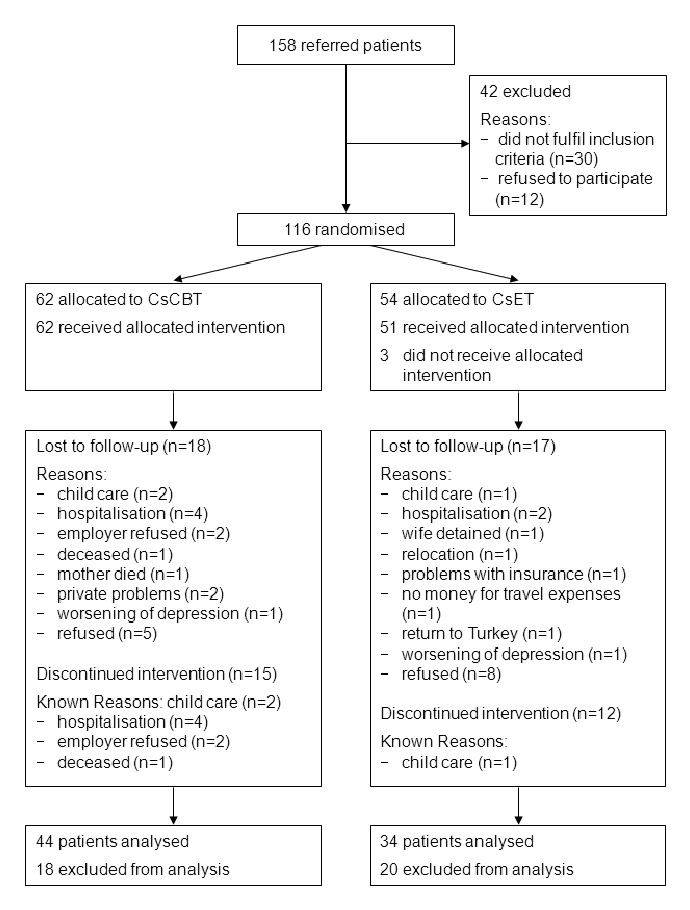
Figure 1
Flow chart of participants.
DOI: https://doi.org/10.4414/smw.2013.13875
Pain disorders are frequently encountered among immigrants. In England, chronic pain is more prevalent among African-Caribbean and South Asians than the English population [1–3].
Results of most investigations on experimental pain show significant ethnic differences in response to experimental pain across multiple stimulus modalities [4–8]. Most clinical pain studies agree that. in contrast to the native population, ethnic minority groups report more severe pain, more depressive symptoms, increased avoidance of activity, more fearful thinking, more physical symptoms, greater physical and psychosocial disability, wider-spread areas of pain, as well as greater disease activity [9–28]. Some authors point out that patient ratings differ from physician ratings. Physicians ascertain no specific difference in global physical assessment in immigrant patients [27, 28], and even less physical damage in these groups [19]. However, affiliation to a racial or an ethnic group may not necessarily be responsible for differences in the perception and experience of pain, as these variations may sometimes be better explained by socioeconomic status and level of education [29–32].
Additionally, racial and ethnic differences exist not only in the experience of pain but also in pain treatment. A majority of studies find that patients with a different ethnic background do not have the same access to pain therapy and are not given the same treatment. This inequality in pain treatment between ethnic groups has been observed across all types of pain and in many settings [15, 33–38]. As an example, white patients with pain were more likely to receive an opioid than black, Hispanic, or Asian patients; these differences did not diminish between 1993 and 2005. White workers claiming compensation were 40% more likely than African Americans to receive a diagnoses of a herniated disc and consequently twice as likely to undergo surgery.
Patients also differ in coping with pain. Compared with native Swedes, immigrants in Sweden rely more on passive coping strategies to manage pain [39]. Passive pain-coping strategies focus on treatment modalities that do not require a patient’s active participation, such as increasing pain medication or massage therapy. First-generation Turkish immigrants in Germany suffering from chronic headache overuse acute headache medication [40]. A comparison of US African-Americans and Caucasians shows the former to be less physically active and report lower perceived control over pain. African-Americans also employ more external pain-coping strategies such as the belief someone else could offer a successful therapy, be it a competent doctor or God himself [41–43]. Similar results have been found in a pain-free sample of young adults [44]. This suggests that ethnic differences in pain coping within clinical samples do not result from prolonged exposure to chronic pain, but might be evident even in the absence of chronic pain.
The importance of a culturally sensitive approach to the treatment of immigrants has been much discussed in the literature [15, 45–47]. Nevertheless, we were unable to find any publication about specific cognitive behavioural programmes for the treatment of culturally diverse patients who suffer from chronic pain. Either such programmes have not yet been developed or, if in existence, have not yet been evaluated. According to our own relatively extensive clinical experience, we assumed that conventional evidence-based cognitive behavioural therapy (CBT) programmes of pain management would not be effective for immigrants with chronic pain. Therefore, we modified a standard treatment programme for chronic pain patients to accommodate the specific needs of an immigrant sample with a culturally sensitive approach. The current paper describes the intervention and reports on its efficacy within a randomised controlled trial.
