Figure 1
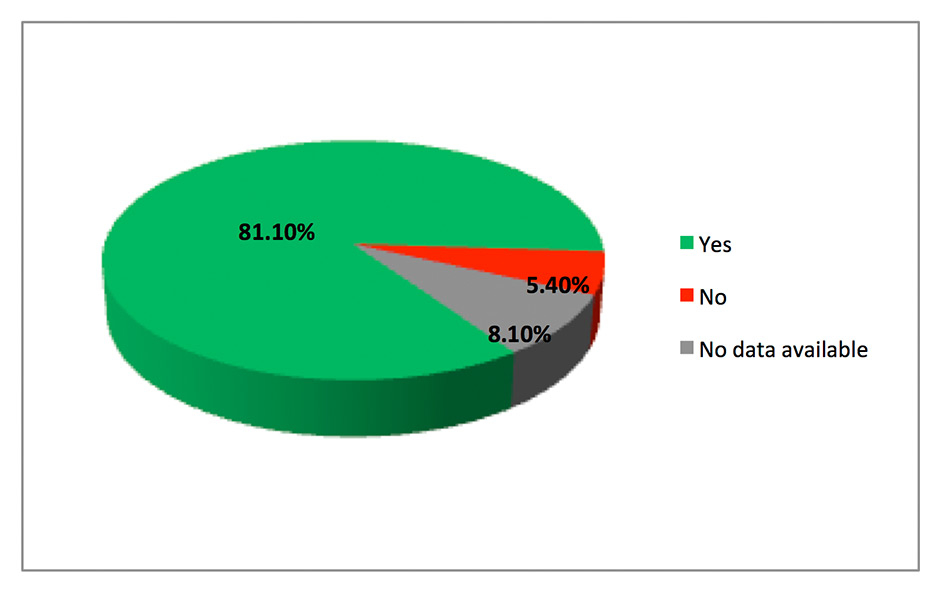
Post-surgical interview (females only): Would you opt for the chosen surgery again?
DOI: https://doi.org/10.4414/smw.2013.13888
Laparoscopic cholecystectomy (CC) was introduced into clinical practice in the mid-1980s [1] and is currently accepted as the standard of care. Recent advances in the field of interventional endoscopy and in laparoscopic surgery promise various benefits in terms of fewer wound complications, less pain, quicker convalescence and better cosmetic outcomes. One new area is natural orifice transluminal endoscopic surgery (NOTES). Pure NOTES implies entering the abdominal cavity via natural orifices with an endoscope avoiding any parietal incision [2, 3]. Various transgastric procedures (e.g., tubal ligation, cholecystectomy, gastrojejunostomy, splenectomy and oophorectomy) have been performed in animal models [4–8]. In humans, CC via pure NOTES has been performed through the vagina [9, 10]. To date, pure transgastric NOTES CC (transgastric NCC) has not been attempted in humans. Whether transgastric NCC achieves significant improvements in the clinical setting compared with standard laparoscopic cholecystectomy (SL-CC) is not yet clear. Hybrid NOTES is a combination of endoluminal access and transparietal assistance. Since 2007, rigid-hybrid transvaginal NOTES CC (tvNCC) has been evaluated worldwide [11–15].
Given the current stage of fast emerging innovative techniques, whether patients are willing to undergo pure NOTES procedures is of interest. Few data are available in the literature, with varying conclusions [16–20]. The aim of this prospective study was to analyse whether patients favour pure transgastric NCC and rigid-hybrid tvNCC over SL-CC. We also assessed an individual’s general risk-taking and perception of risk in order to characterise the type of patient who accepts or declines an innovative surgical procedure. We hypothesised that patients who choose innovative CC techniques are willing to accept greater risk, especially in the domain of health and safety, than patients who choose conventional CC.
The prospective interview-based single-centre survey was designed to assess patients’ opinions about two innovative surgical procedures for CC, pure transgastric NCC and rigid-hybrid tvNCC. Patients were admitted for elective SL-CC. The study was performed in a tertiary surgical centre in the eastern part of Switzerland with a service population of approximately 500,000 people. The study was approved by the local ethics committee.
From January 2009 to January 2010, all inpatients admitted for elective SL-CC were recruited as possible candidates prior to surgery. Inclusion criteria involved all female and male adult patients aged 18–85 years with symptomatic cholelithiasis being admitted for elective laparoscopic CC. Exclusion criteria were the following: acute cholecystitis, previous cholecystitis, known malignancy, hepatobiliary diseases other than biliary stones (e.g., benign stenosis of the biliary duct or liver cirrhosis), former open or laparoscopic abdominal surgery other than vaginal hysterectomy, oophorectomy, inguinal or femoral hernia repair, high perioperative risk (ASA III/IV), abnormal clotting time (international normalised ratio [INR] >1.4), low platelet count (<100,000/ml), pregnancy and missing informed consent. The entire assessment was performed by a single independent interviewer who was a fully trained physician not performing or involved in any surgical or endoscopic procedures. All baseline parameters were recorded in a prospective database.
All surgical techniques (i.e., SL-CC, transgastric NCC, and rigid-hybrid tvNCC [for females only]) were explained and illustrated by the interviewer with a standardised protocol using written and graphic material (Appendix 1). The potential advantages and disadvantages of each technique were discussed in a standardised manner as shown in Appendix 1. Regarding pure transgastric NCC, participants were informed that this type of surgery had not yet been undertaken in humans and that, therefore, potential advantages and disadvantages were theoretical. Furthermore, we stated that at the time of recruitment no studies of NOTES in humans were available to determine complication rates. Regarding rigid-hybrid tvNCC, female participants were informed that our hospital has been offering this surgery for CC since 2008 (worldwide evaluated since 2007). We explicitly stated that the presented collection of potential advantages and disadvantages covers the majority of information. The interviewer had a neutral view towards all procedures and recommended none of them. The complete survey was pilot-tested by the first author with a group of 15 healthy Swiss soldiers aged 19‒28 years on the basis of perception and feasibility.
