Figure 1
Recruitment of psychiatric experts.
DOI: https://doi.org/10.4414/smw.2013.13890
Claimants for a work disability benefit need to undergo an independent medical evaluation (IME) to establish their work capacity. In Switzerland, IMEs are conducted by medical specialists (experts). They may work in their own practice or in a hospital where they treat patients, or they may work in specialised evaluation centres or insurance organisations. IMEs consist of assessments and lead to reports that serve insurers with key information to grant disability benefits [1, 2]. Swiss insurers typically ask medical specialists to evaluate a claimant’s work capacity in both his last job and in suitable alternative work. Work capacity may be obvious in claimants with severe diseases, such as heart failure or cancer, but is often more challenging to determine in claimants with other disorders such as psychiatric disorders. Difficulties arise in assessing the diagnosis [3–5] and the remaining functional capacity [3–12], and in relating functional capacity to work requirements [5, 9–12].
In recent years, claimants, insurers, lawyers and authorities have raised major concerns about the quality of IMEs that provoke legal procedures that are costly both in monetary terms and in human suffering [13, 14]. The Swiss Federal Court concluded that current reports of evaluations lack explicitness and transparency in the decision-making process, and lack reliability in the conclusions [15]. Evidence supports the concerns [3–12]. In one study, 22 German psychiatrists evaluated the work capacity of a claimant with recurrent depression on the basis of a video-taped interview. One-third each attributed a work capacity of <3 hours, 3 to 6 hours or >6 hours per day [4]; a result as good as throwing a dice. In a Danish study, 11 specialists in social medicine agreed poorly on the work capacity of 8 claimants with somatic and psychiatric disorders (kappa 0.33, worse in psychiatric claimants) [12]. Not surprisingly, medical experts have urgent calls for research to sort out the sources of such disagreement and find ways to reduce it [16].
Little research has explored possible sources of inter-rater variability. Two Dutch studies hypothesised that the variability may be related to different assessment routines of medical experts [5, 10]. Training and quality control of IMEs vary considerably among Western countries [17, 18]. In addition, variability in reporting may affect transparency and reliability of IMEs. A recent survey among social insurers in 12 European countries [19] draws a heterogeneous picture: Instruments to report on work capacity are in use in Iceland, the Netherlands, Sweden and the United Kingdom. Germany applies a semi-structured approach, requesting the psychiatrist to report on body function, activities and environmental factors. Belgium, Switzerland, Finland, France, Italy, Norway and Slovenia do not require a formal structure for reporting.
In order to address the concerns about transparency and reliability we need to know the current practice and existing deficits. Given the lack of empirical information about current practice in Switzerland, we performed a nationwide survey. For practical reasons, we focused this survey, and a subsequent research programme ( http://www.unispital-basel.ch/asim/RELY ), on psychiatric disorders. These constitute a major and growing proportion of claims for disability allowance in Switzerland and elsewhere [1, 20]. We aimed to learn about the psychiatric experts’ current practice in assessing and, in particular, reporting on work capacity, and to identify potential sources for lack of transparency and high variability in IMEs that may be amenable to improvement. We contrasted the findings with the current professional guidance and compared psychiatrists in specialised IME centres to other psychiatrists.
