DOI: https://doi.org/10.4414/smw.2013.13725
Tick related diseases seem to be frequent and widespread in Switzerland [1–4]. The most frequent disease is Lyme borreliosis with an estimated 6,000 to 12,000 cases every year in a population of actually about 8 million [5, 6]. Lyme borreliosis is a bacterial disease caused by Borrelia burgdorferisensu lato infections. The following organ systems are involved: skin, musculoskeletal system including joints, peripheral and central nervous system and heart [7, 8]. Asymptomatic infections are frequent and elevated seroprevalences are observed in forestry workers [9] and orienteers [10, 11]. Seroprevalence in blood donors levels around 10% [12]. Lyme borreliosis can be treated by antibiotics and completely cured in most cases. It affects both sexes of all age groups, and is widespread all over Switzerland [5, 13]. The second most common tick borne disease is tick borne encephalitis with about 100 to 250 cases every year [14, 15]. It is caused by a flavivirus. The clinical picture varies from asymptomatic infections to influenza like symptoms to severe neurological disorders or even death. No specific treatment is available. Its geographic distribution is confined to localised endemic areas. The disease is preventable by vaccination [14–16]. Other tick borne diseases such as rickettsiosis, babesiosis or anaplasmosis seem to be rare in Switzerland [1]. Further investigations would be required to elucidate the burden of these infrequent tick-borne infections.
Since 1984, positive laboratory tests for acute tick borne encephalitis have to be notified to the Federal Office of Public Health (FOPH) and the cantonal physician by law. The treating physicians are asked to fill in a specific notification form which has to be sent to the cantonal physician and then forwarded to the FOPH. Both laboratory and physician report forms are registered in a FOPH-hosted central database.
Since 2008, tick bites and Lyme borreliosis are surveyed in a voluntary surveillance system called Sentinella. Sentinella is a national network of about 150 primary care physicians. These physicians report weekly numbers of their consultations and a set of observations, which is defined yearly by a programme committee. All patient data are collected in an anonymous way. Tick bites are reported weekly by a separate reporting form which includes data on age, sex, exposure to ticks and tick borne encephalitis vaccination status. A notification is only done if the tick bite is a reason for the consultation. Lyme borreliosis is notified by a specific reporting form which includes data on tick bite history, clinical picture, laboratory confirmation and antibiotic treatment. A case report is sent if an antibiotic treatment for Lyme borreliosis is initiated.
The present paper is an update on the epidemiology of tick bites and Lyme borreliosis in primary care [13], as well as of tick borne encephalitis [16] in Switzerland during the reporting period of 2008 to 2011. The estimation methods have been improved compared to previous publications [13]. The main objective is to describe the incidence and its determinants (e.g., year, age, sex and residency) of tick bites, Lyme borreliosis and tick borne encephalitis.
The mandatory surveillance database of tick borne encephalitis links laboratory and clinical information. The link is done by initials, date of birth, sex and residency. The physician’s report form includes data on tick bite exposure, reason for laboratory testing, clinical picture, immunisation status, hospitalisation and death.
The Sentinella database of tick bites and Lyme borreliosis is completely anonymous. Data available are age, sex, region of residency (see definition of Sentinella Regions below). For Lyme borreliosis clinical and laboratory information is included and is reported by the physician.
Population data are made available by the Federal Office of Statistics (FOS). The latest data set is available up to 2010. For the estimates the population of 2011 was assumed to be equal to that of 2010.
All cases of tick borne encephalitis, tick bite and Lyme borreliosis reported between week 1 of 2008 to week 52 of 2011 were eligible for the analysis. Tick borne encephalitis cases were included according to defined criteria (appendix). The term “no case” designates the excluded cases from the analysis, because there was only laboratory evidence (increased IgM-Titer only) without clinical symptoms. Therefore the immunological reaction could not be attributed to either disease, vaccination or cross-reaction (e.g. yellow fever, dengue, Hepatitis C). Cases of Lyme borreliosis or tick bites were only included in the analysis if they were reported by regularly reporting physicians. Only confirmed cases of Lyme borreliosis were included into the analysis in accordance with the EUCALB definitions [17].
All analyses were based on cross table calculations, and estimation of rates and proportions. Inference was done by estimating Poisson regressions with an offset of the natural logarithm of the surveyed population. The modelled outcomes were ‘observed numbers of consultations for tick bite’, ‘cases of Lyme borreliosis’ and ‘tick borne encephalitis’. Factors evaluated were year of occurrence, sex, age classes and Sentinella Region. Models were estimated including one factor only as well as a multivariate model which included all factors assuming independence. 95% confidence limits were calculated where adequate.
Age classes were defined according to the standard of the FOS with few adaptations (0 to 5 years, 6 to 19 years, 20 to 39 years, 40 to 64 years, 65 to 79 years, equal or over 80 years). An adaptation was made for the age class ‘0 to 5 years’ because vaccination is not recommended for this group. Cantons were grouped into the 6 Sentinella Regions for the purpose of comparability between tick bites, Lyme borreliosis and tick borne encephalitis: Region 1 includes Geneva (GE), Neuchâtel (NE), Vaud (VD) and Valais (VS). Region 2 includes Berne (BE), Fribourg (FR) and Jura (JU); Region 3 includes Aargau (AG), Basel (BS/BL), and Solothurn (SO); Region 4 includes Lucerne (LU), Obwalden (OW), Nidwalden (NW), Schwyz (SZ), Uri (UR) and Zug (ZG); Region 5 includes Appenzell (AI/AR), Glarus (GL), St. Gallen (SG), Schaffhausen (SH), Thurgau (TG), Zurich (ZH) and the Principality of Lichtenstein (FL); Region 6 includes Grisons (GR) and Ticino (TI) (fig. 1). The time resolution is the week defined by ISO 8601.
All computations were performed by STATA/SE 12.0 and R Statistics Version 2.11.1 for Windows on personal computers with MICROSOFT Windows 7 as the operating system. Data management was done by means of a MICROSOFT SQL-Server. Maps were built by Grass Gis 6.4.1 and R Statistics Version 2.11.1 for Windows. The shape files were provided by the FOS.
To calculate the total case numbers of tick bites and Lyme borreliosis in Switzerland, we estimated the population covered by the Sentinel network (Sentinella). This population is estimated on the basis of the annual number of Sentinella physician-patient contacts (source: Sentinella system), the number of all physician consultations in Switzerland (source: data pool of Santésuisse, the Swiss association of health insurance providers), and on population data (source: FOS).