| Table 1: Demographic characteristics of group participants. | ||
| Characteristic | CsCBT group(n = 44) | CsET group (n = 34) |
| Mean age ± SD, y | 44.0 ± 7.4 | 43.8 ± 7.1 |
| Sex, % | ||
| Female | 70.5 | 67.6 |
| Male | 29.5 | 32.4 |
| Marital status, % | ||
| Married | 93.2 | 91.2 |
| Unmarried (single, widowed, divorced) | 6.8 | 8.8 |
| Nationality, % | ||
| Turkish | 65.9 | 55.9 |
| Kurdish | 34.1 | 41.2 |
| Others | 2.9 | |
| Educational level | ||
| no school | 20.5 | 23.6 |
| elementary | 54.5 | 52.9 |
| Intermediate | 20.5 | 14.7 |
| College | 4.5 | 8.8 |
| Occupation | ||
| Unskilled | 95.5 | 100 |
| Skilled | 4.5 | – |
| Employment status, % | ||
| Employed | 9.1 | 5.9 |
| Unemployed | 90.9 | 94.1 |
| Current source of income, % | ||
| Salary | 9.1 | 5.9 |
| social welfare, unemployment compensation | 25.0 | 32.3 |
| health insurance | – | 23.5 |
| disability insurance, SUVA | 31.8 | 14.8 |
| income of spouse | 27.3 | 23.5 |
| no indication | 6.8 | – |
| Ill or unemployed spouse, % | 56.8 | 44 |
| Mean of years in Switzerland; range | 19; 4–34 | 18; 6–34 |
| Reason of immigration, % | ||
| accompaniment of spouse or parents | 65.9 | 52.9 |
| economic reasons | 18.2 | 20.6 |
| political reasons | 15.9 | 20.6 |
| other | – | 5.9 |
| CsCBT = Culturally sensitive cognitive behavioural therapy; CsET = Culturally sensitive exercise therapy NOTE: Some percentages do not total 100% due to missing data * Multiple answers are possible | ||
The trial was carried out at the Department of Psychosomatic Medicine University of Basel Hospital and was planned as a randomised intervention trial with an active treatment group and a control group who received an equal amount of therapist attention: exercise therapy plus playful activities. An active control group was chosen because there is some evidence that both therapies, a CBT approach and exercise therapy are more effective than a waiting list control group [48–53].
The anonymity of the patients’ data was retained and informed consent was received according to the requirements of the institutional ethical review board. The trial protocol was approved by the Ethical Committee of Canton of Basel on 9 September 2004 (207/04).
First-generation Turkish immigrants in Switzerland suffering from chronic pain, 20–65 years of age, were enrolled in the trial. Patients were referred either from general practitioners, from the outpatient unit of the Hospital or from other clinics in Basel or the region. We defined chronic pain in accordance with the German version of International classification of diseases (ICD) 10: The predominant complaint was severe and distressing pain of more than 6 months duration, which cannot be explained fully by a physiological process or a physical disorder. Psychological factors are assumed to contribute significantly to intensity, exacerbation or persistence of pain (http://www.icd-code.de/icd/code/F45.41.html).
Exclusion criteria among patients were the following: (1.) evidence of physical disability preventing participation in physiotherapeutic exercises, (2.) a request for asylum was pending, (3.) documented behaviour indicating a lack of minimal motivation or inability to cooperate with therapists or other group participants, or (4.) specific conditions, i.e., organic brain syndromes, schizophrenia, affective psychosis, bipolar affective disorders, illegal substance abuse or addiction, dissociative disorders, or pronounced symptoms of post-traumatic stress disorder.
Both patient groups received the same trial information sheet and completed informed consent.
Patients were randomly allocated to attend either culturally sensitive cognitive-behavioural treatment (CsCBT) or culturally sensitive exercise treatment (CsET). Both interventions comprised twenty-five 90-minute sessions within a six-month period and were adapted concerning structural and didactic aspects to a culturally sensitive context.
The CsCBT intervention was based upon a manualised cognitive-behavioural group treatment programme for chronic pain [54] and combined cognitive behavioural principles with culturally sensitive migration-specific elements. Cognitive behavioural approaches focus on the way individuals cope with their pain, instead of assuming that a biological reason for the pain can be identified and treated. Interventions include patient information about the origin of chronic pain, identification of aspects in life that are less affected by pain, and areas that are linked to positive experiences. As part of a behavioural component patients are advised to make bodily experiences by using stretching and strengthening exercises.
The CsET intervention was based on principles of exercise therapy for treatment of non-specific low back pain. Exercise therapy (ET) is defined as “a series of specific movements with the aim of training or developing the body by a routine practice or as physical training to promote good physical health” [55].
Structural adaptations for each of the two interventions included (a) the separation of male and female patients into different groups, (b) an increase in the number of sessions from 14 in the original programme, to 25 in ours,( c) sessions being conducted in Turkish with the aid of an interpreter. Didactic adaptations also took account of the educational level of our sample. The use of written materials was limited in order not to exclude illiterate patients. When written material was used, it contained graphical displays, e.g., for exercises or of the vicious cycle between emotion (a weeping eye), muscle tension (a bent arm) and pain (a painful face).
Groups were co-led by a licensed clinical psychologist and a physiotherapist, both German speaking. The clinical psychologist had extensive prior experience delivering CBT to immigrants with chronic pain. The CsET intervention was conducted by a German-speaking physiotherapist. Since most patients lacked sufficient comprehension of the German language, a Turkish interpreter was required in both interventions. The interpreters were certified by the Swiss organisation for Interpreters as medical professional interpreters, and most of them had already been cooperating with our department for more than four years. They were integrated in the therapist team and received continuous supervision by the first author.
The primary endpoint with respect to efficacy of CsCBT was improvement in physical functioning and mental health from baseline to 12 months after the intervention, as measured by the Short Form 36 (SF-36) in the subscales Physical Functioning and Mental Health [56]. Additional analyses were performed on quality of life in the remaining subscales of the SF-36, depression was measured with the General Health Questionnaire (GHQ) [57], disability was measured with the Pain Disability Index (PDI) [58]. Healthcare costs incurred by the patient, within three months preceding vsafter the intervention, were analysed retrospectively by gathering information from insurance companies.
All subjects were first tested after enrolment in the trial (T1), then after completion of the intervention (T2), and finally after twelve months follow-up (T3). Both groups followed the same assessment protocol.
Semistructured interviews were all translated by trained interpreters. Standardised tests were filled in either by the patient him- or herself or, in the case of illiteracy, together with the interpreter.
1. The revised semistructured Interview of Clinical Symptoms (SICS-R) describes pain history, symptoms, and cognitive and emotional aspects that influence pain.
2. Pain drawings allowed the identification of topographical distribution of pain to be quantitatively recorded.
3. A visual analogue scales (VAS) was used to quantify the intensity of subjective pain.
4. The Turkish translation of the Short Form 36 (SF-36) assessed quality of life in chronic patients for the following scales: physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role and mental health.
