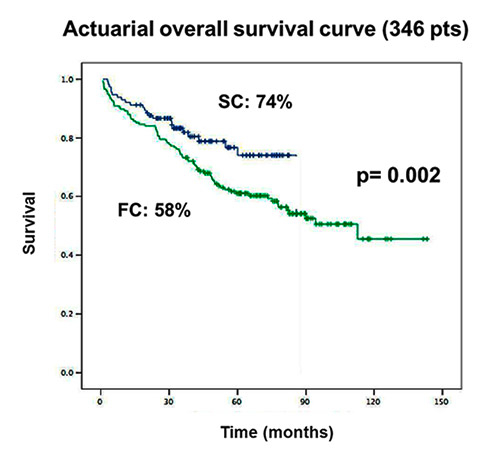
Figure 1
Actuarial overall survival (346 patients); SC: blue; FC: green.
DOI: https://doi.org/10.4414/smw.2013.13858
Despite advances in more accurate diagnoses, improved prosthetic materials, better myocardial and cerebral protection, as well as increased surgical experience, surgery for acute type-A dissection remains an emergency intervention associated with high mortality rates and neurological complications [1, 2]. Long-term survival rates after surgically treated acute type-A aortic dissections are reported to be 52–94% after 1 year and 45–88% after 5 years [3–6].
In regard to cannulation to initialise cardio pulmonary bypass, various techniques are available. Although femoral artery cannulation (FC) has been reported to be the standard cannulation site, it is associated with an increased initial risk of high pressure mal-perfusion into a false lumen which may lead to subsequent brain and visceral damage. On the other hand, subclavian artery cannulation has been demonstrated to be a good alternative since it has two major advantages: SC allows antegrade perfusion of the central nervous system. Furthermore this technique may be performed much easier and safer when compared to the more cumbersome approach of selective cannulation of the cerebral vessels. However, neither mid-term nor long-term results are available in the literature.
The purpose of this study was to assess the long-term results of subclavian artery cannulation versus femoral cannulation for repair of acute type-A dissection. The study aimed to elicit the long-term prevalence and outcomes of the persistence of neurological deficits, mortality and re-operations.
Between January 1992 and December 2005, a total number of 346 patients underwent surgical repair of acute type-A aortic dissection at the University Hospital of Zurich.
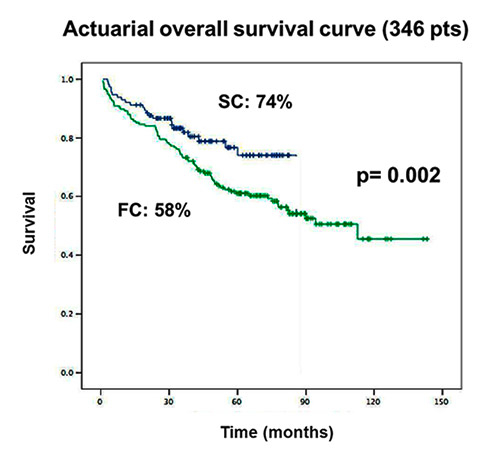
Figure 1
Actuarial overall survival (346 patients); SC: blue; FC: green.

Figure 2
Actuarial survival of hospital survivors (290 patients); SC: blue; FC: green.
After approval from an institutional review board, in this retrospective study, only patients with acute type-A aortic dissection (TA-AAD) who survived the operation and were discharged from the hospital were included (n = 290). Subclavian artery cannulation (SC) was performed in 114 patients. Femoral artery cannulation (FC) was employed in 176 patients.
A standard median sternotomy was performed and cardiopulmonary bypass (CPB) was instituted by cannulating either the femoral artery (FC-group) or the right subclavian artery (SC-group).
The SC group received bilateral radial arterial lines. An additional third line was placed in the right femoral artery for intra-operative pressure monitoring. The right subclavian cannulation was performed either by direct insertion using a 20FR cannula or by an 8 mm Dacron graft anastomosed end to side to the subclavian artery.
During hypothermic circulatory arrest (HCA) generally only the innominate artery was clamped and the brain was selectively antegrade perfused (ACP) with a rate of 800–1000 ml/ min and a temperature of 22–26 °C. Backflow through the left subclavian artery was controlled by means of a balloon catheter (Fogarty) placed in the distal aortic arch or by using an additional clamp when needed.
