Windswept lower limb deformities in patients with hypophosphataemic rickets
DOI: https://doi.org/10.4414/smw.2013.13904
Ali
Al Kaissi, Sebastian
Farr, Rudolf
Ganger, Klaus
Klaushofer, Franz
Grill
Summary
BACKGROUND: X-linked hypophosphataemic rickets is an X-linked dominant disorder that is secondary to renal phosphate-wasting. Genu varum and/or genu valgum have been described as the most common deformities in patients with hypophosphataemic rickets. Windswept deformity, which is valgus deformity in one knee and varus deformity in the other, was the most common deformity encountered in our department.
PATIENTS AND METHODS: We collected seven patients who had phenotypic and genotypic features consistent with the diagnosis of X-linked hypophosphataemic rickets. All presented with windswept lower limb deformity. We discuss the phenotypic and genotypic correlation, and the surgical procedures applied. Surgical interventions were scheduled to correct the triad of appearance, function and biomechanics.
RESULTS: Re-alignment orthopaedic measures were applied to correct and to restore normal growth and development in these children. Post-operative measurements showed dramatic improvements in balance and gait.
CONCLUSION: The most common deformity seen in patients with hypophosphataemic rickets is gradual anetrolateral bowing of the femur combined with tibia vara. Windswept lower limb deformity was the most common angular deformity in our patients with hypophosphataemic rickets. Baseline skeletal surveys and genotypic characterisation were subject to close scrutiny and assessment, with the aim of proper diagnosis and treatment. Nevertheless, recurrence of deformity is a common sequel and younger patients have a higher risk for recurrence.
Introduction
Disturbances of skeletal growth presenting at birth or developing in childhood produce a bewildering array of clinical, radiological and pathological syndromes. The cartilaginous dysplasias are thought to arise from abnormal chondrocyte differentiation and metabolic growth [1].
X-linked hypophosphataemic rickets is a well-studied condition caused by a defect in renal tubular function that leads to diminished reabsorption of phosphate with resulting hypophosphataemia. Affected individuals have short stature and vitamin D-resistant rickets; hypocalcaemia, muscle weakness and tetany do not occur. Deafness can occur. X-linked affected individuals frequently present the following characteristics: short stature, lower-extremity deformity, bone pain, dental abscesses, impairment of hearing, enthesopathy, rickets and osteomalacia [2–4].
Genu varum and or genu valgum have been described as the main clinical deformity in the vast majority of patients with X-linked hypophosphataemic rickets [5, 6]. However, in our series of patients windswept lower limb deformities were the prime clinical presentation. The term “windswept deformity” describes the appearance of an abnormal valgus deformity in one knee in association with varus in the other. It is commonly seen in young children in certain parts of Africa, and its development is secondary to metabolic bone diseases. Metabolic bone diseases frequently result in skeletal deformities, especially in the legs, owing to physeal disturbances or defective mineralisation in children before puberty. Among these disorders, hypophosphataemic rickets, hypophosphatasia and renal osteodystrophy are the most frequent, but, nevertheless, other syndromic entities have been reported [7, 8]. Fulford and Brown [9] applied the term of “windswept deformity” in a different context, to a postural deformity acquired by spastic infants during the first few weeks of life. Golding [10] reported an extensive survey of this condition in West Indian children. Both authors recognised a more common infantile form arising in the first, second or third year of life, and a rarer, usually less severe, adolescent type. Inactivating mutations of the PHEX (phosphate-regulating gene with homology to endopeptidases) gene located at Xp22.1 have been linked with X-linked hypophosphataemic rickets, regardless of the type of the presenting deformity [11, 12]. Identifying patients with unusual skeletal deformities is of value because it illustrates that the more severely involved the locomotor system is, the greater the likelihood of having a syndromic complex.
Patients and methods
The study protocol was approved by the Medical University of Vienna (Ethics Committee, EK Nr.921/2009); in addition informed consent was obtained from the patients’ guardians. The records of seven patients (all males with anaverage age of 12 years) were studied at the osteogenetic department of the Orthopaedic Hospital of Speising, Vienna, Austria. Detailed clinical examination, extensive radiographic investigations and genotypic confirmation were performed accordingly. All our patients with hypophosphataemia showed mutation in the PHEX gene sequence (Xp.22) with subsequent inactivity of the PHEXprotein.

