Costs of current antihypertensive therapy in Switzerland: an economic evaluation of 3,489 patients in primary care
DOI: https://doi.org/10.4414/smw.2013.13854
Hans Hendrik
Schäfer, Uta
Scheunert
Abstract
QUESTION UNDER STUDY: Due to greater life expectancy, costs of medication have increased within the last decade. This investigation assesses health care expenditures needed to manage the current state of blood pressure (BP) control in Switzerland. Objectives: a) average day therapy costs (DTC) of substances, b) actual DTC of currently prescribed antihypertensive therapy, c) monetary differences of treatment regimens within different BP-groups and different high risk patients, d) estimated compliance-related financial loss/annum and adjusted costs/annum. Single-pill-combinations appear to be useful to increase patient’s compliance, to reduce side effects and to bring more patients to their blood pressure goal.
METHODS: Costs were identified based on data from the Swiss department of health. We calculated DTC for each patient using prices of the largest available tablet box.
RESULTS: The average antihypertensive therapy in Switzerland currently costs CHF 1.198 ± 0.732 per day. On average beta blockers were the cheapest substances, followed by angiotensin converting enzyme inhibitors (ARBs), calcium channel blockers and diuretics. The widest price ranges were observed within the class of ARBs. Most expensive were patients with impaired renal function. Throughout all stages, single-pill-combinations appeared to be significantly cheaper than dual-free-combinations. Stage-II-hypertension yielded the highest costs for dual free combination drug use. The actual costs for all patients observed in this analysis added up to CHF 1,525,962. Based on a compliance model, only treatment amounting to CHF 921,353 is expected to be actually taken.
CONCLUSION: A disproportionately high healthcare cost is expected due to compliance reasons. The prescription of monotherapies appears to be a major cost factor, thus, the use of single-pill-combination therapy can be considered as a suitable approach to saving costs throughout all BP- stages.
Introduction
Due to a rising life expectancy and early diagnosis of chronic diseases, costs of antihypertensive therapy have increased remarkably within the last decade [1] while economic resources remain limited [2]. Uncontrolled hypertension (HT) increases the risk and incidences of diabetes, stroke, atherosclerosis and chronic kidney disease [3]. Drug therapy is used as secondary prevention due to high opportunity costs in case of cardiovascular events. However, the success of treatment is often lessened by the lack of adherence [4]. There is evidence that approximately one-half of patients discontinue their treatment within one year [5]. Another study showed that non-adherence leads to health system use costing up to 792 million US-Dollars [6]. It is noteworthy that up to 33% of drug-related admissions to hospital are caused by non-adherence to medication regimens [7]. One of the main reasons for this phenomenon is multiple dose regimens, which are inversely correlated with adherence to medication. Decreasing the amount of tablets can therefore not only lead to higher adherence but also to increase in the persistence of the treatment [8].
Comparing therapies based on single-pill-combination (SPC) and dual free combination (DFC), a study showed a significant increase (26%) of persistence to medication after one year of using two substances in one tablet [9]. However, because random clinical trials are designed and conducted under ideal and monitored conditions, indicating low non-compliance rates [6] they do not reflect compliance in reality. As a result the estimated investment for health care systems would probably be much higher and the preventive benefit remarkably lower.
In Switzerland approximately 84% of hypertensive patients receive therapy and 54% of patients with uncomplicated HT attain target blood pressure below 140/90 mm Hg. These data show that only 28.8% of diabetics meet their targets in Switzerland [10] while approximately 44% of the very elderly (above 80 years) appeared to control their blood pressure (according to the guidelines of the European Society of Hypertension/European Society of Cardiology) [11].
Cost-effectiveness analyses have been introduced in several countries and form the foundation for reimbursement decisions or the establishment of guidelines. However, these analyses alone appear to be insufficient as the monetary value of the measured effect is not taken into consideration [12]. This effect actually helps to evaluate the desirability of a certain policy. It is therefore not only relevant if the right antihypertensive medication is prescribed to patients but also of interest if the same blood pressure goal can be accomplished in another, less expensive way.
The prescriptions of SPC appear to be useful in increasing patient compliance, to reduce side effects and to bring more patients to their target blood pressure goals [13]. Moreover, in many health systems these formulations are often available at prices of monotherapies and an increasing amount of international recommendations start favouring SPC as early combination therapy [14]. Despite accessible information about current rates of target blood pressure attainment in Switzerland, it remains unknown which health care expenditures are needed to manage the current control rates. Therefore, based on data from 3,489 patients this investigation was undertaken to assess:
1. the average day therapy costs of antihypertensive substances and substance classes;
2. the actual day therapy costs of currently prescribed antihypertensive therapy regimens;
3. monetary differences due to different treatment regimens (monotherapies, SPC) within the different blood pressure groups and high risk patients;
4. the estimated financial loss per annum due to lack of compliance reasons and the adjusted costs per annum for the overall population.
Material and methods
For this survey 450 Swiss general practitioners were chosen randomly from a list and asked in a letter to include every adult patient (above 18 yrs.) who visited the doctor’s practice within one week with diagnosed HT. One hundred and fifty physicians responded to this call and submitted data from 4,594 patients using a web-database. Based on the estimation of approximately 5,800 primary care physicians working in Switzerland [15] and estimating that 221,500 patients are treated in primary care for HT (estimated compliance-related financial loss per annum) this paper roughly represents 2.5% of the physician population who manage approximately 5,537 patients with elevated blood pressure. Screening of patients was not recommended in order to prevent a possible bias. Demographic information (age, sex, weight, height), systolic/diastolic blood pressure (SBP/DBP) assessed in sitting position with either the auscultatory or oscillatory method), and heart rate were recorded. General practitioners were asked to report the presence of microalbuminuria (30–300 mg/24h) and the increase of serum creatinine (for males up to 133 µmol/l, for females up to 124 µmol/l). Other clinical measurements were not required. We assessed risk factors including diabetes mellitus, pack years of nicotine abuse and dyslipidaemia (cholesterol >6.5 mmol/l, HDL <1.0 mmol/l, LDL >4.0 mmol/l, triglyceride >1.7 mmol/l). Laboratory values were processed when they were available (fasting glucose, total and HDL cholesterol, potassium, creatinine, triglyceride, urea). Concomitant therapies could be mentioned (antidiabetic therapy, aspirin or lipid lowering therapy) when relevant. Patients were determined to be diabetic if fasting glucose levels were ≥7 mmol/l or if antidiabetic treatment was prescribed. For the documentation of the current therapy, substances or trademarks of both monotherapy and SPC were selected interactively. The data concerning daily dosage and treatment duration was recorded using three time categories (<3 month, 3–6 month, >6 month).