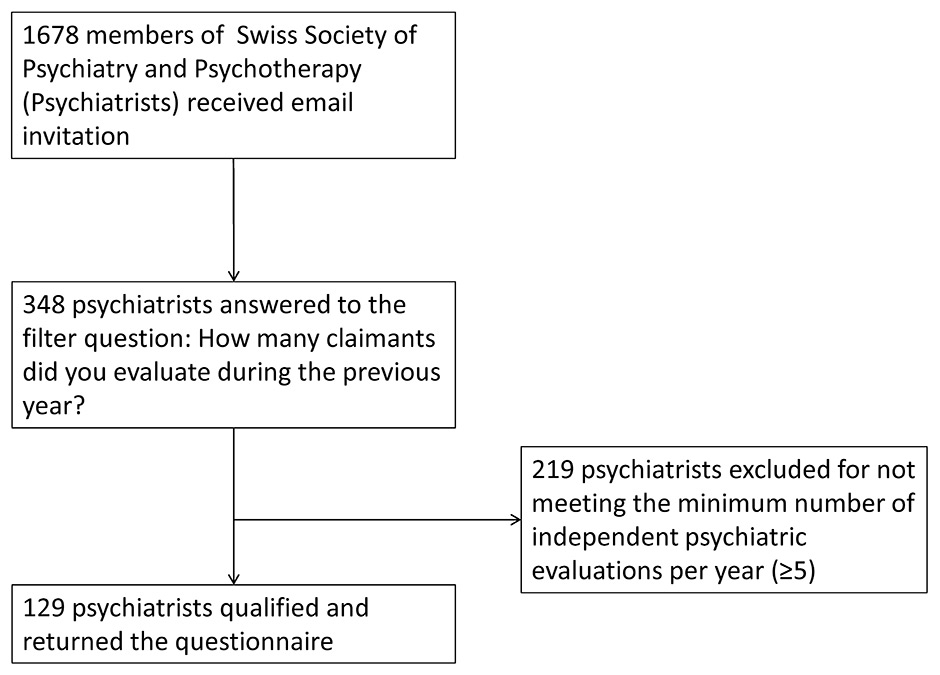
Our study population were psychiatrists who had conducted a minimum of five IMEs of work capacity during the previous year. We distributed the survey through the mailing list of the Swiss Society of Psychiatry and Psychotherapy (SGPP) to its 1,678 members. An invitation letter from the presidents of the SGPP and the Swiss Society of Insurance Psychiatry informed participants about the purpose of the survey, time to completion (15 minutes), confidentiality of the data and our intention to publish the results. We sent a reminder after three weeks.
We identified critical issues in current evaluation practice in three iterative steps. Firstly, we discussed potential issues within our study group consisting of Swiss experts in the field, psychologists and methodologists. Secondly, we reviewed the literature about Swiss IMEs, including newspaper and juridical articles, topped up by empirical studies we could identify in the literature, without performing a systematic review. Thirdly, we studied existing Swiss guidance [1, 5, 13, 14, 21–27]. Three topics seemed to be of high relevance to the Swiss community: reporting of work capacity, the description of a claimant’s previous job and measures of quality assurance applied in practice.
Based on these three topics, we developed a questionnaire. The study group iteratively discussed versions of the questionnaire in order to focus on issues that are amenable to improvement, to develop a clear terminology and to keep the questionnaire concise. Finally, we included questions about various ways to report work capacity (free-text, instruments, percentage and various combinations) and potential interpretations of a percentage work capacity. We asked whether psychiatrists regularly report not only their own judgment on work capacity, but also the claimant’s self-perception. We inquired about the use of measures to standardise the evaluation, such as a description of the current job, process guidelines, reporting forms, reporting instruments, and the use of scientific evidence to support the judgments and the importance of such measures to the psychiatrist. Furthermore, we ascertained the psychiatrists’ training and activities in continuous education. Where applicable, we structured response options on a four-point scale.
We programmed the survey on http://www.surveygizmo.com using verification of data entry, randomised order of response options, and prevention of duplicate participation. Three psychiatric experts pre-tested the survey for clarity and time to completion. The appendix shows the original questions in German and French, and an English translation.
We analysed both complete and incomplete questionnaires unless they contained only demographic information. In order to estimate the response rate we had to approximate the size of our study population, as the number of psychiatrists who performed five or more evaluations of work capacity per year is unknown. Based on discussions within the study group, we assumed that 50% of our study population would hold a voluntary certification for IME that is offered by the Swiss Society of Insurance Medicine. Currently, 206 psychiatrists are certified, corresponding to an estimated population size of 412.
