patients (14.9%) died within 30 days of PCI (15 in hospital and 2 post-discharge). Thirty-day mortality was significantly higher (p <0.001) in the ”high risk” tertile compared with the lower/mid tertiles calculated with each score model. AUC-ROC values using patients’ categorisation based on score tertiles ranged from 0.77 for the SYNTAX score to 0.80 for the GRACE and AMIS scores. AUC-ROC values using scores measured on the continuous scale ranged from 0.80 for the Logistic EuroSCORE to 0.85 for the SYNTAX score (fig. 2).
Risk scores and MACE at 30 days
One of two secondary end points was rates of MACE (the composite of deaths and nonfatal MACE) 30 days after baseline PCI. Because only three patients had nonfatal MACE over this time frame, results for these secondary end points were similar to the primary end point: 30 day MACE were significantly more frequent (p<0.001) in the ”high-risk” tertile compared with the lower/mid tertiles according to each score tested. AUC ranged from 0.73 for the logistic EuroSCORE to 0.79 for the AMIS score (data not shown).
Risk scores and MACE at one year
Another secondary end point was rates of MACE one year after baseline PCI. Twenty-four patients experienced a MACE, including 20 deaths and 4 nonfatal MACE, during this time frame. MACE-free survival at one year in patients stratified according to the aggregate mid-lower tertiles vs the higher tertile of all scores, measured on the continuous scale, is shown in figure 3. Each score tested was able to stratify patients into two significantly different risk groups. In all cases, the predictive accuracy was good using both categorised scores and scores measured on the continuous scale (table 4).
Additional value of combining different scores
We hypothesised that combining different predictor variables would have additional value. Patients classified in the ”high-risk” group according to ≤2 scores were 88 (79%) and those classified in the ‘high-risk’ group according to 3 and 4 scores were 11 (10%) and 12 (11%), respectively. Thirty-day mortality was 3% in patients classified at ”high risk” according to ≤2 scoring systems compared to 45% and 75% in those classified at ”high risk” according to 3 and 4 scoring systems, respectively (OR for linear increase across categories = 9.93, 95% CI = 4.13–23.87; p<0.001; AUC = 0.88, 95% CI = 0.78–0.98). The combined score showed higher predictive accuracy than each clinical score, but not the SYNTAX score, as shown by AUC-ROC values with scores measured on a continuous scale (table 3; p <0.001 vs GRACE score; p = 0.007 vs logistic EuroSCORE; p <0.001 vs AMIS score; p = 0.18 vs the SYNTAX score).
|
Table 3: Mortality at 30 days in patients stratified in the higher and the aggregate lower/mid tertiles according to log EuroSCORE, the GRACE score, the AMIS score, and the SYNTAX score (missing data regarding the AMIS score in one patient; AUC area under the curve; CI: confidence interval; OR: odds ratio). AUC values are shown for scores both on a categorised and on a continuous scale. |
|
Mortality
|
Lower/mid tertiles
|
Higher tertile
|
OR
|
95% CI
|
p
|
AUC-ROC (95%CI)
|
AUC-ROC (95% CI) [continuous]*
|
|
Pts. n
|
Deaths n (%)
|
Pts. n
|
Deaths n (%)
|
|
|
|
|
|
| SYNTAXscore (n = 114) |
79 |
4 (5.1) |
35 |
13 (37.1) |
11.08 |
3.28–37.13 |
<0.001 |
0.77 (0.66–0.88) |
0.85 (0.74–0.95) |
| Logistic EuroSCORE (n = 113) |
82 |
4 (4.9) |
31 |
13 (41.9) |
14.08 |
4.11–48.29 |
<0.001 |
0.79 (0.68–0.90) |
0.80 (0.66–0.95) |
| GRACE score (n = 114) |
79 |
3 (3.8) |
35 |
14 (40.0) |
16.89 |
4.43–64.32 |
<0.001 |
0.80 (0.70–0.91) |
0.83 (0.69–0.97) |
| AMIS score (n = 112) |
77 |
3 (3.9) |
35 |
14 (40.0) |
16.44 |
4.31–62.66 |
<0.001 |
0.80 (0.70–0.90) |
0.82 (0.68–0.96) |
| * score expressed on a continuous scale |
|
Table 4: MACE rates at one year (follow-up started at the time of PCI) in patients stratified in the higher and the aggregate lower/mid tertiles according to log EuroSCORE, the GRACE score, the AMIS score, and the SYNTAX score (CI: confidence interval; HR: hazard ratio). Harrell’s c values are shown for scores both on a categorised and on a continuous scale (*). |
|
MACE
|
Low + intermediate
|
high
|
HR
|