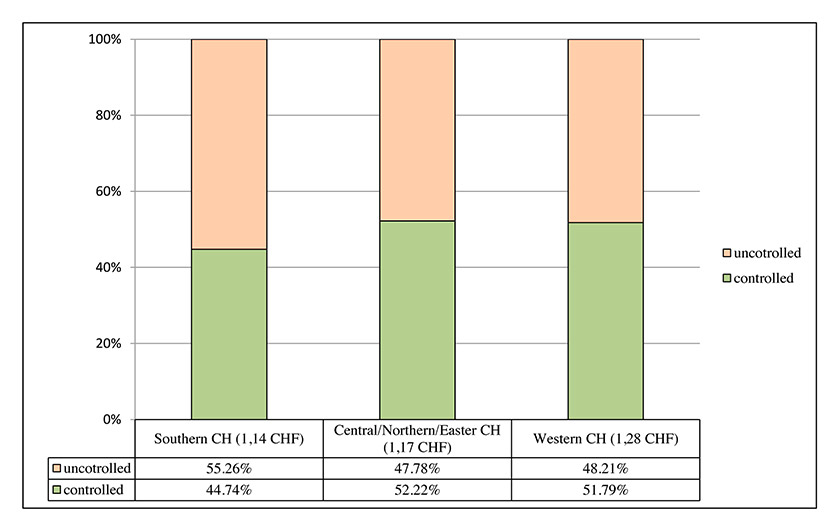
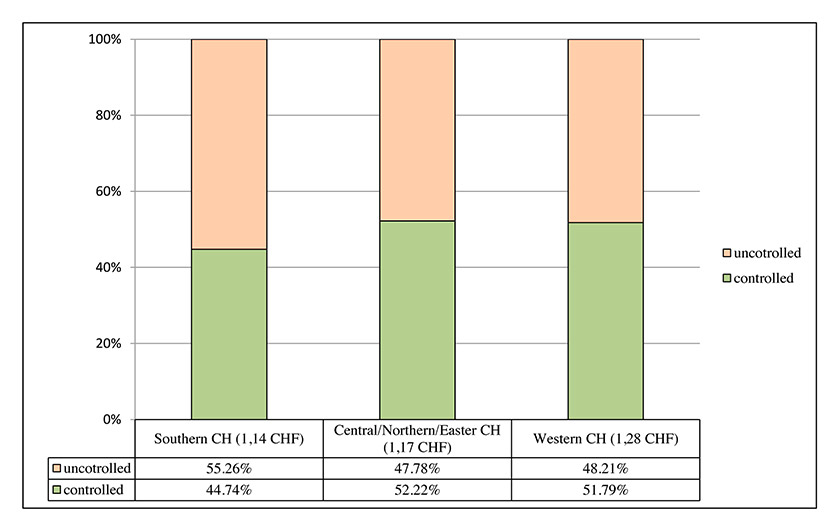
Figure 1
Comparison of day therapy costs according to geographical regions and corresponding target blood pressure attainment. Blood-pressure control rates were calculated pooling threshold attainment of <140/90 mm Hg for uncomplicated hypertension, <130/80 mm Hg for patients with diabetes mellitus and <125/75 mm Hg for patients with impaired renal function.
Due to potential treatment adjustment during the initial establishment of an antihypertensive therapy, patients who received an unchanged treatment regimen of less than 3 months (N = 134) were excluded. Furthermore, patients not receiving any antihypertensive therapy (N = 738) were not reflected in this analysis. Finally N = 233 could not have been reflected in this analysis due to a termination of the medication production or the disappearance of the product from the market they were on, leaving a total patient population of 3,489.
Costs for antihypertensive therapy were identified based on data from the Swiss department of health (Spezialitätenliste 2012). We calculated current day and year therapy costs for each patient using prices of the largest available (and therefore cheapest) tablet box. Day therapy costs were defined as the actual costs that occurred on average for all patients treated with antihypertensive therapy under current conditions and independently of target blood pressure attainment reflecting frequency of doses and substances. In total therapy cost was calculated from 408 different boxes, whereby the box sizes ranged from seven tablets up to 200. Mainly (92.4% resp. 377 out of the 408 tablet boxes) taken into account were boxes with 90, 98 or 100 tablets, representing a long-term treatment.
We assumed, that in general patients with a stable regimen will receive prescriptions, upon which cost calculation appears to be valid. Based on this approach, we have excluded patients receiving antihypertensive therapy within the last three months, because it can be assumed that these patients may be treated with smaller and more expensive tablet boxes and treatment change is more likely to happen when a small tablet box has been prescribed. Tablet prices (unit prices) were investigated by dividing the number of available units/packed by the price of the tablet box (table 1). In a second step we multiplied the unit price with the number of daily prescribed doses. This procedure has been performed for all additional antihypertensive substances in order to calculate the day therapy costs (table 2), which were analysed with regards to target blood pressure attainment thresholds and blood pressure staging to Swiss society of hypertension [16]. In addition, we investigated therapy costs in the light of concomitant cardiovascular diseases and demographic factors (table 3).
Furthermore, we investigated differences in therapy costs in three geographical regions (western Switzerland, southern Switzerland and central/eastern Switzerland). Based on a review from Claxton et al. [17] we then estimated the costs of prescribed but unused drugs in patients receiving unchanged treatment for more than 3 months (table 4A). Claxton and colleagues have investigated compliance rates of 76 studies that used electronic monitoring devices including bottle caps, pillboxes or blister cards. The authors included 26 cardiovascular trials but also other treatments that allowed extrapolation to other medications, formulations and medical disorders. The rates of dose-taking compliance by frequency of regimen are shown in table 4B which formed the basis for the calculation of estimated costs of unused medication. Statistics were performed descriptively and with classical tests of hypotheses using the statistical software package R, version 2.12. Unpaired means were compared using one-way ANOVA. Comparisons of dichotomous outcomes were performed with the chi-square test. Correlations were calculated with Pearson’s moment correlation. For all results according to comparisons or relations of variables mean comparisons are estimated, whereby the significance is shown by the p-values (with p = 0.000 for highly significant up to p = 0.010 for error probability of 10.0%).
