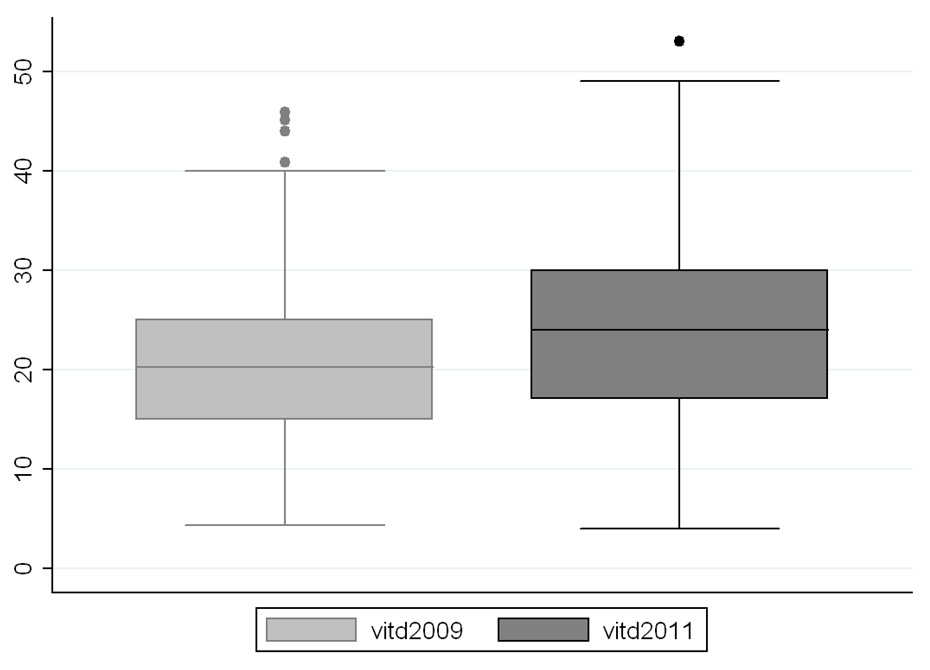
Figure 1
Mean 25-OH vitamin D (in ng/ml) in 2009 and 2011, p = 0.0001
DOI: https://doi.org/10.4414/smw.2013.13891
Vitamin D is an important factor for bone metabolism and neuromuscular function [1]. Vitamin D supplementation is effective in lowering the risk of fall and fracture in elderly subjects [2, 3]. Some experts recommend a level higher than 30 ng/ml (75 nmol/l) for high-risk patients [4–6]. There is an overall consensus among scientific organisations that levels higher than 20 ng/ml (50 nmol/l) are necessary for bone and muscular health [7–9]. Old and recent studies have already shown a high prevalence of hypovitaminosis D in Switzerland [10, 11], and a few studies have also underlined this problem among rheumatology outpatients [12, 13]. We have shown that hypovitaminosis D was highly prevalent in an outpatient population of Swiss rheumatology patients, affecting 86% of subjects in 2009 [14]. This situation could be explained by different causes: lack of sufficient sunshine, sun avoidance in older patients or patients with photosensitivity, inadequate clinician and patient information, infrequent screening and suboptimal adherence to daily substitution or insufficient supplementation. Therefore we aimed to evaluate the evolution of vitamin D status in the same outpatient rheumatology population two years later, after the results of the first study were widely disseminated to local physicians and patients, to determine the evolution of the problem and the impact of physician information.
We evaluated the prevalence of hypovitaminosis D in an outpatient population attending the rheumatology clinic of the University Hospital of Lausanne in November 2009 [14]. Between November 2009 and October 2011, we informed and sensitised local physicians about the risks and the management of hypovitaminosis D and presented results of this first study. Next, we repeated the same screening in November 2011. All patients in our rheumatology clinic were offered a screening test for 25-OH vitamin D. The results were categorised as: deficient (<10 ng/ml or <25 nmol/l), insufficient (10 to 30 ng/ml or 25 to 75 nmol/l) or normal (>30 ng/ml or >75 nmol/l). We also used the more recently recommended cut-off of 20 ng/ml (50 nmol/l) and revaluate the 2011 and 2009 populations with it.
Vitamin D levels were determined using radioimmunological assay with extraction (25-hydroxyvitamin D 125I RIA Kit, DiaSorin®).
