Idiopathic macular epiretinal membrane surgery with simultaneous internal limiting membrane peeling. The experience of the Fribourg Eye Clinic
DOI: https://doi.org/10.4414/smw.2013.13876
Giorgios D
Panos, Philippe
de Gottrau
Abstract
PURPOSE: To evaluate the visual and anatomical outcomes following idiopathic macular epiretinal membrane (ERM) removal.
METHODS: A retrospective study of 30 eyes operated for idiopathic ERM was conducted. Pars plana vitrectomy was combined with ERM removal and indocyanine green (ICG) assisted internal limiting membrane (ILM) peeling.
RESULTS: Mean preoperative best corrected visual acuity (BCVA) was 0.4 logMAR (0.4 in decimal units), whereas mean postoperative BCVA was 0.26 logMAR (0.6 in decimal units). Mean preoperative foveal thickness was 392 μm, whereas mean postoperative foveal thickness was 305 μm. A statistically significant difference was observed between preoperative and postoperative BCVA (p <0.001, Student’s t-test).
Optical coherence tomography (OCT) measurement of postoperative foveal thickness revealed a significant decrease in thickness (p <0.0001, Student’s t-test), however, no correlation was observed between postoperative BCVA and postoperative foveal thickness (Pearson’s correlation coefficient, r = 0.228; p = 0.22).
CONCLUSIONS: Although significant visual acuity improvement and anatomical recovery was detected after idiopathic ERM removal, full restoration of foveal thickness was not achieved in the majority of cases.
Introduction
Macular epiretinal membrane (ERM) proliferation seems to be frequent in patients over 50 years of age, increasing from 2% at 50 years to 20% at 75 years. It is bilateral in 10% to 20% of the cases [1, 2]. Histopathological findings showed the presence of idiopathic ERM in 1.7% to 3.5% of autopsied eyes [3–5].
When the membrane involves the macula it can cause loss of visual acuity (VA), metamorphopsia and sometimes monocular diplopia due to the membrane thickness, retinal distortion, oedema in the macular area and the presence of significant traction causing retinal elevation [6]. ERM is a slowly progressive disease and only 5% of the cases experience severely decreased vision to 0.1 or worse after 10 years of evolution [1, 6, 7].
Vitreoretinal surgery techniques, removing the central vitreous gel then the ERM as a single piece, usually lead to a significant anatomical improvement of the macula. Anatomical outcomes seem to be better using internal limiting membrane (ILM) peeling [8].
Retinal ILM peeling is facilitated by indocyanine green (ICG) staining. In an autopsy study on human cadaveric eyes, ICG contact with the retinal surface resulted in bright green staining of the ILM, facilitating the ILM peeling by providing a stark contrast between the stained ILM and the unstained retina [9].
The purpose of our study was to evaluate the functional and anatomical outcomes following ERM removal with simultaneous ILM peeling.
Material and methods
This was a retrospective cohort study of pseudophakic eyes, operated in our department (Department of Ophthalmology, Cantonal Hospital of Fribourg, Switzerland) for idiopathic macular ERM. A total of 30 pseudophakic patients, who underwent pars plana vitrectomy, ERM peeling and ICG-assisted ILM peeling in 2008 and 2009 were included. Patients with coexisting ocular diseases such as glaucoma, diabetic retinopathy or age-related macular degeneration were not included in the study.
All patients had previously undergone uneventful phacoemulsification. Only pseudophakic eyes were included in order to avoid the potential influence of a cataract on the final visual outcome. Vitreoretinal surgery was performed by the same experienced surgeon (PdG), who used the technique of standard three-port pars plana vitrectomy (Oertli OS3, Oertli, Switzerland). Standard 23-gauge instruments were used. Peeling of the ERM was performed followed by intraocular injection of ICG, followed by peeling of the ILM. In the postoperative period, the same anti-inflammatory and antibiotic drops were used in all cases.
Preoperative and postoperative characteristics were analysed and compared. In particular, best-corrected visual acuity (BCVA) before the operation and at the end of the follow-up period (12 months) was recorded in decimal units, as well as any intraoperative or postoperative complications. The foveal thickness was measured with frequent optical coherence tomography (OCT) examinations (Copernicus OCT, Optopol, Poland). Moreover, the foveal thickness at 12 months and at baseline (before the operation) was compared.
All patients provided written, informed consent and the study was conducted in accordance with institutional guidelines and the Declaration of Helsinki.
