Skin disorders encountered in a Swiss paediatric emergency department
DOI: https://doi.org/10.4414/smw.2013.13731
Brigitte
Landolt, Georg
Staubli, Ulrich
Lips, Lisa
Weibel
Summary
QUESTIONS UNDER STUDY: While skin disorders are commonly seen in paediatric emergency departments (PED), the exact frequency of the various dermatological conditions is unknown. Our aim was to evaluate the occurrence and spectrum of skin disorders in an urban PED and the need for a dermatological opinion.
METHODS: The medical records of patients attending the PED during 120 days over a 1-year period were analysed. The dermatological findings were evaluated as to incidence, demographic details, frequency of dermatological review and treatment. A questionnaire assessed the need for dermatological support.
RESULTS: Skin findings were recorded in 1,572 (17.4%) of the 9,041 attendances. The skin problem was the primary cause of the PED visit or related to the primary complaint in 853 (54.3%) and 335 (21.3%) cases respectively. In 373 patients (23.8%) a diagnosis was only suspected or remained unknown. Inflammatory and allergic disorders were most commonly encountered (42.9%), followed by skin infections (31.8%), physically induced skin lesions (11.9%), varia/unknown (11.1%) and congenital disorders (2.3%). Viral and parainfectious exanthema was the most common diagnosis (17.6%), followed by anogenital dermatitis (7.7%), gingivostomatitis (7.1%), petechiae (6.4%), burns (6.0%), urticaria (5.0%) and insect bite reactions (5.0%). 81 (5.2%) of the patients with skin conditions were hospitalised. The PED doctors expressed the wish for a dermatological opinion in 25% of the patients with skin findings.
CONCLUSIONS: We identified a high frequency, broad spectrum and diagnostic difficulties of paediatric skin conditions. Our data highlight the need for educational measures and close collaboration between the two specialities to improve management of these children.
Introduction
Skin lesions are seen in 11–31% of all visits to paediatric consultancies and clinics [1– 3, 4]. Only a few studies have evaluated skin disorders encountered in a paediatric emergency department (PED). The incidence of dermatological findings was seen to vary from 4% to 40% in these studies [5– 10]. The range of these incidences results from the variable definition of skin disorders used in these studies (e.g., whether trauma-induced skin lesions were included or not), the seasonal period of the study and the method of data collection (under-reporting in the case of retrospective computerised data search). Most of the junior doctors dealing with these patients in the PED have limited training in paediatric dermatology and experience considerable diagnostic difficulties. A relatively poor diagnostic agreement of 18–66% is reported between paediatricians and (paediatric) dermatologists for skin disorders in children [5, 6, 11]. This highlights the need for greater emphasis on dermatological training for paediatric residents and suggests an important role for paediatric dermatologists in PEDs.
The aim of this study was to evaluate the frequency and spectrum of skin disorders seen in a PED, and to assess diagnostic difficulties and the need for a dermatological opinion.
Materials and methods
Patients and data collection
We retrospectively analysed the digital medical records of all pediatric patients who attended the PED at the University Children’s Hospital of Zurich (Switzerland) during the first 10 days of each month from 1 April 2009 to 31 March 2010. Thus a total of 120 days were analysed, evenly distributed over a one-year period. Our hospital is the largest paediatric hospital in Switzerland and the interdisciplinary PED sees 27,000–30,000 child outpatients per year. All patients are first examined by paediatric residents, who are supervised by qualified paediatricians. The majority of cases with dermatological findings are managed by the PED paediatric team without confirmation of the diagnosis by a dermatologist. In more severe cases the paediatric team asks for a dermatological opinion. Only one dermatologist (LW) working 50% at our hospital was available for dermatological support in the PED during the time of the study.