For the following variables we hypothesised that psychiatrists who work in insurance organisations or evaluation centres, differ from psychiatrists who primarily treat patients in their practices or in hospitals: Work experience (numerical, Q4), reporting work capacity through free text / percentage / instrument (all dichotomous, Q8), meanings of percentage work capacity (all dichotomous, Q10 + 12), number of education activities (numerical, Q13), frequency of feedback from insurer (dichotomised, Q20), and quality of this feedback (dichotomised, Q21). We used the Wilcoxon signed rank test with continuity correction for numerical variables that were not normally distributed and the Fisher's exact test for dichotomous / dichotomised variables. We tested two sided with an alpha of 0.05 without correction for multiple testing. We used statistical software R [28].
| Table 1:Demographics. | |
| Language region (n = 91) | |
| German | 84% |
| French | 16% |
| Italian | 0% |
| Gender (n = 91) | |
| Male | 75% |
| Female | 25% |
| Age group (n = 91) | |
| ≤30 | 0% |
| 31–40 | 6% |
| 41–50 | 31% |
| 51–60 | 48% |
| >60 | 15% |
| Psychiatric qualification (n = 129) | |
| Specialist | 98% |
| Resident | 2% |
| Work situation (all options that apply, n = 129) | |
| Office based | 71% |
| Hospital / medical centre | 24% |
| Evaluation centre | 9% |
| Insurance organisation | 12% |
| Other | 5% |
| Work experience (n = 129) | |
| <10 years | 20% |
| ≥10 years | 80% |
| Evaluations of work capacity per year (n = 129) | |
| 5 to 20 | 63% |
| >20 | 37% |
A total of 129 of the responding psychiatrists qualified for the study (fig. 1). The estimated response rates for individual questions varied from 31% (129/412) to 22% (91/412). Table 1 summarises the characteristics of the psychiatrists.
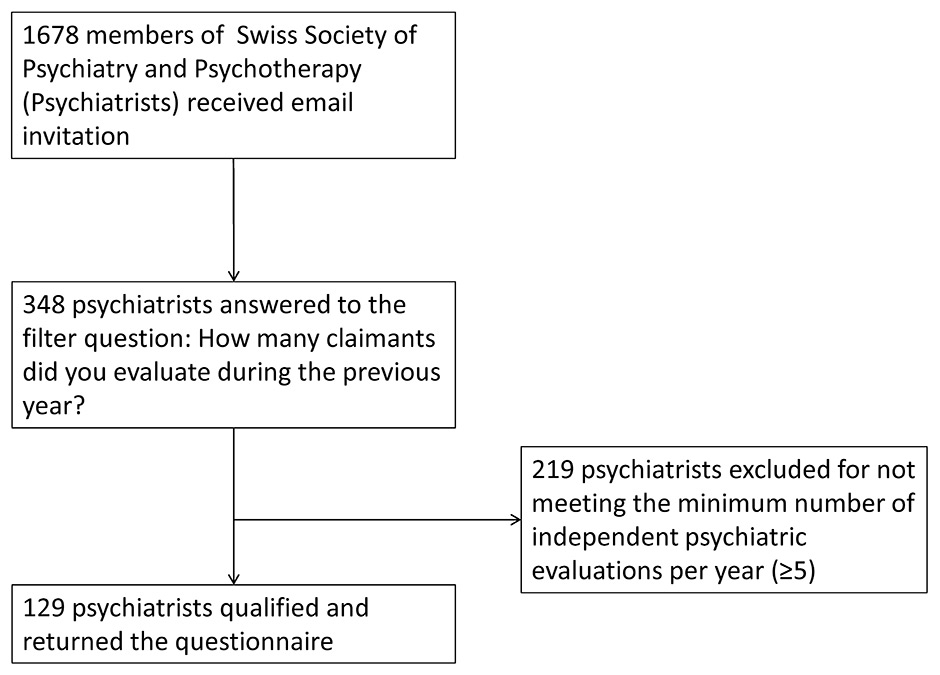
Figure 1
Recruitment of psychiatric experts.
Table 2 shows modes of reporting work capacity. A total of 13% (14/111) of the psychiatrists used one or more instruments, such as the MINI-ICF-APP [29] (11/14), the Global Assessment of Functioning [30] (8/14), or a checklist provided by the insurers (7/14) to document the claimant’s work capacity.