The patients’ opinion of the techniques and their potential advantages and disadvantages was assessed per a standardised questionnaire based on a rating scale of 1 (not relevant) to 4 (relevant) (Appendix 2). The participant was then asked to decide which technique he/she would opt to undergo (males: SL-CC or transgastric NCC; females: SL-CC, transgastric NCC or rigid-hybrid tvNCC).
For a standardised assessment of a patient’s risk-taking and perception of risk, we used the validated 40-item Domain-Specific Risk Attitude Scale (DOSPERT) in German [21, 22] (Appendix 3) after the patient completed their assessment of the surgical techniques. The DOSPERT risk-taking subscale evaluates behavioural intentions, where the likelihood of respondents engaging in risky behaviours originating from five domains of life (ethical, financial, health/safety, social and recreational) is determined using a 5-point rating scale ranging from 1 (extremely unlikely) to 5 (extremely likely). Item ratings are added across all items of a given subscale to obtain subscale scores. Higher scores indicate greater risk-taking in the domain of the subscale. The risk-perception subscale evaluates the respondent’s gut-level assessment of how risky each behaviour is on a 5-point rating scale ranging from 1 (not at all) to 5 (extremely risky).
For categorical variables, data were described with absolute and relative frequencies. For continuous and ordinal variables, arithmetic means together with standard deviations and medians were given. Based on arithmetic means, rankings of ratings regarding advantages and disadvantages of surgical techniques were done in a descriptive way. Two-sided statistical significance testing was applied to compare measurements between males and females as well as between patients who would opt for innovative versus conventional techniques. Ratings regarding advantages and disadvantages as well as DOSPERT scales were compared between these patient groups using the Mann-Whitney U test. A p-value ≤0.05 was considered to indicate statistical significance.
From January 2009 to January 2010, 140 patients (54.3% females) were recruited, of whom 49 (35%) denied to participate in the study interview and 29 (20.7%) were excluded due to predefined exclusion criteria. A total of 60 patients (42.9%) concluded the first assessment, and three did not want to perform the risk behaviour assessment. Thus, a total of 57 patients (65% female, age 18–83 years, mean age 51.5 years) completed the study. Table 1 shows the baseline characteristics regarding the group of patients favouring SL-CC and the group of patients favouring innovative techniques (i.e., transgastric NCC and tvNCC).
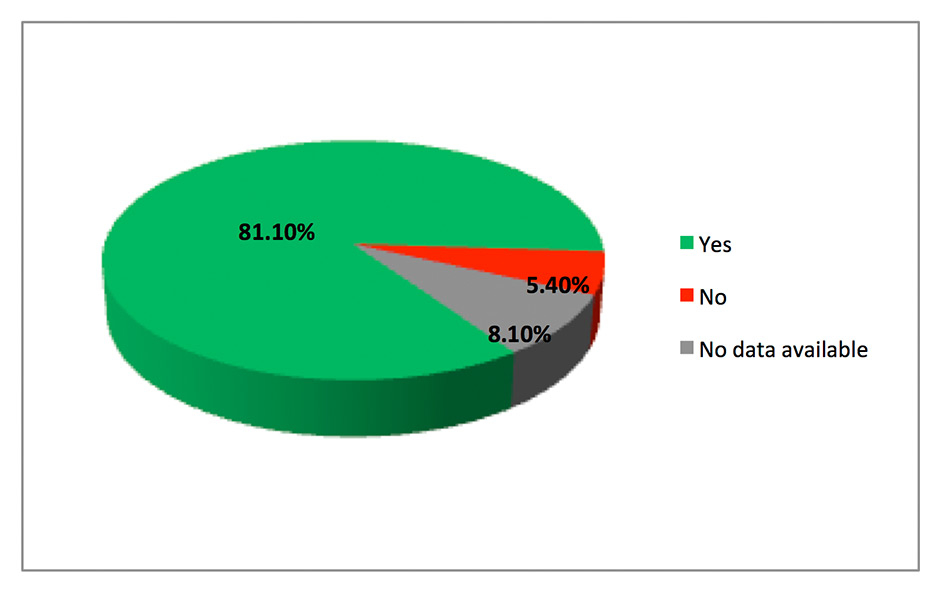
Figure 1
Post-surgical interview (females only): Would you opt for the chosen surgery again?
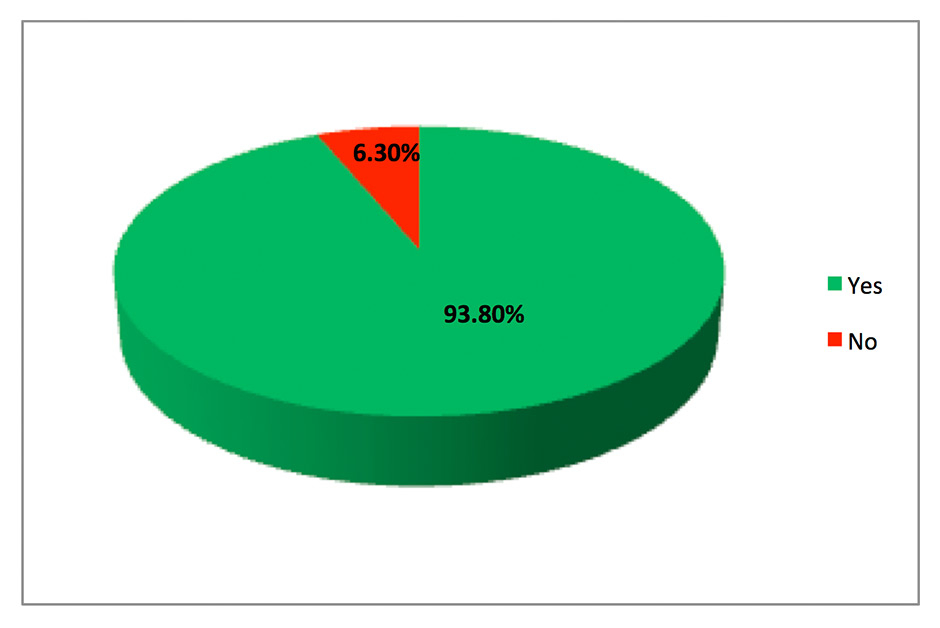
Figure 2
Post-surgical interview (females only): Would you recommend the chosen surgical procedure to your relatives and friends?
