
Figure 1
Estimated number of subjects with a specific disorders of the brain in Switzerland in 2010 based on data from the 2011 European Brain Council (EBC) study.
DOI: https://doi.org/10.4414/smw.2013.13751
According to the Review of Health Systems from the Organisation for economic co-operation and development (OECD) a high performance and responsiveness has been attributed to Switzerland due to a high availability of health services, an unconstrained choice of health care providers, a high patient satisfaction and one of the longest life expectancies of the world. However, this also has its price. In 2009 Switzerland spent 11.4% of its gross national product on health which is more than 2% above the OECD average [1]. In 2005, findings of the first “cost of disorders of the brain in Europe” study of the European Brain Council (EBC) [2] showed that the group of disorders of the brain comprising mental, neurological and substance use disorders contributed to about 16% of the health care costs in Switzerland [3]. Nearly half of it refers to indirect costs while 33% concern direct health care expenses and 19% direct non-medical costs. When findings on total costs from all 25 countries of the European Union plus Iceland, Norway and Switzerland were cumulated, 386 billion EUR were spent in 2005 for the assessed brain disorders. With expenses of 9 billion EUR for its health system, Switzerland had spent most per capita [2]. The largest part of it was spent for “mood disorders” (formerly called “affective disorders”).
Although findings from the 2005 EBC study improved the political recognition of the size and burden of disorders of the brain on different European and national political levels, incomplete age ranges and diagnostic scopes needed an update of the data collection in 2010 including a broader range of mental disorders and neurological conditions across the whole life-span [4]. Whereas the 2005 studies collected data on specific substance use disorders, psychotic, mood and anxiety disorders as well as brain tumors, dementia, epilepsy, headache, multiple sclerosis, Parkinson’s disease, stroke and traumatic brain injury, the new studies additionally included data on child and adolescent disorders, eating disorders, mental retardation, neuromuscular disorders, sleep disorders, somatoform disorders and two additional personality disorders. These additional brain disorders together with those already included in 2005 were thought to have the highest impact on public health and health economy in European countries.
After inclusion of data assessed in 2010, the total European costs of disorders of the brain were estimated at about EUR 798 billion with the largest expenses for mood disorders [5]. Disregarding the newly included disorders and extensions of them in 2010 resulted in EUR 477 billion total costs compared to EUR 386 billion in the 2005 EBC studies. The difference could be explained by simply inflating the cost and population size during the 5 years period. While EUR 164 billion were allocated to extensions of the 2005 disorders (e.g. specific disregarded disorders were added to the already reviewed groups as for example posttraumatic stress disorder to anxiety disorders) the new disorders were estimated at EUR 157 billion total costs [5]. The aim of the present paper is to provide the specific Swiss data from the EBC 2010 study and to discuss them in relation to those of other European countries and the former study in Switzerland in 2005 [2].
The European study was commissioned by the EBC. The EBC is a co-ordinating council formed by European organisations in psychiatry, neurology, neurosurgery, basic neuroscience, and the European patient organisations in psychiatry and neurology as well as representatives of the brain-related pharmaceutical industry. The council was designed and managed by a steering committee that included professors Olesen (Denmark), Wittchen (Germany) and Jönsson (Sweden). The major task of the EBC is to analyse the size and burden of brain disorders in Europe and to make recommendations for politics, research, teaching and public awareness. For the “size and cost of disorders of the brain in Europe-study”, the committee collaborated with the health economists Gustavsson and Svensson as well as members of expert panels related to the investigated disorders1 (see also acknowledgement).
The study follows a societal perspective considering the costs of all resources that were used or lost due to a disorder or disease. These costs included the direct health care costs (i.e., prevention, diagnostic processes and treatment for example in a hospital or by physicians visits), the direct non-medical costs (e.g., social services or caregiving, informal care) and the indirect costs (e.g., through work absence or early retirement). Pharmaceutical expenditures were included in direct costs and estimated through use of the ATC code allowing the identification of drug classes used to treat disorders of the brain. Based on this system, statistics on pharmaceutical sales are available from which costs of drugs related to brain disorders can be derived. The total costs were calculated by using epidemiological data on the prevalence of a disorder under the consideration of economic data stemming from cost of illness studies and national or regional statistics.
Prevalence estimates were generated through expert reviews of already existing findings from general population studies or other sources. Similarly cost data were drawn from literature reviews on already existing economic data. The methodology of the study has been presented in detail elsewhere [4, 5]. The specific steps of this approach that included also reanalyses of epidemiological data will be described in more detail below.
The current study extracts the relevant data from the EBC 2010 study [4, 5] and presents the data for Switzerland in detailed fashion.
The stepwise multi-method study approach of EBC 2010 [4] included first a literature search and review of eligible existing epidemiological data from the general population of the participating countries on the agreed diagnostic spectrum that was performed by expert panels1. Included studies were required to have used a population-based approach, explicit diagnostic information based on either research criteria of ICD-10 (WHO, 1993) or diagnostic criteria of DSM-III-R/DSM-IV (APA, 1994) and an assessment with well-established diagnostic instruments. Prevalence estimates that were drawn from the literature ideally referred to the preceding 12 months and were drawn from studies that were conducted between 1980 and 2010. In addition to international reviews on prevalence findings as for example from Tagliaferri et al. on brain injury epidemiology in Europe [6], that are all available in [5], the following prevalence data from original Swiss studies were included: dementia [7] and child and adolescent disorders [8];
In case original country data from the literature were not suitable the second step included re-analyses of data of accessible epidemiological, nationwide, general population studies as well as re-analyses of data from community studies from the participating countries to fill in gaps of estimates of prevalence and other necessary information (e.g., on comorbidity). If country specific data still missed after these procedures data from other countries were extrapolated to the countries with missing data in a third step. National expert surveys served as an independent validation component of reviewed data or for use of additional “best estimates” on prevalence data in cases data were not available by the first two steps.