95% CI
|
p
|
Harrell’s c (95% CI)
|
Harrell’s c (95% CI) [continuous]*
|
|
Total n
|
MACCE
n (%)
|
Total n
|
MACCE
n (%)
|
|
|
|
|
|
| SYNTAX score, n (%) |
73 |
9 (12.3) |
34 |
15 (44.1) |
4.65 |
2.03–10.65 |
<0.001 |
0.64 (0.57–0.77) |
0.74 (0.63–0.85) |
| Logistic EuroSCORE |
78 |
8 (10.3) |
28 |
16 (57.1) |
8.23 |
3.49–19.39 |
<0.001 |
0.76 (0.67–0.86) |
0.79 (0.68–0.90) |
| Grace Score |
73 |
8 (11.0) |
34 |
16 (47.1) |
5.85 |
2.49–13.71 |
<0.001 |
0.74 (0.65–0.83) |
0.81 (0.71–0.90) |
| AMIS score |
70 |
7 (10.0) |
35 |
16 (45.7) |
6.09 |
2.50–14.83 |
<0.001 |
0.75 (0.66–0.84) |
0.83 (0.75–0.92) |
| * score expressed on a continuous scale |
|
Table 5:Kappa Agreement and Lin’s concordance correlation coefficient (Rho-c) between clinical scores (log EuroSCORE, GRACE score, AMIS score) and the SYNTAX score. |
|
Syntax score (n = 114)
|
Log EuroSCORE (n = 113)
|
GRACE score (n = 114)
|
AMIS score (n = 112)
|
| Kappa (SE) |
0.14 (0.09) |
0.34 (0.09) |
0.22 (0.09) |
| Lin’s Rho-c (95% CI) |
0.18 (0.06–0.30) |
0.33 (0.20–0.45) |
0.24 (0.12–0.36) |
| AMIS score |
Log EuroSCORE |
GRACE score |
|
| Kappa (SE) |
0.46 (0.09) |
0.73 (0.09) |
– |
| Lin’s Rho-c (95% CI) |
0.50 (0.39–0.50) |
0.90 (0.86–0.93) |
– |
| Log EuroSCORE |
|
GRACE score |
|
| Kappa (SE) |
|
0.55 (0.09) |
– |
| Lin’s Rho-c (95% CI) |
|
0.52 (0.41–0.62) |
– |
Discussion
Various patient-based scoring algorithms have been validated for risk stratification in patients referred for cardiovascular interventions. While most of these algorithms are based on clinical variables, the anatomical SYNTAX score was validated recently in multiple clinical settings including STEMI. However, many validation studies have been carried out in all-age groups but not specifically in the elderly [27]. Several studies have demonstrated that elderly patients with ACS referred for PCI are at a higher risk compared to younger patients. The GRACE investigators showed that, among patients presenting with non-ST segment elevation ACS and referred for PCI or CABG, six month mortality increased with age (1.6%, 4.3%, and 7.0% in patients <70 years, 70–80 years, and >80 years, respectively) [32]. In 47,407 consecutive patients who underwent PCI and were prospectively enrolled in the PCI-Registry of the EHS Programme, in-hospital mortality was 1.7% in ACS patients <75 years compared to 5.2% in those ≥75 years [33]. Finally, data from the Zwolle Myocardial Infarction Study Group showed that, among 6,746 consecutive STEMI patients who had primary PCI between 1998 and 2008, 30 day mortality was 1.7% and 3.6% in men and women <65 years, respectively, compared to 6.4% and 9.6% in men and women ≥65 years, respectively [34].
Here, we evaluated three risk scores based on clinical parameters (the logistic EuroSCORE, the GRACE score and the AMIS score) and the angiographic SYNTAX score for risk stratification in the elderly presenting with ACS and treated with PCI within 24 hours of hospital admission. All four scoring systems predicted mortality at 30 days, the study’s primary end point, with fair-to-good discrimination (AUC values: 0.80 to 0.85 with scores on a continuous scale; 0.77 to 0.80 with scores categorised). An advantage of clinical scores over the anatomical SYNTAX score is that the former can be calculated ahead of coronary angiography.
There was limited statistical agreement between the different scores tested in the present study (supplemental table 1), implying limited overlap between risk categories defined by different score models. This observation raised the question as to whether being at a high risk according to multiple scores was associated with a higher actual risk compared to being at a high risk according to just one or two scores. Mortality at 30 days was 3% in patients who were in the higher tertile according to ≤2 scores, 45% in those who were in the higher tertile according to three scores, and 75% in those who were in the higher tertile according to four scores. The discrimination ability of the combined score model was excellent (AUC 88%) and significantly superior to that of each clinical score used individually; however, confirmatory studies in larger populations are needed.