The number of males and females opting for each procedure is given in table 2. The ranking of each potential advantage of transgastric NCC and tvNCC is given in table 3. The most important potential advantage of transgastric NCC was “quicker convalescence”, and the least important potential advantage of transgastric NCC was “natural medicine”. “Scarless surgery” was ranked with a mean value of 2.56 (females: 2.68; males: 2.35) (table 3). The potential advantages “less pain”, “quicker convalescence”, “scarless surgery”, “no risk of abdominal hernia”, and “natural medicine” were rated significantly higher by patients with preference for innovative techniques compared than those patients with preference for SL-CC (table 3). The primary advantage of tvNCC was the reduction in hospital-acquired morbidity. “Quicker mobility”, “quicker convalescence”, “shorter hospital stay”, “fewer infections of the abdominal wall”, “no risk of abdominal hernia”, and “scarless surgery” were advantages which were graded significantly higher by females who opted for tvNCC than those who opted for SL-CC (table 3).
The ranking of potential disadvantages regarding transgastric NCC and tvNCC is shown in table 4. The potential risk of long-term injuries of the stomach was the most important disadvantage of transgastric NCC, followed by “lack of expertise”. The least important potential disadvantage of transgastric NCC was “intentional damage of a previously intact organ”. The primary disadvantage of tvNCC was the risk of vaginal/pelvic infection.
The phone interview with females after surgery (n = 19 SL-CC; n =14 rigid-hybrid tvNCC; n = 1 open CC; two females did not answer; one female did not undergo any surgery) revealed that the majority (81.1%) would choose the same technique again (fig. 1), and 93.8% of females would recommend the selected surgical procedure to their relatives and friends (fig. 2). The initial decision for the surgical technique of CC was changed by 15.6% of females during or after the preoperative interview with the operating surgeon (fig. 3).
Only risk-taking in the domain of recreation was significantly higher in the group of patients who opted for innovative techniques as compared with those who would opt for conventional CC (table 5). Risk-taking and perception of risk did not significantly differ in any of the other domains of life, or in the domain of health and safety (table 5).
| Table 1: Baseline characteristics regarding patient groups opting for standard SL-CC versus innovative techniques of CC. | ||||
| Patient characteristics | Participants opting for: | |||
| Standard SL-CC | Innovative techniques (tvNCC or transgastric NCC) | |||
| n | % | n | % | |
| Sex | ||||
| Female | 19 | 55.88% | 18 | 78.26% |
| Male | 15 | 44.12% | 5 | 21.74% |
| Age (graded) | ||||
| ≤ 60 years | 21 | 61.76% | 16 | 69.57% |
| > 61 years | 13 | 38.24% | 7 | 30.43% |
| BMI (graded) | ||||
| ≤ 25 | 12 | 35.29% | 8 | 36.36% |
| > 25.1 | 22 | 64.71% | 14 | 63.64% |
| Marital status | ||||
| Unmarried | 7 | 20.59% | 8 | 34.78% |
| Married | 24 | 70.59% | 12 | 52.17% |
| Divorced | 2 | 5.88% | 3 | 13.04% |
| Widowed | 1 | 2.94% | ||
| Children | ||||
| Without children | 8 | 23.53% | 9 | 39.13% |
| With children | 26 | 76.47% | 14 | 60.87% |
| Education | ||||
| Junior high school / failed graduation | 7 | 21.88% | 2 | 8.70% |
| Secondary school | 4 | 12.50% | 8 | 34.78% |
| High school / grammar school | 21 | 65.63% | 13 | 56.52% |
| Sportiness | ||||
| Not or slightly sporty | 29 | 85.29% | 19 | 82.61% |
| Sporty/very sporty | 5 | 14.71% | 4 | 17.39% |
| Occupational training | ||||
| Trainee | 4 | 11.76% | 1 | 4.35% |
| Completed training | 28 | 82.35% | 21 | 91.30% |
| University graduate | 2 | 5.88% | 1 | 4.35% |
| Ethnic background | ||||
| Northern Europe | 25 | 73.53% | 20 | 86.96% |
| Asia | 2 | 5.88% | ||
| Southern Europe | 7 | 20.59% | 3 | 13.04% |
| Afro-American | ||||
| Working capacity | ||||
| Working | 27 | 79.41% | 20 | 86.96% |
| Lost working capacity | ||||
| Unemployed | 1 | 2.94% | ||
| Retired | 6 | 17.65% | 3 | 13.04% |
| Denomination | ||||
| Catholic | 14 | 41.18% | 11 | 47.83% |
| Evangelic | 10 | 29.41% | 3 | 13.04% |
| Other | 5 | 14.71% | 5 | 21.74% |
| Atheist | 5 | 14.71% | 4 | 17.39% |
| Smoking status | ||||
| Nonsmoker | 27 | 79.41% | 15 | 68.18% |
| Former smoker | 3 | 8.82% | 3 | 13.64% |
| Smoker | 4 | 11.76% | 4 | 18.18% |
| Transgastric NCC = pure transgastric NOTES cholecystectomy; NOTES = natural orifice translumenal endoscopic surgery; SL-CC = standard laparoscopic cholecystectomy; tvNCC: rigid-hybrid transvaginal NOTES cholecystectomy | ||||
| Table 2: Patients’ choice of the technique of CC. | ||||