For the aggregation of prevalence estimates of diagnostic findings across all EU member states median percentages and interquartile range (IQR) was most often reported. For several diagnoses, the epidemiological panels derived “best estimates” by judgement taking into account the median and range of available estimates. This was the case whenever the median appeared to be heavily biased by methodological factors as for example in case of outlier prevalence due to a limited sample from a certain age group although there is evidence for varying age-specific prevalence estimates. In this instance, panel experts choose the “best estimate” from a reference study. Furthermore, disorder-specific variations between countries (e.g., for alcohol dependence) and the occurrence in specific age groups were taken into account (e.g., for child and adolescent disorders). The last one was considered by calibrating the age specific prevalence reflecting the total population. To avoid double counting specific disorders were adjusted for comorbidity. This was for example done for personality disorders which were assumed to be most likely already counted with another mental disorder. Therefore personality disorders were excluded from overall prevalence estimates. Data for Switzerland were attained by all four aforementioned methods.
An approach consisting of “bottom-up”-cost-illness studies assessing individual costs was chosen to identify country-specific costs of disorders in the EBC 2010 study. It was supplemented by the “top-down”-approach that used statistical national or regional information of groups of disorders for the identification of the specific costs of a certain disorder [5]. Data were primarily drawn from literature analyses of eligible studies conducted in the participating countries. Included were studies that were published from January 1st 2004 on and that investigated the specific diagnoses among patients in the participating countries with a robust methodology. The following original studies contributed to Suisse cost data in the EBC 2010 study: brain tumours [9], epilepsy [10], multiple sclerosis [11] and stroke [12].
Data were entered in a “European cost of illness (COI)”-model that estimated total costs by using the estimated prevalence of the disorders under consideration [5]. The model also considers missing country-specific cost data by extrapolations from other countries. Furthermore variations of cost estimates related to the year of the assessment and the specific currency on which the data were based were considered:
(1) All data on cost estimates were adjusted to 2010 values considering country-specific inflation rates.
(2) All data on cost estimates were converted to real Euro (EUR) with nominal exchange rates from the European Central Bank.
(3) In case of unavailable eligible costs, estimate extrapolation across countries by use of an adjusted median for income, health care expenditure, and wage level differences was performed.
(4) Prevalence estimates were then used to calculate population fractions with the specific brain disorders by multiplying the estimated prevalence ratios with the number of people in each country in 2010 taking into account disorder-specific age ranges and missing costs data for the total population. The numbers of persons with each disorder (the population fractions) were then multiplied with the estimated costs per patient in each country. Specific methods that have been used for missing data are described in [5].
For the current study, relevant data for Switzerland were again gained from all four sources. The currency utilised for computation were EUR adjusted by the purchasing power parity (PPP) that determines the relative value of the specific currencies of each participating country for the EBC 2010 database being in EUR, for the ease of comparability across all involved countries.
Figure 1 shows the estimated numbers of affected subjects by the combined categories of mental disorders and some specific brain disorders.

Figure 1
Estimated number of subjects with a specific disorders of the brain in Switzerland in 2010 based on data from the 2011 European Brain Council (EBC) study.
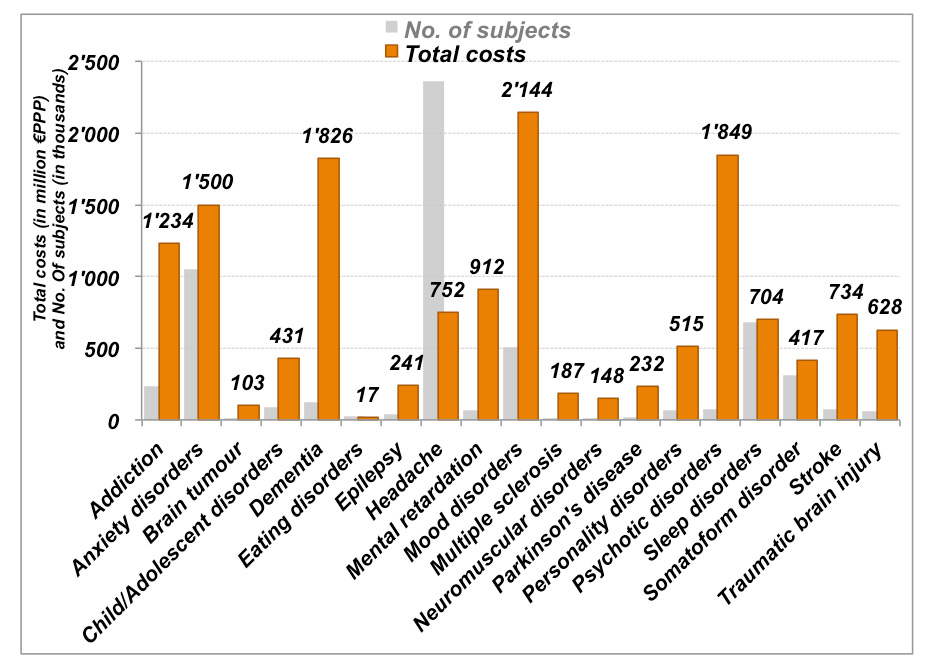
Figure 2
Total costs of specific disorders of the brain in Switzerland.