Most psychiatrists reported work capacity through a percentage, alone or in combination with other reporting modes, to express their judgment about a claimant's work capacity in his/her last job (81%) and in any suitable alternative job (71%). About half of the psychiatrists combined the percentage with free text (49% last job; 42% alternative job). The vast majority reported the claimant’s self-perceived work capacity in the last job (81%) and any suitable alternative job (74%), usually through free text.
We asked the psychiatrists two times to indicate all interpretations of percentage work capacity that they regarded as applicable (a) “in principle”, and (b) “in a recent case”. We offered five options that we had identified through discussion in our group (table 3). Regarding “in principle”, they approved an average of 4 (median, interquartile range [IQR] 3 to 5) interpretations. No clear preference for one single interpretation emerged. Rather, three interpretations – “restrictions of activities”, “working hours per day”, and “productivity” – ranked equally with approval rates around 80%. Regarding “in a recent case”, they selected on average 2 (median, IQR 1 to 3) interpretations. Again, no clear preference emerged (table 3). Most psychiatrists approved productivity (60%) followed by “working hours per day” (48%), “working hours per week” (46%), and “restriction of activities” (41%).
Most psychiatrists (74%, 70/94) rarely received a description of the claimant’s last workplace. If so, 67% (56/83) were dissatisfied or highly dissatisfied with its quality. The provision of a detailed job description by the insurers was considered as mandatory information by 90% (84/93).
When asked about professional guidance and quality control, psychiatrists referred to reporting instructions provided by the insurers (77%), their use of peer consultation (65%), or formal supervision (40%). Half of the psychiatrists (51%) regularly employed process guidelines, and one third (32%) regularly referenced scientific literature in their reports (table 4).
In the two years prior to the survey, 85% (84/99) of psychiatrists attended educational activities related to IMEs (median frequency 3, IQR 1 to 6). Of those, 68% (57/84) experienced the educational meetings as being of high or very high quality. A total of 63% (63/100) of psychiatrists welcomed the idea of compulsory continuing educational activities, while 29% (29/100) opposed it and 8% were indifferent (8/100).
Almost all psychiatrists (92%, 82/89) wanted the insurers to always provide feedback about the final administrative decision on the claimant’s work capacity. However, most psychiatrists (78%; 74/93) rarely received such feedback and if so, they were dissatisfied with its quality (75%; 43/57).
Psychiatrists employed by assessment centres or insurance organisations (n = 28) attended more educational activities related to IMEs compared to practice, or hospital-based psychiatrists (p = 0.001, median 6 versus 2). In addition, they indicated more often that the percentage work capacity in a recent case meant productivity (p = 0.006, OR = 3.5). Group differences were not significant in the other pre-specified variables.
Six Swiss professional societies or opinion leaders in insurance medicine published guidance on how to perform and report independent general and psychiatric evaluations [21–23, 26, 31, 32]. Table 5 compares the recommendations of these publications: Four publications instruct experts to report the claimant’s work capacity as a percentage [21, 22, 31, 32] and three publications refer to the Mini-ICF-APP as an optional tool for reporting functional capacity [22, 23]. One publication stresses the need for comprehensive information about job requirements [21].