| Decision for: | Males | Females | ||
| N | % | N | % | |
| Transgastric NCC | 5 | 25% | 4 | 10.8% |
| TvNCC | na | na | 14 | 37.8% |
| SL-CC | 15 | 75% | 19 | 51.4% |
| NOTES = natural orifice translumenal endoscopic surgery; transgastric NCC = pure transgastric NOTES cholecystectomy; tvNCC = rigid-hybrid transvaginal NOTES cholecystectomy; SL-CC = standard laparoscopic cholecystectomy | ||||
| Table 3: Ranking of potential advantages of transgastric NCC and tvNCC. | ||||||
| Potential advantage of transgastric NCC | All (n = 57) | Females (n = 37) | Males (n = 20) | Group opting for SL-CC (n = 34) | Group opting for innovative techniques (n = 23) | |
| Mean | Mean | p-value | ||||
| Less pain | 2.67 | 2.81 | 2.40 | 2.44 | 3.00 | 0.021 |
| Quicker mobility | 3.14 | 3.14 | 3.15 | 2.94 | 3.43 | 0.077 |
| Quicker convalescence | 3.39 | 3.38 | 3.40 | 3.15 | 3.74 | 0.032 |
| Shorter hospital stay | 3.07 | 2.97 | 3.25 | 2.94 | 3.26 | 0.326 |
| Fewer hospitalisation induced complications (e.g., infections, deep vein thrombosis) | 3.23 | 3.19 | 3.30 | 3.06 | 3.48 | 0.067 |
| Fewer infections of abdominal wall | 3.26 | 3.35 | 3.10 | 3.09 | 3.52 | 0.092 |
| No risk of abdominal hernia | 2.81 | 2.92 | 2.60 | 2.50 | 3.26 | 0.007 |
| Fewer adhesions within abdominal cavity | 3.21 | 3.32 | 3.00 | 3.06 | 3.43 | 0.190 |
| Scarless surgery | 2.56 | 2.68 | 2.35 | 2.00 | 3.39 | 0.001 |
| Quicker resumption of work | 3.11 | 3.11 | 3.10 | 2.91 | 3.39 | 0.059 |
| “Natural medicine” (access by natural orifices) | 2.02 | 2.14 | 1.80 | 1.76 | 2.39 | 0.044 |
| Potential advantage of rigid-hybrid tvNCC | All females (n = 37) | Females opting for SL-CC (n = 19) | Females opting for tvNCC (N = 14) | |||
| Mean | Mean | p-value | ||||
| Less pain | 3.08 | 2.79 | 3.57 | 0.019 | ||
| Quicker mobility | 3.16 | 2.74 | 3.79 | 0.005 | ||
| Quicker convalescence | 3.30 | 3.00 | 3.79 | 0.042 | ||
| Shorter hospital stay | 3.16 | 2.84 | 3.71 | 0.011 | ||
| Fewer hospitalisation induced complications (e.g., infections, deep vein thrombosis) | 3.41 | 3.26 | 3.71 | 0.152 | ||
| Fewer infections of abdominal wall | 3.24 | 2.95 | 3.79 | 0.016 | ||
| No risk of abdominal hernia | 2.97 | 2.42 | 3.71 | 0.003 | ||
| Fewer adhesions within abdominal cavity | 3.27 | 3.11 | 3.64 | 0.174 | ||
| Scarless surgery | 2.68 | 1.95 | 3.57 | 0.001 | ||
| Quicker resumption of work | 3.16 | 2.95 | 3.57 | 0.065 | ||
| “Natural medicine” (access by natural orifices) | 2.08 | 1.89 | 2.29 | 0.553 | ||
| NOTES = natural orifice translumenal endoscopic surgery; transgastric NCC = pure transgastric NOTES cholecystectomy; tvNCC = rigid-hybrid transvaginal NOTES cholecystectomy; SL-CC = standard laparoscopic cholecystectomy Rating scale: 1 = No advantage at all; 2 = Small advantage, but not relevant for me to favour this surgical technique; 3 = Important advantage; 4 = Very important, clearly relevant for me to favour this surgical technique. | ||||||
| Table 4: Ranking of potential disadvantages of transgastric NCC, and rigid-hybrid tvNCC (females only), ranking between the group opting for standard technique and the group opting for each innovative technique (right). | |||||||
| Potential disadvantage of transgastric NCC | All (n = 57) | Females (n = 37) | Males (n = 20) | Group opting for SL-CC (n = 34) | Group opting for transgastric NCC (n = 9) | ||
| Mean | p-value | Mean | p-value | ||||
| Longer operation time | 2.49 | 2.43 | 2.60 | 0.544 | 2.82 | 1.67 | 0.005 |
| Risk of peritonitis due to damage of the stomach wall | 3.18 | 3.32 | 2.90 | 0.066 | 3.38 | 2.44 | 0.007 |
| Difficult healing of damaged stomach wall | 3.47 | 3.54 | 3.35 | 0.411 | 3.68 | 2.89 | 0.051 |
| Potential long-term damage of the stomach | 3.61 | 3.73 | 3.40 | 0.054 | 3.76 | 3.11 | 0.097 |
| Potential injury of vessels | 2.89 | 3.11 | 2.50 | 0.008 | 3.03 | 2.11 | 0.007 |
| Potential damage of the gut | 2.96 | 3.24 | 2.45 | 0.002 | 3.15 | 2.11 | 0.005 |
| Lack of expertise | 3.18 | 3.35 | 2.85 | 0.067 | 3.44 | 1.89 | 0.001 |
| Intentional damage of a previously intact organ | 1.63 | 1.59 | 1.70 | 0.532 | 1.82 | 1.11 | 0.067 |
| Potential disadvantage of rigid-hybrid tvNCC | Females only (n = 37) | Group opting for SL-CC (n = 19) | Group opting for tvNCC (n = 14) | ||||
| Mean | Mean | p-value | |||||
| Longer operation time | 2.16 | 2.53 | 1.86 | 0.065 | |||
| Risk of vaginal infection by intentional injury of the posterior vaginal wall | 3.14 | 3.63 | 2.43 | 0.001 | |||
| Difficult healing of vagina | 3.05 | 3.47 | 2.43 | 0.006 | |||
| Possible damage to sexual function | 2.97 | 3.32 | 2.43 | 0.035 | |||
| Lack of expertise with associated technical failure and complications | 2.76 | 3.37 | 2.07 | <0.001 | |||