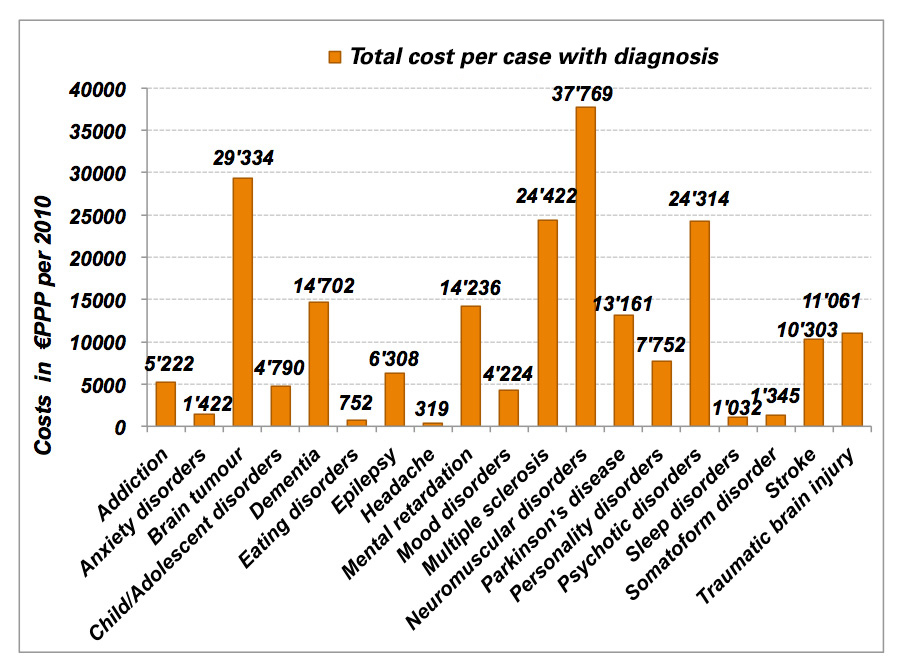
Figure 3
Total costs per affected subject in Switzerland.
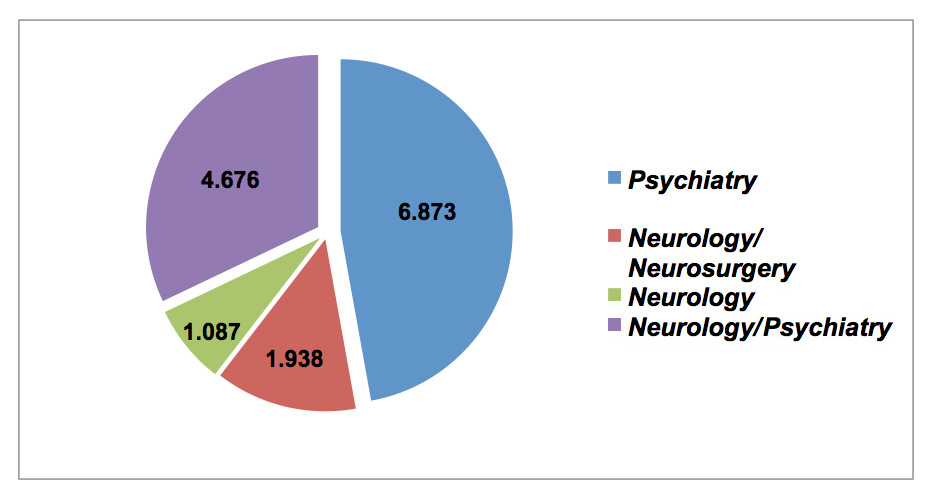
Figure 4
Total costs per discipline (million €PPP, 2010).
Additionally data on the specific disorders within these combined categories are shown in Appendix 1. The numbers of cases per 2010 are based on “best estimates” of the prevalence of the disorders and it is important to note again that for some specific disorders only cases of subpopulations of the relevant age groups are reported. This is true, for example, for child and adolescents disorders, which only encompassed the age range of 0 to 17 years, or dementia, which included only cases of 64 years and older.
Figure 1 reveals that headache with a clear majority of tension-type headache accounted for nearly half of the cases with brain disorders (see Appendix 1). Anxiety disorders with more than one million cases and a majority of specific phobias followed on in the second place. Interestingly, the newly added category of sleep disorders, which included insomnia for a major part (Appendix 1: 444 of the 683 cases), was the third most frequent disorder and was nearly three times more prevalent than addiction. In contrast, neuromuscular disorders, brain tumors, and multiple sclerosis were relatively rare.
Based on the “European COI”-model the total costs of brain disorders were specifically calculated for Switzerland with the reported numbers of subjects as shown above and the reviewed specific costs of disorders. In Switzerland the total costs of all brain disorders under consideration were estimated at 14 Billion and 574 Million EUR (nearly 20 Billion CHF in 2010). Figure 2 displays the total costs by groups of disorders and some specific disorders (orange columns). In addition, the numbers of subjects are represented by grey columns.
With more than 2 Billion Euro expenses in 2010, mood disorders were the most costly group of brain disorders followed by psychotic disorders. Given the relatively low number of cases with psychosis as compared to those with mood disorders, the high total cost of psychosis was probably attributable to the high functional impairment related to this disorder that even doubles the high cost of inpatient treatment. Regarding headache, the 752 Million Euros spent for this condition lie in the mid range of costs despite its high prevalence. In contrast, several disorders with low prevalence caused high total costs. One of them was mental retardation that cost nearly one billion Euros. Another example was stroke, which lies in the mid range of prevalence estimates, but caused costs comparable to those of sleep disorders with a much higher prevalence.
The societal perspective as considered here distinguished between direct health care costs that include all medical costs, direct non-medical costs, including for example costs for social services, and indirect costs encompassing periods of inability to work and early retirement. Table 1 shows how these costs were distributed with respect to the disorders.
Direct health care costs were with 5 Billion and 726 Million EUR the highest burden of brain disorder as shown in the last row of table 1. However nearly the same amount were lost earnings for brain disorders due to inability to work or early retirement, whereas direct non-medical healthcare costs added up to an amount that was lower: 3.2 Billion EUR. It is noteworthy that anxiety disorders required most direct healthcare resources in terms of cost. On the other hand, dementia accounted for nearly half of the total of direct-non medical costs. Moreover, indirect costs were particularly high for mood and for psychotic disorders with one third of all indirect costs being attributable to these two disorders. Similarly, headache, personality disorders and to a lower degree neuromuscular disorders mostly caused indirect costs, whereas stroke for example entailed high direct health care costs and only moderate non-medical and indirect costs. Given the restricted age range, no indirect costs were estimated for dementia and child or adolescent disorders. The other missing values in table 1 were due to lack of information from cost data reviews.