Cannulation of the right femoral artery was surgically exposed prior to sternotomy. The venous cannulation was performed with a single double-stage cannula via the right atrium. For retrograde cerebral perfusion (RCP) the superior vena cava was cannulated separately and during HCA, this vessel was occluded proximally and perfused with a target flow of 500 ml/min under controlled venous pressure not exceeding 40 mm Hg (18 °C). Before inducing RCP the distal ascending aorta was clamped. After completion of distal anastomosis to the aortic arch, re-warming was started through the cannula introduced into the side arm of the graft.
The patient’s head was wrapped in an ice package during prolonged circulatory arrest. Temperature was measured rectally and nasopharyngeally in all patients. The operative technique for acute type-A aortic dissection encompasses glue-aortoplasty (Gelatine-resorcinol-glutaraldehyde/formaldehyde, Trigon GmbH, Mönchengladbach, Germany) for reconstructing the aortic root, if the preservation of the root integrity was possible. A replacement of the ascending aorta with an open distal anastomosis during an interval of HCA was always performed and the primary tear was resected whenever possible. The use of felt or glue was left to the surgeon’s discretion.
Intra-operative neurological monitoring was performed by bispectral index EEG (Aspect® Medical Systems, Leiden, The Netherlands) for an indirect control of brain perfusion. In addition, size and reaction of the pupils were permanently controlled during the procedure.
The presence of neurological dysfunction at the time of discharge from the hospital was divided into four categories and assessed by a neurologist:
a) no symptoms
b) mild: agitation; confusion; transient delirium; all with complete and post-operative remission, negative CT-scan;
c) moderate: facial palsy, amaurosis fugax, hemi-sensory loss;
d) severe: coma, stroke confirmed by CT-scan.
Final neurological outcome classification was divided into two categories: type I was defined as death due to stroke or hypoxic encephalopathy, non-fatal stroke, transient ischemic attack (TIA), or stupor or coma at the time of discharge; and type II was defined as a new deterioration in intellectual function, confusion, agitation, disorientation, memory deficit, or seizure without evidence of focal injury (table 4).
All patients who survived the operation were followed up with a questionnaire to assess for the general health condition of the patient, hospitalisation for cardiac and non-cardiac reasons, the occurrence of stroke as well as any other major cardiac or cerebrovascular event.
The statistical software package SPSS 15.0 (SPSS Inc., Chicago, IL) was used for statistical analysis. Continuous variables were summarised as mean ± standard deviation. In univariate analysis discrete variables were analysed by the chi-square or Fisher’s exact test where appropriate. Continuous variables were analysed by the Mann–Whitney test. Statistical significance was associated with a p-value of less than 0.05. The overall survival, disease free survival and freedom from re-operation were analysed using Kaplan-Meier curves and were compared using the log-rank test.
| Table 1: Demographics. | ||
| SC | FC | |
| Age (18–83) (yrs) | 32–83 | 18–80 |
| Mean age (yrs) | 61 ± 13 | 58 ± 12 |
| Gender (f/m) | 34/80 | 41/135 |
| Follow-up complete 259 / 290 (89.5%) | 3–83 months | 2–143 months |
| Lost to Follow-up 31 / 290 (10.5%) | 16 | 15 |
| SC: Subclavian artery cannulation; FC: Femoral artery cannulation | ||
| Table 2: Aetiologies of deaths after hospital discharge. | |||
| Aetiologies of deaths after hospital discharge | SC | FC | n = 65 |
| Stroke | 3 | 7 | 10 |
| Acute myocardial infarction | 2 | 4 | 6 |
| Heart failure | 2 | 3 | 5 |
| Sudden death | 2 | 2 | |
| During aortic re-operation | 2 | 6 | 8 |
| Ruptured distal aortic aneurysm | 1 | 4 | 5 |
| Malignancy | 3 | 12 | 15 |
| Unknown | 2 | 12 | 14 |
| SC: Subclavian artery cannulation; FC: Femoral artery cannulation | |||
Between January 1992 and December 2005, 346 patients underwent emergency surgery for type-A aortic dissection of which 290 patients survived the operation. Of these patients 26% were women (n = 75) and 74% men (n = 215). The ages of the entire study cohort ranged from 18 to 83 years (table 1). Follow-up was completed in 89.5% (259) patients with a median of 42 months (range: 3–83 months) in the SC- group and 69 months in the FC- group (range: 2–143 months). A total of 31 patients did not answer our follow-up questionnaire for unknown reasons. During a 5 year follow up period, 22.4% of all hospital survivors (65/290) died. 15 patients died in the SC group and 50 patients in the FC group. The causes of death included stroke, acute myocardial infarction, heart failure, aortic re-operation and malignancies (table 2).