All PED patients’ medical records are collected in a computerised database. A doctoral candidate (BL) reviewed the medical notes of each patient presenting to the PED during the above-mentioned time period and recorded any dermatological findings mentioned in these case notes. This was done without the use of computerised search tools but by carefully reading each case note. We excluded trauma-induced skin lesions such as cuts, lacerations, bruises, haematomas and animal bites, but burns, scalds, infected wounds, scars and insect stings were not excluded from the analysis. In addition we excluded neonatal jaundice, anaphylactic shock, nail traumas and dental abscesses. We registered all dermatological findings in total (occasionally more than one per patient) but also the number of children presenting to the PED with skin lesions. It was determined whether the dermatological finding was the primary cause of the PED visit, whether it was related to the primary complaint or whether it represented an incidental finding during the patient’s examination. The demographic data extracted were the following: age, gender, manner of referral (by physician or parental), clinical description of the skin lesion, diagnosis, the certainty of the diagnosis (certain, suspected or unknown), treatment (systemic, topical and systemic, none or other), frequency of hospital admission, frequency of dermatological review and manner of follow-up (paediatrician, dermatologist, other specialist or none). The majority of the children were not seen by a dermatologist and in general the paediatrician’s diagnoses were assumed to be correct. The need for dermatological support in the PED was additionally assessed with the aid of a questionnaire. At the end of the evaluation period, the PED doctors (all qualified paediatricians) were asked to answer the following questions:
– In how many (%) of the dermatological findings would I benefit from a dermatological opinion?
– In how many (%) of the dermatological findings do I consider a dermatological review essential for the patient’s management?
– In how many (%) of these cases is a dermatological review unavailable (i.e. dermatologist unavailable)?
The study was approved and conducted in accordance with the ethical standards of our institution.
Statistical analysis
Data collected from the patients were entered in a computerised database. All analyses were performed with Microsoft Excel 11.5.9 for Macintosh. Mean, standard deviation (SD) and percentages were calculated as appropriate.
Results
Patients and frequency of skin disorders
There were a total of 9,041 (75.3/day) attendances at the PED during the above-mentioned study period (120 days over 1 year). In 1,572 (17.4%) of them skin findings were recorded (13.1 cases/day). If burns and scalds were excluded the number of dermatological findings decreased to 1,478 (16.3%). 99 patients (6.3%) presented with more than one skin lesion and in 86 children (5.5%) the same dermatological problem prompted more than one visit to the PED. In 853 (54.3%) of the total of 1,572 dermatological disorders the skin problem was the primary cause of the PED visit. The dermatological finding was related to the primary complaint or represented an unrelated, incidental finding in 335 (21.3%) and 384 (24.4%) cases respectively. Table 1 summarises the patients’ epidemiological data and treatment. In 373 cases (23.8%) a diagnosis was only suspected or remained unknown as stated by the PED doctors. In only 15 cases (1%) was a dermatological review performed and the patients were seen by a paediatric dermatologist (LW).