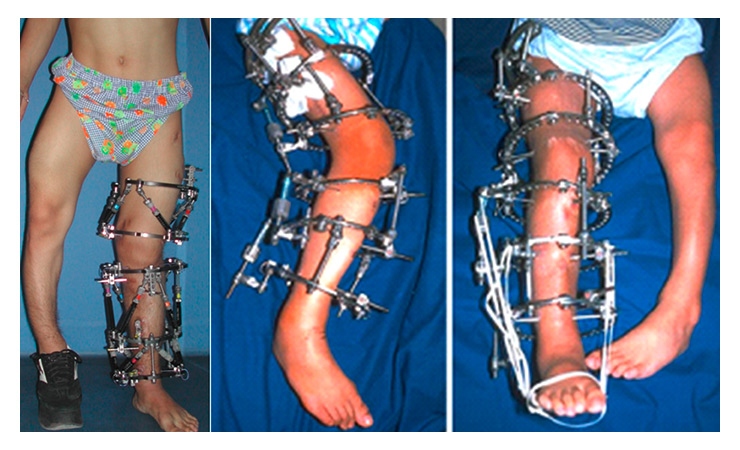
Figure 1
Standing photos of three patients of different ages who presented with windswept deformity (the appearance of an abnormal valgus deformity in one knee in association with varus in the other). Clinically, the average valgus deformity was 35° and the average varus deformity was 22°.
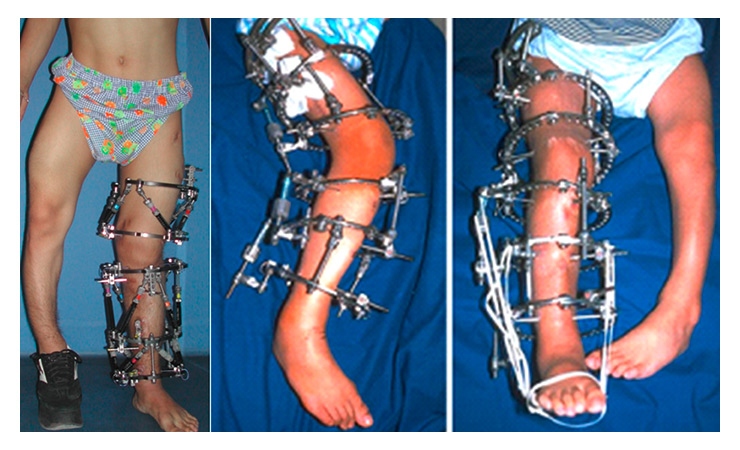
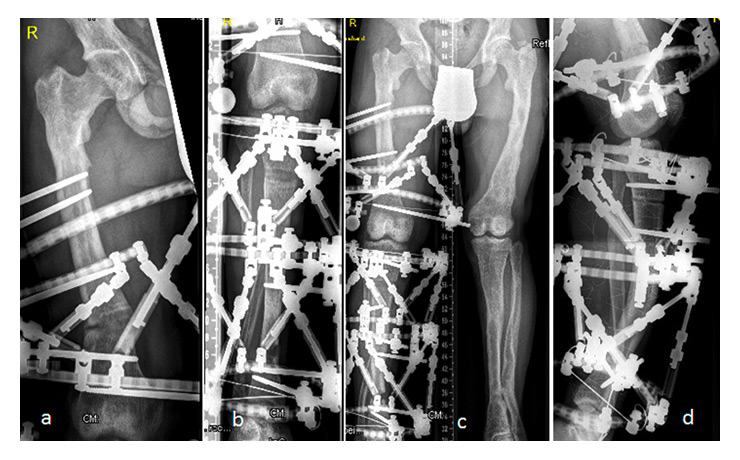
Figure 2
After proximal and distal femoral osteotomy, or a proximal tibial osteotomy of the lower limbs (in different patients), a Taylor spatial frame was applied.