| Intentional damage of a previously intact organ | 1.46 | 1.74 | 1.14 | 0.142 | |||
| NOTES = natural orifice translumenal endoscopic surgery; transgastric NCC = pure transgastric NOTES cholecystectomy; tvNCC = rigid-hybrid transvaginal NOTES cholecystectomy; SL-CC = standard laparoscopic cholecystectomy Rating scale: 1 = No disadvantage at all; 2 = Small disadvantage, but not relevant for me to favour this surgical technique; 3 = Important disadvantage; 4 = Very important, clearly relevant for me to decline this surgical technique. | |||||||
| Table 5: Risk behaviour analysis according to the DOSPERT score (risk perception and risk taking), shown for patients opting for standard SL-CC (left) and for patients opting for innovative techniques of CC (right). | |||||||
| Risk perception subscales | Patients opting for SL-CC (n = 34) | Patients opting for innovative techniques (n = 23) | |||||
| Mean | Median | SD | Mean | Median | SD | p-value | |
| Social | 19.35 | 19.50 | 5.31 | 19.74 | 20.00 | 3.89 | 0.85 |
| Recreational | 34.38 | 35.50 | 5.25 | 33.30 | 35.00 | 5.78 | 0.45 |
| Gambling | 16.03 | 16.00 | 3.25 | 15.70 | 16.00 | 3.50 | 0.81 |
| Health and Safety | 33.50 | 34.00 | 4.36 | 33.74 | 35.00 | 5.25 | 0.70 |
| Ethical | 32.94 | 33.00 | 5.48 | 33.26 | 36.00 | 6.28 | 0.72 |
| Investment | 15.12 | 16.00 | 3.52 | 14.22 | 15.00 | 3.38 | 0.32 |
| Financial (investment and gambling) | 31.15 | 32.00 | 5.91 | 29.91 | 32.00 | 6.47 | 0.63 |
| Risk taking subscales | |||||||
| Mean | Median | SD | Mean | Median | SD | p-value | |
| Social | 25.21 | 24.50 | 4.49 | 27.00 | 26.00 | 4.46 | 0.17 |
| Recreational | 12.59 | 11.50 | 4.55 | 14.70 | 13.00 | 4.74 | 0.05 |
| Gambling | 6.00 | 4.50 | 3.22 | 5.39 | 5.00 | 1.44 | 0.75 |
| Health and safety | 13.38 | 12.00 | 5.34 | 14.00 | 14.00 | 4.58 | 0.47 |
| Ethical | 11.38 | 10.00 | 4.21 | 11.83 | 10.00 | 4.03 | 0.61 |
| Investment | 6.97 | 5.50 | 3.72 | 7.00 | 7.00 | 2.52 | 0.53 |
| Financial (investment and gambling) | 12.97 | 10.50 | 5.92 | 12.39 | 12.00 | 3.30 | 0.70 |
| CC = cholecystectomy; SD = standard deviation; SL-CC = standard laparoscopic cholecystectomy | |||||||
Few data are currently available regarding patients’ perceptions of innovative NOTES surgery [16–20]. The study designs (e.g., composition of study participants, concept of questionnaires and selection of compared surgical techniques) were often different, making it difficult to compare studies. The strength of our study was its ability to recreate real-life situations for patients as best as possible. We selected CC as surgical intervention as one of the most frequent interventions in abdominal surgery. Patients admitted exclusively for elective SL-CC were recruited intentionally. In this setting, patients were considered more likely to be interested in understanding their surgery and also the variety of technical alternatives. We excluded patients with acute cholecystitis, because emergency situations are often associated with uncertainty and anxiety, thus limiting the value of a questionnaire and a complex risk behaviour assessment.
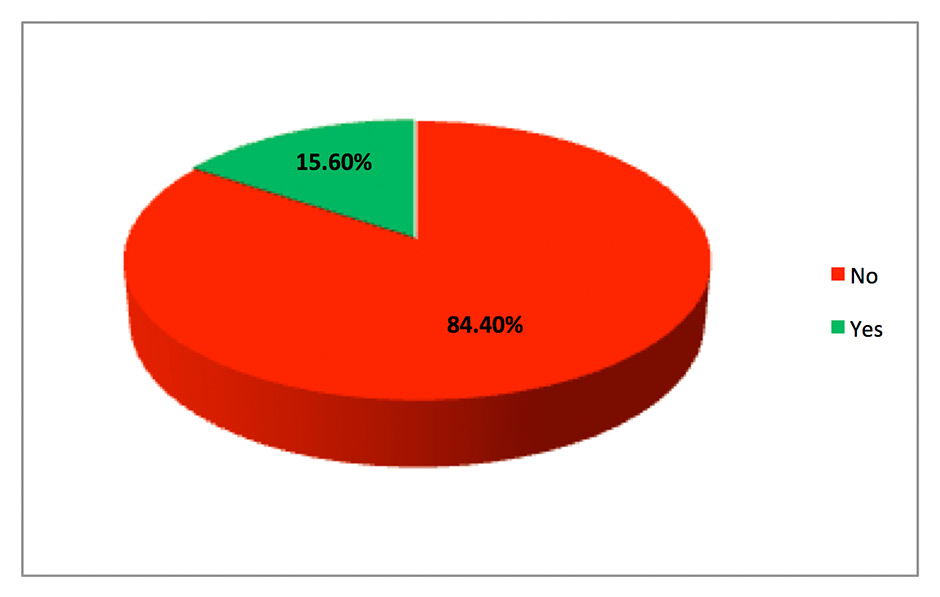
Figure 3
Post-surgical interview (females only): Was the initial decision changed after the pre-operative interview with the operating surgeon?
Our study revealed that half of female patients still prefered the standard laparoscopic CC, whereas 38% of females opted for rigid-hybrid NCC. Transgastric NCC was rarely accepted by females. However, 25% of men stated that they would accept transgastric NCC as an unproven surgical procedure. Rao et al. [23] reported similar results regarding patients’ preferences towards appendectomy via NOTES compared to single port, laparoscopic, and open surgery, based on a hypothetical scenario of acute appendicitis. This study showed that NOTES was the least preferred and single port surgery the most popular method, followed by conventional laparoscopy. Although NOTES appendectomy was not preferred, considering the overall preference for the route of NOTES in the whole study population, the oral route was the most popular (37.1%; vaginal route only 3.8%) [23]. However, in our study 37.8% of females opted for rigid-hybrid transvaginal NCC. Notably, the safety and feasibility study of rigid-hybrid tvNCC by our surgical colleagues revealed an acceptance rate of 85% [13]. This significant difference could be explained by possible interview bias (i.e., surgeon’s emphasis regarding the choice of an operative technique). It may be argued that 84.4% of females in our study stated that their initial decision remained unchanged after the preoperative interview with the operating surgeon.