| Table 2: Current practice of reporting on work capacity through text, instrument(s), percentage or combinations. | ||||
| Modes to report on work capacity | Psychiatrist’s judgment on the claimant’s work capacity (n = 111) | The claimant’s self-perceived work capacity (n = 108) | ||
| Last job | Alternative job | Last job | Alternative job | |
| No reporting | 2% | 8% | 19% | 26% |
| Only free text | 14% | 18% | 51% | 47% |
| Only instruments | 3% | 3% | 0% | 0% |
| Only percentage | 23% | 19% | 9% | 6% |
| Free text + instrument | 1% | 0% | 2% | 0% |
| Free text + percentage | 49% | 42% | 19% | 19% |
| Instrument + percentage | 4% | 2% | 0% | 0% |
| Free text + instrument + percentage | 5% | 8% | 0% | 3% |
| Table 3: Interpretations of percentage work capacity. | ||
| Interpretations of percentage work capacity | Interpretation applicable in principle proportion (95% CI) n = 82 | Interpretation used for a recent case proportion (95% CI) n = 81 |
| Restriction of activities (e.g. “Avoid dangerous work” or “No customer contact”) | 87% (78%‒93%) | 41% (30%‒53%) |
| Working hours per day | 85% (76%‒92%) | 48% (37%‒59%) |
| Productivity (e.g. working speed) | 83% (73%‒90%) | 60% (49%‒70%) |
| Working hours per week | 62% (51%‒72%) | 46% (36%‒58%) |
| Working days per week | 59% (48%‒69%) | 21% (13%‒31%) |
| Don’t know | 1% (0%‒6%) | 0% (0%‒5%) |
| Others | 4% (1%‒10%) | 5% (2%‒12%) |
| Table 4:Activities for quality control used by psychiatric experts. | ||||
| Applied very often | Applied often | Applied rather rarely | Never applied | |
| Reporting instructions from insurer (n = 93) | 45% | 32% | 13% | 10% |
| Peer consulting (n = 94) | 29% | 36% | 29% | 6% |
| Process guidelines (n = 94) | 24% | 27% | 31% | 18% |
| Supervision (n = 94) | 16% | 24% | 37% | 22% |
| Scientific literature (n = 94) | 5% | 27% | 57% | 11% |
| Table 5: Published guidance on psychiatric and general medical evaluations of work capacity. | ||||
| Authors or societies | Health conditions | Description of last job for evaluating work capacity | Instruments to standardize evaluation of work capacity | Percentage to report work capacity |
| Swiss Society of Psychiatry and Psychotherapy + Swiss Society of Insurance Psychiatry 2012[22] | Psychiatric | Indirect: A detailed description of the daily routine is of particular interest | Optional: Mini-ICF-APP [29] | Recommended |
| Hoffmann-Richter et al. 2012[23] | Psychiatric, general | Indirect: Preconditions of an evaluation of work capacity are medical information and knowledge of a claimant´s tasks. | Indirect recommendation of Mini-ICF-APP [29] as tool to increase transparency. Descriptions (no explicit recommendations) of several other instruments: Health assessment questionnaire [33], Neck disability Index [34], Performance Assessment and Capacity Testing [35], Functional Capacity Evaluation [36], Pain Disability Index [37]. Caveat mentioned: Most instruments have not been validated in evaluation of work capacity | No recommendation |
| Riemer-Kafka 2012 [21] | General | Explicitly required: Work capacity depends on work requirements; Each workplace has different work requirements; Any statement about work capacity requires a description of the related workplace. | Future prospect in appendix: Instruments based on the international classification of functioning, e.g. Mini-ICF-APP [29] | Recommended |
| Swiss Society of Insurance Medicine 2012[31] | General | Not mentioned | Not mentioned | Recommended |
| Oliveri et al. 2006[32] | General | Described as important, optional,anduseful; Evaluation of work capacity is substantially based on work requirements. | Optional: Functional Capacity Evaluation [36] for ergonomic assessment | Recommended |
| Swiss Society of Rheumatology 2007[26] | Musculoskeletal, General | Optional: workplace assessment | Optional: Functional Capacity Evaluation [35] for ergonomic assessment | Not mentioned |
We found that reporting on work capacity by psychiatrists is hindered by procedural (interpretation of and reporting about work capacity) and structural deficits (use of job description and quality control).
Guidance consistently requested experts to express a claimant’s work capacity as percentage, and indeed, 81% of psychiatrists reported work capacity exclusively as a percentage, or in combination with free text or an instrument. None of the publications reflected on the advantages and disadvantages of using this percentage, its different options of interpretation, or alternative ways to document work capacity. In our survey, where we had offered five different interpretations of percentage work capacity, the experts indicated all interpretations to be sensible and expressed a high or very high approval to each of four interpretations. The lack of a congruent understanding of percentage work capacity, a key concept in the Swiss evaluation of work capacity, seems an important source of poor transparency and variability in the decisions about work capacity.