The physicians of the Sentinella Network weekly report the number of physician-patient contacts. The weekly physician-patient contact numbers (“Sentinella consultations”) do not include data on age and sex. However twice a year, during two weeks, the network reports detailed patient contacts which include age, sex and region. The regional age-sex distribution from these “2x2 weeks” datasets is extrapolated to the total numbers of Sentinella consultations for each year in order to perform age, sex and region specific analyses. The Santésuisse data pool includes physician-patient contact numbers (“consultations CH”) pooled for age, sex and region. The population under Sentinella surveillance is estimated as follows:
In order to obtain the incidence of tick bites and Lyme borreliosis, the observed number of these events is divided by the population covered by Sentinella. The estimated case numbers are calculated by multiplying the incidence by the Swiss population. The incidences (tick bites, Lyme borreliosis) are rounded to 3 significant digits. Observed case numbers of borreliosis and tick borne encephalitis are specified in full precision (table 2, 3, 4).
Since surveillance of infectious diseases is based on the law of epidemics, the FOPH is obliged to publish aggregated results on a weekly basis, and there are no ethical restrictions.
All cases of tick borne encephalitis (N = 562), tick bites (N = 1,664) and Lyme borreliosis (N = 1,113) reported between week 1 of 2008 to week 52 of 2011 were eligible for the analysis. Some cases of tick borne encephalitis (N = 55) were excluded from the analysis, because they did not fulfil the case definition. Only confirmed cases of Lyme borreliosis were included into the analysis (N = 864 out of 1,113), because only confirmed cases comply with the EUCALB definitions [17].
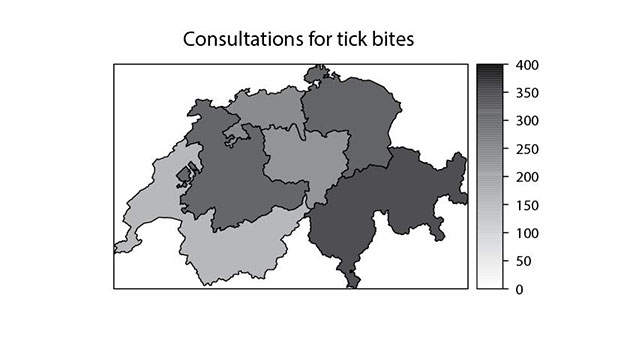
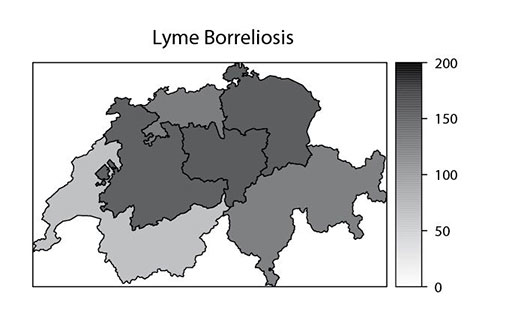
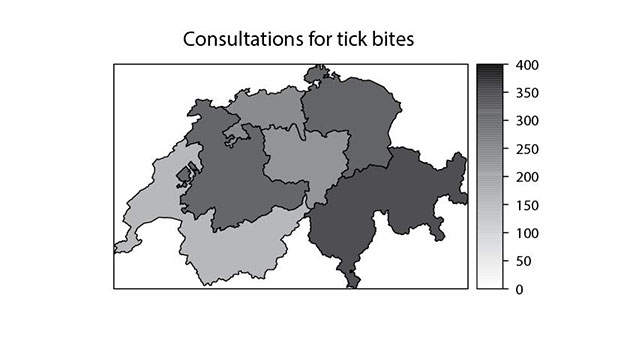
Figure 1
Geographic distribution by Sentinella Regions regarding treated tick bites, Lyme borreliosis and tick borne encephalitis, Switzerland 2008 to 2011. Panel 1: Treated tick bites, yearly incidence per 100,000 inhabitants, 2008–2011. Panel 2: Lyme borreliosis, yearly incidence per 100,000 inhabitants, 2008–2011. Panel 3: Tick borne encephalitis, yearly incidence per 100,000 inhabitants, 2008–2011
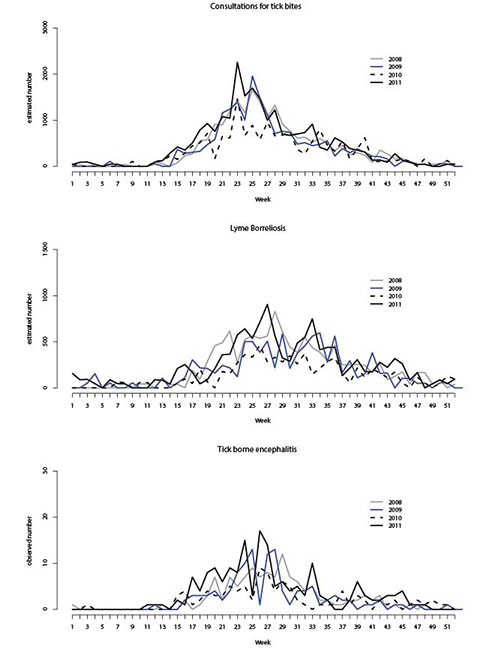
Figure 2
Seasonal time trends of treated tick bites, Lyme borreliosis (both estimated numbers of cases) and tick borne encephalitis (observed number of cases), Switzerland, 2008 to 2011. The week of the year is defined according to ISO 8601. The estimated numbers of consultations for tick bites or Lyme borreliosis, respectively, are represented in Panel 1 and 2. Panel 3 represents the seasonal trend in tick borne encephalitis cases.
A tick bite is a frequent reason to see a primary care physician in Switzerland (yearly incidence 254 per 100,000 inhabitants, 95% confidence limits 244 to 269 per 100,000 inhabitants), followed by Lyme borreliosis (yearly incidence 131 per 100,000, 95% confidence limits 124 to 142 per 100,000 inhabitants) and tick borne encephalitis (yearly incidence 1.6 per 100’000 inhabitants). The estimated incidences and estimated respectively observed case numbers for tick bites, Lyme borreliosis and tick borne encephalitis changed in parallel during 2008 and 2011 (table 1, fig. 2). From 2008 to 2010 the incidences and total numbers decreased. The trend reversed in 2011 (table 1). When comparing 2008 with 2011, the levels increased by 5% for tick bites (2008: estimated N = 22,000; 2011: estimated N = 23,000), 0% for Lyme borreliosis (2008: estimated N = 12,000; 2011: estimated N = 12,000), and 41% for tick borne encephalitis (2008: observed N = 122; 2011: observed N = 172). In 2011, the observed number of tick borne encephalitis cases was 70 times smaller than the estimated number of Lyme borreliosis cases, and about 100 times smaller than the estimated number of tick bites reported by general practitioners. The lowest number of cases was reported in 2010 (tick bites: estimated N = 17,000, Lyme borreliosis: estimated N = 7,000, tick borne encephalitis: observed N = 98).