All parameters used in the study were expressed as the mean ± standard deviation (SD). For calculation of the mean and subsequent statistical comparisons, decimal units of BCVA were transformed to the logarithm of the minimum angle of resolution (logMAR) units. Normality of the data was tested with the Kolmogorov-Smirnov test and quantitative characteristics were compared using the paired Student’s t-test. Furthermore, Pearson’s correlation coefficient was used to search for an existing relationship between final BCVA and foveal thickness at the end of the follow-up period. A p <0.05 was used to mark statistical significance. All statistics were performed using MedCalc ver.10.2 (MedCalc, Belgium).
|
Table 1: Demographic characteristics of the study group. |
| Sex |
15M, 15F |
| Eye affected |
11 right, 19 left |
| Mean age ± SD (years) |
72 ± 5 |
| Follow up (months) |
12 |
Results
The study included a total of 30 pseudophakic eyes presenting with idiopathic macular ERM in one eye. The study group consisted of 30 patients, 15 men and 15 women, with an average age of 72 years(61 to 84 years). The right eye was affected in 11 cases and the left eye in 19 cases. Demographic characteristics are summarised in table 1.
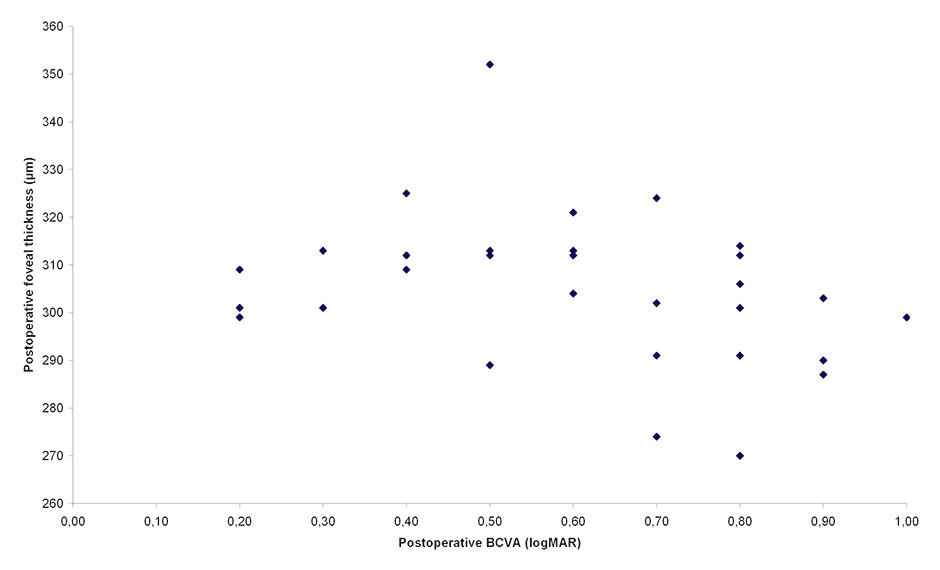
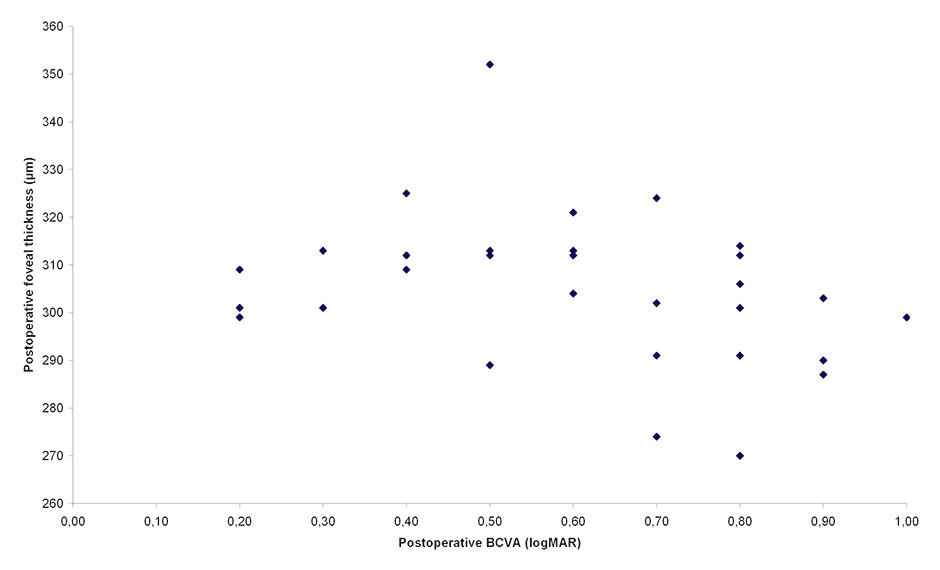
Figure 1
Linear regression analysis of the relationship between postoperative best-corrected visual acuity (BCVA) and postoperative foveal thickness assessed with optical coherence tomography (OCT). No correlation was observed between these two variables (Pearson’s correlation coefficient, r = 0.228; p = 0.22).