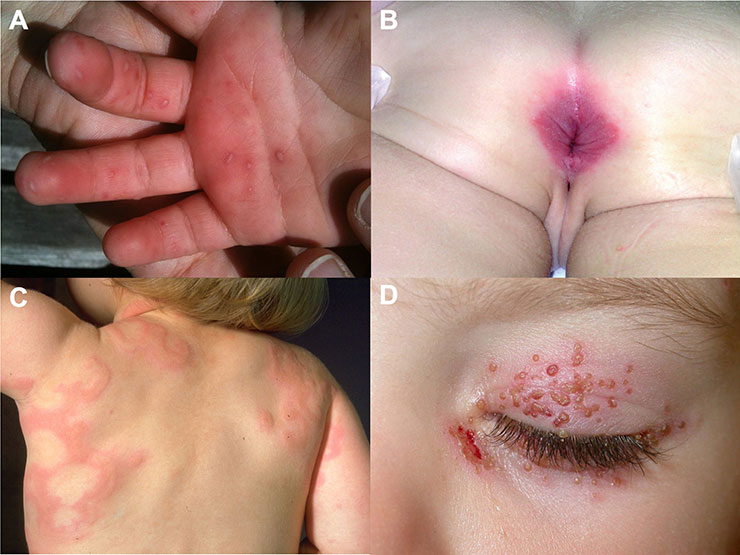
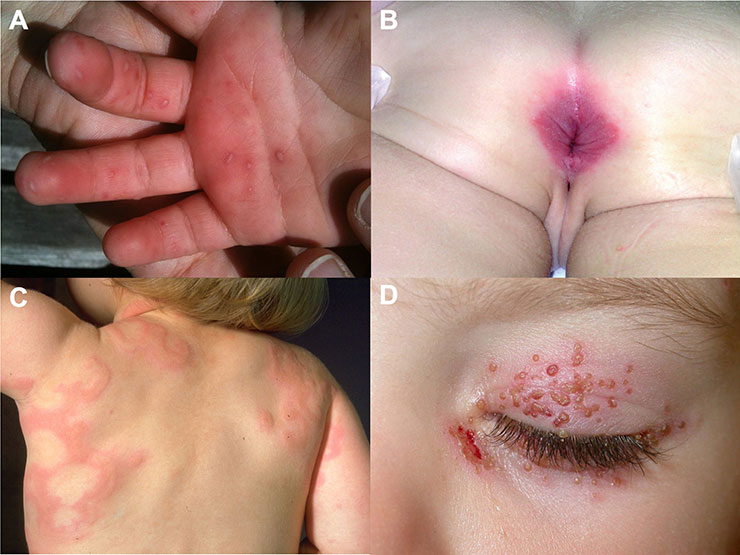
Figure 1
Clinical examples of skin disorders which were commonly encountered in the Pediatric Emergency Department. 1A. Hand-foot-mouth disease. 1B. Perianal streptococcal infection. 1C. Anular urticaria of childhood. 1D. Periocular herpes simplex virus infection.
Spectrum of dermatological diagnoses
Table 2 shows the frequency of the underlying pathogenetic causes of the skin conditions for all patients as well as for different age groups. Systemic conditions with skin eruptions such as Henoch Schoenlein purpura, Kawasaki disease and erythema multiforme were included in the allergic/inflammatory group. A total of 42.9% of diseases were allergic/inflammatory in nature, followed by 31.8% of skin infections (16.2% bacterial and 11.1% viral), physically induced skin lesions in 11.9%, varia/unknown in 11.1% and congenital disorders in 2.3%. In infants allergic/inflammatory diseases were even more frequent (50.1%), skin infections less common (18.7%; fungal infections accounting for 7.8%) and congenital lesions were observed in 5.8%. Over the age of 6 years skin infections, particularly bacterial infections, were the main cause of skin eruptions (41.5%). In table 3 the twenty most common diagnoses are listed according to frequency for all patients and in table 4 by age groups. Viral and parainfectious exanthema was the overall most common diagnosis (17.6%), followed by anogenital dermatitis (7.7%), gingivostomatitis (7.1%), petechiae (6.4%), burns (6.0%), urticaria (5.0%) and insect bite reactions (5.0%). Clinical examples of the most frequently observed diagnoses are shown in figure 1.
Eighty-one (5.2%) of the patients with skin conditions were admitted for in-patient treatment, whereas the overall hospitalisation rate was 11.6% for all attendances at the PED. The main dermatological conditions resulting in hospitalisation were cellulitis/erysipelas, burns/scalds, petechiae (due to idiopathic thrombocytopenic purpura, meningococcal infection or chemotherapy-induced thrombocytopenia), skin abscess, wound infection or atopic dermatitis in 12 (14.8%), 11 (13.6%), 6 (7.4%), 5 (6.2%), 4 (4.9%) and 3 (3.7%) cases respectively.
The questionnaire completed by the qualified PED paediatricians (n = 8) produced the following results: in 24.1% ± 9.6 of the dermatological findings the paediatricians felt that they would benefit from a dermatological opinion. In 15.6% ± 8.6 of skin disorders encountered they considered a dermatological review essential for the patient’s management. They estimated that in 12.8% ± 16.7 of these cases the hospital’s dermatologist was unavailable for a dermatological opinion.