Men were more often affected by tick borne encephalitis than women (yearly incidence was 2.2 versus 1.1/100,000), whereas in Lyme borreliosis, the two sexes were equally affected (yearly incidence was 126 versus 136/100,000) (table 1). However, the trend of this proportion is changing over time. Lyme borreliosis mainly affects patients aged 6 to 19 years and 40 to 79 years. A similar age distribution was observed for tick-bites. Incidence rates of tick bites (yearly incidence across Sentinella Regions: range 152 to 338 per 100,000 inhabitants) and Lyme borreliosis (yearly incidence across Sentinella Regions: range 67 to 158 per 100,000 inhabitants) were high all over Switzerland (fig. 1). The age class of 40 to 79 year olds, being male and living in Region 4 or 5 (the north-east of Switzerland, table 1, fig. 1) was correlated with a high risk of being affected by tick borne encephalitis. Although tick bites, Lyme borreliosis and tick borne encephalitis may occur during the whole year, events such as these mostly occurred during summer (fig. 2).
About 74% of patients with tick borne encephalitis and about 52% of Lyme borreliosis patients remembered a tick bite prior to disease manifestation (analysing only the data sets with this information available; table 2, 3). However, the proportion of data sets which lack the history of tick bites is considerable. About 90% of patients were exposed to ticks during leisure. Professional exposure is rarely reported, although the seroprevalence in the different risk groups is known to be high [9]. Patients suffering from tick bite or Lyme borreliosis were vaccinated against tick borne encephalitis in about 30% of all cases.
About 79% of tick borne encephalitis patients were hospitalised (analysing only the data sets with this information available; table 3). About 1% died from tick borne encephalitis. In about 50 to 60% of all cases, the first manifestation of tick borne encephalitis was an influenza-like syndrome; Meningitis was the clinical picture in 19% and meningoencephalitis in 59%. Neurological symptoms were absent in about 9% of the cases. In about 85 to 90% of the cases, the clinical suspicion led to the diagnostic tests. Mentioning an exposure to ticks was the reason in about 20% of the cases. The diagnosis was based on increased IgM and IgG levels in serum in about 68%, followed by increased IgM levels in blood in about 21% and increased IgM levels in cerebrospinal fluid in about 3% of all cases.
The predominant sign of Lyme borreliosis was Erythema migrans accounting for 90% of cases, with an estimated number of cases between 6,700 and 11,000 cases per year. Late clinical manifestations are relatively rare (table 4). The most frequent forms are Acrodermatitis chronica atrophicans (with an estimated number of around 280 to 630 cases per year) and Lyme Arthritis (with an estimated number around 300 and 900 cases per year). The estimated number of chronic Neuroborreliosis varies from 60 to 300 cases per year.
The most prominent variations in relative risk were observed between the 6 Sentinella Regions. The highest relative risk was observed in Sentinella Region 6 (RR 2.2, 95% confidence limits 1.8 to 2.7) with little variation between the univariate and the multivariate model. Lower relative risks were observed in Sentinella Regions 2 and 5. The balanced sex distribution was coherent with the descriptive analysis. The most affected age groups were the 65 to 79 years old patients. During 2009 and 2010 the relative risks were lower than the one in 2008.
The highest relative risk variations were observed between the 6 Sentinella Regions. The lowest risks were observed in Sentinella Region 1, which was the reference group. The highest relative risk was observed in Sentinella Region 5 (2.4, 95% confidence limits 1.9 to 3.0). However the other regions had an increased relative risk as well. No sex difference was observed. The most affected age groups were the 40 to 64 year and 65 to 79 year old persons. During 2009 and 2010, the relative risks were lower than those in 2008.
We estimated the same models as for consultations for tick bites and Lyme borreliosis. However we only present the relative risks without 95% confidence limits, because tick borne encephalitis is a 100% sample of cases in Switzerland. Therefore, there is no random variation. The highest relative risk variations were observed between the 6 Sentinella Regions. The most affected region was Sentinella Region 5, followed by Regions 4 and 2. There was a clear sex difference with a reduced relative risk in women. The most affected age groups are the 40 to 64 years and 65 to 79 years old persons. The relative risk in 2011 increased with respect to 2008.
| Table 1: Incidences per 100,000 inhabitants of cases of tick bites, Lyme borreliosis and tick borne encephalitis in Switzerland, 2008 to 2011. | |||||||||||||||
| Reported tick bite | Yearly | Lyme borreliosis | yearly | Tick borne encephalitis | yearly | ||||||||||
| Year | 2008 | 2009 | 2010 | 2011 | 2008 | 2009 | 2010 | 2011 | 2008 | 2009 | 2010 | 2011 | |||
| Total | 278 | 238 | 210 | 291 | 254 | 156 | 122 | 91 | 156 | 131 | 1.6 | 1.5 | 1.2 | 2.2 | 1.6 |
| Age groups | |||||||||||||||
| 0 to 5 years | 203 | 343 | 79 | 220 | 211 | 99 | 62 | 119 | 71 | 88 | 0.7 | 0.4 | 0.2 | 0.6 | 0.5 |
| 6 to 19 years | 258 | 284 | 229 | 310 | 270 | 103 | 120 | 66 | 134 | 106 | 1.0 | 0.9 | 0.8 | 1.4 | 1.1 |
| 20 to 39 years | 211 | 130 | 177 | 273 | 198 | 80 | 57 | 61 | 132 | 83 | 1.5 | 1.5 | 0.8 | 1.3 | 1.3 |
| 40 to 64 years | 328 | 252 | 230 | 264 | 268 | 238 | 164 | 119 | 172 | 173 | 1.8 | 1.7 | 1.8 | 3.2 | 2.1 |