5. The validated Turkish version of the General Health Questionnaire (GHQ; Kiliç [59]) is a screening instrument for psychopathological symptoms in general healthcare. The 28-item scale includes four dimensions, somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression.
6. The validated Turkish version of the Pain Disability Index (PDI) [60] assesses the extent of pain-related interference performing activities considered normal for a particular age group.
7. Healthcare utilisation costs for the period of three months before and after participation of the patient in the intervention were calculated by Swiss insurance companies.
Based upon previous experience with the intervention, we expected a treatment-related improvement with an average effect size (Cohen’s d) of 0.6 on the SF-36 primary outcome scales of physical functioning and emotional health (based on published norms, http://www.sf-36.org/research/sf98norms.pdf), manifesting positive outcomes in these two primary outcome variables (α = 0.025): With 45 patients per group, this yielded a power of above 80% in power analyses. We planned to have equal numbers of men and women and to randomise 60 patients in both treatment arms per year (15 men and 15 women in the CsCBT and in the CsET per year, respectively). To include a sufficient number of patients in each arm, we repeated the intervention in the same manner during the second year.
A computer-generated randomisation list was drawn up for each gender by a statistician of the Basel Institute of Clinical Epidemiology. Details of the series were not known to any of the investigators. Allocation concealment was guaranteed through sequentially numbered, opaque, sealed envelopes enclosing assignments. The envelopes were handed over to the research psychologist after intake interviews were completed. Patients had an equal probability of assignment to each groups. The randomisation took place after the initial assessments and was immediately communicated to patients.
All initial and follow-up interviews were conducted by a research psychologist not involved in the treatment. Blinded assessments were not feasible for follow-up meetings because patients inevitably relayed information about their treatment experiences to the research psychologist.
Treatment effects, (means and standard deviations (SDs), were estimated at post-treatment and 12 months follow-up for the primary outcomes (two items of SF-36) and secondary outcomes, which included the other six subscales of the SF-36, the GHQ, the PDI, a visual analogue pain rating scale (VAS), and healthcare costs. Significance levels were p <0.05 (two-tailed analyses). For the questionnaire data and pain rating, change scores (post-treatment or 12 month-follow-up minus pretreatment levels) were computed, and groups were compared employing general linear models, after covariate adjustment for baseline levels of each measure. Independent t-test analyses were used to examine possible differences in healthcare costs between groups. CSS Statistica was employed for all statistical analyses (StatSoft, Inc. STATISTICA (data analysis software system), version 6.0. www.statsoft.com http://www.sf-36.org/research/sf98norms.pdf ).
| Table 2: Clinical characteristics of group members as collected in the Semistructured Interview. | ||
| Characteristic | CsCBT group(n = 44) | CsET group (n = 34) |
| Mean pain chronicity; range, y | 4; 1/2‒17 | 6; 1‒30 |
| Pattern of pain, % | ||
| Permanent pain | 88.6 | 82.4 |
| Several times daily | 9.1 | 14.7 |
| Several times weekly | 2.3 | 2.9 |
| Negative modulation of pain*, % | ||
| Weather | 65.9 | 61.8 |
| Stress | 50.0 | 67.6 |
| Physical strain | 70.5 | 52.9 |
| Pain trigger*, % | ||
| Illness | 9.1 | 2.9 |
| Accident | 25.0 | 35.3 |
| Workload strain | 25.0 | 35.3 |
| Traumatic life events, death in the family | 15.9 | 14.7 |
| Stress and conflict in the family | 11.4 | 11.8 |
| Migration | 2.3 | 8.8 |
| Pregnancy, surgical operation | 11.4 | 26.5 |
| Violent experience | 2.3 | 5.9 |
| Indefinite triggers | 29.5 | 20.6 |
| Do patients recognise any connection between their chronic pain and psychosocial stress? % | ||
| yes | 52.3 | 61.8 |
| none | 47.7 | 38.2 |
| Mood disorders, % | ||
| Mild depressive episode | 27.3 | 44.1 |
| Moderate depressive episode | 27.3 | 32.4 |
| Severe depressive episode | 4.6 | – |
| None | 22.6 | 14.7 |
| Missing data | 18.2 | 8.8 |
| Anxiety disorders, % | ||
| yes | 27.3 | 11.7 |
| none | 72.7 | 88.3 |
| Persistent somatoform pain disorder, % | ||
| yes | 79.5 | 88.2 |
| none | 20.5 | 11.8 |
| CsCBT = Culturally sensitive cognitive behavioural therapy; CsET = Culturally sensitive exercise therapy | ||
Eligible participants were recruited from September 2004 to March 2007. Figure 1 is a flowchart of the trial. A total of 158 potentially eligible patients with chronic pain were referred, 146 patients agreed to take part in the trial. A total of 116 patients completed the pre-trial assessment and were found to be eligible, consented, and were randomised.
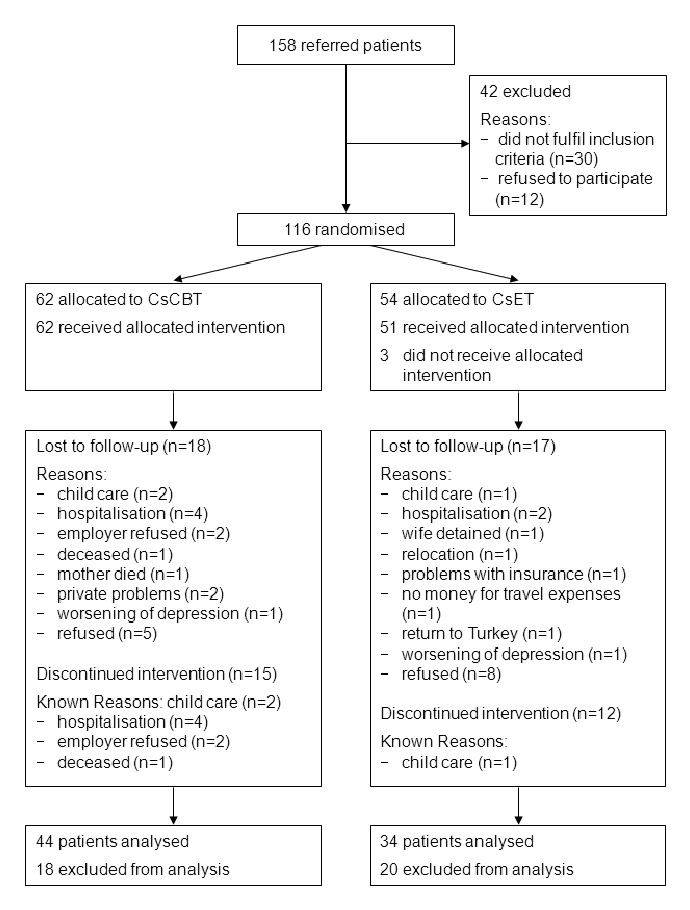
Figure 1
Flow chart of participants.