|
Table 1:Characteristics of the 1,572 attendances at the Paediatric Emergency Department (PED) with dermatological disorders. |
|
Patients’ characteristics
|
N = 1,572
|
| Gender
Male
Female |
871 (55.4%)
701 (44.6%) |
| Age of patients (years)
Mean (SD) |
4.4 (4.2) |
| Manner of referral
By parental request
By physician |
1,335 (84.9%)
237 (15.1%) |
| Diagnosis (as stated by the PED doctors)
Certain
Suspected
Unknown |
1,199 (76.3%)
210 (13.4%)
163 (10.4%) |
| Dermatological review perfomed |
15 (1.0%) |
| Treatment of skin condition
Topical
Systemic
Topical and systemic
Other*
None |
255 (16.2%)
300 (19.1%)
162 (10.3%)
161 (10.2%)
694 (44.1%) |
| Hospitalisation |
81 (5.2%) |
| Follow-up recommended
General practitioner or paediatrician
Dermatologist
Other specialist
None |
318 (20.2%)
15 (1.0%)
113 (7.2%)
1,126 (71.6%) |
| *e.g. surgical therapy, cessation of previous medication. |
|
Table 2: Underlying causes of the skin conditions for all patients and by age groups. |
|
Causes
|
<1 year (n = 347)
|
1–6 years (n = 786)
|
>6 years (n = 439)
|
All ages (n = 1,572)
|
| Allergic/inflammatory reactions* |
174 (50.1%) |
343 (43.6%) |
157 (35.8%) |
674 (42.9%) |
| Skin infections
Bacterial
Viral
Fungal
Parasitosis |
65 (18.7%)
17 (4.9%)
21 (6.1%)
27 (7.8%)
0 (0.0%) |
253 (32.2%)
118 (15.0%)
104 (13.2%)
18 (2.3%)
13 (1.7%) |
182 (41.5%)
120 (27.3%)
49 (11.2%)
4 (0.9%)
9 (2.1%) |
500 (31.8%)
255 (16.2%)
174 (11.1%)
49 (3.1%)
22 (1.4%) |
| Physical‡
|
42 (12.1%) |
92 (11.7%) |
53 (12.1%) |
187 (11.9%) |
| Congenital |
20 (5.8%) |
11 (1.4%) |
5 (1.1%) |
36 (2.3%) |
| Varia and unknown |
46 (13.3%) |
87 (11.1%) |
42 (9.6%) |
175 (11.1%) |
| *Including systemic diseases with skin eruptions such as Henoch Schoenlein purpura, Kawasaki disease and other; parainfectious exanthemata were included as inflammatory reactions and not as viral infections. ‡e.g. scars, petechiae after vomiting/coughing, anal fissure due to constipation |
|
Table 3: The 20 most common skin diagnoses listed by frequency. |
|
Diagnosis
|
n = 1,572
|
| Viral and parainfectious exanthema
Respiratory tract infection
Varicella infection
Fever of unknown origin
Gastrointestinal infection
Roseola infantum (exanthema subitum)
Other
Hand-foot-mouth disease
Fifth disease (erythema infectiosum) |
276 (17.6%)
96
70
41
27
13
13
9
7 |
| Anogenital dermatitis
Irritant-toxic
Bacterial (including balanitis)
Candida infection
Oxyurasis |
121 (7.7%)
56
35
25
5 |
| Gingivostomatitis
Herpes simplex virus infection
Aphthosis
Candida infection
Enterovirus stomatitis (herpangina)
Other |
112 (7.1%)
55
27
21
5
4 |
| Petechiae
Parainfectious
Unknown
Physical cause (e.g. vomiting/coughing)
With thrombocytopenia |
100 (6.4%)
67
16
14
3 |
| Burns and scalds |
94 (6.0%) |
| Urticaria
Unknown trigger
With viral or bacterial infection
With food allergy |
79 (5.0%)
60
14
5 |
| Insect bites and associated inflammatory reactions |
79 (5.0%) |
| Scars |
64 (4.1%) |
| Rash of unknown cause |
60 (3.8%) |
| Cellulitis |
44 (2.8%) |
| Atopic dermatitis and seborrhoeic dermatitis |
42 (2.7%) |
| Xerosis cutis |
37 (2.4%) |
| Paronychium (ingrown nail) |
35 (2.2%) |
| Wound infection |
29 (1.8%) |
| Scarlet fever |
26 (1.7%) |
| Abscess |
24 (1.5%) |
| Impetigo contagiosa |
20 (1.3%) |
| Exanthema toxicum neonatorum |
15 (1.0%) |
| Haemangioma |
15 (1.0%) |
|
Table 4: Most common skin diagnoses listed by age groups and frequency. |
|
<1 year (n = 347)
|
1–6 years (n = 786)
|
>6 years (n = 439)
|
| Viral and parainfectious exanthema (27.4%) |
Viral and parainfectious exanthema (18.1%) |
Viral and parainfectious exanthema (8.9%) |
| Gingivostomatitis (8.1%) |
Anogenital dermatitis (9.9%) |
Petechiae (8.7%) |
| Burns and scalds (6.6%) |
Gingivostomatitis (9.0%) |
Insect bites (8.2%) |
| Rash of unknown cause (6.1%) |
Burns and scalds (7.6%) |
Scar (7.7%) |
| Atopic/seborrhoeic dermatitis (5.2%) |
Urticaria (6.1%) |