Hypophosphataemic rickets encompasses a group of disorders in which normal dietary intake of vitamin D is insufficient to achieve normal mineralisation of bone. There are four major forms, the most common of which is inherited as an X-linked dominant trait, followed in frequency by an autosomal dominant type. The inherent abnormality in familial vitamin D-resistant rickets is the inability of the renal tubules to retain phosphate, which leads to phosphate diabetes and hypophosphataemia. End-organ insensitivity to vitamin D is the cause of autosomal recessive vitamin D-resistant rickets. This form is extremely hard to treat. The third form is characterised by failure of the kidney to perform the second hydroxylation of vitamin D. This type rarely requires orthopaedic intervention because it is easily treated with the administration of dihydroxy-vitamin D. In renal tubular acidosis, the kidney excretes fixed base and wastes bicarbonate. This leads to wasting of calcium and sodium as well. The alkaline urine results in precipitation of calcium and severe renal calcinosis. Tubular resorption of phosphate in the kidney is under the control of the sodium/phosphate contransporters located on the tubular cell membrane [2–4]. The diagnosis of X-linked hypophosphataemic rickets in our group of patients was established at an average age of 2 years and 9 months by physical examination, radiographic interpretation, complete metabolic testing and a family history consistent with this clinical entity, followed by genotypic confirmation.
The initial complaints in our patients were delayed walking and the development of angular deformities of the lower extremities (average age of onset was 14–18 months). The physical findings and the skeletal deformities in our patients resemble those seen in nutritional rickets, but, because of the chronicity of the disease, the deformities become far more severe. Strikingly, short stature, increasing pain and walking difficulties, accompanied by periarticular enlargement associated with widening of the physes and the metaphyses were the prime manifestations. Laboratory studies showed normal calcium levels; parathyroid hormone (PTH) and 25-hydroxy-vitamin D concentrations were normal, but the serum phosphate concentration was significantly decreased. Urine assays for phosphate showed an increased concentration of phosphate in urine (hyperphosphaturia) [9]. The serum alkaline phosphatase concentration was elevated (the average was five times greater than normal). Genetic testing attributed the condition to mutations in the PHEX gene located at Xp22.1.
Windswept deformities were assessed in all our patients by means of clinical and radiographic examination, and by measuring the mechanical axis deviation and the knee orientation lines according to the method described by Paley et al. [13]. Preoperative planning depends on exact analysis of the deformity in all three dimensions and levels (standing radiographs [anteroposterior and lateral of the whole extremity], orthoradiography and rotational computed tomography [CT] scan were applied with usual methodology).
Standing photographs of some patients presenting with windswept deformity (the appearance of an abnormal valgus deformity in one knee in association with varus in the other) are shown in figure 1. Clinically, the average valgus deformity was 35° and the average varus deformity was 22°.
Results
We usually perform corrective procedures at an early stage of deformity, anticipating two or three steps in the corrective procedure during growth, in order to avoid prolonged corrective surgeries, particularly in patients with severe deformities since these deformities are expected to get worse with time. Recurrence of deformities is independent of the correctional procedures applied. In practice, no corrective procedure appeared clearly superior to any other. Nevertheless, we observed that the recurrence rate decreased once the patients achieved skeletal maturity. In general, our surgical techniques depend on the age of the patient and the type of deformity. For children aged 5–7 years with angular deformity, our method of choice is osteotomy and fixation with K-wires or guided growth (temporary or definitive hemiepiphysiodesis). For children prior to skeletal maturation we prefer the Taylor spatial frame. In children after skeletal maturity we usually use interlocking nails. In cases where the deformity is greatest around the epimetaphyses, we usually use external fixation.