The estimation of costs per subject is also important for the allocation of financial resources although the validity of the data of the ECB 2010 was limited due to the possibility of double counting. Even though this bias has been minimized by considering the excess costs of each disorder, this limitation should be acknowledged when costs per subjects are reported. In total, subjects with brain disorders or diseases were estimated to cost 2.624 EUR in 2010. Figure 3 compares the cost per subject by groups of disorders or by specific disorders.
In contrast to the total costs, the costs per case were particularly high among relatively rare brain disorders. Neuromuscular disorders caused the highest costs per case partially due to their severe consequences, whereas ‘headache’ the most common brain disorder, or anxiety disorder, the most prevalent mental disorders, caused relatively low costs per case. Among mental disorders, psychotic- and personality disorders were most expensive when evaluated per subject. Again, all data were adjusted for disorder-specific comorbidity patterns.
Table 2 shows that most direct health care costs per subject were spent for the treatment of brain tumours followed by neuromuscular disorders. As shown in Appendix 1, Guillan-Barré syndrome (GBS) in particular caused very high direct health care costs per subject within the neuromuscular disorder category. In contrast, direct health care costs per subject of dementia were moderate; but the direct non-medical costs per subject were higher than those for all other disorders. Both neuromuscular disorders and psychotic disorders caused particularly high indirect costs per subject. With respect to personality disorders, the relatively high costs per case as compared to the other mental disorders were essentially due to borderline personality disorder (Appendix 1). The costs per subject of the other mental disorders were in the moderate to lower range.
We also aimed to divide the total costs by discipline. Psychiatry includes the following disorders: psychotic, personality, child/adolescent, mood, anxiety, somatoform and eating disorders were assigned to Psychiatry. Neurology alone was decided to include: neuromuscular disorders, multiple sclerosis, headache. A mixed neurology/neurosurgery category was defined to consist of brain tumours, Parkinson’s disease, traumatic brain injury, stroke and epilepsy. A mixed neurology/psychiatry category included dementia, mental retardation, addiction (alcohol use disorders and opioid dependence), and sleep disorders. Note that clinical psychology or neuropsychology contribute to all these medical disciplines to a greater or lesser extent.
Figure 4 shows that 6.9 billion EUR total costs were allocated to Psychiatric care. If neurological costs were combined with psychiatric and neurosurgery costs they summarize to 7.7 billion EUR with 1.087 Billion EUR allocated to core neurological diseases.
| Table 1: Total costs of direct healthcare-, non-medical- and indirect costs. | ||||
| Costs (million €PPP, 2010) | ||||
| Collapsed groups of brain disorders/ specific disorders | Total costs | Direct healthcare costs | Direct non-medical costs | Indirect costs |
| Addiction | 1.234 | 490 | 287 | 457 |
| Anxiety disorders | 1.500 | 987 | 2 | 511 |
| Brain tumour | 103 | 68 | * | 35 |
| Child/Adolescent disorders | 431 | 55 | 376 | n.a. |
| Dementia | 1.826 | 355 | 1.471 | n.a. |
| Eating disorders | 17 | 13 | 1 | 3 |
| Epilepsy | 241 | 148 | 25 | 68 |
| Headache | 752 | 182 | 570 | |
| Mental retardation | 912 | 628 | 284 | * |
| Mood disorders | 2.144 | 557 | 307 | 1.280 |
| Multiple sclerosis | 187 | 54 | 71 | 62 |
| Neuromuscular disorders | 148 | 39 | 29 | 80 |
| Parkinson’s disease | 232 | 109 | 96 | 27 |
| Personality disorders | 515 | 72 | 54 | 389 |
| Psychotic disorders | 1.849 | 622 | * | 1.227 |
| Sleep disorders | 704 | 419 | 285 | |
| Somatoform disorder | 417 | 205 | * | 212 |
| Stroke | 734 | 510 | 172 | 52 |
| Traumatic brain injury | 628 | 213 | 66 | 349 |
| Total | 14.574 | 5.726 | 3.241 | 5.607 |
| * = unavailable; n.a. = not applicable due to restricted age range | ||||
| Table 2: Direct healthcare, non-medical and indirect costs annually per subject. | ||||
| Costs per subjects (€PPP, 2010) | ||||
| Collapsed groups of brain disorders/ specific disorders | Total costs | Direct healthcare costs | Direct non-medical costs | Indirect costs |
| Addiction | 5.222 | 2.073 | 1.216 | 1.933 |
| Anxiety disorders | 1.422 | 936 | 2 | 485 |
| Brain tumour | 29.334 | 19.295 | * | 10.039 |
| Child/Adolescent disorders | 4.790 | 609 | 4.181 | n.a. |
| Dementia | 14.702 | 2.858 | 11.844 | n.a. |
| Eating disorders | 752 | 559 | 62 | 131 |
| Epilepsy | 6.308 | 3.879 | 645 | 1.785 |
| Headache | 319 | 77 | 242 | |
| Mental retardation | 14.236 | 9.808 | 4.428 | * |
| Mood disorders | 4.224 | 1.098 | 605 | 2.521 |
| Multiple sclerosis | 24.422 | 7.073 | 9.258 | 8.090 |
| Neuromuscular disorders | 37.769 | 9.913 | 7.348 | 20.508 |
| Parkinson’s disease | 13.161 | 6.172 | 5.446 | 1.543 |
| Personality disorders | 7.752 | 1.082 | 818 | 5.852 |
| Psychotic disorders | 24.314 | 8.174 | * | 16.140 |
| Sleep disorders | 1.032 | 614 | * | 418 |
| Somatoform disorder | 1.345 | 662 | * | 683 |
| Stroke | 10.303 | 7.161 | 2.417 | 725 |
| Traumatic brain injury | 11.061 | 3.745 | 1.164 | 6.152 |
| Total | 2.624 | 988 | 559 | 1.076 |
| * = unavailable; n.a. = not applicable due to restricted age range | ||||
The new data on the size and burden of brain diseases or disorders from the EBC 2010 studies have provided an update of the 2005 assessment of disorders of the brain in the European Union, Iceland, Norway and Switzerland. The inclusion of a broader set of diagnoses than in the first study in 2005 has led to a two times higher estimate of the costs of brain disorders in 2010. With respect to Switzerland, the total cost of nearly 9 Billion EUR in 2005 rose to 14.5 Billion EUR in 2010, which is a slightly smaller increase compared to that of other countries. The specific findings and limitations as well as the implications will be discussed in the following sections.