|
Table 1: Substance/substance class therapy costs in Swiss Francs (CHF) (unit price)* |
|
Substance class/substance
|
Substance therapy costs in CHF
|
|
Avg
|
Min
|
Max
|
Median
|
|
Monotherapy
|
|
Diuretics
|
0,6445
|
0,1440
|
3,5275
|
0,4425
|
| Hydrochlorotiazide |
0,1808 |
0,1440 |
0,2080 |
0,1850 |
| Furosemide |
0,4598 |
0,1660 |
2,2100 |
0,1750 |
| Torasemide |
0,6065 |
0,1895 |
1,7360 |
0,4630 |
|
ACEIs
|
0,4697
|
0,2030
|
0,9730
|
0,4425
|
| Enalaprile |
0,4715 |
0,3183 |
0,7020 |
0,4507 |
| Lisinoprile |
0,4298 |
0,2045 |
0,8930 |
0,3885 |
|
ARBs
|
1,0056
|
0,3592
|
2,0286
|
1,0306
|
| Losartan |
0,6371 |
0,3592 |
1,4684 |
0,5393 |
|
CCBs
|
0,6167
|
0,2795
|
1,0990
|
0,5857
|
| Amlodipine |
0,6356 |
0,3930 |
0,9445 |
0,6355 |
| Diltiazem |
0,5363 |
0,4030 |
0,8545 |
0,4393 |
| Felodipine |
0,6704 |
0,5085 |
0,9165 |
0,6083 |
| Nifedipine |
0,5487 |
0,2795 |
0,9080 |
0,4875 |
|
BBs
|
0,4316
|
0,1565
|
1,0385
|
0,3985
|
| Atenolol |
0,2873 |
0,1565 |
0,4480 |
0,2645 |
| Carvedilole |
0,5051 |
0,3150 |
1,0385 |
0,4000 |
|
DRIs
|
1,4227
|
1,3128
|
1,5327
|
1,4227
|
|
Dual-SPC
|
|
ARB/Ds
|
1,2159
|
0,5806
|
1,9495
|
1,1518
|
| Losartan/HCTZ |
0,9128 |
0,5806 |
1,4684 |
0,8628 |
|
ACEI/Ds
|
0,6517
|
0,3690
|
2,1092
|
0,5492
|
| Enalapril/HCTZ |
0,6811 |
0,5536 |
0,7745 |
0,6895 |
| Lisinopril/HCTZ |
0,4771 |
0,3690 |
0,6060 |
0,5235 |
|
ARB/CCBs
|
1,2351
|
0,9673
|
1,5449
|
1,2403
|
|
DRI/Ds
|
1,3166
|
1,2158
|
1,4173
|
1,3166
|
|
CCB/BBs
|
1,0428
|
0,7910
|
1,4220
|
0,9155
|
|
BB/Ds
|
0,5151
|
0,2689
|
1,1732
|
0,4750
|
| Atenolole/ Chlortalidone |
0,3817 |
0,2689 |
0,5230 |
0,3793 |
|
Triple-SPC
|
|
ARB/CCB/Ds
|
1,6279
|
1,5694
|
1,6571
|
1,6571
|
| ACEIs angiotensin converting enzyme inhibitors, BBs beta blocker, DRIs direct renin inhibitors, ARBs angiotensin receptor subtype I inhibitors, CCBs calcium channel blockers, Ds diuretics, Avg average, CHF Swiss Francs, SPC single-pill-combinations, HCTZ hydrochlorothiazide
*Substances that occurred at least three times in the survey are displayed in this table. Cost calculations of substance classes reflect all prescribed substances in this survey. |
|
Table 2: Day therapy costs in Swiss Francs (CHF) according to gender differences. |
| |
Day therapy costs in CHF
|
|
All
N = 3489
|
MalesN = 1753
|
FemalesN = 1736
|
| Mm Hg (overall population) |
1.1983 ± 0.7329 |
1.2295 ± 0.7367 |
1.1667 ± 0.7280 |
|
According to staging (SSH)
Optimal (<120/80)
Normal (120–129/80–84)
High normal (130–139/85–89)
Stage I (140–159/90–99)
Stage II (160–179/100–109)
Stage III (≥180/≥110) |
1.2359 ± 0.8340
1.1428 ± 0.6832
1.1483 ± 0.6776
1.2433 ± 0.7707
1.3755 ± 0.8296
1.2529 ± 0.6966 |
1.2764 ± 0.7927
1.1293 ± 0.6693
1.2011 ± 0.7094
1.2671 ± 0.7665
1.4606 ± 0.8270
1.4963 ± 0.7292 |
1.1798 ± 0.8888
1.1572 ± 0.6986
1.0930 ± 0.6384
1.2209 ± 0.7746
1.3108 ± 0.8291
1.1166 ± 0.6530 |
|
According to duration of HT
0–3 years
4–10 years
>10 years |
1.0352 ± 0.5991
1.0944 ± 0.6642
1.3101 ± 0.7878 |
1.1224 ± 0.6231
1.1386 ± 0.6563
1.3369 ± 0.8111 |
0.9148 ± 0.5436
1.0450 ± 0.6699
1.2866 ± 0.7665 |
|
According to concomitant cardiovascular diseases
Diabetes mellitus
History of myocardial infarction
History of stroke
Impaired renal function
Heart failure |
1.4177 ± 0.8680
1.3684 ± 0.8387
1.2642 ± 0.7481
1.5105 ± 0.9248
1.4913 ± 0.8456 |
1.4246 ± 0.8817
1.3480 ± 0.8166
1.2451 ± 0.7435
1.5322 ± 0.9666
1.5375 ± 0.8832 |
1.4081 ± 0.8497
1.4103 ± 0.8938
1.2853 ± 0.7557
1.4831 ± 0.8721
1.4512 ± 0.8082 |
|
According to age
<65 years
65–79 years
≥80 years |
1.1513 ± 0.7240
1.2329 ± 0.7337
1.2093 ± 0.7418 |
1.1993 ± 0.7332
1.2647 ± 0.7225
1.2215 ± 0.7752 |
1.0800 ± 0.7048
1.2011 ± 0.7439
1.2022 ± 0.7225 |
|
According to regions
Southern CH1
Central/Northern/Eastern CH2
Western CH |
1.1498 ± 0.7779
1.1717 ± 0.7232
1.2879 ± 0.7215 |
1.1669 ± 0.8158
1.2126 ± 0.7175
1.3055 ± 0.7270 |
1.1323 ± 0.7381
1.1304 ± 0.7268
1.2702 ± 0.7163 |
| N number, CH Confederatio Helvetica, HT hypertension
1 Innerschweiz, Tessin; 2 Bern, Oberwallis, Ostschweiz, Aargau, Basel, Zürich, Thurgau |
Results
Patients’ characteristics
The gender distribution in this survey was balanced while the average body mass index was marginally higher in the male population than in the female population (table 1). While males had lower SBP (135.2 ± 13.9 mm Hg) than females, their DBP was slightly higher than in the other gender (80.8 ± 9.1 vs 79.9 ± 9.1 mm Hg). Most patients could be assigned to Stage-I-HT (36.67%) according to the Swiss society of hypertension [16] followed by high normal staging (35.88%). Slightly more females than males showed Stage-I, -II and -III HT as well as normal blood pressure, while this relationship appeared to be reversed in high normal and optimal blood pressure.
