
Figure 1
a) Difficult assessment of the posterior pelvic ring on standard x-ray.
b) CT-scan of the same patient reveals bilateral fracture of the lateral mass of the sacrum.
DOI: https://doi.org/10.4414/smw.2013.13859
Pubic rami fractures in the elderly often occur as a result of a low-energy trauma, typically a fall from standing height [1–4]. These fractures represent the most frequent type of pelvic fractures. The overall incidence of a pelvic ring fracture is 20–37/100,000 per year [5]. The incidence rises to 92/100,000 per year when considering people >65 years only [6]. In this age group fractures typically are associated with pre-existing osteoporosis [7]. Osteoporosis and falls increase with age. With respect to demographic changes, the incidence of these fractures will increase even more [8]. Therefore prevention and treatment of osteoporosis are of major interest and research in this field has led to development of new drugs and therapeutic strategies in recent years [9, 10]. Nevertheless, osteoporotic fractures represent a substantial portion in orthopaedic trauma surgery.

Figure 1
a) Difficult assessment of the posterior pelvic ring on standard x-ray.
b) CT-scan of the same patient reveals bilateral fracture of the lateral mass of the sacrum.
Pubic rami fractures are classified as fractures of the anterior pelvic ring and from a biomechanical point of view they are considered stable fractures that allow full weight bearing. As a consequence conservative treatment consisting of analgesia and mobilisation with weight bearing as tolerated is generally applied. Contrary to this, is the experience that for many patients, even under strong analgesics, early mobilisation often is not possible or insufficient and hospitalisation becomes necessary. Different authors pointed out that isolated fractures of the anterior pelvic ring are rare. A coexistent lesion of the posterior pelvic ring is typical [11–13]. Assessment of the posterior pelvic ring with iliosacral joints and sacrum is difficult on a standard X-ray of the pelvis (fig. 1a); hence injuries of the posterior pelvic ring are frequently missed. At this time the detection of concomitant anterior and posterior pelvic ring injuries is typically done by computer tomography (CT), whereas a lesion of the posterior pelvic ring is a frequent finding (fig. 1b). With other words a relevant proportion of conventionally classified pubic rami fractures in reality comprise a posterior lesion making the injury substantially more unstable. This may explain failure of conservative treatment with persistent or even progressive pain and immobilisation after more than four to six weeks. In addition to the conventional plate and screw fixation, recent literature reports some descriptions of alternative operative techniques for pelvic ring fractures in the elderly like ramoplasty and sacroplasty where the injuries are treated with bone cement [14, 15]. These techniques are based on the principle known from vertebroplasty for the treatment of vertebral compression fractures. The reason for the report on such techniques is probably based on the fact that unsatisfying courses of these injuries are more common than generally assumed. But overall there is little literature about epidemiology, length of hospital stay, functional outcome and mortality due to these injuries [16]. The purpose of this study was based on the question of whether pelvic ring fractures from low-energy trauma in geriatric patients are underdiagnosed and undertreated or not. To answer this question we were interested in epidemiologic data from elderly patients with low-energy pelvic ring fractures. Furthermore, we were especially interested in the frequency of concomitant posterior pelvic ring lesions, the percentage of patients for whom surgery was indicated due to conservative treatment failure, and if earlier surgical treatment may be appropriate.
The present work represents a retrospective, descriptive study approved by the local ethics committee. From January 2009 to December 2011 all consecutive patients with pubic rami fractures presenting at our emergency department of a level I trauma centre have been screened. Further inclusion criteria were age >65 years and low-energy trauma. Exclusion criteria were coexistent fractures in other regions of the body, high-energy trauma, acetabular fractures, and pathological fractures by tumours. The diagnosis of pubic ramus fracture has been confirmed by standard pelvic X-ray in a.p.-projection. During the observation period additional imaging in the form of a pelvic CT-scan was performed in case of posterior pelvic ring pain as mentioned by the patient himself or in case of local tenderness in the clinical examination, although this guideline was not strictly followed. As study parameters were collected: age; sex; place of residence before injury; duration of acute hospital stay; place of residence after acute hospital stay; additional imaging (CT and/ or MRI); if CT-scan was performed, could a lesion on the posterior pelvic ring be identified (yes or no); Charlson comorbidity index (CCI); mortality after 30 days and one year mortality. Follow-up data were obtained by telephone interviews with the patient, or relatives, or primary care provider. Patient data were maintained confidentially, analysed anonymously and an accordant commitment for confidentiality was signed by all authors.
| Table 1:Baseline characteristics. | |
| Age (y) | 83.5 (IQR 66–100) |
| Gender, n (%) women | 113 (85.6%) |
| Gender, n (%) men | 19 (14.4%) |
| Charlson comorbidity index | 1.5 (0–9) |
| Residence before injury | |
| Own home, n (%) | 91 (69%) |
| Nursing home, n (%) | 37 (28%) |
| Others, n (%) | 4 (3%) |
Between January 2009 and December 2011, 182 patients older than 65 years with pubic rami fractures diagnosed on standard pelvic X-ray in a.p.-projection were screened. Fifty patients were excluded: 10 patients sustained a high energy trauma, 24 patients showed concomitant acetabular fracture, 4 patients suffered pathologic fracture, and 12 patients presented with additional fractures caused by the same the accident.