Reporting tools can help to standardise process and content of an IME. However, instruments documenting work ability have not yet found their place in current Swiss psychiatric evaluations of work capacity. Only 13% of psychiatrists reported the regular use of an instrument, such as the Mini-ICF-APP [29] and / or the Global Assessment of Functioning [30]. The low uptake by psychiatric experts seems to mirror both the lack of instruments that have been validated in the context of evaluation of work capacity [23] and the low importance that the professional recommendations attach to these tools. The professional guidance that referred to instruments, did so in an unassertive manner and mentioned these only as one option to report on activity and participation deficiencies [22, 23] (table 5).
Most psychiatrists found it mandatory to have an informative job description in order to relate a claimant’s deficits and remaining abilities to his or her last work. However, they rarely received this from the insurer, and if provided, its quality was regarded as insufficient. Current guidance hardly comments on the job description. Only the most recent interdisciplinary guidance [21] demands unambiguously that the medical experts need to know the claimant’s work requirements.
The majority of psychiatric experts follow specific education (85%), and adhere to reporting instructions from the insurers (77%) and guidelines (51%). The widespread acceptance of these measures indicates that they may be suitable for addressing the deficits that we identified in this study. Although we did not explore the content of education programmes and instructions from insurers, there may be high potential for improvement if we assume that specific instructions on reporting and use of job profiles may be equally vague as in current guidance (table 5).
A proportion of 65% psychiatrists regularly uses peer consulting. Although we did not explore the psychiatrists understanding of peer consulting, which may range from a side comment in a conversation to a formal exchange, this indicates that a majority is interested in consolidating their own judgments through the professional consensus. In contrast, few psychiatrists use supervision. This may be explained by the longstanding experience of most experts (median age between 51 and 60 years). A total of 32% of the psychiatrist referenced literature on a regular basis. This seems promising considering the lack of research in the field.
We identified critical issues in current psychiatric IMEs of work capacity and generated the questionnaire using an iterative approach with input from literature and experts. Its nationwide administration captures key elements of the practice of psychiatrists across Switzerland. We contrasted the critical issues with published guidance on performing IMEs. This enabled us to identify inconsistent or vague recommendations that may cause variability in the current practice of psychiatric experts.
Our study has limitations. An estimated response rate of 31% cautions against overconfident generalising of the findings. We could not compare the characteristics of our sample with the study population as sufficient information about the latter is lacking. We did not cover the entire assessment process and other deficits may be relevant as well, although we did not find these in preparing the survey. We did not go into detail about quality control. Furthermore, it is uncertain as to what degree reporting of work capacity, description of a claimant’s previous job, and measures of quality control actually contribute to poor transparency and inter-rater variability. Although being of high relevance for the community, empirical evidence seems to be completely lacking.
We conducted a survey that essentially draws on respondents’ opinions and memory of their practice. This may therefore be biased. Ideally, the practice of reporting could be verified in a random sample of IME reports.
We addressed Swiss psychiatrists, but evidence suggests that similar problems exist in other disciplines and in other countries [6, 9]. In addition, we did not address other important stakeholders such as insurers, patients, judges, and lawyers who may have a different perspective from psychiatric experts. We will address these stakeholders in a subsequent survey.
Swiss psychiatrists have heterogeneous routines of assessing and reporting on work capacity in IMEs. Regular use of reporting instruments is uncommon and the key concept of expressing work capacity as a percentage lacks a universally accepted interpretation. In addition, psychiatrists miss a detailed job description and feedback from insurers. These deficiencies may reduce the transparency of decision-making and contribute to the variability in the reports. The impact of these deficits needs to be established. Education, engagement of insurers, and new professional guidelines might be effective means of implementing intended improvements.
Acknowledgement: We thank all participating psychiatrists and Dr. Thomas Zumbrunn for statistical advice.