The follow-up period was 12 months. Mean preoperative BCVA was 0.4 logMAR (0.4 in decimal units), whereas mean postoperative BCVA was 0.26 logMAR (0.6 in decimal units). A statistically significant difference was observed between pre-operative and post-operative BCVA (p <0.001, Student’s t-test).
At the end of the follow-up period (12 months), BCVA was improved in 23 patients (76.7%), stable in 3 patients (10%) and decreased in 4 patients (13.3%). Of interest, in 11 patients (36.67%) there was an improvement of visual acuity of 3 Snellen lines or more. The detailed status of preoperative and postoperative BCVA is summarised in table 2.
Mean preoperative foveal thickness was 392 ± 20 μm, whereas mean postoperative thickness was 305 ± 16 μm (decrease in foveal thickness of 87 μm on average). A statistically significant difference was observed between preoperative and postoperative foveal thickness (p <0.0001, Student’s t-test), however no correlation was observed between post-operative BCVA and post-operative foveal thickness (Pearson’s correlation coefficient, r = 0.228; p = 0.22) (fig. 1).
There was no ERM recurrence during the follow-up period. One eye was noted to have retinal detachment, during the 1st month of the follow-up period, which was then successfully treated with a second vitrectomy. The detailed status of preoperative and postoperative foveal thickness is summarised in table 2.
|
Table 2: Detailed preoperative and postoperative status of the patients. |
|
Patient
|
Sex
|
Age
|
BCVA pre-op
(logMAR)
|
BCVA postop.
(logMAR)
|
BCVA
difference
|
Preop. foveal
thickness (μm)
|
Postop. foveal
thickness (μm)
|
Foveal thickness
difference (μm)
|
| 1 |
M |
78 |
0.30 |
0.05 |
0.26 |
360.00 |
290.00 |
70.00 |
| 2 |
M |
66 |
0.70 |
0.22 |
0.48 |
387.00 |
312.00 |
75.00 |
| 3 |
F |
71 |
0.40 |
0.22 |
0.18 |
403.00 |
304.00 |
99.00 |
| 4 |
M |
72 |
0.70 |
0.52 |
0.18 |
389.00 |
313.00 |
76.00 |
| 5 |
M |
70 |
0.52 |
0.70 |
–0.18 |
378.00 |
299.00 |
79.00 |
| 6 |
M |
70 |
0.30 |
0.15 |
0.15 |
414.00 |
324.00 |
90.00 |
| 7 |
M |
75 |
0.40 |
0.10 |
0.30 |
419.00 |
306.00 |
113.00 |
| 8 |
M |
69 |
0.22 |
0.15 |
0.07 |
376.00 |
302.00 |
74.00 |
| 9 |
F |
71 |
0.40 |
0.10 |
0.30 |
360.00 |
270.00 |
90.00 |
| 10 |
F |
74 |
0.22 |
0.22 |
0.00 |
393.00 |
321.00 |
72.00 |
| 11 |
F |
81 |
0.40 |
0.22 |
0.18 |
372.00 |
313.00 |
59.00 |
| 12 |
F |
84 |
0.52 |
0.30 |
0.22 |
354.00 |
289.00 |
65.00 |
| 13 |
M |
76 |
0.30 |
0.30 |
0.00 |
423.00 |
352.00 |
71.00 |
| 14 |
F |
70 |
0.52 |
0.10 |
0.43 |
411.00 |
314.00 |
97.00 |
| 15 |
M |
74 |
0.40 |
0.00 |
0.40 |
392.00 |
299.00 |
93.00 |
| 16 |
M |
61 |
0.30 |
0.10 |
0.20 |
381.00 |
301.00 |
80.00 |
| 17 |
M |
71 |
0.52 |
0.70 |
–0.18 |
412.00 |
309.00 |
103.00 |
| 18 |
M |
72 |
0.30 |
0.15 |
0.15 |
381.00 |
291.00 |
90.00 |
| 19 |
F |
68 |
0.52 |
0.05 |
0.48 |
392.00 |
303.00 |
89.00 |
| 20 |
M |
77 |
0.40 |
0.10 |
0.30 |
402.00 |
312.00 |
90.00 |
| 21 |
F |
71 |
0.52 |
0.40 |
0.12 |
423.00 |
325.00 |
98.00 |
| 22 |
F |
64 |
0.30 |
0.05 |
0.26 |
375.00 |
287.00 |
88.00 |
| 23 |
F |
73 |
0.40 |
0.52 |
–0.12 |
425.00 |
301.00 |
124.00 |
| 24 |
M |
73 |
0.40 |
0.70 |
–0.30 |
391.00 |
301.00 |
90.00 |
| 25 |
F |
66 |
0.40 |
0.30 |
0.10 |
387.00 |
312.00 |
75.00 |
| 26 |
M |
81 |
0.40 |
0.40 |
0.00 |
376.00 |
309.00 |
67.00 |
| 27 |
F |
81 |
0.40 |
0.30 |
0.10 |
399.00 |
313.00 |
86.00 |
| 28 |
F |
70 |
0.22 |
0.10 |
0.12 |
382.00 |
291.00 |
91.00 |
| 29 |
F |
67 |
0.40 |
0.15 |
0.24 |
379.00 |