Table 1 shows the baseline characteristics of patients. Average age was 83.5 years (women 83.7, men 82.5). Women were affected 6 times more often than men (113 women, 19 men). Median Charlson Co-morbidity Index in 132 patients was 1.5 (0–9) [17].
Ninety-one (69%) patients were living independently in their own home, 37 (28%) patients were living in nursery home (NH), 1 patient came from a psychiatric hospital and for 3 patients we don’t know their previous place of residency.
In seventy (53%) patients a primary CT-scan of the pelvis was carried out in addition to the standard X-ray of the pelvis on the basis of the above mentioned criteria (dorsal pain and/or local tenderness). In thirty-eight (54%) patients a fracture of the posterior pelvic ring, mostly of the massa lateralis, was present.
No patient received primary operative fracture stabilisation. Secondary operative fracture stabilisation was performed in 5 (4%) of 132 patients. Indication for surgery was based on failure of conservative treatment what we defined as persisting or even increasing pain causing immobilisation after more than four to six weeks. In these situations we proceeded as follows: a CT-scan was performed to analyse the pelvic fracture pattern. In the case of a concomitant posterior pelvic ring injury we indicated surgical stabilisation of the fracture. We therefore used percutaneous iliosacral screw fixation for the stabilisation of the posterior pelvic ring [13] combined, if necessary, with a plate osteosynthesis of the anterior pelvic ring. Surgery was not performed before six weeks after injury. Operative treatment consisted of CT-guided percutaneous iliosacral screw fixation without bone cement augmentation in all five patients. In 4 cases the intervention was performed after 6 weeks and in one case after 12 weeks. In two of the five cases an additional anterior pelvic ring stabilisation using plates and screws was performed. All these patients gained considerable and rapid pain relief due to the stabilisation of the pelvic ring and immediate mobilisation was possible.
From 37 patients admitted from a nursing home 28 (75.7%) were returned back there the same day. Four patients (10.8%) were transferred to a rehabilitation facility with acute medical care and five patients (13.5%) stayed at the university hospital for two days on average before returning to the nursing home. Of the 91 patients coming from their own home only 2 (2.2%) of them were treated on an outpatient basis, while the other 89 patients needed hospital care. Median length of stay was 39 days (IQR 28–52).
Table 2 shows one-year mortality and changes in residential status. Of the 132 patients 2 patients were lost during follow-up. Of the remaining 130 patients 24 (18.5%) patients died within the first year. Four (12.5%) out of these 24 patients died within 30 days after injury (one on day 1, one after 2 days, one after 4 days, and one after 26 days) due to exacerbation of underlying cardiovascular disease. Of the remaining 106 patients the residential status 1 year after injury was as follows: 59 patients lived at their own home, 46 patients were institutionalised in a nursing home (NH), and one patient in an assisted living centre.
| Table 2:Residential status and mortality. | ||||
| Residence before injury | One-year mortality, n | Residence one year after injury | Loss of follow-up | |
| Own home, n (%) | 91 (69) | 7 | 59 (55.6) | |
| Nursing home, n (%) | 37 (28) | 16 | 46 (43.4) | |
| Others, n (%) | 4 (3) | 1 | 1 (1) | |
| Total (n) | 132 | 24 (18.5%) of 130 | 106 | 2 (1.5%) |
This retrospective study showed that coexistent posterior pelvic ring fractures in elderly patients with diagnosed pubic rami fractures due to low-energy trauma are frequent. As a consequence these fractures are substantially more unstable resulting in longer periods of immobilisation caused by pain. Functional impairment means loss of independence. We could show that 98% of previous community dwellers in our cohort needed a hospital stay for a mean duration of 39 days which is significantly longer than stated by other authors [2, 18–24]. Baseline characteristics of our patient cohort with a mean age of 83.5 years and a mortality rate of 18.5% correspond to those known from geriatric patients with proximal femur fractures [25–29]. The latter are in extensive focus of research for years whereas observance of pelvic ring fractures in elderly patients is lacking.