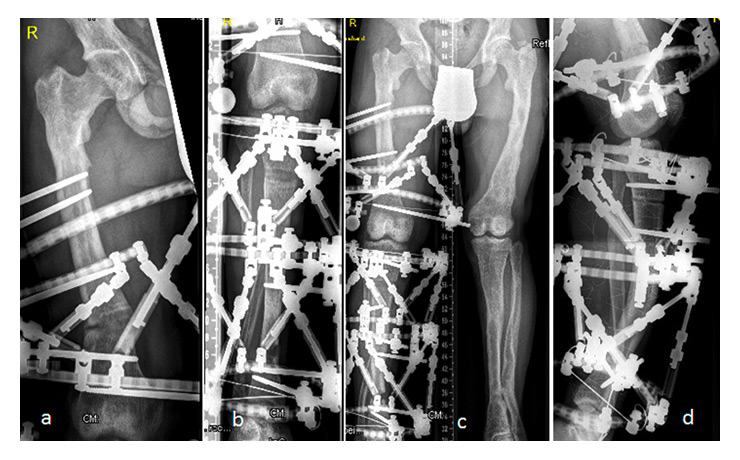
Figure 3 (a,b,c).
Femoral or proximal tibial osteotomies (in different patients). It is evident that the severe varus deformity was corrected by gradual distraction using a Taylor spatial frame. External fixation allowed fine-tuning of the alignment postoperatively.
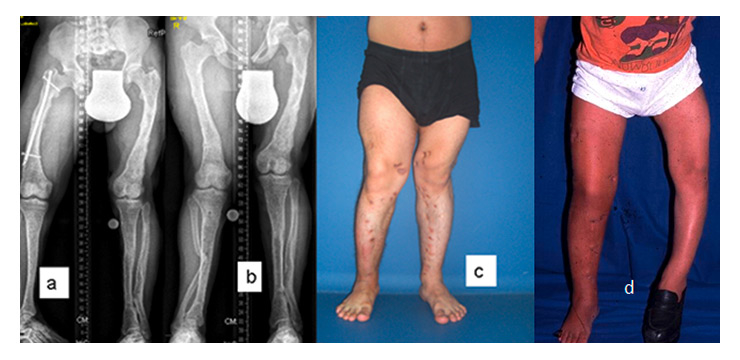
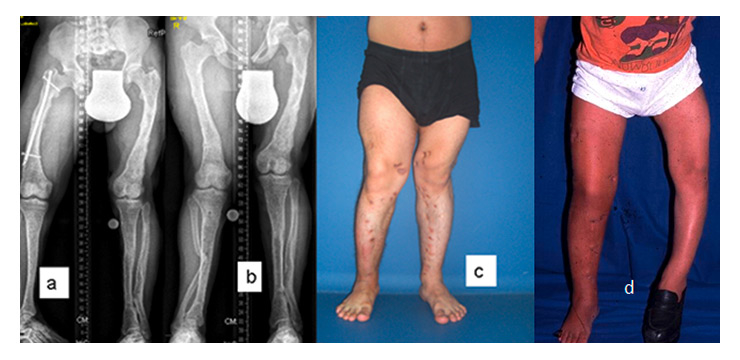
Figure 4
Clinical status after corrections in four patients. (a) After full correction and acceptable bony consolidation, an intramedullary fixation by means of locked nails was inserted along the right femur and the patient was able to stand. (b) Alignment and orientation are best judged using standing long anteroposterior view radiographs of the entire lower extremity. (c) Orthopaedic interventions to realign the lower limbs in our patients were successful in producing a better balance and gait in these children, thereby our patients were able to stand almost normally. (d) A patient’s photograph shows the results of correcting the deformity and the results of the re-alignment of the lower limbs. The average postoperative valgus deformity in our patients was 8.2° and the average varus deformity was 12.4°
Regardless of the type of fixation used, we carried out careful preoperative planning and assessment of the surgical treatment to realign the deformities. In our current patients, multiple osteotomies in three planes were required in both the tibiae and the femora, as well as limb-length equalisation; the aim was to correct satisfactorily the mechanical axis deviation of the limb. After a proximal and distal femoral osteotomy, or a proximal tibial osteotomy of the lower limbs (in different patients), a Taylor spatial frame was applied (fig. 2). After femoral or proximal tibial osteotomy along the lower limbs (in different patients), the severe varus deformity was corrected by gradual distraction using a Taylor spatial frame. External fixation allowed fine-tuning of the alignment postoperatively (fig. 3). After full correction and acceptable bony consolidation, intramedullary fixation by means of locked nails was inserted along the right femur, and the patients were able to stand. Alignment and orientation are best judged using standing long anteroposterior view radiographs of the entire lower extremity.