All four scores accurately stratified MACE-free survival after 12 months of follow-up. Most events took place in the first month after PCI, however, indicating that elderly patients with ACS discharged alive after PCI had relatively good outcomes.
Direct comparisons of clinical scoring systems with the SYNTAX score in PCI patients are scarce. Garg et al. [35] reported a modest yet significant difference between the ACEF (Age, serum Creatinine, and Ejection Fraction) score, the SYNTAX score, and the clinical SYNTAX score (a combination of a modified ACEF score and the SYNTAX score) for prediction of 5 year mortality (C-statistics: 0.65, 0.62, and 0.69, respectively) and MACE (C-statistics: 0.57, 0.59, and 0.62, respectively) in patients presenting with complex coronary disease and stable or unstable angina or silent ischaemia, who were referred for PCI. Another study by the same group [24] showed a higher predictive value for the clinical PAMI (Primary Angioplasty in Myocardial Infarction) score compared with the SYNTAX score with respect to one year mortality (C statistics: 0.81 and 0.65, respectively) and MACE (C-statistics: 0.68 and 0.64, respectively) in STEMI patients treated by PCI. Palmerini et al. [36] compared the GRACE score, the New Risk Stratification score (NERS), the ACEF score, the Thrombolysis in Myocardial Infarction (TIMI) score, the SYNTAX score and the clinical SYNTAX score (CSS) in patients with non-ST elevation ACS. The NERS, the SYNTAX score and the CSS were the only scores showing both good discrimination and calibration for cardiac mortality at one year. Scores incorporating clinical and angiographic variables (CSS and NERS) showed the best trade-off between discrimination and calibration for most end points. Most recently, patient-level merged data from >6,000 patients in seven contemporary coronary stent trials was used to develop a logistic regression model, the Logistic Clinical SYNTAX score, to predict one year outcomes [37]. A core model (composed of the SYNTAX score, age, creatinine clearance, and LVEF) and an extended model (incorporating the core model and six additional, best performing clinical variables) were developed and validated. The core model demonstrated a substantial improvement in predictive ability for one year any cause death compared with the SYNTAX score alone (AUC: 0.753 vs 0.660). The core model alone therefore was retained in the final Logistic Clinical SYNTAX score model. Recently, a combination of anatomical and clinical factors in SYNTAX score II was shown to predict long-term ( four year) mortality in patients with complex CAD and to better guide decision making between CABG and PCI than the original anatomical SYNTAX score [38].
An important feature in the elderly which was not specifically addressed by the scoring systems used in the present study is frailty, as described by Fried and coworkers [39]. A recent study of 628 non-ACS patients ≥65 years not presenting with ACS and discharged after PCI showed a three year mortality of 28% for frail patients compared to 6% for non-frail patients [40]. After adjustment, frailty (HR, 4.19; 95% CI, 1.85–9.51) was associated with mortality.
It should be emphasised that the low sample size included represents a major limitation of our analysis, and therefore the prognostic values of different scores could not be assessed precisely. Nevertheless, the prognostic value of all scores tested was demonstrated at a statistically significant level. It also should be noted that the scores used in this study were originally developed for different purposes: the GRACE score for predicting six month mortality in patients discharged after an ACS episode [3], the euroSCORE for quality assessment of cardiac surgical care [8], the AMIS score for risk estimation of in-hospital mortality [13, 14], the SYNTAX as an angiographic tool grading the complexity of coronary lesions to predict prognosis and outcome at different time points [15, 16]. Finally, limitations of the SYNTAX score in patients with acute vessel occlusions were addressed previously [24, 25].
In conclusion, our data indicate that several clinical risk scores as well as the angiographic SYNTAX score predict mortality and MACE at 30 days in elderly patients presenting with ACS and referred for PCI within 24 hours of admission. Risk assessment can be improved by using multiple clinical scores in combination.
References
1 Fox KA, Clayton TC, Damman P, Pocock SJ, de Winter RJ, Tijssen JG, et al.; FIR Collaboration. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome: a meta-analysis of individual patient data. J Am Coll Cardiol. 2010;55(22):2435–45.
2 De Luca G, Suryapranata H, van ’t Hof AW, de Boer MJ, Hoorntje JC, Dambrink JH, et al. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: implications for early discharge. Circulation. 2004;109(22):2737–43.