Anogenital dermatitis (5.7%) |
| Anogenital dermatitis (5.2%) |
Petechiae (5.9%) |
Wound infection (5.2%) |
| Petechiae (4.6%) |
Insect bites (5.1%) |
Urticaria (4.6%) |
| Exanthema toxicum neonat. (4.3%) |
Rash of unknown origin (4.2%) |
Cellulitis (4.3%) |
| Scar (3.7%) |
Cellulitis (2.9%) |
Paronychium (4.1%) |
Discussion
This study reveals a high incidence of skin disorders (17.4%) with a broad clinical spectrum in the PED of an Swiss urban university children’s hospital. Previous studies evaluating skin findings in PEDs reported an incidence of 4%–40%. However, if trauma-induced skin lesions are excluded from these studies the incidence falls to 4%–20%. [5–10]. Compared to these rates the incidence of skin lesions in our study remains high, even if burns are excluded (16.3%). The reported incidences probably vary with hospital size and facilities, seasonal influences and the data collection method. Whilst we thoroughly read every case note to identify all recorded skin findings, a computerised data search (with use of key words and ICD codes), together with a prospective setting with selection of only one diagnosis, are likely to result in under-reporting [7, 10]. We included as many skin lesions per patient as were found in the medical records, regardless of whether the dermatological finding prompted the PED visit or not. The lack of an open-access dermatology outpatient clinic in our hospital may also have increased the incidence of skin disorders seen in the PED. The high incidence of dermatological conditions in the PED correlates well with studies from paediatric consultancies and clinics reporting skin lesions in 11%–31% [1–4]. It is our observation that paediatricians in the community see a large number of skin diseases and many of them report difficulties in dealing with these conditions.
In accordance with previous studies we identified a broad spectrum of skin conditions of which the majority are of inflammatory/allergic (42.9%) and infectious (31.8%) nature [5, 7]. Viral and parainfectious exanthema followed by anogenital dermatitis and gingivostomatitis were the most common diagnoses seen in our PED. This differs from the dermatological disorders encountered in paediatric dermatology outpatient clinics. In these clinics more chronic conditions are seen, such as atopic dermatitis, warts and molluscum contagiosum, acne, melanocytic nevi, vitiligo, alopecia areata, psoriasis and haemangiomas [12–14]. There are very few data on the frequency with which skin conditions in the PED necessitate inpatient treatment. We observed a hospitalisation rate of 5.2%, which is slightly lower than the frequency of 8.2% reported by Kramkimel et al. [7]. Whilst outpatient management is appropriate for the majority of cases, some conditions may be severe (e.g. Kawasaki disease, Stevens-Johnson syndrome/toxic epidermal necrolysis, staphylococcal scalded skin syndrome, erysipelas, eczema herpeticatum) and require prompt diagnosis and admission and immediate treatment.
In a relatively high proportion (23.8%) of the dermatological findings in our study a diagnosis could only be suspected or remained unknown. According to the questionnaires, the paediatricians expressed their wish for a dermatological opinion in 24% and considered a dermatology review essential for the management of the patient in 16%. However, only 1% of the patients with skin findings were seen by a dermatologist. This discrepancy is probably due to the limited availability of the dermatologist at our hospital, but also reflects the high degree of autonomy of the PED doctors and the usually mild nature of the skin conditions encountered. However, with the limited availability of dermatologists and time that can be spent on a patient with a non-severe condition in a busy PED, a dermatological opinion is unfortunately not routinely sought for teaching reasons.