Between 2005 and 2010 the estimated number of diagnoses of disorders of the brain in Switzerland increased remarkably [3]. A significant part of the increase resulted from the inclusion of the tension type headache that had not been assessed in 2005. Together with the two other new types of headache it accounted for 1.5 Million cases. Another million cases were attributable to disorders that were newly included in the 2010 assessment. These new disorders included sleep disorders, somatoform disorders and child and adolescent disorders. However, compared to the assessment in 2005 there was also an increase within the anxiety disorders category (about 300’000 more cases), mood disorders and addiction (each about 100’000 subjects more), and psychotic disorders (40 000 more cases). A part of some of the increase within categories relied on the extension in the EBC 2010 coverage of disorders, e.g., post-traumatic stress disorder was recently included in the anxiety disorders category and opioid dependence has been only recently added [4]. Therefore the real increase of affected individuals was much lower than suggested by the overall difference of affected subjects between the two assessments which is in line with findings from other participating EBC countries that partially found few differences between the two assessments when regarding the former disorder categories [4].
With respect to the relatively small remaining increase of affected individuals (about 700.000 persons) in Switzerland that might be not attributable to the extensions the specific Swiss data from more recent studies, new country specific reports or updated “best estimates” for Switzerland that regarded for example the country-specific increase of older age cohorts may have been responsible. Furthermore an overall population increase has been notified from the Switzerland and other European countries between 2005 and 2010,
On the other hand there is an ongoing debate on other causes. In clinical studies it could be attributable to lower barriers for individuals with mental disorders to seek professional help. Alternatively, increased proneness of subjects to report psychiatric symptoms or a real cohort effect as for example an increase of cases in younger cohorts as for example with respect to substance use disorders could explain elevated prevalence estimates of mental disorders in more recent studies [13]. In contrast the increasing prevalence of dementia is expected given the aging of the population in developed countries [14] and the 25% risk for dementia of all causes in individuals aged 90 years and older [15].
The costs of disorders of the brain raised from EUR 8.9 Billion in 2005 to EUR 14.5 Billion in 2010. These higher costs were mostly attributable to the increase of subjects and diagnoses, respectively, included into the 2010 report. Similarly to the 2005 assessment, the largest part of the total costs in Switzerland was allocated to care for mood disorders [3]. Dementia costs increased from 320 Million by a factor of 5.5 to 1.8 Billion. Swiss data from 2007 [16] reported even higher costs of 3.5 billion (without indirect cost), but these differences may be explained by different calculations for institutional care costs. For substance use disorders the overall costs remained unchanged despite an increase of the prevalence of these disorders since 2005.
However, there were also some significant reductions of costs of some disorders. For instance, epilepsy costs decreased from 370 million to 240 million, while Multiple sclerosis costs decreased from 290 to 190 million. These developments are difficult to explain. Compared with the 2005 data, direct non-medical costs decreased for both epilepsy and multiple sclerosis. Moreover, there was a strong decrease of indirect costs for epilepsy, raising the possibility that improved treatment options and altered patterns of care were largely responsible for the overall decrease in cost.
In the neurology/neurosurgery area the total costs for stroke increased by a factor of 2.5 fold to 730 Million EUR. This increase is in line with high costs reported in the United Kingdom for this category [17, 18]. It might reflect increased use of new treatment options such as thrombolytic therapy and more extensive neurorehabilitation which, however, should result in a stronger decrease in indirect cost than has been reported so far. But even more, the new data on traumatic brain injury also revealed a steep increase from 67 to 628 Million EUR. In 2005 cost data for this category lacked direct non-medical costs as well as indirect costs and were estimated to a three times lower amount for direct health care costs [3]. This latter difference may be due to different uses in disease registration; registration for TBI or subarachnoid haemorrhage is currently only in the process of its nationwide establishment [18, 19].
When comparing the Swiss total costs to the European partners of the EBC study as has been done by Gustavsson et al. [5], Switzerland lies between Portugal (13.130 €PPP million) and Austria (15.996 €PPP million) which corresponds to much lower expenditures as compared to the leading partner Germany with 152,719 €PPP million. However, more meaningful to compare but also limited to model estimations and different wage levels are the costs per capita which show that Switzerland is in 2010 in the 7th position right behind Germany among the 30 partners with about 1.900 EUR per capita (European mean, 1.550 EUR).
Although the present paper was based on information from a variety of Swiss or international studies as well as the judgment of experts in the field, the results need to be considered in the context of several limitations:
First, data on prevalence estimates from epidemiological studies were not available for all disorders in all participating countries including Switzerland. This limitation was minimized by using different methods to include other data on prevalence e.g., from national reports or by assuming a European median prevalence which was used for extrapolation of data across countries. Moreover there were only few complete original cost-data available for Switzerland which made it necessary to use data from other countries for cost extrapolation after adaptation to the income, expenditure or wage level of Switzerland.
Second, most cost data were based on clinical samples that were not representative for the overall patient population of disorders under consideration. The risk of an overestimation of costs by using mostly treated subjects was reduced by the introduction of severity categories.
Third, double counting of subjects affected by more than one disorder could have entailed an overestimation of aggregated costs although cost estimates were based on excess costs of the specific disorders.