Patients were asked about their calcium and vitamin D supplementation. We compared the results with those of November 2009 after exclusion of patients who were not regularly followed in our clinic and those who received a high dose (300,000 IU) of oral or intramuscular vitamin D in the previous six months in both screening populations.
We asked the central laboratory and pharmacy of our university hospital about the evolution of 25-OH vitamin D dosages and vitamin D3 prescriptions between 2008 and 2011. Finally, to try and determine the impact of local physician education, we evaluated the number of publications on vitamin D in the three most important Swiss medical journals of the French speaking part of Switzerland. We searched for publications with the word "vitamin D" in Swiss Medical Weekly, Swiss Medical Forum and La Revue Médicale de la Suisse Romande.
We tested for normal distribution of the results by Shapiro-Wilk and Shapiro-Francia tests for normality. All results were normally distributed. To compare proportions, we performed a Chi square test. To compare vitamin D level between the two unpaired samples, we performed a t-test for unpaired measurement. A p-value <0.05 was considered significant.
A total of 336 patients were screened in 2011. We excluded 37 patients who received a high dose of vitamin D in the six months preceding the study and 60 patients who were not regularly followed up in our clinic between 2009 and 2011. We then analysed the results of the 239 remaining patients, compared with 230 patients in 2009 using the same exclusion criteria.
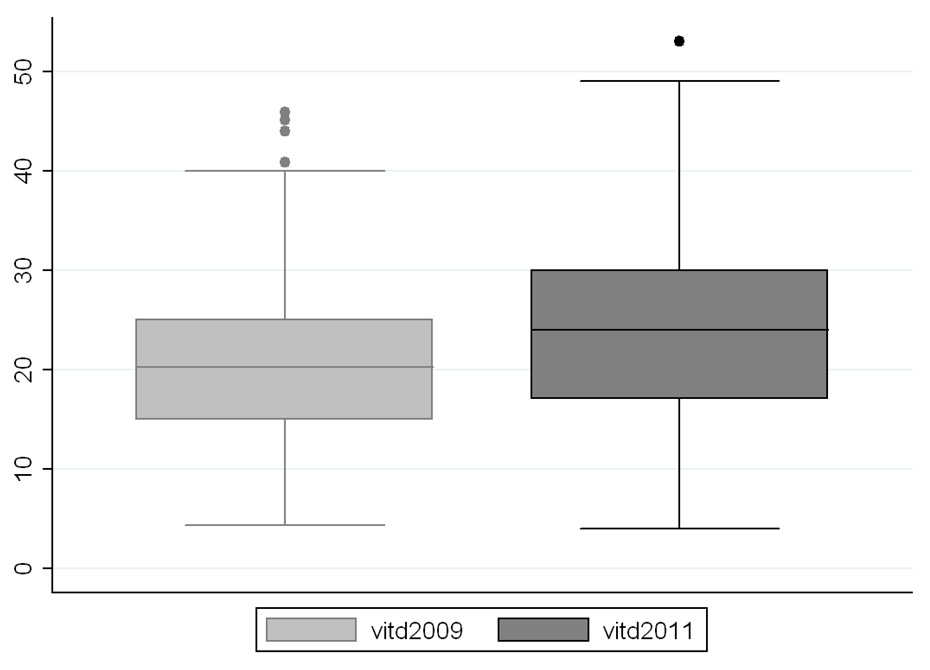
Figure 1
Mean 25-OH vitamin D (in ng/ml) in 2009 and 2011, p = 0.0001
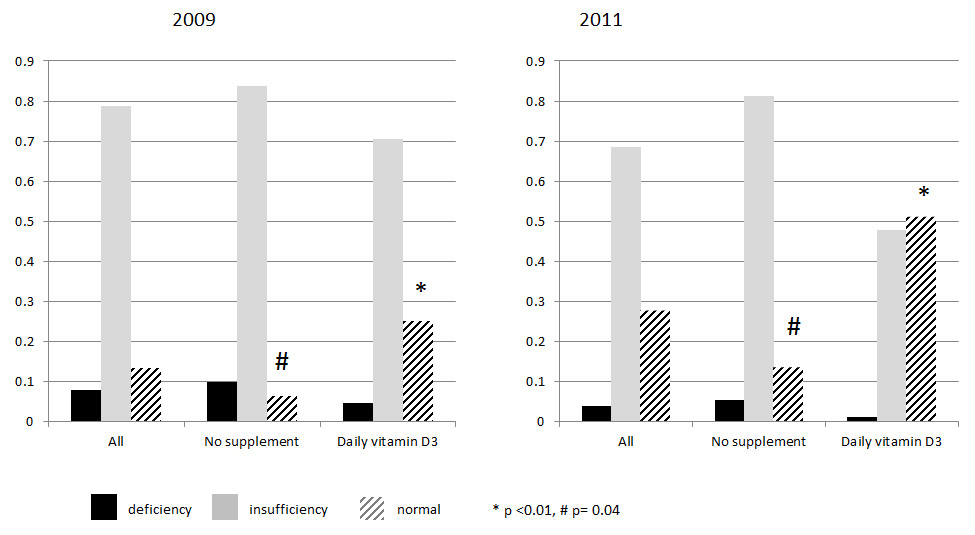
Figure 2
Effects of vitamin D3 supplementation: X-axis: 3 groups: all patients, nonsupplemented patients and patients with daily supplement of vitamin D3; Y-axis: percentage of patients with deficiency, insufficiency or normal results (1 = 100%); * and #: comparison between 2009 and 2011, the number of patients with normal results being significantly higher in 2011