Other investigators have shown a preference towards NOTES (68% of women and 78% of men and women) [16, 17]. Our study compared patients’ perceptions of transgastric NCC and rigid-hybrid tvNCC; whereas pure transgastric NOTES is not yet established in the clinical setting, rigid-hybrid tvNCC has been evaluated clinically and is currently offered to women worldwide. Our hospital has been offering the option of tvNCC since 2008, reporting a large case volume in this field [13]. A possible reason for the different observations here is that women in our study could choose from these innovative surgical options and favoured the technique, which has already being evaluated for potential advantages over pure transgastric NCC. Women in other studies [16, 17] might have opted for the hybrid procedure (tvNCC) if it was an available technical alternative to pure NOTES procedures.
Our ranking analysis of the potential advantages of tvNCC and transgastric NCC revealed that scarless surgery was not particularly important for patient perception, a finding which is consistent with several other NOTES studies [17, 19, 20]. From the patient’s perspective, the most relevant potential advantages of transgastric NCC are quicker convalescence, and fewer hospitalisation-induced complications and quicker convalescence for tvNCC. Similar results were obtained by the surveys mentioned above [17, 19, 20].
Similar to the present study, Peterson et al. [17] found that women were mainly concerned with infection issues (83%) and the impact of transvaginal NOTES surgery on a healthy sex life (81%). Bucher et al. [24] showed that 96% of females had worries regarding transvaginal access, including dyspareunia (68%) or decreased sensitivity during intercourse (43%). These aspects seem to hinder women from opting for minimally invasive surgery through the vaginal route. However, Linke et al. [13, 25] showed that dyspareunia is even less frequent after tvNCC than before surgery, and vaginal infections were not significantly more frequent.
Our findings point out that, in regard to transgastric NCC, patients are mainly concerned about delayed healing of the stomach wall and long-term stomach problems. Although pure transgastric NCC is not yet performed in humans, a few publications from North America have looked at staging, access, and insufflation in transgastric NOTES protocols [26–29]. Recently, Nau et al. [30] concluded from a retrospective review that transgastric pure NOTES is a safe alternative for accessing the peritoneal cavity in humans, and the risk of bacterial contamination secondary to peroral and transgastric access is clinically insignificant. Knowing the fears of patients regarding transgastric NCC and the recently published data about safety and feasibility of transgastric access should improve the quality of pre-surgical interviews. However long-term results are not available which makes it difficult to address patients’ fear without improved evidence.
To the best of our knowledge, this is the first study assessing patients’ perceptions of innovative minimally invasive surgery and general risk-taking behaviours in combination. The strength of the validated and widely used DOSPERT scale is that it involves different domains of life for risk assessment – an important issue because individuals have not shown themselves to consistently seek risk across different domains and situations [21, 22, 31, 32]. In our study, only the risk-taking subscale of recreation showed a significant difference between participants who opted for innovative/experimental surgical techniques and those who opted for standard surgery. Thus, the group of patients who opted for one of the innovative techniques in our survey exhibited greater risk-taking in the recreational domain of life than those who opted for the standard technique. This finding is not unexpected. However, clinicians who feel responsible for their patients need to be aware of the different temperaments of patients to protect them from taking unnecessary risks regarding medical decisions. No significant difference was found regarding risk-taking in the domain of health and safety.
The main limitation of this study is the relatively small sample size compared to other survey studies [16, 17, 19, 20]. The reason for the small sample size may have been the fairly long interview time in addition to the pre-surgical examination and interview by the anaesthetist and surgeon. In addition, the exclusion rate was high (20.7%), mainly because we aimed to imitate the potential clinical settings for pure NOTES procedures as much as possible. Moreover, our surgical colleagues performed a feasibility and safety study of rigid-hybrid tvNCC (9/2008-9/2009). This situation reduced the number of female elective CC patients being recruited into our survey study. We did not recruit females who already underwent a pre-surgical interview prior to our study inclusion, which significantly delayed the inclusion of female patients.
In conclusion, the results of this study indicate that transgastric NCC is rarely accepted by females but accepted by 25% of males. Females consider the minimally invasive nature of rigid-hybrid tvNCC and the standard laparoscopic SL-CC to be attractive. Regarding rigid-hybrid tvNCC, females were mainly concerned about infection and the impact of the procedure on a healthy sex life. These aspects seem to hinder women from opting for minimally invasive surgery through the vaginal route. Thus, explaining recent safety data on tvNCC could reduce a woman’s fear and improve further their perception. Regarding transgastric NCC, patients were concerned mainly about delayed healing of the stomach wall and long-term stomach problems. This issue should be taken seriously but is so far not answered sufficiently by controlled studies.
The patient is asked to assess each of the following 11 potential advantages of transgastric NCC on a rating scale of 1‒4:
1 = “no advantage at all”; 2 = “small advantage, but not relevant for me to favour this surgical procedure”; 3 = ”important advantage”; 4 = “very important, clearly relevant for me to favour this surgical procedure”.
The patient is asked to assess each of the following 8 potential disadvantages on a rating scale of 1‒4:
1 = “no disadvantage at all”; 2 = “small disadvantage, but not relevant for me to decline this surgical procedure for cholecystectomy”; 3 = ”important disadvantage”; 4 = “very important disadvantage, clearly relevant for me to decline this surgical procedure”.
The female patient is asked to assess each of the following 11 potential advantages of tvNCC on a rating scale of 1‒4:
1 = “no advantage at all”; 2 = “small advantage, but not relevant for me to favour this surgical procedure”; 3 = ”important advantage”; 4 = “very important, clearly relevant for me to favour this surgical procedure”.