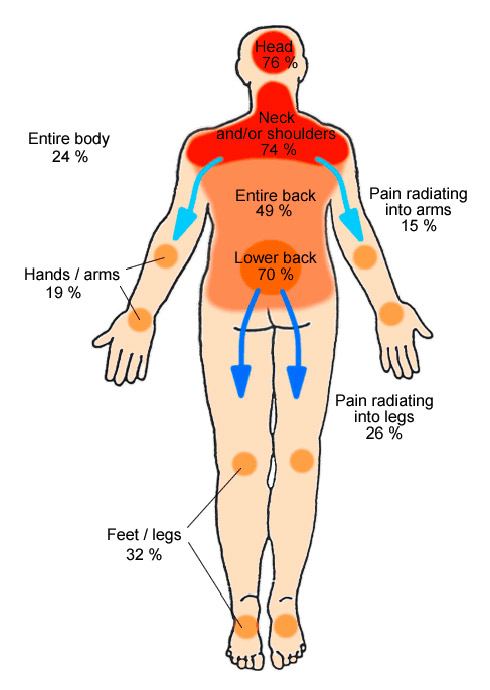
Figure 2
Graphical display of pain localisation, reported by the patients on a sketch as shown. Multiple responses were allowed (n = 114).
At the follow-up 12 months later, the drop-out rate for both groups was quite high: 29% with CsCBT and 37% with CsET. Only a small percentage refused therapy, 6% in the CsCBT group and 15% in the CsET group. Most patients gave plausible reasons not to continue to attend group therapy. Their reasons are listed in figure 1.
There was one protocol violation regarding the recruitment of men. We could not recruit as many male patients as we had planned. We chose to include more female participants to obtain a sufficient number of patients, but at the same time had to abstain from analysing data separately for men and women.
Baseline demographic characteristics are presented in table 1. Examination of demographic characteristics at baseline showed only one difference between groups: a larger percentage of participants in CsET reported that compensation from health insurance was their main source of income. Mean age was 43.9 years (range 29–61). Overall, 61% of patients were of Turkish and 38 % were of Kurdish origin; 54% of patients had formal education of five years or less; 22% of patients were illiterate. Almost all (98%) had worked as unskilled workers in the cleaning business or in construction. The majority (92%) of patients were unemployed at enrolment.
Baseline clinical characteristics of trial groups are presented in table 2. In the majority of patients pain was distributed among multiple regions of the body (fig. 2).
Participants were tested after randomisation (baseline) and again after their participation in the intervention, and finally after 12 months follow-up. Of 116 randomly assigned participants, a total of 87 were included in the analysis of baseline and post-treatment effects, and 78 patients in the analysis of the difference between baseline and follow-up 12 months later. Intention-to-treat analyses were not performed owing to lack of significant effects (the three significant findings reported in table 3 can be attributed to chance as a result of the multiplicity of comparisons).
Primary and secondary outcome scores of SF-36, GHQ and PDI for men and women in both groups showed no improvement, neither at short term follow-up after three months, nor at long-term follow-up at 12 months (table 3). Interestingly, the SF-36 scores were extremely low, indicating low levels of quality of life and functioning (see table 3). The same was true for any single score of the SF-36.
The same holds for GHQ scores which indicated low quality of life and showed no improvement in either group. The pain disability index demonstrated a high pre-intervention level of disability due to chronic pain.
The analysis of pain intensity (VAS) presented in table 4 showed no significant change.
Health insurance companies provided the data on healthcare procedures and costs for 105 patients. Again, there was no significant difference before and after treatment, or between groups.
Patients also evaluated the therapy in the semistructured interviews in a less formal way: 80 percent of participants claimed to be satisfied with the intervention. Patients especially liked that the therapy was offered in their mother tongue.