274.00 |
105.00 |
| 30 |
F |
77 |
0.52 |
0.40 |
0.12 |
412.00 |
312.00 |
100.00 |
| Mean ± SD |
|
72 ± 5 |
0.41 ± 0.12 |
0.26 ± 0.20 |
0.15 ± 0.19 |
392 ± 20 |
305 ± 16 |
87 ± 15 |
Discussion
Functional results
Pars plana vitrectomy has been found to successfully remove ERMs from the macula resulting in an improvement in vision in 75% to 85% of eyes [10–14]. In addition to visual acuity improvement, metamorphopsia was often reduced postoperatively [10, 14–16]. In our study the mean final BCVA was significantly different from preoperative BCVA (p <0.001), and at the end of the follow-up period BCVA was improved in 23 patients (76.7%), stable in 3 patients (10%) and decreased in 4 patients (13.3%).
Eyes with poor preoperative BCVA (<0.25) have been reported to improve more frequently and to a greater extent than eyes with better preoperative vision [14]. However, eyes with lower levels of preoperative BCVA usually had lower final vision. A previously published study [10] reported that performing surgery on eyes with preoperative vision of 0.25 or better probably has as much to gain as eyes with preoperative vision of less than 0.25.
Anatomical results
OCT measurement of postoperative foveal thickness revealed a significant thickness decrease in our study; however, no correlation was observed between post-operative BCVA and post-operative foveal thickness (see fig. 1). The absence of normal foveal anatomical recovery does not influence the functional results [17]. Mechanical traction due to peeling of the ERM associated with removal of the ILM may be the cause of these microanatomical results [17]. These findings are in agreement with other studies on removal of ERM with simultaneous ILM peeling using Brilliant Blue G and ICG [18, 19].
Removal of the ILM during ERM surgery remains controversial. Chang [20] reported that ILM peeling associated with ERM removal does not affect the visual outcome but may reduce the incidence of later recurrence. On the other hand, Lee and Kim [21] in a comparative study found that thickening of the macula with loss of the normal foveal contour was more frequent in patients who underwent ERM and ILM peeling than in patients who underwent ERM peeling alone. They also reported that although ILM peeling during ERM surgery had no harmful effect on final functional outcomes, there may have been mechanical damage to the Müller cells and the structure of the fovea. Guigou et al. [22], in a recent case report, observed that ERM surgery combined with ILM peeling can cause functional (microscotomas) and anatomical (dissociated optic nerve fibre layer disorders and swelling of the arcuate retinal fibre layer) disorders. Lim et al. [23] observed that ERM and ILM removal result in multifocal electroretinography (ERG) abnormalities persisting even 12 months after surgery, despite functional and anatomical improvement.
There are several limitations to our study. Firstly, it was a retrospective study. In addition there was no group of patients who underwent ERM surgery without ILM peeling, thus we cannot compare these two techniques. Moreover, ERG measures are not available.
In conclusion, in our study recovery of a normal foveal thickness was not achieved in the majority of the cases, despite final BCVA improvement following idiopathic ERM removal. ERM removal with ICG assisted ILM peeling improves the vision and the anatomy of the macula, however, its use remains questionable due to the potential retinal toxic effect.