| 65 to 79 years | 390 | 386 | 283 | 460 | 380 | 219 | 216 | 97 | 285 | 204 | 2.2 | 1.9 | 1.6 | 3.1 | 2.2 |
| ≥80 years | 156 | 96 | 179 | 191 | 156 | 49 | 17 | 75 | 27 | 42 | 1.4 | 1.6 | 1.1 | 1.3 | 1.3 |
| Sex | |||||||||||||||
| Men | 269 | 215 | 206 | 315 | 251 | 156 | 111 | 93 | 147 | 126 | 2.2 | 2.1 | 1.7 | 2.6 | 2.1 |
| Women | 287 | 261 | 215 | 268 | 258 | 155 | 133 | 89 | 166 | 136 | 1.0 | 0.9 | 0.7 | 1.7 | 1.1 |
| Sex ratio (m:f) | 1:1 | 2:3 | 1:1 | 1:1 | 1:1 | 1:1 | 1:1 | 1:1 | 1:1 | 1:1 | 2:1 | 2:1 | 2:1 | 3:2 | 2:1 |
| Sentinella regions | |||||||||||||||
| Region 1: GE, NE, VD, VS | 146 | 129 | 135 | 196 | 152 | 59 | 60 | 55 | 93 | 67 | 0.4 | 0.1 | 0.2 | 0.8 | 0.4 |
| Region 2: BE, FR, JU | 360 | 216 | 287 | 341 | 301 | 184 | 113 | 123 | 197 | 154 | 1.6 | 1.5 | 1.4 | 2.0 | 1.6 |
| Region 3: AG, BL, BS, SO | 292 | 205 | 161 | 288 | 236 | 161 | 170 | 86 | 105 | 130 | 1.1 | 1.1 | 1.1 | 2.1 | 1.3 |
| Region 4: LU, OW, NW, SZ, UR, ZG | 249 | 83 | 298 | 250 | 220 | 154 | 102 | 127 | 248 | 158 | 1.6 | 1.1 | 1.6 | 2.4 | 1.7 |
| Region 5: AR, AI, GL, SG, SH, TG, ZH, FL | 302 | 374 | 214 | 325 | 303 | 202 | 151 | 88 | 185 | 156 | 2.9 | 3.0 | 2.0 | 3.6 | 2.9 |
| Region 6: GR, TI | 382 | 345 | 242 | 382 | 338 | 168 | 124 | 96 | 125 | 128 | 0.6 | 0.6 | 0.2 | 0.6 | 0.5 |
| Table 2: Reports of Lyme borreliosis in Switzerland, 2008 to 2011. | |||||||||||
| Year | 2008 | 2009 | 2010 | 2011 | Total | ||||||
| N | % | N | % | N | % | N | % | N | % | ||
| Case classification | |||||||||||
| Possible case | 50 | (15.0) | 38 | (17.4) | 39 | (23.1) | 67 | (19.3) | 194 | (18.1) | |
| Confirmed case | 281 | (84.1) | 174 | (79.8) | 128 | (75.7) | 281 | (80.7) | 864 | (80.8) | |
| Unclassified | 3 | (0.9) | 6 | (2.8) | 2 | (1.2) | (0.0) | 11 | (1.0) | ||
| Total | 334 | (100.0) | 218 | (100.0) | 169 | (100.0) | 348 | (100.0) | 1069 | (100.0) | |
| History of tick bite* | |||||||||||
| Yes | 150 | (53.4) | 89 | (51.1) | 74 | (57.8) | 130 | (46.3) | 443 | (51.3) | |
| No | 125 | (44.5) | 84 | (48.3) | 53 | (41.4) | 149 | (53.0) | 411 | (47.6) | |
| Unknown | 6 | (2.1) | 1 | (0.6) | 1 | (0.8) | 2 | (0.7) | 10 | (1.2) | |
| Exposure* | |||||||||||
| Professional | 17 | (6.0) | 14 | (8.0) | 10 | (7.8) | 9 | (3.2) | 50 | (5.8) | |
| Leisure | 237 | (84.3) | 149 | (85.6) | 105 | (82.0) | 251 | (89.3) | 742 | (85.9) | |
| Both | 18 | (6.4) | 1 | (0.6) | 8 | (6.3) | 11 | (3.9) | 38 | (4.4) | |
| Unknown | 9 | (3.2) | 10 | (5.7) | 5 | (3.9) | 10 | (3.6) | 34 | (3.9) | |
| * confirmed cases | |||||||||||
| Table 3: Clinical symptoms, exposure and further details of tick borne encephalitis in Switzerland, 2008 to 2011. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Year | 2008 | 2009 | 2010 | 2011 | Total | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| N | % | N | % | N | % | N | % | N | % | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Case classification | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Possible case | 9 | (7.4) | 23 | (20.0) | 16 | (16.3) | 25 | (14.5) | 73 | (14.4) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Probable case | 27 | (22.1) | 25 | (21.7) | 24 | (24.5) | 47 | (27.3) | 123 | (24.3) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Confirmed case | 86 | (70.5) | 67 | (58.3) | 58 | (59.2) | 100 | (58.1) | 311 | (61.3) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Total | 122 | (100.0) | 115 | (100.0) | 98 | (100.0) | 172 | (100.0) | 507 | (100.0) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Diagnosis | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Meningitis | 23 | (18.9) | 13 | (11.3) | 29 | (29.6) | 32 | (18.6) | 97 | (19.1) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Meningoencephalitis | 77 | (63.1) | 68 | (59.1) | 53 | (54.1) | 103 | (59.9) | 301 | (59.4) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Encephalomyelitis | 7 | (5.7) | 4 | (3.5) | 1 | (1.0) | 3 | (1.7) | 15 | (3.0) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Radiculitis | 2 | (1.6) | 5 | (4.3) | (0.0) | 4 | (2.3) | 11 | (2.2) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Doubtful neurolog. Symptoms | 2 | (1.6) | 4 | (3.5) | 1 | (1.0) | 6 | (3.5) | 13 | (2.6) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No neurolog. Symptoms | 9 | (7.4) | 9 | (7.8) | 11 | (11.2) | 15 | (8.7) | 44 | (8.7) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown* | 2 | (1.6) | 12 | (10.4) | 3 | (3.1) | 9 | (5.2) | 26 | (5.1) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Death | 2 | (1.6) | 2 | (1.7) | 1 | (1.0) | (0.0) | 5 | (1.0) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Referral to hospital | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | 92 | (75.4) | 82 | (71.3) | 74 | (75.5) | 124 | (72.1) | 372 | (73.4) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | 23 | (18.9) | 21 | (18.3) | 19 | (19.4) | 35 | (20.3) | 98 | (19.3) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown | 7 | (5.7) | 12 | (10.4) | 5 | (5.1) | 13 | (7.6) | 37 | (7.3) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| History of tick bites | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | 48 | (39.3) | 39 | (33.9) | 50 | (51.0) | 79 | (45.9) | 216 | (42.6) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | 25 | (20.5) | 14 | (12.2) | 13 | (13.3) | 25 | (14.5) | 77 | (15.2) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown | 49 | (40.2) | 62 | (53.9) | 35 | (35.7) | 68 | (39.5) | 214 | (42.2) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Visiting the nature during 4 weeks before disease onset | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | 77 | (63.1) | 51 | (44.3) | 56 | (57.1) | 100 | (58.1) | 284 | (56.0) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | 2 | (1.6) | 3 | (2.6) | 1 | (1.0) | 3 | (1.7) | 9 | (1.8) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown | 43 | (35.2) | 61 | (53.0) | 41 | (41.8) | 69 | (40.1) | 214 | (42.2) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| *only laboratory reports | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Table 4: Clinical symptoms of Lyme Borreliosis in Switzerland, 2008 to 2011*. | |||||||||||||||||||||