| Table 3:Tests of change ccores during treatment at post-treatment and follow-up. | ||||||||||
| Primary outcomes | Group | Baseline scores | Change: baseline to post-treatment | Change: baseline to 12-month follow-up | ||||||
| Mean | Lower 95% CI | Upper 95% CI | Mean Change | Lower 95% CI | Upper 95% CI | Mean Change | Lower 95% CI | Upper 95% CI | ||
| Physical functioning (SF-36)** | CsCBT | 32.22 | 27.57 | 36.87 | –1.74 | –7.44 | 3.96 | –3.30 | –11.45 | 4.85 |
| CsET | 32.92 | 28.22 | 37.62 | –2.75 | –9.17 | 3.67 | –4.79 | –13.95 | 4.37 | |
| Mental health (SF-36)** | CsCBT | 42.53 | 39.23 | 45.83 | 2.36 | –1.94 | 6.66 | 1.39 | –5.52 | 8.30 |
| CsET | 44.63 | 39.99 | 49.27 | 2.46 | –3.92 | 8.84 | 4.59 | -2.85 | 12.03 | |
| Secondary outcomes | ||||||||||
| Physical role (SF-36)** | CsCBT | 4.17 | 0.95 | 7.39 | 5.85* | –1.52 | 13.22 | –1.14 | –9.75 | 7.47 |
| CsET | 1.56 | –0.12 | 3.24 | –4.38* | –9.85 | 1.09 | –2.21 | –8.68 | 4.26 | |
| Bodily pain (SF-36)** | CsCBT | 47.17 | 39.08 | 55.26 | .87 | –3.79 | 5.53 | –3.05 | –9.22 | 3.12 |
| CsET | 52.41 | 42.36 | 62.46 | –5.50 | –10.46 | -0.54 | –3.09 | –9.16 | 2.98 | |
| General health (SF-36)** | CsCBT | 54.06 | 47.90 | 60.22 | 1.21 | –3.60 | 6.02 | –.80 | –6.07 | 4.47 |
| CsET | 52.55 | 45.48 | 59.62 | –1.79 | –6.83 | 3.25 | 2.42 | –4.35 | 9.19 | |
| Vitality (SF-36)** | CsCBT | 37.50 | 33.03 | 41.97 | .04 | –5.11 | 5.19 | .23 | –7.23 | 7.69 |
| CsET | 43.13 | 38.25 | 48.01 | 1.75 | –5.36 | 8.86 | 5.88 | –2.63 | 14.39 | |
| Social functioning (SF-36)** | CsCBT | 45.49 | 40.93 | 50.05 | 2.39 | –4.82 | 9.60 | –3.69 | –12.25 | 4.87 |
| CsET | 50.39062 | 44.48 | 56.30 | 3.75 | –4.47 | 11.97 | 6.25 | –5.81 | 18.31 | |
| Role-emotional (SF-36)** | CsCBT | 4.63 | 0.04 | 9.22 | 2.84 | –6.02 | 11.70 | –7.58 | –19.47 | 4.31 |
| CsET | 12.50 | 3.93 | 21.07 | .83 | –9.40 | 11.06 | 5.05 | –5.70 | 15.80 | |
| Physical symptoms (GHQ)*** | CsCBT | 13.61 | 12.56 | 14.66 | .23 | –1.27 | 1.73 | –1.23 | –2.92 | 0.46 |
| CsET | 13.47 | 12.16 | 14.78 | .95 | –0.79 | 2.69 | –1.29 | –3.18 | 0.60 | |
| Anxiety (GHQ)*** | CsCBT | 13.42 | 12.30 | 14.54 | .87 | –0.57 | 2.31 | –.84 | –2.45 | 0.77 |
| CsET | 12.41 | 11.03 | 13.79 | .54 | –1.26 | 2.34 | –.03 | –2.02 | 1.96 | |
| Impairment of social functioning (GHQ)*** | CsCBT | 13.89 | 12.85 | 14.93 | 1.49 | 0.06 | 2.92 | –.37 | –1.93 | 1.19 |
| CsET | 13.19 | 11.97 | 14.41 | 1.10 | –0.48 | 2.68 | –1.18 | –3.11 | 0.75 | |
| Depression (GHQ)*** | CsCBT | 9.06 | 7.94 | 10.18 | –.91 | –2.39 | 0.57 | –.95 | –2.78 | 0.88 |
| CsET | 8.78 | 7.25 | 10.31 | .72 | –1.08 | 2.52 | –1.12 | –3.15 | 0.91 | |
| Pain Disability Index (PDI)**** | CsCBT | 38.96 | 35.40 | 42.52 | 1.35 | –3.22 | 5.92 | .60 | –4.54 | 5.74 |
| CsET | 40.72 | 36.55 | 44.89 | 4.98 | 0.81 | 9.15 | .76 | –4.85 | 6.37 | |
| CI = confidence interval; CsCBT = Culturally sensitive cognitive behavioural therapy; CsET = Culturally sensitive exercise therapy ** The percentage scores range from 0% (lowest or worst possible level of functioning) to 100% (highest or best possible level of functioning). *** Simple Likert Scoring 0-1-2-3 measuring symptoms from ‘not all’ to ‘much more than usual’ **** Scoring 0-1-2-3-4-5-6-7: 0 – no disability, 7 – worst disability | ||||||||||
| Table 4: Means and standard seviations (SD) of pain intensity on a visual analogue scale (0–10). | |||||||
| Secondary outcomes | Group | Pretreatment | Post-treatment | 12-Month follow-up | |||
| Mean | SD | Mean | SD | Mean | SD | ||
| Pain intensity (visual analogue scale) | CsCBT | 7.38 | 1.99 | 7.62 | 1.60 | 7.43 | 1.91 |
| CsET | 7.47 | 2.12 | 7.42 | 1.89 | 7.50 | 1.96 | |
| Pooled | 7.42 | 2.03 | 7.53 | 1.71 | 7.46 | 1.92 | |
| CsCBT = Culturally sensitive cognitive behavioural therapy; CsET = Culturally sensitive exercise therapy | |||||||
| Table 5:Means and standard deviations of healthcare utilisation (estimated yearly costs in Swiss Francs). | ||||||
| Secondary outcome | Group* | Pretreatment | Post-treatment | p | ||
| Mean | SD | Mean | SD | |||
| Healthcare costs** | CsCBT | 8,112 | 17,412 | 8,592 | 19,040 | |
| CsET | 2,156 | 2,604 | 2,996 | 6,720 | ||
| Pooled | 5,444 | 13,344 | 6,088 | 15,048 | 0.704 | |
| CsCBT = Culturally sensitive cognitive behavioural therapy; CsET = Culturally sensitive exercise therapy * Estimated yearly healthcare costs based on 3 months before intervention and 3 months after intervention. **Costs were calculated according to Tarmed (health cost scale of Swiss Medical Association) | ||||||
Sixty-nine percent of our patients successfully completed the intervention, which indicates that long-term behavioural interventions on an out-patient basis is generally feasible in this patient group. Also, anecdotal feedback from patients indicated a broad acceptance of the intervention. We have no indication of any significant difference between participants who were included at the beginning of the intervention and later dropped out, and those who generated data at the end of the intervention. These findings are important, in themselves, in suggesting that first-generation Turkish immigrants in Switzerland suffering from chronic pain are amenable to long-term interventions of a behavioural nature that attempt to be culturally sensitive. On the other hand, the general lack of treatment effects was disappointing: There was no significant or clinically relevant improvement at the 12month follow-up in any of the major outcome measures, including the SF-36, GHQ, PDI or in VAS pain. Modest beneficial effects of two SF-36 scales, assessed directly after treatment, were no longer found 12 months later. Healthcare costs remained unchanged from before to after therapy.