3 Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, et al.; GRACE Investigators. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6–month postdischarge death in an international registry. JAMA. 2004;291(22):2727–33.
4 Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000;102(17):2031–7.
5 Addala S, Grines CL, Dixon SR, Stone GW, Boura JA, Ochoa AB, et al. Predicting mortality in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention (PAMI risk score). Am J Cardiol. 2004;93(5):629–32.
6 Halkin A, Singh M, Nikolsky E, Grines CL, Tcheng JE, Garcia E, et al. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. J Am Coll Cardiol. 2005;45(9):1397–405.
7 Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al.; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction); American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association of Cardiovascular and Pulmonary Rehabilitation; Society for Academic Emergency Medicine. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Am Coll Cardiol. 2007;50(7):e1–157.
8 Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R; EuroSCORE study group. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardio-thoracic Surg. 1999;16(1):9–13.
9 Sukiennik A, Ostrowska-Nowak J, Wiśniewska-Szmyt J, Radomski M, Rychter M, Jabłoński M, et al. Predicted and observed in-hospital mortality after left main coronary artery stenting in 204 patients. Cardiol J. 2008;15(3):268–76.
10 Rodés-Cabau J, Deblois J, Bertrand OF, Mohammadi S, Courtis J, Larose E, et al. Nonrandomized comparison of coronary artery bypass surgery and percutaneous coronary intervention for the treatment of unprotected left main coronary artery disease in octogenarians. Circulation. 2008;118(23):2374–81.
11 Min SY, Park DW, Yun SC, Kim YH, Lee JY, Kang SJ, et al. Major predictors of long-term clinical outcomes after coronary revascularization in patients with unprotected left main coronary disease: analysis from the MAIN-COMPARE study. Circ Cardiovasc Interv. 2010;3(2):127–33.
12 Lehmann R, Fichtlscherer S, Schächinger V, Held L, Hobler C, Baier G, et al. Favorable long-term survival in patients undergoing multivessel-PCI compared to predicted prognosis of CABG estimated by EuroSCORE: procedural and clinical determinants of long-term outcome. J Interv Cardiol. 2009;22(6):511–9.
13 Radovanovic D, Erne P. AMIS Plus: Swiss registry of acute coronary syndrome. Heart. 2010;96(12):917–21.
14 Kurz DJ, Bernstein A, Hunt K, Radovanovic D, Erne P, Siudak Z, Bertel O. Simple point-of-care risk stratification in acute coronary syndromes: the AMIS model. Heart. 2009;95(8):662–8.
15 Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. Eurointervention. 2005;1(2):219–27.
16 Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al.; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–72.
17 Valgimigli M, Serruys PW, Tsuchida K, Vaina S, Morel MA, van den Brand MJ, et al.; ARTS II. Cyphering the complexity of coronary artery disease using the syntax score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol. 2007;99(8):1072–81.
18 Serruys PW, Onuma Y, Garg S, et al. 5–Year clinical outcomes of the ARTS II (Arterial Revascularization Therapies Study II) of the sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. J Am Coll Cardiol. 2010;55(11):1093–101.
19 Capodanno D, Capranzano P, Di Salvo ME, Caggegi A, Tomasello D, Cincotta G, et al. Usefulness of SYNTAX score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. J Am Coll Cardiol Cardiovasc Intervent. 2009;2(8):731–8.
20 Chakravarty T, Buch MH, Naik H, White AJ, Doctor N, Schapira J, et al. Predictive accuracy of SYNTAX score for predicting long-term outcomes of unprotected left main coronary artery revascularization. Am J Cardiol. 2011;107(3):360–6.
21 Chen SL, Chen JP, Mintz G, Xu B, Kan J, Ye F, et al. Comparison between the NERS (New Risk Stratification) score and the SYNTAX (Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) score in outcome prediction for unprotected left main stenting.J Am Coll Cardiol Cardiovasc Intervent. 2010;3(6):632–41.
22 Kim YH, Park DW, Kim WJ, Lee JY, Yun SC, Kang SJ, et al. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) score for prediction of outcomes after unprotected left main coronary revascularization. J Am Coll Cardiol Cardiovasc Intervent. 2010;3(6):612–23.
23 Wykrzykowska J, Garg S, Girasis C, de Vries T, Morel MA, van Es GA, et al. Value of the Syntax Score (SX) for risk assessment in the “Allcomers” Population of the Randomized Multicenter Leaders Trial. J Am Coll Cardiol. 2010;56(4):272–7.