| Year | 2008 | 2009 | 2010 | 2011 | Total | ||||||||||||||||
| Ob- ser- ved num- ber | % | Esti- mated num- ber | inci- dence per 100,000 | Ob- ser- ved num- ber | % | Esti- mated num- ber | inci- dence per 100,000 | Ob- ser- ved num- ber | % | Esti- mated num- ber | inci- dence per 100,000 | Ob- ser- ved num- ber | % | Esti- mated num- ber | inci- dence per 100,000 | Ob- ser- ved num- ber | % | Esti- mated 4 years mean num- ber | yearly inci- dence per 100,000 | ||
| Number of confirmed cases | 281 | (100.0) | 12,044 | 156 | 174 | (100.0) | 9,559 | 122 | 128 | (100.0) | 7,174 | 91 | 281 | (100.0) | 12,369 | 156 | 864 | (100.0) | 10,287 | 131 | |
| Erythema migrans | 246 | (87.5) | 10,544 | 137 | 155 | (89.1) | 8,515 | 109 | 120 | (93.8) | 6,726 | 85 | 255 | (90.7) | 11,470 | 142 | 776 | (89.8) | 9,239 | 118 | |
| Lympho- cytoma benignum | 10 | (3.6) | 429 | 6 | 14 | (8.0) | 769 | 10 | 7 | (5.5) | 392 | 5 | 8 | (2.8) | 360 | 4 | 39 | (4.5) | 464 | 6 | |
| Acrodermatitis chronica | 12 | (4.3) | 514 | 7 | 10 | (5.7) | 549 | 7 | 5 | (3.9) | 280 | 4 | 14 | (5.0) | 630 | 8 | 41 | (4.7) | 488 | 6 | |
| Early neuro- borreliosis | 6 | (2.1) | 257 | 3 | (0.0) | 3 | (2.3) | 168 | 2 | 1 | (0.4) | 45 | 1 | 10 | (1.2) | 119 | 2 | ||||
| Lyme carditis | 1 | (0.4) | 43 | 1 | (0.0) | 1 | (0.8) | 56 | 1 | 3 | (1.1) | 135 | 2 | 5 | (0.6) | 60 | 1 | ||||
| Lyme arthritis | 14 | (5.0) | 600 | 8 | 10 | (5.7) | 549 | 7 | 6 | (4.7) | 336 | 4 | 19 | (6.8) | 855 | 11 | 49 | (5.7) | 583 | 7 | |
| Chronic neuro- borreliosis | 6 | (2.1) | 257 | 3 | 1 | (0.6) | 55 | 1 | 2 | (1.6) | 112 | 1 | 4 | (1.4) | 180 | 2 | 13 | (1.5) | 155 | 2 | |
| * Estimated numbers based on a sentinel system (Sentinella Survey) for the whole of Switzerland. | |||||||||||||||||||||
| Table 5: Determinants of cases of tick bites, Lyme borreliosis and tick borne encephalitis by poisson regression in Switzerland, 2008 to 2011. | ||||||
| RR | 95% Confidence limits | Adjusted RR* | 95% Confidence limits | |||
| Tick bites | ||||||
| Year | ||||||
| 2008 | 1 | 1 | ||||
| 2009 | 0.88 | 0.76 | 1.01 | 0.87 | 0.76 | 0.99 |
| 2010 | 0.76 | 0.66 | 0.88 | 0.76 | 0.66 | 0.88 |
| 2011 | 1.10 | 0.96 | 1.22 | 1.07 | 0.95 | 1.21 |
| Age groups | ||||||
| 0 to 5 years | 1 | 1 | ||||
| 6 to 19 years | 1.35 | 1.08 | 1.70 | 1.34 | 1.07 | 1.68 |
| 20 to 39 years | 1.07 | 0.86 | 1.33 | 1.02 | 0.82 | 1.28 |
| 40 to 64 years | 1.42 | 1.15 | 1.75 | 1.36 | 1.10 | 1.68 |
| 65 to 79 years | 2.01 | 1.60 | 2.52 | 1.89 | 1.51 | 2.38 |
| ≥ 80 years | 0.83 | 0.59 | 1.17 | 0.79 | 0.55 | 1.12 |
| Sex | ||||||
| Men | 1 | 1 | ||||
| Women | 0.99 | 0.90 | 1.09 | 0.99 | 0.90 | 1.09 |
| Sentinella regions | ||||||
| Region 1: GE, NE, VD, VS | 1 | 1 | ||||
| Region 2: BE, FR, JU | 1.94 | 1.63 | 2.30 | 1.92 | 1.61 | 2.28 |
| Region 3: AG, BL, BS, SO | 1.57 | 1.30 | 1.90 | 1.53 | 1.27 | 1.86 |
| Region 4: LU, OW, NW, SZ, UR, ZG | 1.36 | 1.10 | 1.68 | 1.36 | 1.10 | 1.68 |
| Region 5: AR, AI, GL, SG, SH, TG, ZH, FL | 1.98 | 1.69 | 2.32 | 1.97 | 1.68 | 2.31 |
| Region 6: GR, TI | 2.22 | 1.82 | 2.71 | 2.18 | 1.79 | 2.67 |
| Lyme borreliosis | ||||||
| Year | ||||||
| 2008 | 1 | 1 | ||||
| 2009 | 0.79 | 0.66 | 0.96 | 0.78 | 0.65 | 0.94 |
| 2010 | 0.59 | 0.48 | 0.72 | 0.59 | 0.47 | 0.72 |
| 2011 | 1.03 | 0.88 | 1.23 | 1.03 | 0.88 | 1.22 |
| Age groups | ||||||
| 0 to 5 years | 1 | 1 | ||||
| 6 to 19 years | 1.10 | 0.79 | 1.54 | 1.10 | 0.79 | 1.53 |
| 20 to 39 years | 0.92 | 0.67 | 1.28 | 0.89 | 0.64 | 1.23 |
| 40 to 64 years | 1.93 | 1.43 | 2.60 | 1.84 | 1.36 | 2.49 |
| 65 to 79 years | 2.22 | 1.61 | 3.07 | 2.12 | 1.54 | 2.94 |
| ≥80 years | 0.41 | 0.21 | 0.79 | 0.39 | 0.20 | 0.75 |
| Sex | ||||||
| Men | 1 | |||||
| Women | 1.04 | 0.91 | 1.19 | 1.05 | 0.92 | 1.20 |
| Sentinella regions | ||||||
| Region 1: GE, NE, VD, VS | 1 | 1 | ||||
| Region 2: BE, FR, JU | 2.33 | 1.81 | 3.01 | 2.30 | 1.78 | 2.97 |
| Region 3: AG, BL, BS, SO | 2.02 | 1.53 | 2.65 | 1.90 | 1.44 | 2.50 |
| Region 4: LU, OW, NW, SZ, UR, ZG | 2.36 | 1.78 | 3.11 | 2.34 | 1.77 | 3.10 |
| Region 5: AR, AI, GL, SG, SH, TG, ZH, FL | 2.42 | 1.91 | 3.06 | 2.34 | 1.85 | 2.96 |
| Region 6: GR, TI | 1.95 | 1.42 | 2.68 | 1.87 | 1.36 | 2.56 |
| Tick borne encephalitis | ||||||
| Year | ||||||
| 2008 | 1 | 1 | ||||
| 2009 | 0.93 | 0.94 | ||||
| 2010 | 0.79 | 0.79 | ||||
| 2011 | 1.38 | 1.38 | ||||
| Age groups | ||||||
| 0 to 5 years | 1 | 1 | ||||
| 6 to 19 years | 2.17 | 2.16 | ||||
| 20 to 39 years | 2.66 | 2.65 | ||||
| 40 to 64 years | 4.38 | 4.40 | ||||
| 65 to 79 years | 4.52 | 4.67 | ||||
| ≥80 years | 2.77 | 3.16 | ||||
| Sex | ||||||
| Men | 1 | 1 | ||||
| Women | 0.51 | 0.50 | ||||
| Sentinella regions | ||||||
| Region 1: GE, NE, VD, VS | 1 | 1 | ||||
| Region 2: BE, FR, JU | 4.30 | 4.23 | ||||
| Region 3: AG, BL, BS, SO | 3.53 | 3.38 | ||||
| Region 4: LU, OW, NW, SZ, UR, ZG | 4.41 | 4.32 | ||||
| Region 5: AR, AI, GL, SG, SH, TG, ZH, FL | 7.53 | 7.38 | ||||
| Region 6: GR, TI | 1.24 | 1.20 | ||||
| * Adjusted relative risks for all factors in the model assuming independence between the factors year, age groups, sex and region. | ||||||