Although the intervention showed no improvement in standardised assessment scales, 80% of participating patients in both groups reported satisfaction with the intervention. In fact, many expressed regret that the intervention could not continue beyond six months. This might point to a mismatch between study assessments of treatment efficacy, on the one hand, and patient perception of their own personal benefit, on the other. Given the fact that similar CBT-based interventions have been shown to work well in other populations [45, 47–49, 61] (with one exception [62]), one might consider whether the apparent failure of the intervention had to do with the particular needs of the population under study. We certainly attempted to pay attention to the specific cultural factors of the patient population, mostly from rural Turkey, and adjusted the intervention accordingly. Still, one must consider if more intensive therapy might have yielded better results, although the limited evidence available regarding in-patient treatment of migrant patients suffering from chronic pain, even with a much higher intensity of treatment than ours, has not shown impressive results [63–66].
On the other hand, one might question whether the assessment strategy was conceived in a sufficiently culturally sensitive manner in respect to several dimensions considered below.
The population under study certainly was unique. In contrast to other patient groups previously described, Turkish-speaking patients in our sample showed a strikingly low quality of life as assessed with the SF-36 [67], and were characterised by very low levels of education and a severe lack of socioeconomic resources. They suffered from a combination of economic stress and many emotional burdens in terms of family stresses, e.g., compromised family members as illustrated in the high percentage of chronically ill spouses (see table 1). Future prospect of work for our patients remained grim: Before acquiring their pain syndrome, they had typically been performing heavy physical work, were unskilled and had poor language competence. During disability and the period of unemployment, they also almost certainly became physically deconditioned. Frequently they sought to improve their financial situation by applying for disability benefits. However, during the period of our trial, the Swiss Court issued a decision that rescinded the previous eligibility of chronic pain as a ground for early retirement disability. If we assume that self-reported evaluations of pain are also expressions of a more general statement of “not being well”, patients may have been reluctant to acknowledge in test results that they were getting better, out of fear of further reducing their chances of disability benefits.
We chose questionnaires that had validated in Turkish populations to increase the likelihood of obtaining reliable data. However, these instruments had been validated among samples significantly different from the population that we studied: respondents were much better educated and had a substantially higher socioeconomic status [54]. Assessment instruments for the kind of participants in this study do not yet exist, and it seems very plausible that they might not be appropriate, reliable or valid for this population. Thus it is possible that the global feedback of satisfaction with the programme provided the only reasonably accurate indication of patient perception. In any case, this study highlights the need for development of measurement instruments that can demonstrate properties of validity and reliability for such poorly educated immigrant populations ‒ populations very much a reality in Western European countries.
As one example of disparities regarding our patient sample and others, in terms of levels of health-related quality of life, participants in our study differed from every other comparison group with which we are familiar: All scores on emotional, social and physical role functioning were extremely low [67]. It remains unclear whether the SF-36 is a valid instrument for an immigrant patient group in which one-fifth is illiterate, or whether the SF-36 accurately describes these patients’ state of well-being. Of course, it is possible that the level of despair, despondency and resignation, often enough articulated by patients, were, indeed, reflected by quality of life scores, and that the level of intervention was insufficient to address the enormous adversities of these patients. In any case, until properly validated assessment instruments are developed for such populations, it may be impossible to determine efficacy of interventions or to explore relationships among salient variables in such groups.
In conclusion, our investigation suggests a very incipient state of knowledge in research on immigrants with low educational background who suffer from long-term pain. As a feasibility study, the study was highly successful at motivating participants to attend, and they appeared genuinely satisfied with a six-month programme of culturally sensitive cognitive-behavioural intervention. Nevertheless, our findings cast doubt over aspects of validity and reliability of outcome measures in this population. Our results may also call into question the adequacy of psychotherapeutic intervention as the sole strategy to help immigrants with chronic pain. Since the life challenges of this population are often so overwhelming, a far broader approach may be necessary that includes far greater efforts to integrate such individuals into their host society and workforce. Perhaps only then may CBT or alternative interventions begin to show positive results. Finally, despite our lack of positive findings, this intervention trial will hopefully stimulate further efforts to address a problem that saps both the human spirit and societal resources.
Implications of this research: Given the fact that we observed no changes at all, even no pooled effects, the lack of findings cannot be attributed to our employment of an active control intervention procedure. Additionally, given the absence of even tendencies toward effects of treatment, it is hard to argue that an increase in the number of participants (and hence the power of the analysis) might have been beneficial for detection of reliable treatment effects. One possibility is that our choice of assessment instruments did not target the underlying problem of these patients? Perhaps more fundamentally, one might wish to question, in the first place, whether such an immigrant population with chronic pain suffers ‘pain’ from the cultural understanding defined by a Western taxonomy, or whether the term “pain” refers more to a fundamental sense of ‘ill-being’ that simply cannot be addressed by a pain-oriented treatment program.
Acknowledgement: The study was financed by Swiss National Funding Programme “Chronic Musculoskeletal Pain”.
1 Allison TR, Symmons DP, Brammah T, Haynes P, Rogers A, Roxby M, et al. Musculoskeletal pain is more generalised among people from ethnic minorities than among white people in Greater Manchester. Ann Rheum Dis. Vol. 61, 2002:151–6.
2 Rogers A, Allison T. What if my back breaks? Making sense of musculoskeletal pain among South Asian and African-Caribbean people in the North West of England. J Psychosom Res. 2004;57:79–87.
3 Palmer B, Macfarlane G, Afzal C, Esmail A, Silman A and Lunt M. Acculturation and the prevalence of pain amongst South Asian minority ethnic groups in the UK. Rheumatology. (Oxford) 2007;46:1009–14.
4 Campbell CM, Edwards RR, Fillingim RB. Ethnic differences in responses to multiple experimental pain stimuli. Pain. 2005;113:20–6.