Orthopaedic interventions to realign the lower limbs were successful in producing a better balance and gait in our patients; thereby, our patients were able to stand almost normally. The average postoperative valgus deformity was 8.2° and the average varus deformity was 12.4° (fig. 4). After bony consolidation of the osteotomy, we usually evaluate the mechanical axis deviation with an average of 5 mm medial to the centre of the knee joint. Deviation of the mechanical axis and the knee joint lines was noticed to increase within 5–12 months. Also, we noticed that the recurrence rate (mechanical axis deviation extending beyond the knee joint) was 90% after the first surgical correction, 60% after the second operation, and so forth.
Discussion
Osteochondrodysplasias are a heterogeneous group of genetic skeletal dysplasias [1, 2].These disorders are diagnosed and classified in accordance with the phenotypic and genotypic characterisation. Patients with these disorders commonly develop a bewildered combination of skeletal deformities, such as angular deformities of the lower limbs, scoliosis and kyphosis [14].
The usual medical treatment for patients with hypophosphataemic rickets consists of oral replacement of phosphorus in large doses and the administration of vitamin D. Nephrocalcinosis is a significant complication of medical treatment. In a recent study, renal calcinosis was present in 79% of treated children with hypophosphataemic rickets, and the severity of the calcinosis correlated with the dose of phosphorus. Because nephrocalcinosis is a significant complication, the decision whether to offer treatment to children with hypophosphataemic rickets has become controversial [15–17]. On the other hand, in children with radiographic features of active rickets (cupping and widening of the growth plates) and the distinctive phenotypic constellation of pigeon chest, rachitic rosary and asymmetrical or symmetrical limb deformities. We usually encounter dramatic clinical and radiographic improvement in response to vitamin D or its derivatives in these patients. In normal children, growth and development of the skeleton requires adequate supplies of calcium and phosphate, and deficiency of these minerals results in impaired bone mineralisation. The compromised bone quality in patients with hypophosphataemic rickets occurs in connection with, firstly, reduced serum levels of phosphate and calcitriol levels with normal serum calcium and PTH levels. Secondly, the aberrant regulation of the 25(OH)D-1-α-hydroxylase accounts for the paradoxical occurrence of inappropriately normal or reduced calcitriol levels in the face of hypophosphataemia, with subsequent development of rickets/osteomalacia [18]. Thirdly, in hypophosphataemia, an intrinsic osteoblast defect contributes to the low bone quality. Miao et al. [19] suggested that a mutant PHEXgene results in abnormal bone matrix protein expression and deposition.
In general, genu varum with tibiofemoral widening and cupping are much more often observed in patients with hypophosphataemic rickets than genu valgum [20, 21]. This fact is mainly due to the varus alignment at the time of manifestation, established when the child begins to stand and walk. Thus, both the Ilizarov and the Taylor spatial frames are powerful tools for correction of angular deformities. A special feature of the Taylor spatial frame, and an advantage compared with the Ilizarov device, is its virtual hinge, which allows for the simultaneous gradual correction of multiplanar deformities and limb lengthening through one osteotomy site [22]. The power of the spatial frame lies in its precise control over the final limb length and alignment and its ability to correct a residual deformity. The stability of this multiplanar circular fixator permits earlier weight-bearing and provides an ideal environment for both new bone formation and soft tissue healing. Although a high recurrence rate of 90% after the first corrective procedure and 60% after the second were observed in a retrospective follow-up [23], Kanel and Price [24] stated that external fixation allows fine-tuning of the alingnment postoperatively, when the patient is able to stand. Ferris et al. [25] advocated the use of intramedullary fixation or plating in the management of patients with hypophosphataemic rickets. Adults with hypophosphataemic rickets are prone to the development of arthritis. Degradation of articular cartilage resembling osteochondritis dissecans has been described. Joint stiffness and bone pain are common complaints. Although Rubinovitch et al. [26] believed that recurrent deformity is a common sequel of osteotomies in patients with hypophosphatemic rickets, Loeffler and Sherman [27] believed that younger patients have a higher risk of recurrence.