The occurrence of tick related diseases has changed over the past years, by region, age and sex. However, the three tick related diseases have their own specific epidemiology. The estimated number of tick bites of about 17,000 to 23,000 cases every year is based on reports from primary care physicians. It represents the number of consultations due to tick bites. This estimation does not represent the total number of tick bites observed in Switzerland, since most people do not seek medical advice in case of a tick bite. Studies have shown that about 5% of tick-bites result in an infection caused by Borrelia [18, 19]. Considering the yearly 7,000 to 12,000 estimated cases of Lyme borreliosis, we projected the number of tick-bites in Switzerland to be 150–200,000 every year. About 10% of Lyme borreliosis patients are diagnosed during more advanced stages. This amounted to about 700 to 1,200 cases per year. The number of chronic Neuroborreliosis levels to about 60 to 300 cases every year. Tick borne encephalitis is rare, however often results in serious conditions. Hospitalisation was required in 73% of all cases. The yearly incidence of 1.6 cases per 100,000 has to be interpreted with caution since tick borne encephalitis occurs in local clusters meaning that the local incidences are much higher than this estimate. The reason for not reporting local incidences in this paper is that the focus of this paper was to compare consultations for tick bites, Lyme borreliosis and tick borne encephalitis in a general way.
The data on tick borne encephalitis are probably the most complete data set available for tick related diseases in Switzerland. The Swiss mandatory surveillance system theoretically covers 100% of all cases. However, underreporting is an issue and should be evaluated in a capture-recapture study. The Swiss data on tick bites and Lyme borreliosis, however, are based on less firm data, but they are the best estimates currently available. The estimates may be over-estimations since the Sentinella network consists of general practitioners (including paediatricians and internists) who may see tick bites and Lyme borreliosis more often than other physicians. Another source of potential bias is that the participating physicians in the Sentinella system work in places where the people aggregate, and not in a regular geographic distribution. This leads to local differences of Sentinella’s coverage and therefore limits the generalisation of our estimates. From a statistical point of view, it would be an advantage if a random sample of contributing physicians could be drawn for Switzerland, and if the physicians in this sample would be 100% compliant with the requirements of the sentinel system. This system would allow a better estimation of the confidence limits around the estimated numbers and incidence rates. However, the effort of creating a 100 per cent compliant physician’s network is an unrealistic target. It is therefore preferable to have self-selected but compliant physicians rather than randomly-selected and less compliant physicians. Unfortunately, the direction and size of bias due to self-selection is unpredictable, and the evaluation of the play of chance in the present sentinel system is of limited value.
The occurrence of tick borne encephalitis has been increasing since 1984 [6, 14, 15]. Case numbers have risen from about 50 cases per year during 1990 to 1994 to about 140 cases per year during 2002 to 2011. In Switzerland, first epidemiological investigations were performed in the late 1960s and the early 1970s [20]. The authors described the clinical picture, the epidemiology and the entomology in detail. They reported a seroprevalence in blood donors of 0.2 to 0.3%, and for the first time described endemic areas. The seroprevalence was studied again in 1994 and showed that healthy blood donors had a prevalence of 0.6%, whereas hospitalised patients showed a seroprevalence of 2.4% [6]. Since then, no further seroprevalence studies have been performed in Switzerland. A detailed report on tick borne encephalitis was published for the canton of Thurgau during 1990 to 1995 [21]. During this period, the authors observed 30 cases with an incidence of 5.4 per 100,000 inhabitants which was clearly above the national incidence of 0.5 per 100,000. They described the disease as mild in most cases with a case fatality rate of 1 to 2%. In a subsequent study, data on tick borne encephalitis in the canton of Thurgau was analysed for the period of 1996 to 1999 [22]. The authors concluded that the disease was spreading in the canton, and that the number of new cases was increasing as its incidence rose remarkably. They also noted that more than 80% of all cases suffered from disabling neurasthenic syndromes which led to absence from work for two months on average. Later, another study was published concerning the late consequences of tick borne encephalitis in Switzerland [23]. A few weeks after discharge from hospital, 73% of patients still had complaints, and one year later 56% still suffered from the disease. They also described a persisting neurasthenic syndrome in 10% of the cases. In 2005, the FOPH noted for the first time a steep increase in the incidence of the disease [14]. For the first time since introduction of the notification system, 202 cases were reported. In 2006, the highest number of cases in Switzerland was notified with 246 cases. The recommendations for vaccination were therefore revised in 2006 [16]. Basically, exposed persons aged over 6 years should be vaccinated, if they live in or visit an endemic area. The actual list of endemic areas is available from the website of the FOPH with regular updates (last in December 2011 [24]).