Fourth, the estimates of the size and costs of disorders of the brain did not include the whole range of disorders of the brain which resulted in cost estimates that were rather conservative. For example, nicotine dependence was not included. In addition, not all costs for specific disorders were available.
Despite the above-mentioned limitations, this update to the EBC studies currently presents the best possible estimate of the size and burden of disorders of the brain in Switzerland. The total costs of these disorders that were assessed in 2010 correspond to nearly 10% of the costs of the Suisse health system if only the direct health care costs are taken. This significantly exceeds the estimations of the 2005 EBC data for Switzerland [3] and, thus, highlights the clinical and society burden of disorders of the brain which must be taken into account by decision makers in health services and finance departments. Only cardiovascular diseases, which occupy the second position in terms of cost, cause a comparable burden of disease [20].
Very few data exist on the other disorder groups in Switzerland for the last 5 years besides the already in [3] mentioned obesity, asthma and severe sepsis. Particular cost estimations were recently published on Swiss data on acute coronary syndrome [21], psoriasis [22], low back pain [21] and major surgical procedures [23]. Again, in accordance with WHO data on the burden of diseases in high and middle income countries, the costs of disorders of the brain far outweigh the costs of other disease-groups like cancer and metabolic diseases.
The enormous size and burden of disorders of the brain in Switzerland emphasizes the major need of increased efforts in research fields of psychiatry, neurology, and neurosurgery as well as of neuropsychology and epidemiology. This should be considered as a priority for the national health and research budget. Switzerland, like other highly developed countries in the world, should focus its research on causes and risks of diseases with the ultimate goal of improving prevention. If national policy has recently reinforced the role of primary care medicine, this effort has to be balanced out with appropriate means to also strengthen the role of medical and psychological specialities. Although some of the most prevalent disorders of the brain, such as mood or sleep disorders, headache and dementia also play a significant role in primary care, the progress in treating these and more cost-intensive conditions will depend on scientific progress in the concerned specialities.
Structurally, being one of the smaller European countries, Switzerland has the chance to develop new models of integrated research cooperation that include governmental bodies, private health-care and pharmaceutical companies. This would be a promising approach, especially in the areas of the highly complex disorders of the brain. Finally, as already outlined in [3] with respect to the 2005 data, the Swiss society needs a permanent effort to monitor and analyse the size and burden of these disorders through continuous studies in order to improve the allocation of health services in the future.
| Appendix 1 | |||||||||
| Disorders/diseases | Number of subjects (in thousands) | Cost per subject (in €PPP per 2010) | Total cost (in million €PPP per 2010) | ||||||
| Direct healthcare cost | Direct non-medical cost | Indirect cost | Total cost | Direct healthcare cost | Direct non-medical cost | Indirect cost | Total cost | ||
| Addiction | 236 | 2.073 | 1.216 | 1.933 | 5.222 | 490 | 287 | 457 | 1.234 |
| – Alcohol | 221 | 1.904 | 1.285 | 2.055 | 5.244 | 422 | 284 | 455 | 1.161 |
| – Opioids | 15 | 4.582 | 187 | 116 | 4.886 | 68 | 3 | 2 | 73 |
| Anxiety disorders | 1.054 | 936 | 2 | 485 | 1.422 | 987 | 2 | 511 | 1.499 |
| – Agoraphobia | 134 | 471 | 911 | 1.382 | 63 | 122 | 185 | ||
| – GAD | 135 | 1.378 | 273 | 1.652 | 185 | 37 | 222 | ||
| – OCD | 44 | 775 | 270 | 1.045 | 34 | 12 | 46 | ||
| – Panic disorder | 120 | 1.179 | 792 | 1.971 | 142 | 95 | 237 | ||
| – PTSD | 117 | 1.488 | 18 | 1.506 | 174 | 2 | 177 | ||
| – Social phobia | 154 | 1.018 | 570 | 1.588 | 157 | 88 | 244 | ||
| – Specific phobia | 350 | 659 | 449 | 1.108 | 231 | 157 | 388 | ||
| Brain tumour | 4 | 19.295 | 10.039 | 29.334 | 68 | 35 | 103 | ||
| Child/Adolescent disorders | 90 | 609 | 4.181 | 4.790 | 55 | 376 | 430 | ||
| – ADHD | 50 | 656 | 393 | 1.048 | 32 | 19 | 52 | ||
| – Autism | 8 | 1.799 | 35.168 | 36.967 | 15 | 291 | 306 | ||
| – Conduct Disorder | 32 | 228 | 2.026 | 2.255 | 7 | 65 | 72 | ||
| Dementia | 124 | 2.858 | 11.844 | 14.702 | 355 | 1.471 | 1.826 | ||
| Eating disorders | 23 | 559 | 62 | 131 | 752 | 12,8 | 1,4 | 3,0 | 17,2 |