In 2011, 173 patients had inflammatory rheumatic disease (essentially rheumatoid arthritis or spondylarthropathy), 65 had osteoporosis and 26 had degenerative disease compared with 200, 33 and 23 patients, respectively, in 2009 (nonexclusive categories).
As far as body mass index (BMI) and sex were concerned, there was no significant difference between the two populations: BMI was 26.2 kg/m2 in 2009 versus 26.5 kg/m2 in 2011 and 70% of patients were women in 2009 and in 2011. Nevertheless, the population was significantly older in 2011 (age 51.9 vs 55.9 year old, p <0.01). Only 48 patients (20%) were the same in 2009 and 2011.
Mean vitamin D levels in 2009 and 2011 are summarised in table 1. In 2011, it was 23.8 ng/ml, range 4–53 ng/ml (20.8 ng/ml in 2009, p = 0.0001, fig. 1). Nine patients (4%) had vitamin D deficiency (18 [8%] in 2009), 163 patients (68%) had insufficiency (181 [79%] in 2009) and 66 patients (28%) had normal results (31 [13%] in 2009). Ninety patients (38%) were on daily oral supplementation of vitamin D (38% in 2009). One (1%) of them had a deficiency (4/88 [5%] in 2009), 43 (48%) insufficiency (62/88 [70%] in 2009) and 46 (51%) had normal results (22/88 [25%] in 2009). A total of 149 patients were not receiving any supplementation: 8 (5%) had deficiency (14/142 [10%] in 2009), 121 (81%) insufficiency (119/142 [83%] in 2009) and 20 [13%] normal vitamin D level (9/142 [6%] in 2009). Compared with 2009, significantly more patients had normal results in 2011, both those on oral daily supplementation (p <0.01) and those without any supplementation (p = 0.04) (fig. 2).
If we used 20 ng/ml as a cut-off (rather than 30 ng/ml), 52% patients had levels >20 ng/ml in 2009 and 66% in 2011 and the difference was statistically significant (p = 0.001).
During the years separating the two study periods the number of 25-OH vitamin D dosages (3,056 in 2008 and 6,896 in 2011) and the prescription of high doses of vitamin D3 (660 in 2008 and 2,530 in 2011) increased in our hospital (fig. 3). In the general outpatient clinic of the same hospital the prescription of high doses of vitamin D3 increased by more than 300% between 2008 and 2011. On the other hand in the same clinic, the prescription of daily supplements increased only of 40%.