There are limitations to our study. The retrospective nature of this analysis includes potential bias since not all skin problems may have been effectively recorded. The diagnoses reported were usually clinically established by the PED doctors, and thus the diagnostic accuracy remains unknown. Particularly rare dermatological conditions may have been misdiagnosed and therefore missed. We did not evaluate the diagnostic concordance between paediatricians and dermatologists since a dermatological review was performed only in a minority of cases. Other studies have demonstrated a moderate rate of diagnostic concordance between paediatricians and dermatologists of 58%–66% [5, 6]. This highlights the importance of close collaboration between the two specialities in the PED if medical care for these patients is to be improved. In line with previous studies, our data demonstrate the need for improved training of PED doctors in dermatology, and highlights the importance of implementing paediatric dermatology as an integral part of the paediatric curriculum [5, 6]. At the same time dermatologists providing opinions at PEDs should be specifically trained in assessment of acute skin diseases in children. A possible solution is for residents to spend rotations in a paediatric dermatology clinic, including on-site teaching in a PED under the supervision of a paediatric dermatologist. The exchange of trainees between the departments can help to establish bridges of collaboration and may foster the development of curricula in paediatric dermatology to meet these educational needs. Another possibility is the creation of an open-access outpatient clinic for paediatric dermatology.
In summary, this study shows a high frequency and a broad spectrum of paediatric emergency skin conditions. Training for PED doctors should focus on inflammatory/allergic and infectious skin disorders, but also on recognition of potentially severe diseases. Our data underline the need to train paediatricians and dermatologists in the management of paediatric skin diseases and the importance of close collaboration between the two specialities for the benefit of these patients.
References
1 Fung W, Lo K. Prevalence of skin disease among school children and adolescents in a Student Health Service Center in Hong Kong. Pediatr Dermatol. 2000;17:440–6.
2 Hayden G. Skin diseases encountered in a pediatric clinic. A one-year prospective study. Am J Dis Child. 1985;139:36–8.
3 Largo R, Diethelm M, Kessler R, Suter FE. Prospective study of the work of the practising pediatrician. Helv Paediatr Acta Suppl. 1986;51:1–73.
4 Tunnessen WJ. A survey of skin disorders seen in pediatric general and dermatology clinics. Pediatr Dermatol. 1984;1:219–22.
5 Auvin S, Imiela A, Catteau B, Hue V, Martinot A. Paediatric skin disorders encountered in an emergency hospital facility: a prospective study. Acta Derm Venereol. 2004;84:451–4.
6 Dolan O, Bingham E, Glasgow J, Burrows D, Corbett JR. An audit of dermatology in a paediatric accident and emergency department. J Accid Emerg Med. 1994;11:158–61.
7 Kramkimel N, Soussan V, Beauchet A, Duhamel A, Saiag P, Mahé E. High frequency, diversity and severity of skin diseases in a paediatric emergency department. J Eur Acad Dermatol Venereol. 2010;24:1468–75.
8 Krauss B, Harakal T, Fleisher G. The spectrum and frequency of illness presenting to a pediatric emergency department. Pediatr Emerg Care. 1991;7:67–71.
9 Nelson D, Walsh K, Fleisher G. Spectrum and frequency of pediatric illness presenting to a general community hospital emergency department. Pediatrics. 1992;90:5–10.
10 Shivaram V, Christoph R, Hayden G. Skin disorders encountered in a pediatric emergency department. Pediatr Emerg Care. 1993;9:202–4.
11 Soriano-Hernández Y, Orozco-Covarrubias L, Tamayo-Sánchez L, Duràn-McKinster C, Sosa-de-Martinez C, Ruiz-Maldonado R. Exanthems in hospitalized pediatric patients: concordance between pediatric and dermatological diagnoses. Dermatology. 2002;204:273–6.
12 Nanda A, Al-Hasawi F, Alsaleh Q. A prospective survey of pediatric dermatology clinic patients in Kuwait: an analysis of 10,000 cases. Pediatr Dermatol. 1999;16:6–11.
13 Schachner L, Ling N, Press S. A statistical analysis of a pediatric dermatology clinic. Pediatr Dermatol 1983;1:157–64.
14 Wenk C, Itin P. Epidemiology of pediatric dermatology and allergology in the region of Aargau, Switzerland. Pediatr Dermatol. 2003;20:482–7.