Another method for correction of malalignment is via hemiepiphysiodesis [28]. Several different, mini-invasive devices (i.e. eight-plate, Orthofix) are available for temporary hemiepiphysiodesis and guided growth. However, a slower correction was observed in patients with metabolic causes, which suggests an earlier start of intervention compared with idiopathic deformities. A slight overcorrection of 5° is, furthermore, recommended to achieve the desired effect.
On the other hand, children with hypophosphataemic rickets are generally prone to developing spinal deformities such as thoracolumbar kyphosis, commonly known as “rachitic cat-back”, or scoliosis [29]. Modalities and results of rachitic scoliosis treatment had already been described in the early fifties by Katthagen [30]. Among preschool aged children of 6–7 years with asymmetric posture, 27.8% were diagnosed as having rickets, suggesting the possibility of an ongoing deformational spinal process. This significant association between trunk asymmetry and rickets resulted in an increased odds ratio of up to 3.42 in children with advanced rickets [31]. However, an increased mortality was noticed in a long-term follow-up of patients with untreated scoliosis of different aetiologies, including rickets [32]. In contrast, secondary kyphotic deformities are usually not as striking as in the long bones and rarely progress to a severe deformity [33].
Conclusion
In evaluating a patient with lower limb deformity, physicians and orthopaedic surgeons must keep in mind the important concept that the more severely involved the patient is, the greater the likelihood of the patient having an intrinsic bone disorder. Lower limb deformities may be the outcome of the adverse effects of weight bearing, particularly when exerted on bones and joints with poor bone quality, such as we encountered in patients with skeletal dysplasia and, particularly, in patients with congenital metabolic abnormalities. Surgical correction was carried out when the deformity had reached the irreversible mechanical point, and progression was notable. Nevertheless it seems hard to predict the skeletal prognosis in patients with skeletal dysplasias because of the progressive mechanism of low bone quality.
References
1 Beals R, Horton W. Skeletal dysplasias: An approach to diagnosis. J Am Acad Orthop Surg. 1995;3:174–81.
2 Balsan S, Tieder M. Linear growth in patients with hypophosphatemic vitamin D-resistant rickets: influence of treatment regimen and parental height. J Pediatr. 1990;116:365–71.
3 Condon JR, Nassim JR, Rutter A. Pathogenesis of rickets and osteomalacia in familial hypophosphataemia. Arch Dis Child. 1971;46:269–72.
4 Fishman G, Miller-Hansen D, Jacobsen C, Singhal VK, Alon US. Hearing impairment in familial X-linked hypophosphatemic rickets. Eur J Pediatr. 2004;163:622–3.
5 Patzer L, Van’T Hoff W, Dillon MJ. X-linked hypophosphataemic rickets: recognition, treatment and prognosis. Curr Paediatr. 1998;8:26–30.
6 Petje G, Meizer R, Radler C, Aigner N, Grill F. Deformity correction in children with hereditary hypophosphatemic rickets. Clin Orthop Relat Res. 2008;466(12):3078–85.
7 Smyth EHJ. Windswept deformity. J Bone Joint SurgBr. 1980;62-B:166–7.
8 Al Kaissi A, Ganger R, Klaushofer K, Grill F. Windswept deformity in a patient with Schwartz-Jampel syndrome. Swiss Med Wkly. 2012 Mar 19;142:w13519. doi: 10.4414/smw.2012.13519
9 Fulford GE, Brown JK. Position as a cause of deformity in children with cerebral palsy. Dev Med Child Neurol. 1976;18:305–14.
10 Golding JSR. Tibia vara. J Bone Joint Surg Br. 1962;44-B:216.
11 Roetzer KM, Varga F, Zwettler E, Nawrot-Wawrzyniak K, Haller J, Forster E, Klaushofer K. Novel PHEX mutation associated with hypophosphatemic rickets. Nephron Physiol. 2007;106(1):p8–12.