In addition the number of publications about vitamin D had increased between 2008 and 2011. Specifically, the number of publications with the phrase “vitamin D” in Swiss Medical Weekly, Swiss Medical Forum and Revue Médicale Suisse increased from four to nineteen.
| Table 1: Patients’ characteristics in 2009 and 2011. | |||
| 2011 | 2009 | ||
| All | Number of patients | 239 (167 women) | 230 (162 women) |
| 25-OH Vitamin D (ng/ml) | 23.8 | 20.8 | |
| Daily vitamin D3 supplement | 38% | 38% | |
| Age (years) | 56 | 52 | |
| Deficiency | Number of patients | 9 | 18 |
| 25-OH Vitamin D (ng/ml) | 6.6 | 8.2 | |
| Daily vitamin D3 supplement | 11% | 22% | |
| Age (years) | 53 | 50 | |
| Insufficiency | Number of patients | 164 | 181 |
| 25-OH Vitamin D (ng/ml) | 20.3 | 19.5 | |
| Daily vitamin D3 supplement | 26% | 34% | |
| Age (years) | 54 | 52 | |
| Normal | Number of patients | 66 | 31 |
| 25-OH Vitamin D (ng/ml) | 34.9 | 35.6 | |
| Daily vitamin D3 supplement | 70% | 71% | |
| Age (years) | 62 | 54 | |
Prevalence of hypovitaminosis D decreased in two years from 86% to 72% (or from 48% to 34% using the cut-off of 20 ng/ml) despite the fact that the population was older in 2011. These results were mainly due to the higher number of normal 25-OH vitamin D levels observed in patients taking oral daily vitamin D (increasing from 25% to 51%).
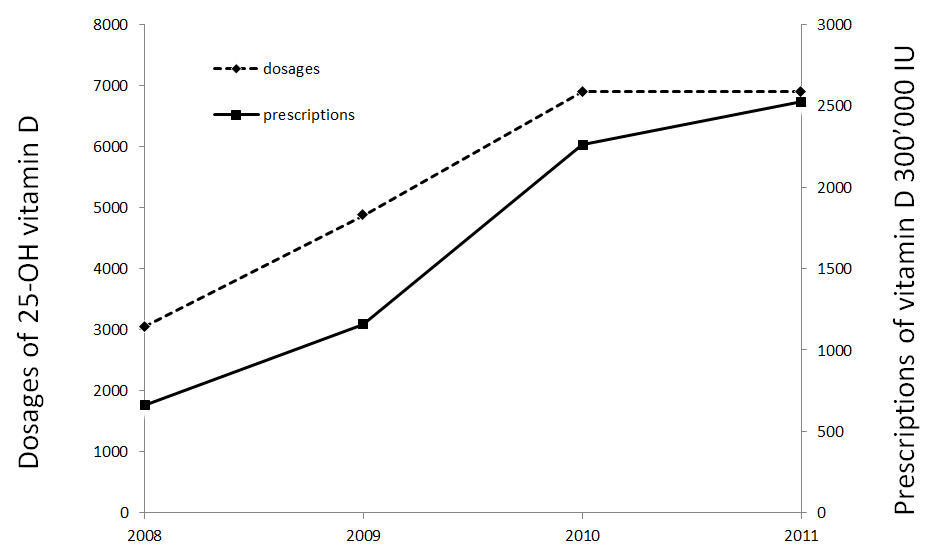
Figure 3
Evolution of vitamin D dosages and prescriptions between 2008 and 2011 in Lausanne University Hospital
This was not explained by a higher prescription of daily vitamin D supplement (38% in both years). In addition, this could not be related to a difference in sun exposure since the average of sunshine in the region was globally higher in summer 2009 compared to summer 2011. (Internet: http://www.meteoschweiz.admin.ch/web/fr/climat/). It was probably related with better adherence to daily oral supplements by the supplemented patients.
It could also be minimally related to the higher percentage of patients with osteoporosis in 2011, since they are possibly more motivated than the patients with inflammatory rheumatic or degenerative disease to take their supplements regularly.
We also think this might be due to better information and awareness of the physicians about hypovitaminosis D who probably asked more regularly about vitamin D supplementation adherence and helped themselves and the patients with more systematic 25-OH vitamin D level measurements.
It could also be related to higher prescription of high doses of vitamin D3 supplement in the previous years in our department particularly in the nonsupplemented patients. Of note, this kind of supplementation has been shown to be efficient in selected cases despite some controversy concerning its safety [15].
It is also reasonable to think that patients not receiving regular prescriptions for vitamin D were simply more aware of the problem of hypovitaminosis D and took more regular natural supplement, in food for example.