1 Baer N, Frick U, Fasel T. Dossieranalyse der Invalidisierungen aus psychischen Gründen. Typologisierung der Personen, ihrer Erkrankungen, Belastungen und Berentungsverläufe. 2009; Available from: http://www.bsv.admin.ch/
2 DeBoer WEL. Organisation of disability evaluation in 15 countries. Pratiques et organisation des soins. 2007;38:205–17.
3 Chibnall JT, Dabney A, Tait RC. Internist judgments of chronic low back pain. Pain Med. 2000;1(3):231–7.
4 Dickmann JR, Broocks A. Psychiatric expert opinion in case of early retirement – how reliable? Fortschr Neurol Psychiatr. 2007;75(7):397–401.
5 Spanjer J, Krol B, Brouwer S, Groothoff JW. Sources of variation in work disability assessment. Work. 2010;37(4):405–11.
6 Clark WL, Haldeman S, Johnson P, Morris J, Schulenberger C, Trauner D, et al. Back impairment and disability determination. Another attempt at objective, reliable rating. Spine (Phila Pa 1976). 1988;13(3):332–41.
7 Clark W, Haldeman S. The development of guideline factors for the evaluation of disability in neck and back injuries. Division of Industrial Accidents, State of California. Spine (Phila Pa 1976). 1993;18(13):1736–45.
8 Horneij E, Hemborg B, Johnsson B, Ekdahl C. Clinical tests on impairment level related to low back pain: a study of test reliability. J Rehabil Med. 2002;34(4):176–82.
9 Kerstholt JH, DeBoer WEL, Jansen NJ. Disability assessments: effects of response mode and experience. DisabilRehabil. 2006;28(2):111–5.
10 Schellart AJ, Mulders H, Steenbeek R, Anema JR, Kroneman H, Besseling J. Inter-doctor variations in the assessment of functional incapacities by insurance physicians. BMCPublic Health. 2011;11(1471-2458):864.
11 Harrington M. An Independent Review of the Work Capability Assessment – year three [Internet]. London: Department for Work and Pensions; 2012. Available from: http://www.dwp.gov.uk/wca-review
12 Rudbeck M, Fonager K. Agreement between medical expert assessments in social medicine. Scand J Public Health. 2011;39(7):766–72.
13 Stöhr S, Bollag Y, Auerbach H, Eichler K, Imhof D, Fabbro T, et al. Quality assessment of a randomly selected sample of Swiss medical expertises. A pilot study. Swiss Med Wkly. 2011;141:w13173.
14 Pizala HJP. Evaluation von psychiatrischen Gutachten – Thesis. [University of Basel]; 2011.
15 Schweizerisches Bundesgericht. Urteil 9C_243/2010 des Schweizerischen Bundesgerichtes vom 28.06.2011 [Internet]. Available from: http://www.bger.ch/
16 Hesse B, Gebauer E. Disability assessment for the statutory pension insurance: significance, need for research, and opportunities. Rehabilitation (Stuttg). 2011;50(1):17–24.
17 De Boer WEL, Brenninkmeijer V, Zuidema W. Long-term disability arrangements. A comparative study of assessment and quality control. [Internet]. The Netherlands Organisation for Applied Scientific Research; 2004. Available from: http://www.eumass.com/
18 De Wind A. Education programmes for medical assessors. Their roles and responsibilities in EUMASS countries. Proceedings of the 2nd International Congress of Medical Assessors [Internet]. Maribor, Slowenia; 2011. p. 49. Available from: http://www.kongres-izvedencev.si/2011/
19 Anner J, Kunz R, de Boer WEL. The handicapped role – a framework for reporting disability in social insurance in Europe. submitted. 2012;
20 OECD. Sickness, Disability and Work: Breaking the Barriers. A Synthesis of Findings across OECD Countries. Paris: OECD Publishing; 2010.
21 Riemer-Kafka G. Versicherungsmedizinische Gutachten. Ein interdisziplinärer juristisch-medizinischer Leitfaden. 2nd ed. Bern: EMH Schweizerischer Ärzteverlag; 2012.