5 Watson PJ, Latif RK. Rowbotham DJ. Ethnic differences in thermal pain responses: a comparison of South Asian and White British healthy males. Pain. 2005;118:194–200.
6 Komiyama O, Kawara M, De Laat A. Ethnic differences regarding tactile and pain thresholds in the trigeminal region. J Pain. 2007;8:363–9.
7 Rahim-Williams FB, Riley JL, 3rd, Herrera D, Campbell CM, Hastie BA, Fillingim RB. Ethnic identity predicts experimental pain sensitivity in African Americans and Hispanics. Pain. 2007;129:177–84.
8 Campbell CM, France CR, Robinson ME, Logan HL, Geffken GR. Fillingim RB. Ethnic differences in the nociceptive flexion reflex (NFR). Pain. 2008;134:91–6.
9 Baker TA. Chronic pain in older Black Americans: the influence of health and psychosocial factors. Ethn Dis. 2005;15:179–86.
10 Baker TA, Green CR. Intrarace differences among black and white Americans presenting for chronic pain management: the influence of age, physical health, and psychosocial factors. Pain Med. 2005;6:29–38.
11 David M, Braun T and Borde T. Pain and ethnicity – results of a survey at three internal/gynecological first-aid stations in Berlin. Zentralbl Gynakol. 2004;126:81–6.
12 Edwards RR, Doleys DM, Fillingim RB and Lowery D. Ethnic differences in pain tolerance: clinical implications in a chronic pain population. Psychosom Med. 2001;63:316–23.
13 Faucett J, Gordon N and Levine J. Differences in postoperative pain severity among four ethnic groups. J Pain Symptom Manage. 1994;9:383–9.
14 Gepstein R, Arinzon Z, Folman Y, Shabat S, Adunsky A. Lumbar spine surgery in Israeli Arabs and Jews: a comparative study with emphasis on pain perception. Isr Med Assoc J. 2007;9:443–7.
15 Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4:277–94.
16 Green CR, Baker TA, Sato Y, Washington TL, Smith EM. Race and chronic pain: A comparative study of young black and white Americans presenting for management. J Pain. 2003;4:176–83.
17 Green CR, Baker TA, Smith EM and Sato Y. The effect of race in older adults presenting for chronic pain management: a comparative study of black and white Americans. J Pain. 2003;4:82–90.
18 Green CR, Ndao-Brumblay SK, Nagrant AM, Baker TA, Rothman E. Race, age, and gender influences among clusters of African American and white patients with chronic pain. J Pain. 2004;5:171–82.
19 Griffiths B, Situnayake RD, Clark B, Tennant A, Salmon M, Emery P. Racial origin and its effect on disease expression and HLA-DRB1 types in patients with rheumatoid arthritis: a matched cross-sectional study. Rheumatology. (Oxford) 2000;39:857–64.
20 Im EO, Chee W, Guevara E, Liu Y, Lim HJ, Tsai HM, et al. Gender and ethnic differences in cancer pain experience: a multiethnic survey in the United States. Nurs Res. 2007;56:296–306.
21 McCracken LM, Matthews AK, Tang TS, Cuba SL. A comparison of blacks and whites seeking treatment for chronic pain. Clin J Pain. 2001;17:249–55.
22 Ndao-Brumblay SK, Green CR. Racial differences in the physical and psychosocial health among black and white women with chronic pain. J Natl Med Assoc. 2005;97:1369–77.
23 Norrefalk JR, Ekholm J and Borg K. Ethnic background does not influence outcome for return-to-work in work-related interdisciplinary rehabilitation for long-term pain: 1- and 3-year follow-up. J Rehabil Med. 2006;38:87–92.
24 Riley JL, 3rd, Wade JB, Myers CD, Sheffield D, Papas RK, Price DD. Racial/ethnic differences in the experience of chronic pain. Pain. 2002;100:291–8.
25 Ruehlman LS, Karoly P, Newton C. Comparing the experiential and psychosocial dimensions of chronic pain in african americans and Caucasians: findings from a national community sample. Pain Med. 2005;6:49–60.
26 Taylor BA, Casas-Ganem J, Vaccaro AR, Hilibrand AS, Hanscom BS and Albert TJ. Differences in the work-up and treatment of conditions associated with low back pain by patient gender and ethnic background. Spine. (Phila Pa 1976) 2005;30:359–64.
27 Vlaar AP, ten Klooster PM, Taal E, Gheith RE, El-Garf AK, Rasker JJ, et al. A cross-cultural study of pain intensity in Egyptian and Dutch women with rheumatoid arthritis. J Pain. 2007;8:730–6.
28 Yazici Y, Kautiainen H and Sokka T. Differences in clinical status measures in different ethnic/racial groups with early rheumatoid arthritis: implications for interpretation of clinical trial data. J Rheumatol. 2007;34:311–5.
29 Edwards RR, Moric M, Husfeldt B, Buvanendran A, Ivankovich O. Ethnic similarities and differences in the chronic pain experience: a comparison of african american, Hispanic, and white patients. Pain Med. 2005;6:88–98.
30 Lofvander MB, Engstrom AW. The immigrant patient having widespread pain. Clinical findings by physicians in Swedish primary care. Disabil Rehabil. 2007;29:381–8.
31 Neumann L, Buskila D. Ethnocultural and educational differences in Israeli women correlate with pain perception in fibromyalgia. J Rheumatol. 1998;25:1369–73.
32 Weisenberg M, Caspi Z. Cultural and educational influences on pain of childbirth. J Pain Symptom Manage. 1989;4:13–9.
33 Bonham VL. Race, ethnicity, and pain treatment: striving to understand the causes and solutions to the disparities in pain treatment. J Law Med Ethics. 2001;29:52–68.
34 Chibnall JT, Tait RC, Andresen EM, Hadler NM. Race differences in diagnosis and surgery for occupational low back injuries. Spine. (Phila Pa 1976) 2006;31:1272–5.
35 Nguyen M, Ugarte C, Fuller I, Haas G and Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6:301–14.
36 Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299:70–8.