Our study has many limitations. Firstly, it is an uncontrolled study. Secondly, the two populations compared are different. Thirdly, we did not perform a specific verification of compliance with daily vitamin D supplementation. Finally we could not determine precisely which patients benefited from prescription of high doses of vitamin D3 between December 2009 and April 2011 (incomplete files). Therefore we cannot demonstrate the proposed relation between the increase in adherence with daily supplement and the prescription of high doses of vitamin D and the better results in 2011.
Our study has nevertheless some strengths. Interestingly we could show a significant increase in vitamin D levels despite the older age and decreased sun exposure. Most importantly it is a true population-based study and the two populations are very similar. We used the same dosage method and we did the blood tests at the same time of the year (same month) at the same policlinic (same place). And finally it gives a simple and strong message about the possibility of improving the vitamin D status in a population with better physician information and patient education.
It is indeed very important to improve our capacity to supplement a rheumatology population considering the well-known relationship between hypovitaminosis D and musculoskeletal health and the increasing evidences of a correlation between the activity of autoimmune rheumatic disease and vitamin D status [16–18].
In conclusion, the prevalence of low vitamin D decreased in two years from 86% to 72%. These results were mainly due to the higher number of normal 25-OH vitamin D levels observed in patients taking oral daily vitamin D (increasing from 25% to 51%). These results may be explained by: 1) better adherence to oral daily vitamin D in the supplemented patients; 2) better information of physicians about hypovitaminosis D; 3) more frequent screening of vitamin D level and 4) higher prescription of high doses of vitamin D if this is deemed needed.
1 Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–81.
2 Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, et al. Effect of Vitamin D on falls: a meta-analysis. JAMA: the journal of the American Medical Association. 2004;291(16):1999–2006.
3 Janssen HC, Samson MM, Verhaar HJ. Vitamin D deficiency, muscle function, and falls in elderly people. Am J Clin Nutr. 2002;75(4):611–5.
4 Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
5 Bischoff-Ferrari HA, Willett WC, Wong JB, Stuck AE, Staehelin HB, Orav EJ, et al. Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Arch Intern Med. 2009;169(6):551–61.
6 Bischoff-Ferrari HA, Willett WC, Orav EJ, Lips P, Meunier PJ, Lyons RA, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;367(1):40–9.
7 Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GE, et al. IOF position statement: vitamin D recommendations for older adults. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2010;21(7):1151–4.
8 Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–8.
9 Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
10 Guessous I, Dudler V, Glatz N, Theler JM, Zoller O, Paccaud F, et al. Vitamin D levels and associated factors: a population-based study in Switzerland. Swiss Med Wkly. 2012;142:0.
11 Burnand B, Sloutskis D, Gianoli F, Cornuz J, Rickenbach M, Paccaud F, et al. Serum 25-hydroxyvitamin D: distribution and determinants in the Swiss population. Am J Clin Nutr. 1992;56(3):537–42.
12 Mouyis M, Ostor AJ, Crisp AJ, Ginawi A, Halsall DJ, Shenker N, et al. Hypovitaminosis D among rheumatology outpatients in clinical practice. Rheumatology. 2008;47(9):1348–51.
13 Chiu G. Vitamin D deficiency among patients attending a central New Zealand rheumatology outpatient clinic. N Z Med J. 2005;118(1225):U1727.
14 Stoll D, Dudler J, Lamy O, Hans D, So A, Krieg MA, et al. High prevalence of hypovitaminosis D in a Swiss rheumatology outpatient population. Swiss Med Wkly. 2011;141:w13196.
15 Stoll D, Dudler J, Lamy O, Hans D, Krieg MA, Aubry-Rozier B. Can one or two high doses of oral vitamin D3 correct insufficiency in a non-supplemented rheumatologic population? Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2013;24(2):495–500.
16 Marques CD, Dantas AT, Fragoso TS, Duarte AL. The importance of vitamin D levels in autoimmune diseases. Rev Bras Reumatol. 2010;50(1):67–80.
17 Gatenby P, Lucas R, Swaminathan A. Vitamin D deficiency and risk for rheumatic diseases: an update. Curr Opin Rheumatol. 2013;25(2):184–91.
18 Pludowski P, Holick MF, Pilz S, Wagner CL, Hollis BW, Grant WB, et al. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality – A review of recent evidence. Autoimmun Rev. 2013;12(10):976–89.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.