22 Colomb E, Dittmann V, Ebner G, Hermelink U, Hoffmann-Richter U, Kopp E, et al. Qualitätsleitlinien für psychiatrische Gutachten in der Eidgenössischen Invalidenversicherung [Internet]. Swiss Society of Psychiatry and Psychotherapy; 2012. Available from: www.psychiatrie.ch
23 Hoffmann-Richter U, Jeger J, Schmidt H. Das Handwerk ärztlicher Begutachtung. Theorie, Methodik und Praxis. 1st ed. Stuttgart: Kohlhammer; 2012.
24 Auerbach H, Bollag Y, Eichler K, Gyr N, Imhof D, Stöhr S. Medizinische Gutachtensituation in der Schweiz, Studie zur Einschätzung der Marktsituation und zur Schaffung von Markttransparenz und Qualitätssicherung [Internet]. Academy of Swinn Insurance Medicine, Zürich University of Applied Sciences; 2011. Available from: URL: http://www.sml.zhaw.ch/
25 Jeger J, Murer E. Medizinische Begutachtung: Vorschläge zur Lösung des Unabhängigkeitsproblems und zur Qualitätssteigerung. Möglichkeiten und Grenzen der medizinischen Begutachtung. Bern: Stämpfli Verlag; 2010. p. 247–274.
26 Jeger J. Leitlinien der schweizerischen Gesesschaft für Rheumatologie zur Begutachtung rheumatologischer Krankheiten und Unfallfolgen. Schweizerische Ärztezeitung. 2007;88(17):73642.
27 Jeger J. Die Kritik an Anwaltschaft und Versicherer aus der Sicht des medizinischen Gutachters. Möglichkeiten und Grenzen der medizinischen Begutachtung. Bern: Stämpfli Verlag; 2010. p. 159–194.
28 R Development Core Team (2011). R: A language and environment for statistical computing. [Internet]. Vienna, Austria: R Foundation for Statistical Computing; Available from: http://www.R-project.org/
29 Linden M, Baron S. The “Mini-ICF-Rating for Mental Disorders (Mini-ICF-P)”. A short instrument for the assessment of disabilities in mental disorders. Rehabilitation (Stuttg). 2005;44(3):144–51.
30 Hall RC. Global assessment of functioning. A modified scale. Psychosomatics. 1995;36(3):267–75.
31 Swiss Insurance Medicine. Arbeitsunfähigkeit. Leitlinie zur Beurteilung der Arbeitsunfähigkeit nach Unfall und bei Krankheit. 3rd ed. 2012.
32 Oliveri M, Kopp HG, Stutz K, Klipstein A, Zollikofer J. Grundsätze der ärztlichen Beurteilung der Zumutbarkeit und Arbeitsfähigkeit. Schweiz Med Forum. 6:420–431 (Part 1) und 448–454 (part 2).
33 Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23(2):137–45.
34 Vernon H, Mior S. The Neck Disability Index – a Study of Reliability and Validity. J Manip Physiol Ther. 1991;14(7):409–15.
35 Matheson LN, Matheson ML, Grant J. Development of a measure of perceived functional ability. J Occup Rehab. 1993;3(1):15–30.
36 Isernhagen SJ, Hart DL, Matheson LM. Reliability of independent observer judgments of level of lift effort in a kinesiophysical Functional Capacity Evaluation. Work. 1999;12(2):145–50.
37 Tait RC, Pollard CA, Margolis RB, Duckro PN, Krause SJ. The Pain Disability Index: psychometric and validity data. Arch Phys Med Rehabil. 1987;68(7):438–41.
Author Contributions: StS, KF, RaM, UHR, JJ, ReM, RK, and WdB were involved in developing the concept and design of the study and the questionnaire. StS performed the data collection. StS conducted the statistical analysis. All authors revised the manuscript and approved the final version.
Funding / potential competing interests: No funds were received for the study or the preparation of this manuscript. asim, the Department of Insurance Medicine at the University Hospital in Basel, is funded in part by donations from public insurers and a consortium of private insurance companies. The present study was initiated on asim’s own initiative. Insurers were not involved in any phase of the study.