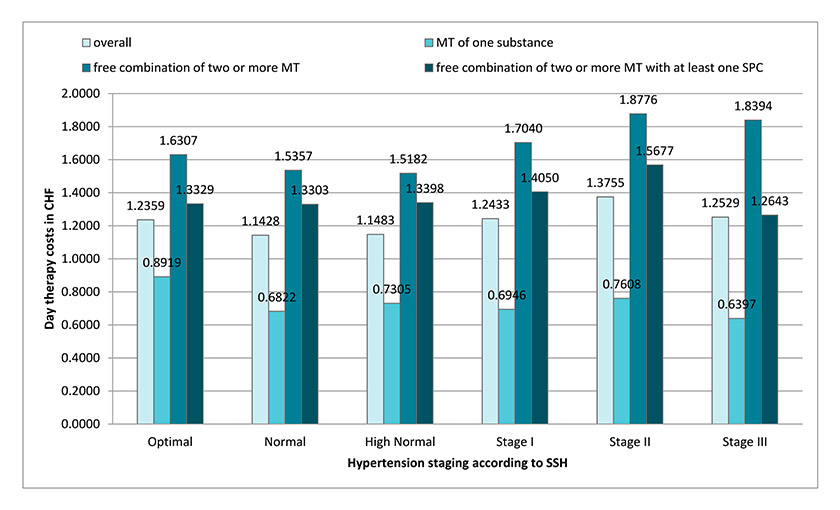
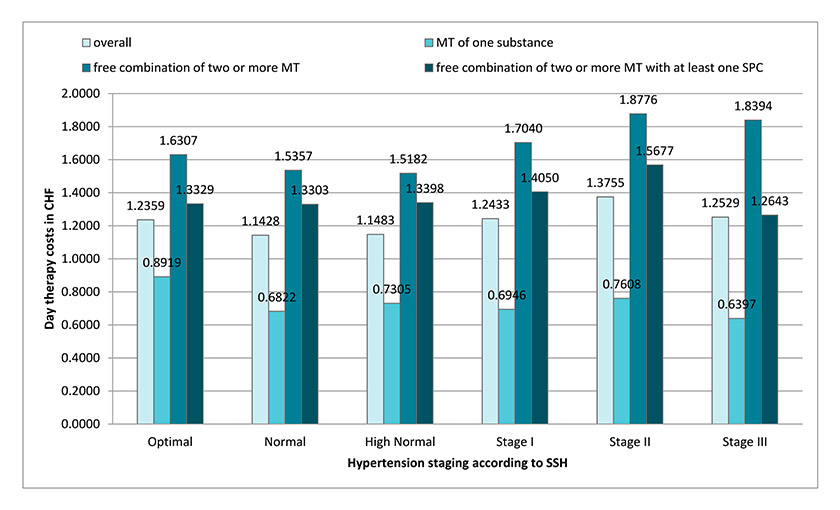
Figure 2
Current day therapy costs in Swiss Francs (CHF) according to SSH-staging: optimal (<120/180 mm Hg), normal (120–129/80–84 mm Hg), high normal (130–139/85–89 mm Hg), stage I (140–159/90–99 mm Hg), stage II (160–179/100–109 mm Hg), stage III (≥180/≥110 mm Hg).
MT: monotherapy; SPC: single pill combination; SSH: Swiss Society of Hypertension.
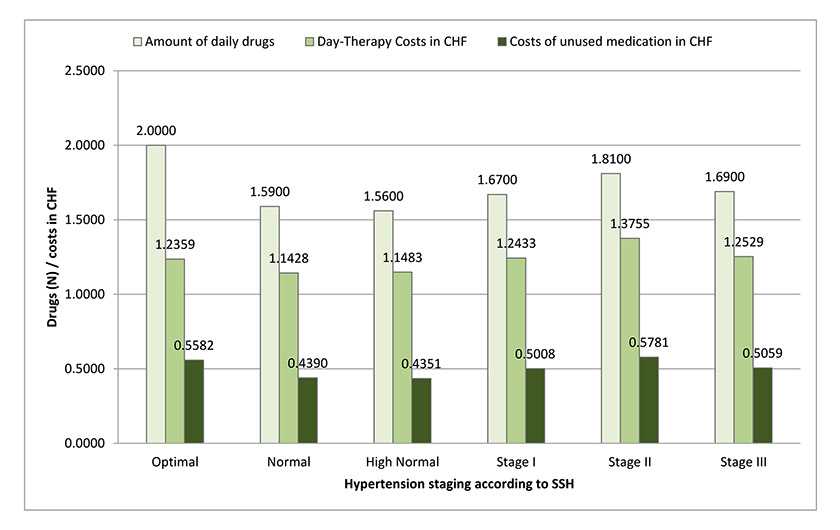
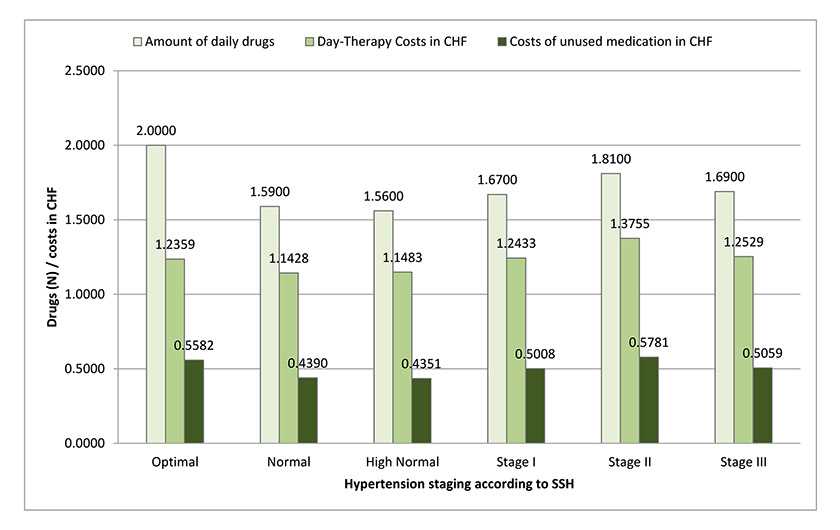
Figure 3
Current costs of unused medication in Swiss Francs (CHF) according to SSH-staging: optimal (< 120/180 mm Hg), normal (120–129/80–84 mm Hg), high normal (130–139/85–89 mm Hg), stage I (140–159/90–99 mm Hg), stage II (160–179/100–109 mm Hg), stage III (≥180/≥110 mm Hg).