The female patient is asked to assess each of the following 6 potential disadvantages of tvNCC on a rating scale of 1‒4:
1 = “no disadvantage at all”; 2 = “small disadvantage, but not relevant for me to decline this surgical procedure for cholecystectomy”; 3 = ”important disadvantage”; 4 = “very important disadvantage, clearly relevant for me to decline this surgical procedure”.
For males: What is the main reason for you to undergo transgastric NCC?
For females: What is the main reason for you to undergo transgastric NCC, tvNCC, or SL-CC?
Assuming that transgastric NOTES would be a cholecystectomy technique within a controlled trial as an alternative to the standard cholecystectomy, which method would you prefer?
The rigid-hybrid NCC is currently offered in our hospital. Transgastric NOTES cholecystectomy has been performed in animal trials only. Assuming that transgastric NOTES would be a cholecystectomy technique within a controlled trial as an alternative to the standard cholecystectomy, which method would you prefer?
For each of the following statements, please indicate the likelihood that you would engage in the described activity or behaviour if you were to find yourself in that situation. Provide a rating from Extremely Unlikely to Extremely Likely using the following scale:
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Extremely | Moderately | Somewhat | Not Sure | Somewhat | Moderately | Extremely |
| Unlikely | Unlikely | Unlikely | Likely | Likely | Likely |
People often see some risk in situations that contain uncertainty about what the outcome or consequences will be and for which there is the possibility of negative consequences. However, riskiness is a very personal and intuitive notion, and we are interested in your gut level assessment of how risky each situation or behaviour is.
For each of the following statements, please indicate how risky you perceive each situation. Provide a rating from Not at All Risky to Extremely Risky, using the following scale:
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Not at All | Slightly | Somewhat | Moderately | Risky | Very | Extremely |
| Risky | Risky | Risky | Risky | Risky | Risky |
The 40 items are as follows:
1. Admitting that your tastes are different from those of your friends. (S)
2. Going camping in the wilderness beyond the civilization of a campground. (R)
3. Betting a day’s income at the horse races. (G)
4. Buying an illegal drug for your own use. (H)
5. Cheating on an exam. (E)
6. Chasing a tornado or hurricane by car to take dramatic photos. (R)
7. Investing 10% of your annual income in a moderate growth mutual fund. (I)
8. Consuming five or more servings of alcohol in a single evening. (H)
9. Cheating by a significant amount on your income tax return. (E)
10. Disagreeing with your father on a major issue. (S)
11. Betting a day’s income at a high stake poker game. (G)
12. Having an affair with a married man or woman. (E)
13. Forging somebody’s signature. (E)
14. Passing off somebody else’s work as your own. (E)
15. Going on a vacation in a third-world country without prearranged travel and hotel accommodations. (R)
16. Arguing with a friend about an issue on which he or she has a very different opinion. (S)
17. Going down a ski run that is beyond your ability or closed. (R)
18. Investing 5% of your annual income in a very speculative stock. (I)
19. Approaching your boss to ask for a raise. (S)
20. Illegally copying a piece of software. (E)
21. Going whitewater rafting during rapid water flows in the spring. (R)
22. Betting a day’s income on the outcome of a sporting event (e.g., baseball, soccer, or football). (G)
23. Telling a friend if his or her significant other has made a pass at you. (S)
24. Investing 5% of your annual income in a conservative stock. (I)
25. Shoplifting a small item (e.g., lipstick or a pen). (E)
26. Wearing provocative or unconventional clothes on occasion. (S)
27. Engaging in unprotected sex. (H)
28. Stealing an additional TV cable connection off the one you pay for. (E)
29. Not wearing a seatbelt as a passenger in the front seat. (H)
30. Investing 10% of your annual income in government bonds (treasury bills). (I)
31. Periodically engaging in a dangerous sport (e.g., mountain climbing or sky diving). (R)
32. Not wearing a helmet when riding a motorcycle. (H)
33. Gambling a week’s income at a casino. (G)
34. Taking a job that you enjoy over one that is prestigious but less enjoyable. (S)
35. Defending an unpopular issue that you believe in at a social occasion. (S)
36. Exposing yourself to the sun without using sunscreen. (H)
37. Trying out bungee jumping at least once. (R)
38. Piloting your own small plane, if you could. (R)
39. Walking home alone at night in a somewhat unsafe area of town. (H)
40. Regularly eating high cholesterol foods. (H)
Note: E = ethical, I = investment, G = gambling, H = health/safety, R = recreational, and S = social.
Acknowledgments:We acknowledge Elke U. Weber’s support regarding the DOSPERT analysis (Jerome A. Chazen Professor of International Business, Co-Director, Centre for Research On Environmental Decisions and Centre for Decision Sciences, Columbia University, New York, United States). We also acknowledge Hanno Ulmer for professional support as a statistician (Head of Department of Medical Statistics, Informatics and Health Economics, Innsbruck Medical University, Innsbruck, Austria). We appreciate the logistic support of the surgical secretaries Mrs Leena Lüthi and Mrs Esther Koller.
1 Reynolds W Jr. The first laparoscopic cholecystectomy. JSLS. 2001;1:89–94.
2 Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions. Gastrointest Endosc. 2004;60:114–7.
3 Pai RD, Fong DG, Bundga ME, Odze RD, Rattner DW, Thompson CC. Transcolonic endoscopic cholecystectomy: a NOTES survival study in a porcine model (with video). Gastrointest Endosc. 2006;64:428–34.
4 Jagannath SB, Kantsevoy SV, Vaughn CA, Chung SSC, Cotton PB, Gostout CJ, et al. Peroral transgastric enscopic ligation of fallopian tubes with long-term survival in a porcine model. Gastrointest Endosc. 2005;61:449–53.
5 Park PO, Bergström M, Ikeda K, Fritscher-Ravens A, Swain P. Experimental studies of transgastric gallbladder surgery: cholecystectomy and cholecystogastric anastomosis. Gastrointest Endosc. 2005;61:601–6.