37 Portenoy RK, Ugarte C, Fuller I, Haas G. Population-based survey of pain in the United States: differences among white, African American, and Hispanic subjects. J Pain. 2004;5:317–28.
38 Green CR, Baker TA, Ndao-Brumblay SK. Patient attitudes regarding healthcare utilization and referral: a descriptive comparison in African- and Caucasian Americans with chronic pain. J Natl Med Assoc. 2004;96:31–42.
39 Soares JJ, Grossi G. Experience of musculoskeletal pain. Comparison of immigrant and Swedish patient. Scand J Caring Sci. 1999;13:254–66.
40 Kavuk I, Weimar C, Kim BT, Gueneyli G, Araz M, Klieser E, et al. One-year prevalence and socio-cultural aspects of chronic headache in Turkish immigrants and German natives. Cephalalgia. 2006;26:1177–81.
41 Jordan MS, Lumley MA, Leisen JC. The relationships of cognitive coping and pain control beliefs to pain and adjustment among African-American and Caucasian women with rheumatoid arthritis. Arthritis Care Res. 1998;11:80–8.
42 Tan G, Jensen MP, Thornby J and Anderson KO. Ethnicity, control appraisal, coping, and adjustment to chronic pain among black and white Americans. Pain Med. 2005;6:18–28.
43 Cano A, Mayo A and Ventimiglia M. Coping, pain severity, interference, and disability: the potential mediating and moderating roles of race and education. J Pain. 2006;7:459–68.
44 Hastie BA, Riley JL, 3rd and Fillingim RB. Ethnic differences in pain coping: factor structure of the coping strategies questionnaire and coping strategies questionnaire-revised. J Pain. 2004;5:304–16.
45 Lasch KE. Culture, pain, and culturally sensitive pain care. Pain Manag Nurs. 2000;1:16–22.
46 Davidhizar R, Giger JN. A review of the literature on care of clients in pain who are culturally diverse. Int Nurs Rev. 2004;51:47–55.
47 Lo HT, Fung KP. Culturally competent psychotherapy. Can J Psychiatry. 2003;48:161–70.
48 Molton IR, Graham C, Stoelb BL, Jensen MP. Current psychological approaches to the management of chronic pain. Curr Opin Anaesthesiol. 2007;20:485–9.
49 Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999;80:1–13.
50 van Tulder MW, Ostelo R, Vlaeyen JW, Linton SJ, Morley SJ and Assendelft WJ. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane Back Review Group. Spine. (Phila Pa 1976) 2000;25:2688–99.
51 van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomized controlled trials of the most common interventions. Spine. (Phila Pa 1976) 1997;22:2128–56.
52 Smeets RJ, Vlaeyen JW, Hidding A, Kester AD, van der Heijden GJ, van Geel AC, et al. Active rehabilitation for chronic low back pain: cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229]. BMC Musculoskelet Disord. 2006;7:5.
53 Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. Bmj. 2001;322:1511–6.
54 Basler H-D. Chronische Kopf- und Rückenschmerzen. Psychologisches Trainingsprogramm. Göttingen: Vandenhoeck & Ruprecht, 2001.
55 Abenhaim L, Rossignol M, Valat JP, Nordin M, Avouac B, Blotman F, et al. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. Spine. (Phila Pa 1976) 2000;25:1S–33S.
56 Ware JE, Kosinski M. SF-36 Physical & Mental Health Summary Scales: a manual for users of Version 1. Rhode Island: QualityMetric Incorporated Lincoln, 2004.
57 Goldberg DP, Williams P. A users guide to the General Health Questionnaire. Windsor: NFER-Nelson, 1988.
58 Tait RC, Chibnall JT, Krause S. The Pain Disability Index: psychometric properties. Pain. 1990;40:171–82.
59 Kilic C, Rezaki M, Rezaki B, Kaplan I, Ozgen G, Sagduyu A, et al. General Health Questionnaire (GHQ12 & GHQ28): psychometric properties and factor structure of the scales in a Turkish primary care sample. Soc Psychiatry Psychiatr Epidemiol. 1997;32:327–31.
60 Werries A. Evaluation einer türkischen Fragebogenbatterie zur Erfassung chronischen Schmerzes. Marburg (Dissertation), 1997.
61 Calliess IT, Schmid-Ott G, Akguel G, Jaeger B, Ziegenbein M. Attitudes towards psychotherapy of young second-generation Turkish immigrants living in Germany. Psychiatr Prax. 2007;34:343–8.
62 Johnson RE, Jones GT, Wiles NJ, Chaddock C, Potter RG, Roberts C, et al. Active exercise, education, and cognitive behavioral therapy for persistent disabling low back pain: a randomized controlled trial. Spine. (Phila Pa 1976) 2007;32:1578–85.
63 Nickel C, Lojewski N, Muehlbacher M, Cangoez B, Muller-Rabe T, Buschmann W, et al. Treatment results from inpatient psychosomatic rehabilitation of Turkish migrants: a prospective study. Gesundheitswesen. 2006;68:147–53.
64 Nickel M, Cangoez B, Bachler E, Muehlbacher M, Lojewski N, Mueller-Rabe N, et al. Bioenergetic exercises in inpatient treatment of Turkish immigrants with chronic somatoform disorders: a randomized, controlled study. J Psychosom Res. 2006;61:507–13.
65 Schmeling-Kludas C, Froschlin R, Boll-Klatt A. Inpatient psychosomatic rehabilitation for Turkish migrants: what can be realized, what are the effects? Rehabilitation. (Stuttg) 2003;42:363–70.
66 Rodewig K. Stationäre psychosomatische Rehabilitation von Migranten aus der Türkei. Sind monokulturelle Behandlungseinheiten sinnvoll? Psychotherapeut. 2000;45 350–5.
67 Sleptsova M. Cultural, social and linguistic barriers. Can they be overcome? Asian Hospital & Healthcare. Management. 2009;19:36–8.
Funding/ potential competing interests: The trial was financed by Swiss National Funding Programme “Chronic Musculoskeletal Pain”.