N: amount of drugs; SSH: Swiss Society of Hypertension.
Target blood pressure was attained by 58.29% of patients with uncomplicated HT (<140/90 mm Hg) while only 27.26% reached their targets in the population of patients with diabetes mellitus (<130/80 mm Hg). Only a small amount of the 19.69% patients with impaired kidney function (<125/75 mm Hg) met the desired target blood pressure.
Significantly more males than females had a history of myocardial infarction (14.95% vs. 7.37%; p = 0.000). SPC was used slightly more in males than in females. The opposite holds true for mono-substance-prescriptions indicated by a mono-substance SPC-Ratio of 2.06 in males and 2.34 in females.
Substance therapy costs of antihypertensive substances and classes in Swiss Francs (CHF)
Beta blocker (BBs) were the cheapest substances (CHF 0.43) in the Swiss market, followed by angiotensin converting enzyme inhibitors (ACEIs), calcium channel blockers (CCBs) and diuretics (Ds, CHF 0.64). The fairly new direct renin inhibitor (DRI) costs CHF 1.42 daily, while the median price of Ds and ACEIs was similar (CHF 0.44). Price differences in the substance class of Ds could be observed. While the cheapest hydrochlorothiazide (HCTZ)-formulation costs CHF 0.181 per day, the highest dose of furosemide was CHF 2.21 (table 2). The widest range of prices could be observed within the substance class of ARBs while the maximal and minimal dose of DRIs differed by only 0.21 Rp. Dual SPC ACEI/Ds yielded the widest price ranges (CHF 1.74) while DRI/Ds showed flatpricing with a marginal difference of CHF 0.20 between the highest and lowest available dose. The combination of BB/Ds appeared to be the cheapest combination followed by ACEI/Ds (CHF 0.65). Most interestingly, the average cost of triple combination therapy (ARB/CCB/Ds) was only CHF 0.41 and CHF 0.39 more expensive than the corresponding SPC of ARB/Ds and ARB/CCB respectively (table 2).
Monetary costs of treatment regimens with regards to blood pressure staging and according to high-risk patients
The average antihypertensive therapy (average daily intake) in Switzerland currently costs CHF 1.19 ± 0.73 (table 3), therefore working out to CHF 437.36 per annum by calculating non balanced daily therapy costs (representing 365 days). Overall blood pressure staging, the antihypertensive therapy of male patients (CHF 1.22 ± 0.73) appeared to be significantly (p = 0.011) more expensive than for females (CHF 1.16 ± 0.72). Major differences were found in Stage-III HT in which day therapy costs for males were approximately CHF 1.49 ± 0.72 while treatment regimens for women only accounted for CHF 1.11 ± 0.65 (p = 0.103). Our results show that overall, the most expensive groups in Swiss primary care were patients with impaired renal function (CHF 1.51 ± 0.92). Paradoxically, costs for patients with a history of stroke were similar to the costs for the overall population and therefore relatively low. The most expensive high-risk group was males with heart failure (CHF 1.53 ± 0.88). In this analysis N = 38 and N = 171 patients received furosemide and torasemide respectively. The vast amount of these patients had either heart failure or an impaired renal function. Patients with stroke and myocardial infarction also received loop diuretics in a moderate manner. Regardless of gender, there were highly significant (p = 0.000) average differences of costs comparing patients treated for hypertension between 0–3 and 4–10 years and the group, which received antihypertensive medication for more than 10 years. Most interestingly, male patients between 65–79 years received the most expensive treatment while women were most cost-intensive in the age group older than 79 years. With regards to the geographical region (fig. 1) and irrespective of gender, our results show that western Switzerland had the highest average day therapy costs (CHF 1.28 ± 0.72, p = 0.000) compared to the other two regions (CHF 1.17 ± 0.72 and CHF 1.14 ± 0.77 respectively). Even though western Switzerland had a relatively high rate of blood pressurecontrol (51.79%) their costs for medication invested in patients not attaining target blood pressure were the highest in Switzerland (CHF 1.41). According to the overall costs, Stage-II comprised the most expensive patients (CHF 1.37) while the expenses for patients with normal blood pressure were the lowest (CHF 1.14, p = 0.000). Throughout all stages, the use of SPC appeared to be significantly cheaper than dual monotherapies (p = 0.000). Stage-II-HT yielded the highest costs for DFC drug use (CHF 1.88), while the average costs for SPC were only CHF 1.57 (p = 0.000). In stage III the average costs of SPC (free combination of two or more monotherapies with at least one SPC) equalled the average costs of overall prescribed therapies (fig. 2), while the mean monetary difference between SPC (CHF 1,26) and DFC (CHF 1,83) was the highest (CHF 0.57).
Estimated compliance-related financial loss per annum
Based on the data from Claxton et al. [17] compliance decreases from 79% to 69% (1 dose/d, 2 doses/d) and from 65% to 51% comparing three doses/d and four doses/d. According to these rates of dose taking compliance by frequency of regimen (table 4b), we estimated the waste cost by taking the ratio of compliance per number of prescribed antihypertensive drugs (number of daily tablets), which leads to a financial loss of CHF 604,607 for all patients observed in this survey (table 4a). Therefore, we should consider that the financial loss might be rather under-than overweighed, since the estimated waste relatively weighted to the daily drug amount does not cover the overall medication per patient in regards of additional drug use for the treatment of other diseases. This amount corresponds to a total waste of 39.26%. Given the fact, that the actual cost for all patients observed in this analysis added up to CHF 1,525,962, only treatment amounting to CHF 921,353 was expected to be actually taken. Figure 3 illustrates the daily costs of unused medication and the corresponding day therapy costs. With approximately 8 million inhabitants [18] it is estimated that in Switzerland approximately every fourth adult patient has HT [19]. This assumption is based on data from the 2007 health questionnaire leaving a total of 41,2000 patients that possibly profit from treatment. (In 2011 20.6% of the Swiss population was under 20 years of age [20]).