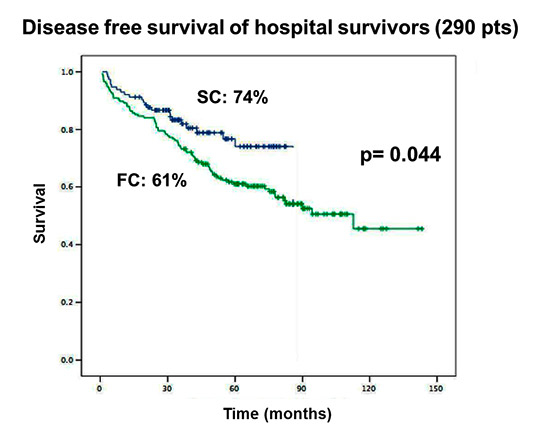
Figure 3
Disease free survival of hospital survivors (290 patients); SC: blue; FC: green.

Figure 4
Freedom from re-operation at follow-up (290 patients); SC: blue; FC: green.
The actuarial overall survival (of the 346 patients) was significantly higher in the SC group (74% vs. 58%; p = 0.002) at five years. When focussing on the hospital survivors (n = 290), the survival benefit in the SC group also remained clearly visible (83% vs. 71%; p = 0.022) (fig. 1 and 2).
The disease-free survival was significantly higher in the SC group (74% vs. 61%; p = 0.044), (fig. 3) and additionally freedom of re-operation at 5 year follow-up appeared to be increased in the SC group when compared to the FC group (89% vs. 79%; p = 0.125), however failed to achieve statistical significance (fig. 4 and table 3).
In regard to neurological complications, 28 patients (11/114 vs. 17/176; p = 0.58) presented with neurological deficits during the follow-up period. Of these, 12 patients (8/11 vs. 4/17) only suffered from temporary neurological dysfunctions and recovered completely within 1.5 years. Of the 16 remaining patients suffering from permanent neurological deficits at the 5 year follow-up, significantly more belonged to the FC group indicating an improved neurological outcome for the SC group (3/11 vs. 13/17; p = 0.019) (table 4).
| Table 3: Reoperations after type A correction. | |||
| SC | FC | p | |
| Supracoronary graft replacement | 2 (16%) | 4 (12%) | n.s. |
| Valve replacement | 3 (24%) | 7 (21%) | n.s. |
| Tubular Dacron graft | 2 (16%) | 6 (18%) | n.s. |
| Composite Graft | 4 (32%) | 12 (36%) | n.s. |
| Graft (AAA) | 1 (8%) | 4 (12%) | n.s. |
| AAA: abdominal aortic aneurysm; SC: Subclavian artery cannulation; FC: Femoral artery cannulation | |||
| Table 4: Neurological dysfunctions. | |||
| SC (n = 114) | FC (n = 176) | p | |
| All Neurological disorders during follow-up (n = 28) | 11 (9%) | 17 (9.8%) | n.s. |
| Temporary neurology (n = 12) | 8 (73%) | 4 (24%) | n/a |
| Persistent neurology (Type I) (n = 16) | 3 (27%) | 13 (76%) | 0.019 |
This study demonstrates excellent long-term outcomes after emergency surgery for acute type-A dissection with 225 survivors (65% of the entire study cohort; n = 346) at five years. Furthermore, our findings indicate that subclavian artery perfusion represents a superior approach to repair acute type-A dissection when compared to femoral artery cannulation. Besides a significantly higher overall and disease-free survival, subclavian cannulation was associated with a significantly improved long term neurological outcome at five years. Additionally these patients presented with a trend to a decreased need for re-operation.