| – Anorexia | 13 | 992 | 104 | 223 | 1.319 | 12,6 | 1,3 | 2,8 | 16,7 |
| – Bulimia | 10 | 22 | 10 | 17 | 49 | 0,2 | 0,1 | 0,2 | 0,5 |
| Epilepsy | 38 | 3.879 | 645 | 1.785 | 6.308 | 148 | 25 | 68 | 241 |
| Headache | 2.360 | 77 | 242 | 319 | 182 | 570 | 752 | ||
| – Migraine | 767 | 114 | 324 | 438 | 87 | 248 | 336 | ||
| – Medicine overuse | 107 | 420 | 2.396 | 2.817 | 45 | 257 | 302 | ||
| – Other headaches | 166 | 45 | 28 | 73 | 7 | 5 | 12 | ||
| – Tension type | 1.319 | 32 | 45 | 77 | 42 | 60 | 102 | ||
| Mental retardation | 64 | 9.808 | 4.428 | 14.236 | 628 | 284 | 912 | ||
| Mood disorders | 508 | 1.098 | 605 | 2.521 | 4.224 | 557 | 307 | 1.280 | 2.144 |
| – Bipolar disorder | 46 | 870 | 733 | 7.125 | 8.727 | 40 | 34 | 328 | 402 |
| – Major depression | 462 | 1.121 | 593 | 2.062 | 3.775 | 517 | 274 | 952 | 1.743 |
| Multiple sclerosis | 8 | 7.073 | 9.258 | 8.090 | 24.422 | 54 | 71 | 62 | 187 |
| Neuromuscular disorders | 3,9 | 9.913 | 7.348 | 20.508 | 37.769 | 38,6 | 28,6 | 79,9 | 147,1 |
| – ALS | 0,8 | 15.611 | 15.056 | 5.537 | 36.204 | 12,5 | 12,1 | 4,4 | 29,1 |
| – CIDP | 0,2 | 21.538 | 3.578 | 4.461 | 29.577 | 4,7 | 0,8 | 1,0 | 6,4 |
| – GBS | 0,1 | 71.863 | 2.789 | 74.651 | 7,2 | 0,0 | 0,3 | 7,5 | |
| – MMN | 0,0 | 21.538 | 3.578 | 4.461 | 29.577 | 0,8 | 0,1 | 0,2 | 1,2 |
| – Muscular dystrophies | 2,0 | 1.833 | 7.226 | 35.831 | 44.890 | 3,7 | 14,7 | 72,8 | 91,2 |
| – Myasthenia gravis | 0,6 | 12.672 | 1.014 | 1.319 | 15.006 | 7,9 | 0,6 | 0,8 | 9,3 |
| – PDN | 0,1 | 21.538 | 3.578 | 4.461 | 29.577 | 1,7 | 0,3 | 0,3 | 2,3 |
| Parkinson's disease | 18 | 6.172 | 5.446 | 1.543 | 13.161 | 109 | 96 | 27 | 232 |
| Personality disorders | 66 | 1.082 | 818 | 5.852 | 7.752 | 72 | 54 | 389 | 515 |
| – Antisocial | 31 | 784 | 3.249 | 4.033 | 24 | 100 | 124 | ||
| – Borderline | 36 | 1.337 | 1.519 | 8.083 | 10.939 | 48 | 54 | 289 | 392 |
| Psychotic disorders | 76 | 8.174 | 16.140 | 24.314 | 622 | 1.227 | 1.849 | ||
| Sleep disorders | 683 | 614 | 418 | 1.032 | 419 | 285 | 705 | ||
| – Hypersomnia | 48 | 1.142 | 549 | 1.691 | 54 | 26 | 80 | ||
| – Insomnia | 444 | 213 | 213 | 95 | 95 | ||||
| – Narcolepsy | 1 | 2.577 | 4.541 | 7.117 | 4 | 6 | 10 | ||
| – Sleep apnea | 190 | 1.404 | 1.331 | 2.734 | 267 | 253 | 520 | ||
| Somatoform disorder | 311 | 662 | 683 | 1.345 | 205 | 212 | 418 | ||
| Stroke | 71 | 7.161 | 2.417 | 725 | 10.303 | 510 | 172 | 52 | 733 |
| Traumatic brain injury | 57 | 3.745 | 1.164 | 6.152 | 11.061 | 213 | 66 | 349 | 628 |
| Total | 5.793 | 988 | 559 | 1.076 | 2.624 | 5.724 | 3.241 | 6.234 | 15.199 |
| 1 = Alcohol use disorders and opioid dependence | |||||||||
1 OECD-World Health Organization. OECD reviews of health systems – Switzerland: OECD Publishing; 2011.
2 Andlin-Sobocki P, Jonsson B, Wittchen H-U, Olesen J. Cost of disorders of the brain in Europe. Eur J Neurol. 2005;12:1–27.
3 Jäger M, Sobocki P, Rössler W. Cost of disorders of the brain in Switzerland with a focus on mental disorders. Swiss Med Wkly. 2008;138(1):4–11.
4 Wittchen H-U, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–79.
5 Gustavsson A, Svensson M, Jacobi F, Allgulander C, Alonso J, Beghi E, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–79.
6 Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J. A systematic review of brain injury epidemiology in Europe. Acta Neurochir. 2006;148(3):255–68.
7 Gostynski M, Ajdacic-Gross V, Gutzwiller F, Michel JP, Herrmann F. Prevalence of dementia in the City of Zurich. Soz Praventivmed. 2002;47(5):330–5.
8 Steinhausen HC, Metzke CW, Meier M, Kannenberg R. Prevalence of child and adolescent psychiatric disorders: The Zurich Epidemiological Study. Acta Psychiatr Scand. 1998;98(4):262–71.
9 Wasserfallen JB, Ostermann S, Leyvraz S, Stupp R. Cost of temozolomide therapy and global care for recurrent malignant gliomas followed until death. Neuro Oncol. 2005;7(2):189–95.
10 Gessner U, Sagmeister M, Horisberger B. The cost of epilepsy in Switzerland. Int J Health Sci. 1993;4:121–8.
11 Kobelt G, Berg J, Lindgren P, Gerfin A, Lutz J. Costs and quality of life of multiple sclerosis in Switzerland. Eur J Health Econ. 2006;7:86–95.
12 Mahler MP, Zuger K, Kaspar K, Haefeli A, Jenni W, Leniger T, et al. A cost analysis of the first year after stroke – early triage and inpatient rehabilitation may reduce long term costs. Swiss Med Wkly. 2008;138:459–65.
13 Horwitz AV, Wakefiled JC. The loss of sadness. How psychiatry transformed normal sorrow into depressive disorder. Oxford: Oxford University Press; 2007.
14 Kalaria RN, Maestre GE, Arizaga R, Friedland RP, Galasko D, Hall K, et al. Alzheimer’s disease and vascular dementia in developing countries: Prevalence, management, and risk factors. The Lancet Neurology. 2008;7(9):812–26.