The fact that approximately 36% of all hypertensive patients do not know about their disease [21] and about 16% of diagnosed hypertensive patients do not receive any treatment in Switzerland [10] it can be expected that the health cost implication can be calculated on a total amount of approximately 221,500 Swiss patients. Based on this number we anticipate that a total amount of CHF 38,383,000 could be saved per annum if treatment decisions would be shifted more towards SPC rather than DFC (table 4A).
|
Table 3:Patients characteristicsaccording to gender differences. |
|
|
Patient characteristics
|
|
All
N = 3489
|
Males
N = 1753
|
Females
N = 1736
|
| Sex |
|
50.24% |
49.76% |
| Age |
69.0 ± 12.7 |
66.6 ± 12.5 |
71.5 ± 12.5 |
| Weight |
79.2 ± 15.8 |
85.1 ± 13.9 |
73.1 ± 15.3 |
| Height |
167.9 ± 9.0 |
173.8 ± 6.8 |
161.9 ± 6.8 |
| BMI (kg/m2) |
28.9 ± 4.9 |
28.2 ± 4.2 |
27.9 ± 5.6 |
| BP |
SBP (mm Hg) |
136.1 ± 14.2 |
135.2 ± 13.9 |
137.1 ± 14.5 |
| DBP (mm Hg) |
80.3 ± 9.1 |
80.8 ± 9.1 |
79.9 ± 9.1 |
| Heart Rate (bmp) |
73.0 ± 10.2 |
72.4 ± 10.7 |
73.7 ± 9.7 |
| BP staging in mm Hg (SSH) |
Optimal (<120/80) |
7.25% |
8.39% |
6.11% |
| Normal (120–129/80–84)
High normal (130–139/85–89) |
18.77%
35.88% |
17.28%
36.57% |
18.26%
35.20% |
| Stage I (140–159/90–99)
Stage II (160–179/100–109)
Stage III (≥180/≥110) |
36.67%
6.31%
1.12% |
29.55%
5.42%
0.80% |
31.80%
7.20%
1.44% |
| TBPA in mm Hg |
Uncomplicated HT (<140/90) |
58.29% |
65.18% |
52.70% |
| Diabetes mellitus (<130/80)
IRF (<125/75) |
27.26%
19.69% |
27.16%
23.36% |
27.40%
15.12% |
| Concomitant cardiovascular
diseases |
History of myocardial infarction |
11.18% |
14.95% |
7.37% |
| History of stroke |
7.05% |
7.36% |
6.74% |
| Impaired renal function |
11.06% |
12.21% |
9.91% |
| Diabetes mellitus
Heart failure |
19.66%
13.24% |
22.48%
13.58% |
16.82%
12.90 |
| Treatment regimens |
N of overall substances used |
2.03 |
2.02 |
2.04 |
| N of mono-substances used |
1.06 |
1.03 |
1.1 |
| N of SPC used |
0.48 |
0.50 |
0.47 |
| Mono-substance-SPC-ratio |
2.21 |
2.06 |
2.34 |
| BMI body mass index, SBP/DBP systolic/diastolic blood pressure, IRF impaired renal function, N number, SPC single pill combination, HT hypertension, TBPA target blood pressure attainment |
|
Table 4a: Potential cost savings in Swiss Francs (CHF) according to occurrence of diabetes mellitus with/without additional comorbidities. |
|
Other comorbidities
|
DM
|
N
|
Potential cost savings within the analysis
(per annum in total, in CHF)
|
Potential cost savings within the analysis
(per annum, per person, in CHF)
|
Potential cost savings in Switzerland
(per annum in CHF)
|
| No |
No |
1933 |
273,671 |
142 |
|
| Yes |
No |
719 |
143,598 |
200 |
|
| No |
Yes |
494 |
91,433 |
185 |
|
| Yes |
Yes |
343 |
95,897 |
280 |
|
| total |
3489 |
604,607 |
|
|
| |
221,500 |
|
|
38,383,620
|
| CHF Swiss Francs, DM diabetes mellitus, QD administration once per day, BID administration twice per day, TID administration three times per day, QID administration four times per day, N number |
|
Table 4b: Applied compliance rates in % according to Claxton et al. 2001 [17]. |
| |
Frequency of regimen
|
| QD |
BID |
TID |
QID |
| Compliance rate in % |
79 ± 14 |
69 ± 15 |
65 ± 16 |
51 ± 20 |
Discussion
In comparison to developing countries, where approximately 1.7 drugs/day [22] are prescribed, patients in Switzerland receive approximately 2.03 substances, which can be considered as an intensive treatment approach. Currently, the daily treatment of hypertension produces an average cost of CHF 1.198 ± 0.732. Similar to our findings, cost studies of other countries yielded the highest investment for patients in a HT-stage-II [23]. This might be explained by either a low compliance rate or by additional comorbidities occurring in this population. A paradox was the declining day therapy costs in woman comparing stage-III and-II as well as stage-III and stage-I-HT owing to a higher frequency of SPC-prescription in stage-III-HT. Thus, net-costs for medication were lower than in other stages. However, the interpretation of this result should reflect the fact that the patient population in stage-III HT was relatively small. The same holds true for the intergender differences in stage-III. Patients treated for longer than 10 years appeared to be more cost-intensive which might be explained by resilience to change towards alternative and cheaper combinations once a treatment plan has been established. It is especially the older generation of physicians and general practitioners in rural areas who show more hesitation concerning the use of SPC in elderly patients [11]. Surprisingly, elderly and very elderly patients did not generate remarkably higher financial expenditures compared to patients who were less than 56 years of age. A Swiss study showed that less SPCs are prescribed to the very elderly compared to younger patients [11] which consequently would have an impact on therapy costs in this cohort. This paradox is even more striking because another study showed that only 20% of patients aged 65 years and above show “good adherence” to their medication [24]. Therefore, the only suitable explanation is in general a greater adherence to medication, unique to the Swiss setting, reflecting accuracy as a function of mentality.
Even though costs could be reduced by using SPC even further in the very elderly cohort it must be considered that for some conditions, SPC are not practical when adjustments to medication need to be performed frequently. These special conditions are diseases of older age (e.g. heart failure). In addition it must be mentioned that e.g. cortical dementia also increases the risk of non-adherence to medication, and physicians may believe that with twice-daily (BID)-administration the probability for taking at least one dosage/day is higher than prescribing SPC where the forgiveness factor is low when skipping one dosage. Furthermore, it must not be forgotten that the initial use of a SPC can result in a substantial drop in blood pressure.