24 Garg S, Sarno G, Serruys PW, Rodriguez AE, Bolognese L, Anselmi M, et al.; STRATEGY and MULTISTRATEGY Investigators. Prediction of 1–year clinical outcomes using the SYNTAX score in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a substudy of the STRATEGY (Single High-Dose Bolus Tirofiban and Sirolimus-Eluting Stent Versus Abciximab and Bare-Metal Stent in Acute Myocardial Infarction) and MULTISTRATEGY (Multicenter Evaluation of Single High-Dose Bolus Tirofiban Versus Abciximab With Sirolimus-Eluting Stent or Bare-Metal Stent in Acute Myocardial Infarction Study) trials.J Am Coll Cardiol Cardiovasc Intervent. 2011;4(1):66–75.
25 Magro M, Nauta S, Simsek C, Onuma Y, Garg S, van der Heide E, et al. Value of the SYNTAX score in patients treated by primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: The MI SYNTAXscore study. Am Heart J. 2011;161(4):771–81.
26 Palmerini T, Genereux P, Caixeta A, Cristea E, Lansky A, Mehran R, et al. Prognostic value of the SYNTAX score in patients with acute coronary syndromes undergoing percutaneous coronary intervention: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage StrategY) trial. J Am Coll Cardiol. 2011;57(24):2389–97.
27 Vrints CJ. Acute coronary syndrome in the elderly. Eur Heart J. 2008;29(10):1213–4.
28 Scherff F, Vassalli G, Sürder D, Mantovani A, Corbacelli C, Pasotti E, et al. The SYNTAX score predicts early mortality risk in the elderly with acute coronary syndrome having primary PCI. J Interv Cardiol. 2011;23(12):505–10.
29 Task Force for Diagnosis and Treatment of Non-ST-Segment Elevation Acute Coronary Syndromes of European Society of Cardiology, Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernández-Avilés F, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. The Task Force for the Diagnosis and Treatment of Non-ST-Segment Elevation Acute Coronary Syndromes of the European Society of Cardiology. Eur Heart J. 2007;28(13):1598–660.
30 Van de Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KA, et al.; Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2003;24(1):28–66.
31 Müller C: New ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Swiss Med Wkly. 2012;142:w13514.
32 Devlin G, Gore JM, Elliott J, Wijesinghe N, Eagle KA, Avezum A, et al.; GRACE Investigators. Management and 6–month outcomes in elderly and very elderly patients with high-risk non-ST elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Eur Heart J. 2008;29(10):1275–82.
33 Bauer T, Möllmann H, Weidinger F, Zeymer U, Seabra-Gomes R, Eberli F, et al. Predictors of hospital mortality in the elderly undergoing percutaneous coronary intervention for acute coronary syndromes and stable angina. Int J Cardiol. 2011;151(2):164–9.
34 Otten AM, Maas AH, Ottervanger JP, Kloosterman A, van ’t Hof AW, Dambrink JH, et al.; Zwolle Myocardial Infarction study Group. Is the difference in outcome between men and women treated by primary percutaneous coronary intervention age dependent? Gender difference in STEMI stratified on age. Eur Heart J Acute Cardiovasc Care. 2013;2(4):334–41.
35 Garg S, Sarno G, Garcia-Garcia HM, Girasis C, Wykrzykowska J, Dawkins KD, Serruys PW; ARTS-II Investigators. A new tool for the risk stratification of patients with complex coronary artery disease. The Clinical SYNTAX Score. Circ Cardiovasc Interv. 2010;3(4):317–26.
36 Palmerini T, Caixeta A, Genereux P, Cristea E, Lansky A, Mehran R, et al. Comparison of clinical and angiographic prognostic risk scores in patients with acute coronary syndromes: Analysis from the Acute Catheterization and Urgent Intervention Triage StrategY (ACUITY) trial. Am Heart J. 2012;163(3):383–91,391.e1–5.
37 Farooq V, Vergouwe Y, Räber L, Vranckx P, Garcia-Garcia H, Diletti R, et al. Combined anatomical and clinical factors for the long-term risk stratification of patients undergoing percutaneous coronary intervention: the Logistic Clinical SYNTAX score. Eur Heart J. 2012;33(24):3098–104.
38 Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381(9867):639–50.
39 Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156.
40 Singh M, Rihal CS, Lennon RJ, Spertus JA, Nair KS, Roger VL. Influence of frailty and health status on outcomes in patients with coronary disease undergoing percutaneous revascularization. Circ Cardiovasc Qual Outcomes. 2011; 4(5):496–502.