15 Corrada MM, Brookmeyer R, Paganini-Hill A, Berlau D, Kawas CH. Dementia incidence continues to increase with age in the oldest old: the 90+ study. Ann Neurol. 2010;67(1):114–21.
16 Kraft E, Marti M, Werner S, Sommer H. Cost of dementia in Switzerland. Swiss Med Wkly. 2010;140.
17 Rivero-Arias O, Gray A, Wolstenholme J. Burden of disease and costs of aneurysmal subarachnoid haemorrhage (aSAH) in the United Kingdom. Cost Eff Resour Alloc. 2010;8:6.
18 Rivero-Arias O, Wolstenholme J, Gray A, Molyneux AJ, Kerr RS, Yarnold JA, et al. The costs and prognostic characteristics of ischaemic neurological deficit due to subarachnoid haemorrhage in the United Kingdom. Evidence from the MRC International Subarachnoid Aneurysm Trial. J Neurol. 2009;256:367–73.
19 Schatlo B, Fung C, Fathi A-R, Sailer M, Winkler K, Daniel RT, et al. Introducing a nationwide registry: the Swiss study on aneurysmal subarachnoid haemorrhage (Swiss SOS). Acta Neurochir. 2012.
20 Mathers C, Fat DM, Boerma JT. The global burden of disease: 2004 update. Geneva: World Health Organisation; 2008.
21 Wieser S, Horisberger B, Schmidhauser S, Eisenring C, Brügger U, Ruckstuhl A, et al. Cost of low back pain in Switzerland in 2005. Eur J Health Econ. 2011;12(5):455–67.
22 Navarini AA, Laffitte E, Conrad C, Piffaretti P, Brock E, Ruckdaeschel S, et al. Estimation of cost-of-illness in patients with psoriasis in Switzerland. Swiss Med Wkly. 2010;140(5):85–91.
23 Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Müller MK, Hahnloser D, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254(6):907–13.
“Cost of Disorders of the Brain in Europe” Study Group: Members from Switzerland were Roselind Lieb, Hans-Christoph Steinhausen, Martin Preisig, and Andreas Maercker.
Acknowledgement: Besides the EBC steering committee from the European Brain Council (http://www.europeanbraincouncil.org/) consisting of Jes Olesen (Danish Headache Centre, Department of Neurology, Glostrup University Hospital, Denmark), Hans-Ulrich Wittchen (Institute of Clinical Psychology and Psychotherapy, Dresden, Germany) and Bengt Jönsson (Stockholm School of Economics, Sweden) in collaboration with lead health economists Anders Gustavsson (Optuminsight, Stockholm, Sweden) and Mikael Svensson (Department of Economics and Statistics, Karlstad University, Sweden) enormous and unpaid efforts of epidemiological and economic experts who have worked voluntarily for the 2010 Cost of disorders of the brain study of the EBC should be acknowledged : Stefanie Drabsch (University of Florence, Italy), Manfred Döpfner (University of Cologne, Germany), Simon Forstmeier (University of Zürich, Switzerland), Andrea Gabilondo (Generalitat de Catalunya, Barcelona, Spain), Andrew Gloster (Technische Universität Dresden, Germany), David Hilton-Jones (University of Oxford, United Kinfdom), Michael Höfler (Technische Universität Dresden, Germany), Corinna Jacobi (Technische Universität Dresden, Germany), Danica Klempova (EMCDDA, Lisbon, Portugal), Rafael Martinez Leal (University of Granada, Spain), Gunther Meinlschmidt (University of Basel, Switzerland), Jayadeep Patra (Centre for Addiction and Mental Health, Toronto, Canada), Rafael Martínez-Leal, Jose García-Ibáñez, and Francisco Aguilera (Fundació Villablanca Reus), Peter van den Bergh (The Université catholique de Louvain, Belgium), Julian Vicente (EMCDDA, Lisbon, Portugal), Frank Verhulst (Erasmus Medical Center– Sophia Children’s Hospital, Rotterdam, Netherlands), Johannes Wancata (Universitätsklinik für Psychiatrie, Vienna). Julien Mendlewicz (Hospital Erasme ULB, Department of Psychiatry, Brussels), Hristo Hinkov (Department of Global Mental Health, National Centre for Public Health Protection, Sofia), Ioanna Katsounari (The Chicago School Of Professional Psychology, Chicago), Cyril Höschl (Prague Psychiatric Center, Prague); Denmark: Povl Munk-Jörgensen (Aalborg Psychiatric Hospital, Aalborg), Eduard Maron (University of Tartu, Tartu), Erkki Isometsä (Institute of Clinical Medicine, Helsinki), Jean-Pierre Lèpine (Hôpital FernandWidal, Paris), Petros Skapinakis (School of Medicine, Ioannina), Zoltan Rihmer (National Institute for Psychiatry and Neurology, Budapest), Jon G. Stefánsson (Landspitalinn-University Hospital, Reykjavík), Donna Tedstone Doherty (Health Research Board, Dublin), Elmārs Rancāns (Latvian Academy of Medicine, Riga), Gintautas Daubaras (Mental Health Center, Vilnius), Arunas Germanavicius (Vilnius University, Vilnius), Ron de Graaf (Trimbos-Instituut, Utrecht), Kari Ann Leiknes (University of Oslo, Oslo), Bogdan Ioan Voinescu (University of Medicine and Pharmacy, Cluj-Napoca), Alexandra Brazinova (International Neurotrauma Research Organisation, Vienna), Mojca Dernovsek (Educational and Research Institute Ozara, Ljubljana), Jordi Alonso (Institut Municipal d'Investigació Mèdica, Barcelona), Rafael Martínez-Leal, Jose García-Ibáñez, and Francisco Aguilera (Fundació Villablanca Reus), Martin Preisig (University of Lausanne, Prilly-Lausanne), and Traolach Brugha (Leicester General Hospital).
Funding / potential competing interests: Information about the sponsoring organization, the European Brain Council, is available at its Web site http://www.europeanbraincouncil.org