Interestingly, the treatment of males appeared to be more expensive than the treatment of females, even though women generally exhibit more non-adherent behaviour compared to men [25]. On the other hand, it can be argued that the treatment of complicated hypertension with comorbidities such as heart failure, impaired renal function and stroke, diagnosed more frequently in males, requires a more intensified and therefore more expensive treatment approach. Surprisingly, our results show that patients with a history of stroke caused similar health expenses to the overall population. Because ARBs and Ds are recommended for these patients and because a Swiss survey showed ARBs and Ds to be the predominantly prescribed SPC in a primary care setting, it is understandable that the expenses for both populations do not differ dramatically. Contrary to this, patients with impaired renal function generated exceedingly high costs. Even though blockers of the renin-angiotensin- aldosteron-system are commonly used in patients with impaired renal function, loop diuretics might often be used for volume control. Worthwhile mentioning is the net benefit of an aggressive treatment with ARBs in patients in stages of diabetic nephropathy in which a significant renoprotective effect can be observed. Slowing the progression of end-stage renal disease, substantial cost savings can be made [26]. It is assumable that the higher day therapy costs for patients with impaired renal function may result from the increased use of ARBs. As per table 1, costs of these substances are remarkably higher compared to HCTZ. Due to the fact that loop diuretics are not commonly used as combination therapy partners and because patients with impaired renal function frequently need individualised adjustments to their therapy, SPCs may not be the first choice for these patients.
Possibly also the hope for the results of ALTITUDE [27] may have induced a more frequent use of DRIs in these patients, contributing to a pool of factors for higher costs. Patient management appears to be equally difficult in patients with heart failure and shows the same monetary implications.
ARBs exceeded the medication costs for ACEIs. However, considering the latest cost-efficacy analyses, it must be noted that despite nominally higher daily treatment costs, the antihypertensive effect and the adverse side-effect profile for ARBs are more favourable than for older drugs like Ds or BBs. The increased compliance resulting in substantial cost savings [28] may therefore justify higher daily treatment costs. The use of flat priced combination therapies of ARBs within SPCs may lead to a further increase of compliance compensating additional therapy costs. Compared to a German study, average day therapy costs for SPC of either ARB/Ds or ARB/CCB/Ds appeared to be cheaper (CHF 1.67 – CHF 2.66 [universal currency converter, accessed 11.12.2012, http://www.xe.com/ucc/ ] vs. CHF 0.56 – CHF 1.94 in Switzerland) [29]. Despite the findings of an Italian investigation reporting Ds and BBs to be highly cost-effective, control rates remained low with these drugs [30]. Studies show that BBs aggravate insulin resistance (with the exception of carvedilol and nebivolol) and are therefore not recommended as first-line therapies [31]. Also, highly dosed Ds have diabetogenic potential.
The data from Swiss surveys indicates an exceedingly high use of Ds in Swiss primary care [32] as Ds are often perceived to be the preferred approach for initial treatment of mild to moderate hypertension [33]. Considering increased costs for potential new onset diabetes of 549 US-Dollars per patient and incremental costs of 30,000 US-Dollars, the use of Ds/BBs has been shown to be economically and medically unpropitious [34]. Another analysis yielded savings of 18,96 Euros in Great Britain and 13,21 Euros in Sweden for new-onset diabetes mellitus using CCBs instead of BBs [34]. Our data showed only a marginal monetary difference comparing prices of the maximal doses of either, CCBs (CHF 1.09) and BBs (CHF 1.03).
The results of this study show that DFC implies a higher burden in the Swiss healthcare system than SPC. Due to high tablet consumption, it can be estimated that only 60% of the prescribed pills are actually taken. Currently, an average compliance-related financial loss of CHF 604,607 per year can be expected for all patients in the analysis. A study indicated that significant improvements (p <0.001) in compliance could be accomplished using SPC (mean compliance 78.1%) compared to DFC (mean compliance 71.5%) leading to a reduction in all-cause hospitalisations in a real-life general practice [29]. Some authors therefore state that a general lowdose combination therapy might be an appropriate cost-effective method to improve tolerability, efficacy and compliance [30]. As opposed to other countries where health insurers reimburse only restricted formularies, Switzerland is less dramatically faced with the necessity to switch to cheaper but less tolerated substances [35]. Therefore, this factor may not contribute that much to extensive add-on treatment decisions if the patient is not controlled. SPCs not only appear to be cheaper, they also lower the risk of treatment interruptions due to side effects. Studies show that patients who have interrupted their antihypertensive treatment within the first year had higher hospitalisation rates and higher healthcare expenses [36].
Conclusions
Day therapy costs for the Swiss antihypertensive treatments differ according to region, substance class, cardiovascular risk and additional diseases. A disproportionately high amount of money is expected to be wasted due to compliance reasons. The prescription of monotherapies appears to be a major cost factor especially in stage-II-and III-HT and in patients with blood pressure measuring <120/80 mm Hg due to the preferred prescription of monotherapies or DFC. The use of a SPC-therapy can be considered as an intelligent treatment approach throughout all blood pressure stages and can contribute to major cost savings up to CHF 38,383,000 per annum. In addition, SPC are known to increase efficacy and reduce side effects. Therefore their use in patients with hypertension should be – whenever possible – and depending on additional comorbidities, the preferred choice of drug formulation.
Limitations and future work
In our analysis we exclusively used prices of the largest available tablet-boxes on the Swiss market. Due to obvious price differences, we had to assume that physicians prescribe these packs more often to patients treated with an unchanged regimen of more than three months. The calculation of day therapy costs was based on the largest available tablet boxes, which implied the cheapest expenditures. Because this is an assumption, the actual day therapy costs might be higher. Another limitation can be seen in the nature of the study. Because this is a cross sectional analysis, calculated annual therapy costs cannot sufficiently reflect possible dropouts due to the death of patients. Additionally, it must be taken into consideration that the calculation of compliance-related financial loss is based on a model and compliance has not actually been investigated. As a result calculated costs are estimations and the validity of the data cannot be completely assured. It also must be mentioned that compliance rates investigated by Claxton et al. [17] were analysed in a controlled setting. Their transferability in a real world setting, like a cross sectional analysis may imply limitations especially with regards to the duration of treated hypertension. Furthermore, loop diuretics account for high daily therapy costs and a vast amount of patients receiving furosemide and torasemide were diagnosed with heart failure or impaired renal function. Therefore, this investigation partly reflects a patient population that has to be treated intensively according to severe current conditions other than hypertension. This cost impact partly distorts calculations and must be taken into consideration.
Based on our data a follow-up investigation should be undertaken to assess the actual savings potential of every patient receiving more than one monosubstance by assessing the possibility of switching the patient on SPC comprising the exact same substance (1st level) and on another substance within the same substance class (2nd level). However, it must not be forgotten that there are major differences in efficacy and safety profiles of compounds within the same substance class. Therefore, an investigation on 2nd level would be more relevant for academic reasons and less relevant for daily practice. In addition, further research on the size of prescribed tablet boxes is needed to investigate whether or not the savings potential of choosing the right package may benefit the Swiss health economy.