References
1 Pearlstone AD. The incidence of idiopathic preretinal macular gliosis. Ann Ophthalmol. 1985;17(6):378–80.
2 Sidd RJ, Fine SL, Owens SL, Patz A. Idiopathic preretinal gliosis. Am J Ophthalmol. 1982;94(1):44–8.
3 Clarkson JG, Green WR, Massof D. A histopathologic review of 168 cases of preretinal membrane. Am J Ophthalmol. 1977;84(1):1–17.
4 Roth AM, Foos RY. Surface wrinkling retinopathy in eyes enucleated at autopsy. Trans Am Acad Ophthalmol Otolaryngol. 1971;75(5):1047–58.
5 Wilson DJ, Green WR. Histopathologic study of the effect of retinal detachment surgery on 49 eyes obtained post mortem. Am J Ophthalmol. 1987;103(2):167–79.
6 Wise GN. Clinical features of idiopathic preretinal macular fibrosis. Schoenberg Lecture. Am J Ophthalmol. 1975;79(3):349–7.
7 Wiznia RA. Natural history of idiopathic preretinal macular fibrosis. Ann Ophthalmol. 1982;14(9):876–8.
8 Gaudric A, Fardeau C, Goberville M, Cohen D, Paques M, Mikol J. Ablation of the internal limiting membrane, macular unfolding and visual outcome in surgery of idiopathic epimacular membranes. J Fr Ophtalmol. 1993;16(11):571–6.
9 Burk SE, Da Mata AP, Snyder ME, Rosa RH, Jr., Foster RE. Indocyanine green-assisted peeling of the retinal internal limiting membrane. Ophthalmology. 2000;107(11):2010–4.
10 Donati G, Kapetanios AD, Pournaras CJ. Complications of surgery for epiretinal membranes. Graefes Arch Clin Exp Ophthalmol. 1998;236(10):739–46.
11 Margherio RR, Cox MS, Jr., Trese MT, Murphy PL, Johnson J, Minor LA. Removal of epimacular membranes. Ophthalmology. 1985;92(8):1075–83.
12 Michels RG. Vitreous surgery for macular pucker. Am J Ophthalmol. 1981;92(5):628–39.
13 Poliner LS, Olk RJ, Grand MG, Escoffery RF, Okun E, Boniuk I. Surgical management of premacular fibroplasia. Arch Ophthalmol. 1988;106(6):761–4.
14 Rice TA, De Bustros S, Michels RG, Thompson JT, Debanne SM, Rowland DY. Prognostic factors in vitrectomy for epiretinal membranes of the macula. Ophthalmology. 1986;93(5):602–10.
15 de Bustros S, Thompson JT, Michels RG, Rice TA, Glaser BM. Vitrectomy for idiopathic epiretinal membranes causing macular pucker. Br J Ophthalmol. 1988;72(9):692–5.
16 Michels RG. A clinical and histopathologic study of epiretinal membranes affecting the macula and removed by vitreous surgery. Trans Am Ophthalmol Soc. 1982;80:580–656.
17 Mazit C, Scholtes F, Rabaut C, Jallet G, Cochereau I. Assessment of macular profile using optical coherence tomography after epiretinal membrane surgery. J Fr Ophtalmol. 2008;31(7):667–72.
18 Kifuku K, Hata Y, Kohno RI, Kawahara S, Mochizuki Y, Enaida H, et al. Residual internal limiting membrane in epiretinal membrane surgery. Br J Ophthalmol. 2009;93(8):1016–9.
19 Pournaras CJ, Emarah A, Petropoulos IK. Idiopathic macular epiretinal membrane surgery and ILM peeling: anatomical and functional outcomes. Semin Ophthalmol. 2011;26(2):42–6.
20 Chang S. Controversies regarding internal limiting membrane peeling in idiopathic epiretinal membrane and macular hole. Retina. 2012;32(Suppl 2):S200–3; discussion S3–4.
21 Lee JW, Kim IT. Outcomes of idiopathic macular epiretinal membrane removal with and without internal limiting membrane peeling: a comparative study. Jpn J Ophthalmol. 2010;54(2):129–34.
22 Guigou S, Courjaret JC, Marc C, Benhammar J. Anatomical and functional repercussions of internal limiting membrane peeling in epiretinal membrane surgery. J Fr Ophtalmol. 2012.
23 Lim JW, Cho JH, Kim HK. Assessment of macular function by multifocal electroretinography following epiretinal membrane surgery with internal limiting membrane peeling. Clin Ophthalmol. 2010;4:689–94.