In Switzerland, the epidemiology of Lyme borreliosis has been intensively studied. The first epidemiological investigation on Lyme borreliosis in Switzerland was performed in 1986 [8]. The authors reported 350 serologically positive cases. They found that Erythema migrans was present in 45%, neurological manifestations in 25%, acrodermatitis chronica atrophicans in 15%, arthritis in 31% and carditis in 4% of all cases. This is in contrast to our findings, especially for Erythema migrans, which makes up to 90% of all cases in our series. The most probable explanation is that the study in 1986 was based on a seropositive population. It is well established today that Erythema migrans is a clinical observation, and that the serology is infrequently positive [25]. We found a similar age and sex distribution with patients mainly aged 40-79, and a predominance of women. During 1987 to 1988, Erythema migrans was first surveyed by the Swiss Sentinella system. Based on this data, the estimated number of cases levelled to 6,000 cases per year [6].
In the early 1990s the focus of epidemiological research concerning Lyme borreliosis was on seroprevalences. In a study of 259 forestry workers in the canton of Solothurn, a seroprevalence of 35% was detected which increased with age [9]. A study in 950 Swiss orienteers found a seroprevalence of 26%. This was high with respect to two control groups with seroprevalences between 4 and 6%. In a follow-up after six months, 8% seroconverted and 1 case developed Lyme borreliosis [11]. In a case-control study with 378 neurological patients and 1,134 healthy blood donors as controls, a seroprevalence of about 10% was found in both groups. No neurological syndrome could be associated with Lyme borreliosis in that study, and screening neurologically affected patients for Lyme borreliosis was not an option to be recommended [12].
The epidemiology of Lyme borreliosis in the French-speaking part of Switzerland was published in 2000 [26]. Based on a survey the authors estimated the incidence of Lyme borreliosis mainly in seropositive cases, although seronegative cases were included as well. They found an incidence of 9 per 100,000 in the Valais and 95 per 100,000 inhabitants in the canton of Neuchâtel. The proportion of Erythema migrans was 46 %; 33 % were in stage II of the disease, and 21% in stage III of the disease. This again is in contrast with our findings in a population treated by general practitioners where Erythema migrans patients make up to 90 % of the reported cases. However, we found similar incidences in the French speaking part of Switzerland with 59 to 93 cases per 100,000 inhabitants. In 2011, the FOPH published its last report on Lyme borreliosis [13]. The estimation methods were improved since it is now possible to estimate incidences in a more credible way (this report: per 100,000 inhabitants; report 2011 [13]: per 1,000 consultations). Due to a revision of the case definition, the proportion of Erythema migrans increased by about 10% compared to the report in 2011. The adapted definition now includes a reddening of less than 5 cm diameter as Erythema migrans if a central livid paling is reported and a treatment with antibiotics is started.
The consequences of a tick bite seem to be mild. Between 1997 and 1998, fever after tick bite was investigated in 75 patients in the north eastern part of Switzerland, an endemic area for tick borne encephalitis and Lyme borreliosis [27]. In 52 % of all cases no causative agent could be found. However, there was evidence of antibodies to Borrelia burgdorferi sensu latoin 25 %, of antibodies to tick borne encephalitis virusin 11 %, of antibodies to Ehrlichia species in 10% and of antibodies to Rickettsia helveticain 11%. In 8% of the cases dual infections were found. The risk of developing Lyme borreliosis after tick bite seems to be low in Switzerland. Out of 376 patients recently bitten by a tick, only 8 (2.1%) developed Erythema migrans, and no serious diseases were recorded [28]. In a further recent study on tick bites in a highly endemic area of Switzerland, seroconversion and development of Lyme borreliosis was investigated in 269 patients [18]. The authors found a seroconversion rate of 3.5%, and 5% developed Erythema migrans. Seroconversion rates and development of Erythema migrans were dependent on the infection status of the tick carrying Borrelia burgdorferi sensu lato. If patients were bitten by a Borrelia infected tick, 1.6% seroconverted and 6.6% developed Erythema migrans. Patients bitten by uninfected ticks developed seroconversion in 2.4% and Erythema migrans in 3.2% of cases [18]. This may be explained by the fact that a tick bite by an infected tick was missed. Similar findings have been observed in Sweden [19].
Tick borne diseases are frequent in Switzerland. During the considered period, Lyme borreliosis and tick borne encephalitis increased in number and widespread all over Switzerland. Tick borne encephalitis remains restricted to endemic areas; however, new areas have been detected recently. In general, consequences of tick bites seem to be mild, but long term follow-up cohort studies with reasonably large study populations after tick bite would be required to elucidate the risk of developing a tick borne disease.
The case definition of tick borne encephalitis is based on clinical and laboratory criteria. Clinical criteria are: influenza-like symptoms or meningitis, meningoencephalitis, encephalomyelitis and radiculitis. Laboratory criteria are: presence of IgM, IgM and IgG, seroconversion, a fourfold increase in IgG and presence of specific nucleic acids. Presence of IgM without clinical symptoms is defined as “no case”. Presence of IgM or seroconversion and influenza like symptoms or doubtful neurological symptoms is defined as “possible case”. Presence of IgM and meningitis, meningoencephalitis, encephalomyelitis, radiculitis as well as presence of IgM and IgG or seroconversion with influenza like symptoms or doubtful neurological symptoms is defined as “probable case”. If laboratory criteria and clinical criteria are fulfilled, the case is defined as “confirmed case”.
The case definition of Lyme borreliosis is an adapted version of the EUCALB definition [17]. A case is confirmed if it is in line with the following clinical situations:
– Erythema migrans, defined as a local reddening of more than 5 cm diameter, or a local reddening of less than 5 cm diameter with a central livid paling and the physicians decision to start an antibiotic treatment.
– Lymphocytoma benigna, a painless, livid plaque at the ear lobe or helix, at the mammilla or at the scrotum, confirmed either by serology or by histology.
– Early neuroborreliosis, a painful meningoradiculoneuritis possibly including cranial nerves with serological confirmation or proof of specific intrathecal antibody production.
– Lyme carditis, defined as a proof of acute heart bloc grade I to III with rhythmic disorder, or myo- or pancarditis with serological confirmation or molecular proof in a biopsy of the endocardium.
– Lyme arthritis, defined by recurrent, short attacks of joint swelling in one or few larger joints, with serological confirmation or molecular proof in synovial fluid or biopsy. (This is a epidemiological definition. The clinical decision to treat or not to treat the patient may be difficult and has to be judged based on the individual situation.)