12 Sabbagh Y, Jones AO, Tenenhouse HS. PHEXdb, a locus-specific database for mutations causing X-linked hypophosphataemia. Hum Mutat. 2000;16:1–6.
13 Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planing for frontal and sagittal plan corrective osteotomies. Orthop Clin North Am. 1994;25:425–46.
14 Wynne-Davies R, Gormley J. The prevalence of skeletal dysplasias. An estimate of their minimum frequency and the number of patients requiring orthopaedic care. J Bone Joint Surg Br. 1985;67B:133–7.
15 Seikaly M, Browne R, Baum M. Nephrocalcinosis is associated with renal tubular acidosis in children with X-linked hypophosphatemia. Pediatrics. 1996;97.
16 Marie PJ, Glorieux FH. Stimulation of cortical bone mineralization and remodeling by phosphate and 1,25 dihydroxyvitamin D in vitamin D-resistant rickets. Metab Bone Dis Relat Res. 1981;3:159.
17 Verge CF, Lam A, Simpson JM, et al. Effects of therapy in X-linked hypophosphataemic rickets. N Engl J Med. 1991;325:1843.
18 Carpenter TO. New perspectives on the biology and treatment of X linked hypophosphatemic rickets. Pediatr Clin North Am. 1997;44:443–60.
19 Miao D, Bai X, Dibyendu P, McKee MD, Karapalis AC, Goltzman D. 2001 Osteomalacia in Hyp mice is associated with abnormal Phex expression and with altered bone matrix protein. Endocrinology. 142:926–37.
20 Brooks WC, Gross RH. Genu Varum in Children: Diagnosis and Treatment. J Am Acad Orthop Surg. 1995;3(6):326–35.
21 White GR, Mencio GA. Genu Valgum in Children: Diagnostic and Therapeutic Alternatives. J Am Acad Orthop Surg. 1995;3(5):275–83.
22 Manner HM, Huebl M, Radler C, Ganger R, Petje G, Grill F. Accuracy of complex lower-limb deformity correction with external fixation: a comparison of the Taylor Spatial Frame with the Ilizarov ring fixator. J Child Orthop. 2007;1(1):55–61.
23 Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27(3):253–9.
24 Kanel JS, Price CT. Unilateral external fixation for corrective osteotomies in patients with hypophosphataemic rickets. J Pediatr Orthop. 1995;15:232.
25 Ferris B, Walker C, Jackson A, et al. The orthopaedic management of hypophosphataemic rickets. J Pediatr Orthop. 1991;11:367.
26 Rubinovitch M, Said SE, Glorieux FH, et al. Principles and results of corrective lower limb osteotomies for patients with vitamin-D- resistant hypophosphatemic rickets. Clin Orthop Relat Res. 1988;237:264.
27 Loeffler RD Jr, Sherman FC. The effect of treatment on growth and deformity in hypophosphatemic vitamin D-resistant rickets. Clin Orthop Relat Res. 1982;162:4.
28 Boero S, Michelis MB, Riganti S. Use of the eight-Plate for angular correction of knee deformities due to idiopathic and pathologic physis: initiating treatment according to etiology. J Child Orthop. 2011;5(3):209–16.
29 Brunk M. The importance of rickets in childhood as a cause of scoliosis in adult age. Acta Orthop Scand Suppl. 1951;9:3–114.
30 Katthagen A. Treatment of early rachitic scoliosis. Z Orthop Ihre Grenzgeb. 1951;81(3):460–5.
31 Juskeliene V, Magnus P, Bakketeig LS, Dailidiene N, Jurkuvenas V. Prevalence and risk factors for asymmetric posture in preschool children aged 6–7 years. Int J Epidemiol. 1996;25(5):1053–9.
32 Pehrsson K, Larsson S, Oden A, Nachemson A. Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine (Phila Pa 1976). 1992;17(9):1091–6.
33 Hensinger RN. Kyphosis secondary to skeletal dysplasias and metabolic disease. Clin Orthop Relat Res. 1977;(128):113–28.