These findings are in line with our previous short term report highlighting the superior results for subclavian artery cannulation in patients presenting with acute type-A aortic dissection (TA-AAD) [7]. However, although long-term data are available for the femoral cannulation technique [2, 3, 6, 8, 9], the impact of the subclavian technique on the long-term outcome has not been elucidated yet. Our data display a survival benefit for the SC group at one, three and five years.
Furthermore, severe, permanent neurological deficits could be prevented by employing subclavian artery perfusion. The cannulation of the subclavian artery provides the benefit of an antegrade cerebral perfusion (ACP) during treatment of these urgent cases [10, 11]. Ideally, an optimal cerebral protection during CPB might be established by continuous perfusion of all cerebral arterial vessels. However, such an approach would require a more time-consuming and cumbersome ACP. Consequently, in this cohort we preferred the approach of clamping the innominate artery, which allowed for a selective ACP through only the right carotid artery during periods of systemic circulatory arrest.
The significant disadvantage for the femoral-group (FC) might be related to several, already well described, disadvantages of this technique, such as the relatively high rates of fluid sequestration, significant cerebral oedema, and mild cerebral histopathology [12]. Studies by Ehrlich et al. [13] demonstrated conclusively that a significantly reduced capillary flow occurs during retrograde cerebral perfusion (RCP) which in turn might also explain the lack of improved clinical outcomes as described by Hagl et al. [14, 15]. Moreover, dynamic occlusion of the renal artery by the dissection membrane and/or thrombus embolisation out of the false channel or embolisation from the atherosclerotic aortic wall might follow a retrograde perfusion of the abdominal aorta. A post-mortem study by van Arsdell et al. [16] of patients with aortic dissections demonstrated that a large part were at high risk for the occurrence of false lumen mal-perfusion (dynamic occlusion) if the femoral artery would have been used to establish CPB.
Several reasons determine the need of a later re-operation comprising of the primary disease, its consequent postoperative medical treatment and systematic clinical follow-up (CT-scan, etc). In our study the actuarial need for re-operations did not vary significantly between both groups at 5 year follow-up. The major need for re-operations was linked to aortic valve and aortic root related problems as well as the formation of aneurysms. An excellent re-operation-free survival of 92% at 25 year follow-up was recently presented by Chiappini and colleagues [3]. The authors concluded that their excellent results being far above the generally reported 60–80% in other studies [9, 17], could be achieved due to their aggressive and extended surgical management of aortic repair. On the other hand, several other authors still do recommend conservative aortic root operations for acute type-A aortic dissections, with the exception of the Marfan syndrome, with satisfying mid- and long-term results [18–20].
There are several limitations to mention: Firstly, it was a retrospective single centre analysis and all disadvantages apply. Next, there was a relevant time-shift between the two groups. Between 1992 and 2000 FC was practiced (FC group) and from 2000 up to 2005 SC was practiced (SC group). Hence, there could have been a few changes in strategies with regard to surgical technique, anaesthesiology and technology in the FC group. Additionally, there was no search for specific determinants influencing early and late outcomes in our institution during this time. Risk analysis has only been started recently.
In conclusion, our data indicate, that subclavian artery cannulation technique for ACP represents an excellent approach in the strategy to repair acute type-A aortic dissection and seems to provide excellent long term outcomes. Multicentre, controlled-randomised trials are mandatory to validate these results.
1 Bachet J, Goudot B, Dreyfus GD, Brodaty D, Dubois C, Delentdecker P, et al. Surgery for acute type A aortic dissection: the Hopital Foch experience (1977–1998). Ann Thorac Surg. 1999;67:2006–9; discussion 2014–2009.
2 Svensson LG, Crawford ES, Hess KR, Coselli JS, Safi HJ. Dissection of the aorta and dissecting aortic aneurysms. Improving early and long-term surgical results. Circulation. 1990;82:IV24–38.
3 Chiappini B, Schepens M, Tan E, Dell’ Amore A, Morshuis W, Dossche K, et al. Early and late outcomes of acute type A aortic dissection: analysis of risk factors in 487 consecutive patients. Eur Heart J. 2005;26:180–6.