– Acrodermatitis chronica atrophicans, a reddish to livid dermal change at the extremities with light swelling or atrophy and serological, histological, molecular or cultural proof of Lyme borreliosis.
– Chronic neuroborreliosis, defined as long lasting encephalitis, encephalomyelitis, meningoencephalomyelitis independent of radicular signs, with lymphocytosis in the cerebrospinal fluid and with intrathecal production of specific antibodies.
Acknowledgement:We thank all the physicians of the Swiss Sentinel Surveillance Network (Sentinella) who have identified and provided information on all the study items concerning tick bites and Lyme borreliosis, as well as all those who reported tick borne encephalitis cases within the mandatory notification system.
1 Gern L, Lienhard R, Péter O. Maladies et agents pathogènes transmis par les tiques en Suisse, Rev Med Suisse. 2010;6:1906–9.
2 Zimmermann H, Koch D. Epidemiologie der Frühsommer-Meningo-enzephalitis (FSME) in der Schweiz 1984 bis 2004. Therapeutische Umschau 2005;62(11):719–25.
3 Egger M. Lyme-Borreliose – Übersicht. Therapeutische Umschau. 2005;62(11):731–6.
4 Rossi M. Spätmanifestationen der Lyme-Borreliose. Therapeutische Umschau. 2005;62(11):745–50.
5 Bundesamt für Gesundheit. Lyme-Borreliose: Sentinella-Erhebung 2008/2009 – Das Nationale Referenzzentrum für Zecken und zeckenübertragene Krankheiten stellt sich vor. Bull BAG. 2010;22:579–82.
6 Bundesamt für Gesundheit. Zeckenenzephalitis und Lyme Borreliose in der Schweiz. Bull BAG. 1995;37:6–16.
7 Orach C, Itin P, Flückiger U. Lyme Borreliose in der Schweiz. Schweiz Med Forum. 2007;7:850–5.
8 Aeschimann A, Chamot E, Gigon F, Jeanneret JP, Kesseler D, Walther C. B. burgdorferi in Switzerland. Zbl Bakt Hyg. A 1986;263:450–8.
9 Nadal W, Wunderli W, Briner H, Hansen K. Prevalence of antibodies to Borrelia burgdorferi in forestry workers and blood donors from the same region in Switzerland. Eur J Clin Microbiol Infect Dis. 1989;8(11):992–5.
10 Fahrer H, Sauvain MJ, van der Linden S, Zhioua E, Gern L, Aeschlimann A. Prävalenz der Lyme Borreliose in einer Schweizer Risikopopulation. Schweiz. Med. Wochenschr. 1988;118(2):65–9.
11 Fahrer H, van der Linden SM, Sauvain MJ, Gern L, Zhioua E, Aeschlimann A. The prevalence and incidence of clinical and asymptomatic Lyme borreliosis in a population at risk. J Infect Dis. 1991;163(2):305–10.
12 Altpeter ES, Meier C. Epidemiologische Aspekte der neurologischen Komplikationen der Lyme-Borreliose in der Schweiz. Schweiz. Med. Wochenschr. 1992;122(1–2):22–6.
13 Bundesamt für Gesundheit. Lyme-Borreliose: Sentinella-Erhebung 2008 bis 2010. Bull. BAG. 2011;24:895–8.
14 Bundesamt für Gesundheit. Zeckenenzephalitis (FSME): deutliche Zunahme der gemeldeten Fälle. Bull BAG. 2005;38:671–3.
15 Bundesamt für Gesundheit. Zeckenenzephalitis (FSME): weitere Zunahme der gemeldeten Fälle im 2006. Bull BAG. 2007;4:57–60.
16 Bundesamt für Gesundheit. Empfehlungen zur Impfung gegen Zeckenenzephalitis. Bull BAG. 2006;13:225–31.
17 EUCALB. European Concerted Action on Lyme Borreliosis. Vienna. [Update 2011 Jul 4; cited 2012 March 3]. Available from: http://meduni09.edis.at/eucalb/http://meduni09.edis.at/eucalb/
18 Huegli D, Moret J, Rais O, Moosmann Y, Erard P, Malinverni R, Gern L. Prospective study on the incidence of infection by Borrelia burgdorferi sensu lato after tick bite in a highly endemic area of Switzerland. Ticks and Tick-borne Diseases. 2011;2(3):129–36.
19 Fryland L, Wilhelmsson P, Lindgren PE, Nyman D, Ekerfelt C, Forsberg P. Low risk of developing Borrelia burgdorferi infection in the south-east of Sweden after being bitten by a Borrelia burgdorferi-infected tick. Int J Infect Dis. 2011;15(3):174–81.
20 Wyler R, Matile H. Zeckenenzephalitis in der Schweiz: 1. Klinik und Epidemiologie, 2. Diagnose und Immunprophylaxe, Schweiz. Rundschau Med. (PRAXIS) 1984;73(19):601–19.
21 Baumberger P, Krech T, Frauchiger B. Entwicklung der Frühsommer-Meningoenzephalitis (FSME) in der Region Thurgau 1990–1995 – ein neues Endemiegebiet? Schweiz Med Wochenschr. 1996;126(48):2072–7.
22 Schwanda M, Oertli S, Frauchiger B, Krause M. Die Frühsommer-Meningoenzephalitis im Kanton Thurgau: eine klinisch-epidemiologische Analyse, Schweiz Med Wochenschr. 2000;130(41):1447–55.
23 Lämmli B, Müller A, Balmer PE. Spätfolgen nach Frühsommer-Meningoenzephalitis. Schweiz Med Wochenschr. 2000;130(24):909–15.
24 Bundesamt für Gesundheit. Berne. [Update 2012 March 1, cited 2012 March 3]. Available from: http://www.bag.admin.ch/themen/medizin/00682/00684/06330/index.html
25 Stanek G, Wormser GP, Gray J, Strle F. Lyme borreliosis, Lancet. 2012;379:461–73.
26 Nahimana I, Gern L, Péter O, Praz G, Moosmann Y, Francioli P. Epidémiologie de la borréliose de Lyme en Suisse romande. Schweiz Med Wochenschr. 2000;130(41):1456–61.
27 Baumann D, Pusterla N, Péter O, Grimm F, Fournier PE, Schär G, et al. Fieber nach Zeckenstich: Klinik und Diagnostik von akuten Zeckenstiche-assozierten Infektionskrankheiten in der Nordostschweiz. Dtsch Med Wochenschr. 2003;128(19):1042–7.
28 Nahimana I, Gern L, blanc DS, Praz G, Francioli P, Péter O. Risk of Borrelia burgdorferi infection in western Switzerland following tick bite. Eur J Clin Microbiol Infect Dis. 2004;23(8):603–8.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.