References
1 Simpson FO. Long-term cost and life-expectancy consequences of hypertension. J Hypertens. 1998;16:1099–100.
2 Leone A. The Economic Costs for the Control of Cardiovascular Risk: An Overview. Current Pharmaceutical Design. 2013;19(13):2447–53.
3 Aronow WS. Optimal Blood Pressure Goals in Patients With Hypertension at High Risk for Cardiovascular Events. Am J Ther. 2013 (epub ahead of print).
4 Karakurt P, Kasikci M. Factors affecting medication adherence in patients with hypertension. Journal of vascular nursing: official publication of the Society for Peripheral Vascular Nursing 2012;30:118–26.
5 Chrostowska M, Narkiewicz K. Improving patient compliance with hypertension treatment: mission possible? Curr Vasc Pharmacol. 2010;8:804–7.
6 LaFleur J, Oderda GM. Methods to measure patient compliance with medication regimens. J Pain Palliat Care Pharmacother. 2004;18:81–7.
7 McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. The Ann Pharmacother. 2002;36:1331–6.
8 Sherrill B, Halpern M, Khan S, Zhang J, Panjabi S. Single-pill vs free-equivalent combination therapies for hypertension: a meta-analysis of health care costs and adherence. J Clin Hypertens. (Greenwich) 2011;13:898–909.
9 Jackson K. Persistence of fixed versus free combination with valsartan and HCTZ for patients with hypertension. Value Health Suppl. 2006;9:A363.
10 Schafer HH, Sudano I, Theus GR, Noll G, Burnier M. Target blood pressure attainment with antihypertensive therapy in Swiss primary care. Blood pressure. 2012;21:211–9.
11 Schafer HH, Sudano I, Theus GR, Zilla P, Noll G, Burnier M. Blood pressure target attainment in the background of guidelines: the very elderly in Swiss primary care. Fam Pract. 2012;29:511–20.
12 Bleichrodt H, Quiggin J. Life-cycle preferences over consumption and health: when is cost-effectiveness analysis equivalent to cost-benefit analysis? J Health Econ. 1999;18:681–708.
13 Chrysant SG. Using fixed-dose combination therapies to achieve blood pressure goals. Clin Drug Investig. 2008;28:713–34.
14 Kjeldsen SE, Messerli FH, Chiang CE, Meredith PA, Liu L. Are fixed-dose combination antihypertensives suitable as first-line therapy? Curr Med Res Opin. 2012;28:1685–97.
15 Schweizereische Eidgenossenschaft BfS. Gesundheitsdienste und Personal, Andere ambulante Dienste – Indikatoren. Ärzte und Zahnärzte 2011. http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/03/03/key/01.html
16 Swiss Society of Hypertension. Arterielle Hypertonie, Empfehlungen für Ärzte, Expertenmeinung ohne Haftung. www.swisshypertension.ch/docs/guidelines_2009_d_leaflet.pdf, last access date 29.08.2013.
17 Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clinical therapeutics. 2001;23:1296–310.
18 Schweizerische Eidgenossenschaft, Bundesamt für Statistik. Schätzungen zur Bevölkerung der Schweiz 2012. http://www.news.admin.ch/message/index.html?lang=de&msg-id=45493, last access date 29.08.2013.
19 Schweizerische Herzstiftung. Zahlen und Fakten zum Bluthochdruck. 2007. http://www.blutdruck-offensive.ch/uploads/media/zahlen_und_fakten_d_01.pdf, last access date 29.08.2013.
20 Schweizerische Eidgenossenschaft BfS. Bevölkerungsstand und -struktur – Indikatoren, Bevölkerung nach Alter, Ständige Wohnbevölkerung nach Alter am Jahresende 2012. In; 2012
21 Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA: the journal of the American Medical Association 2003;289:2363–9.
22 Edwards PR, Lunt DW, Fehrsen GS, Lombard CJ, Steyn K. Improving cost-effectiveness of hypertension management at a community health centre. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde 1998;88:549–54.
23 Ilesanmi OS, Ige OK, Adebiyi AO. The managed hypertensive: the costs of blood pressure control in a Nigerian town. Pan Afr Med J. 2012;12:96.
24 Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health. 1996;86:1805–8.
25 Van Wijk BL, Klungel OH, Heerdink ER, de Boer A. The association between compliance with antihypertensive drugs and modification of antihypertensive drug regimen. J Hypertens. 2004;22:1831–7.
26 Coca A. Economic benefits of treating high-risk hypertension with angiotensin II receptor antagonists (blockers). Clin Drug Investig. 2008;28:211–20.
27 Parving HH, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD, et al. Baseline characteristics in the Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Endpoints (ALTITUDE). Journal of the renin-angiotensin-aldosterone system: JRAAS 2012;13:387–93.
28 Bramlage P, Hasford J. Blood pressure reduction, persistence and costs in the evaluation of antihypertensive drug treatment – a review. Cardiovasc Diabetol. 2009;8:18.
29 Breitscheidel L, Ehlken B, Kostev K, Oberdiek MS, Sandberg A, Schmieder RE. Real-life treatment patterns, compliance, persistence, and medication costs in patients with hypertension in Germany. J Med Econ. 2012;15:155–65.
30 Ambrosioni E. Pharmacoeconomic challenges in disease management of hypertension. Journal of hypertension Supplement: official journal of the International Society of Hypertension 2001;19:S33–40.
31 Mansia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 ESH-ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood pressure. 2007;16:135–232.
32 Schafer HH, de Villiers JD, Sudano I, Theus GR, Sivukhina E, Burnier M, et al. Management of hypertension in patients with diabetes mellitus and metabolic syndrome in Swiss primary care. Int J Clin Pract. 2012;66:1125–6.
33 Rochefort CM, Morlec J, Tamblyn RM. What differentiates primary care physicians who predominantly prescribe diuretics for treating mild to moderate hypertension from those who do not? A comparative qualitative study. BMC family practice. 2012;13:9.
34 Grimm C, Koberlein J, Wiosna W, Kresimon J, Kiencke P, Rychlik R. New-onset diabetes and antihypertensive treatment. GMS health technology assessment 2010;6:doc03. doi: 10.3205/hta000081.
35 Wilson J, Axelsen K, Tang S. Medicaid prescription drug access restrictions: exploring the effect on patient persistence with hypertension medications. Am J Manag Care. 2005; 11 Spec No: SP27–34
36 McCombs JS, Nichol MB, Newman CM, Sclar DA. The costs of interrupting antihypertensive drug therapy in a Medicaid population. Medical care. 1994;32:214–26.