4 Haverich A, Miller DC, Scott WC, Mitchell RS, Oyer PE, Stinson EB, et al. Acute and chronic aortic dissections – determinants of long-term outcome for operative survivors. Circulation. 1985;72:II22–34.
5 Lai DT, Robbins RC, Mitchell RS, Moore KA, Oyer PE, Shumway NE, et al. Does profound hypothermic circulatory arrest improve survival in patients with acute type a aortic dissection? Circulation. 2002;106:I218–28.
6 Sabik JF, Lytle BW, Blackstone EH, McCarthy PM, Loop FD, Cosgrove DM. Long-term effectiveness of operations for ascending aortic dissections. J Thorac Cardiovasc Surg. 2000;119:946–62.
7 Reuthebuch O, Schurr U, Hellermann J, Pretre R, Kunzli A, Lachat M, et al. Advantages of subclavian artery perfusion for repair of acute type A dissection. Eur J Cardiothorac Surg. 2004;26:592–8.
8 Glower DD, Speier RH, White WD, Smith LR, Rankin JS, Wolfe WG. Management and long-term outcome of aortic dissection. Ann Surg. 1991;214:31–41.
9 Tsai TT, Fattori R, Trimarchi S, Isselbacher E, Myrmel T, Evangelista A, et al. Long-term survival in patients presenting with type B acute aortic dissection: insights from the International Registry of Acute Aortic Dissection. Circulation. 2006;114:2226–31.
10 Kazui T, Kimura N, Yamada O, Komatsu S. Surgical outcome of aortic arch aneurysms using selective cerebral perfusion. Ann Thorac Surg. 1994;57:904–11.
11 Sabik JF, Lytle BW, McCarthy PM, Cosgrove DM. Axillary artery: an alternative site of arterial cannulation for patients with extensive aortic and peripheral vascular disease. J Thorac Cardiovasc Surg. 1995;109:885–890; discussion 890–881.
12 Ehrlich MP, Hagl C, McCullough JN, Zhang N, Shiang H, Bodian C, et al. Retrograde cerebral perfusion provides negligible flow through brain capillaries in the pig. J Thorac Cardiovasc Surg. 2001;122:331–8.
13 Ehrlich MP, Fang WC, Grabenwoger M, Kocher A, Ankersmit J, Laufer G, et al. Impact of retrograde cerebral perfusion on aortic arch aneurysm repair. J Thorac Cardiovasc Surg. 1999;118:1026–32.
14 Griepp RB. Cerebral protection during aortic arch surgery. J Thorac Cardiovasc Surg. 2001;121:425–7.
15 Hagl C, Ergin MA, Galla JD, Lansman SL, McCullough JN, Spielvogel D, et al. Neurologic outcome after ascending aorta-aortic arch operations: effect of brain protection technique in high-risk patients. J Thorac Cardiovasc Surg. 2001;121:1107–21.
16 Van Arsdell GS, David TE, Butany J. Autopsies in acute type A aortic dissection. Surgical implications. Circulation. 1998;98:II299–302; discussion II302–294.
17 Pugliese P, Pessotto R, Santini F, Montalbano G, Luciani GB, Mazzucco A. Risk of late reoperations in patients with acute type A aortic dissection: impact of a more radical surgical approach. Eur J Cardiothorac Surg. 1998;13:576–80; discussion 580–571.
18 Fann JI, Smith JA, Miller DC, Mitchell RS, Moore KA, Grunkemeier G, et al. Surgical management of aortic dissection during a 30-year period. Circulation. 1995;92:II113–121.
19 Niederhauser U, Kunzli A, Seifert B, Schmidli J, Lachat M, Zund G, et al. Conservative treatment of the aortic root in acute type A dissection. Eur J Cardiothorac Surg. 1999;15:557–63.
20 von Segesser LK, Lorenzetti E, Lachat M, Niederhauser U, Schonbeck M, Vogt PR, et al. Aortic valve preservation in acute type A dissection: is it sound? J Thorac Cardiovasc Surg. 1996;111:381–90; discussion 390–381.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.
Authors’ contribution: PFS and MYE contributed equally to the manuscript.
This work was presented at the 22nd Annual Meeting of the European Association for Cardiothoracic Surgery in Lisbon, 2008.