6 Kantsevoy SV, Jagannath SB, Nijyama H, Vaughn CA, Chung SSC, Cotton PB, et al. Endoscopic gastrojejunostomy with survival in a porcine model. Gastrointest Endosc. 2005;62:287–92.
7 Kantsevoy SV, Hu B, Jagannath SB, Vaughn CA, Beitler DM, Chung SS, et al. Transgastric endoscopic splenectomy: is it possible? Surg Endosc. 2006;20:522–5.
8 Wagh MS, Merrifield BF, Thompson CC. Survival studies after endoscopic transgastric oophorectomy and tubectomy in a porcine model. Gastrointest Endosc. 2006;63:473–8.
9 Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007;142:823–6.
10 Zorrón R, Maggioni LC, Pombo L, Oliveira AL, Carvhalo GL, Filgueiras M. NOTES transvaginal cholecystectomy: preliminary clinical application. Surg Endosc. 2008;22:542–7.
11 Zornig C, Mofid H, Emmermann A, Alm M, von Waldenfels HA, Felixmuller C. Scarless cholecystectomy with combined transvaginal and transumbilical approach in a series of 20 patients. Surg Endosc. 2008;22:1427–9.
12 Burghardt J, Federlein M, Elling D, Gellert K, Borchert D. Transvaginale Cholezystektomie – die Etablierung und Nutzung eines neuen Zugangs zur Bauchhöhle für die Viszeralchirurgie. CHAZ. 2008;923–6.
13 Linke GR, Tarantino I, Hoetzel R, Warschkow R, Lange J, Lachat R, et al. Rigid-hybrid transvaginal NOTES cholecystectomy: evaluation in routine clinical practise. Endoscopy. 2010;42:571–5.
14 Arezzo A, Zornig C, Mofid H, Fuchs KH, Breithaupt W, Noguera J, et al. The EURO-NOTES clinical registry for natural orifice transluminal endoscopic surgery: a 2-year activity report. Surg Endosc. 2013; Mar 22. [Epub ahead of print]
15 Demetrios NM, Konstantinos JB, Eleftherios IM, Efstathios LP, Athanasios SP, Alexandros EP. Surgery via natural orifices in human beings: yesterday, today, tomorrow. Am J Surg. 2012;204:93–102.
16 Varadarajulu S, Tamhane A, Drelichman ER. Patient perception of natural orifice transluminal endoscopic surgery as a technique for cholecystectomy. Gastrointest Endosc. 2008;67:854–60.
17 Peterson CY, Ramamoorthy S, Andrews B, Horgan S, Talamini M, Chock A. Women’s positive perception of transvaginal NOTES surgery. Surg Endosc. 2009;23:1770–4.
18 Hagen ME, Wagner OJ, Christen D, Morel P. Cosmetic issues of abdominal surgery: results of an enquiry into possible grounds for a natural orifice transluminal endoscopic surgery (NOTES) approach. Endoscopy. 2008;40:581–3.
19 Strickland AD, Norwood MG, Behnia-Willison F, Olakkengil SA, Hewett PJ. Transvaginal natural orifice translumenal endoscopic surgery (NOTES): a survey of women’s views on a new technique. Surg Endosc. 2010;24:2424–31.
20 Swanstrom LL, Volckmann E, Hungness E, Soper NJ. Patient attitudes and expectations regarding natural orifice translumenal endoscopic surgery. Surg Endosc. 2009;23:1519–25.
21 Johnson JG, Wilke A, Weber EU. Beyond a trait view of risk-taking: a domain-specific scale measuring risk perceptions, expected benefits, and perceived-risk attitude in German-speaking populations. Polish Psychological Bulletin. 2004;35:153–63.
22 Weber EU, Blais A-R, Betz NE. A domain-specific risk-attitude scale: measuring risk perceptions and risk behaviours. J Behav Dec Making. 2002;15:263–90.
23 Rao A, Kynaston J, MacDonald ER, Ahmed I. Patient preferences for surgical techniques: should we invest in new approaches? Surg Endosc. 2010;24:3016–25.
24 Bucher P, Ostermann S, Pugin F, Morel P. Female population perception of conventional laparoscopy, transumbilical LESS, and transvaginal NOTES for cholecystectomy. Surg Endosc. 2011;25:2308–15.
25 Linke GR, Luz S, Janczak J, Zerz A, Schmied BM, Siercks I, et al. Evaluation of sexual function in sexually active women 1 year after transvaginal NOTES: a prospective cohort study of 106 patients. Langenbecks Arch Surg. 2013;398:139–45.
26 Nau P, Ellison EC, Muscarella P Jr, Mikami D, Narula VK, Needleman B, et al. A review of 130 humans enrolled in transgastric NOTES protocols at a single institution. Surg Endosc. 2011;25:1004–11.
27 Hazey JW, Narula VK, Renton DB, Reavis KM, Paul CM, Hinshaw KE, et al. Natural-orifice transgastric endoscopic peritoneoscopy in humans: initial clinical trial. Surg Endosc. 2008;22:16–20.
28 Nau P, Anderson J, Yuh B, Muscarella P Jr, Ellison EC, Happel L, et al. Diagnostic transgastric endoscopic peritoneoscopy: extension of the initial human trial for staging of pancreatic head masses. Surg Endosc. 2010;24:1440–6.
29 Nau P, Anderson J, Needleman B, Ellison EC, Melvin WS, Hazey JW. Endoscopic peritoneal access and insufflation: natural orifice transluminal endoscopic surgery. Gastrointest Endosc. 2010;71:485–9.
30 Nau P, Anderson J, Happel L, Yuh B, Narula VK, Needleman B, et al. Safe alternative transgastric peritoneal access in humans: NOTES. Surgery. 2011;149:147–52.
31 Blais AR, Weber EU. A Domain-Specific Risk-Taking (DOSPERT) scale for adult populations. Judgm Decis Mak. 2006;1:33–47.
32 Harrison JD, Young JM, Butow P, Salkeld G, Solomon MJ. Is it worth the risk? A systematic review of instruments that measure risk propensity for use in the health setting. Soc Sci Med. 2005;60:1385–96.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.