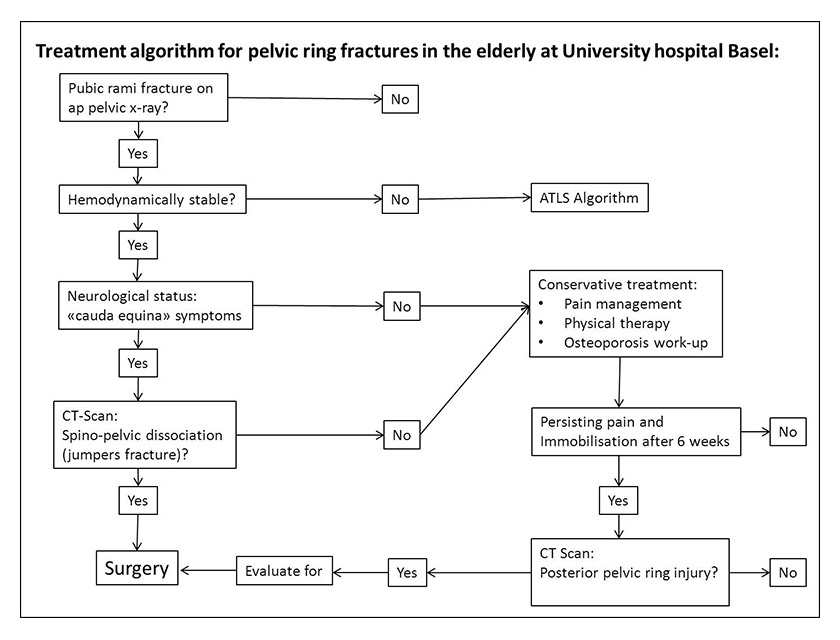
Figure 2
Currently used treatment algorithm for pelvic ring fractures in elderly patients.
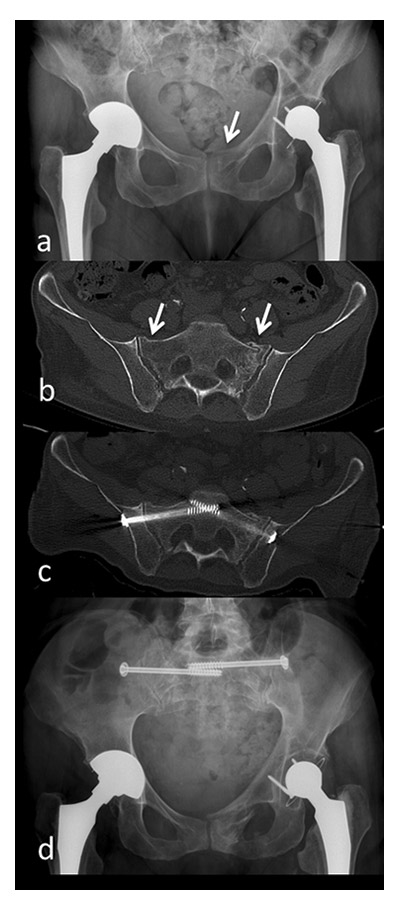
Figure 3
a) pubic ramus fracture on the left side b) CT scan six weeks after initial trauma due to increasing pain: There is a fracture of the massa lateralis on the left and a discontinuation of the cortical bone of the massa lateralis on the right c) CT-guided percutaneous screw fixation d) pelvic X-ray six weeks after surgery.
Pennal et al. in 1980 were the first to highlight that a lesion of the anterior pelvic ring must be associated with a posterior lesion [11]. The difficulty lies in the detection of posterior pelvic ring lesions on standard X-rays where they are often missed and hence not treated. To get a precise diagnosis of a pelvic fracture a CT-scan is mandatory. In our patient collective a CT-scan in addition to standard pelvic X-ray for primary diagnostics was done in 70 patients. In 54% of cases a posterior injury of the pelvic ring could be identified. This corresponds to the results published in literature [30–33]. Predictive value of anamnesis and clinical examination concerning posterior pelvic ring lesion is controversial [32, 34]. In our series we only found information about the presence or absence of posterior pelvic ring pain in 49 of 132 patients. Because of this low number and the lack of information about the pain (localisation, quantification/ score), we decided not to use this information.
Henes et al. compared the sensitivity of MRI and CT concluding that MRI is significantly more sensitive than CT for the identification of posterior pelvic ring lesions [35].
However, the question is how extensive primary additional imaging shall be used? We believe that this depends on treatment strategies. In our sample, the CT had no influence on primary therapy. For that reason we will forgo the CT-scan for primary diagnostics in our current treatment algorithm (fig. 2) that was established as a consequence of this review. On the other hand, we strongly recommend the CT-scan for precise diagnostics and planning when surgical treatment is considered.
In this study all 132 patients included were primarily subject to non-operative treatment. 5 patients (4% ) showed unsuccessful evolution with persistant pain and impaired mobility 4 to 6 weeks after injury. In all these patients secondary operative treatment with osteosynthesis by percutaneous iliosacral screw fixation (all 5 cases) and additional anterior plating (2 cases) was performed (fig. 3). Nevertheless, a comparison of these 5 cases to conservatively treated patients is inappropriate due to the low number of patients operated and the fact that patients were not initially operated on. Furthermore, it was not a purpose of this study to compare conservative and surgical treatment of these injuries. Scheyerer et al. reported operative treatment in 30% of cases, whereas patients from all ages and origin of trauma (high- and low-energy) were included [30]. Alost et al. subdivided patients into those >65 years and <65 years but they did not differentiate between low- and high-energy traumas [3]. To sum up, the literature about operative treatment for geriatric pelvic ring fractures from low-energy trauma is limited. Furthermore, authors often do not distinguish between the age of the patients and the mechanism of injury making the studied patient cohorts extremely heterogenic.
Another interesting finding of our study was the fact that the proportion of patients treated on an outpatient basis was much higher for patients coming from a nursing home (89.2%) than for previous community dwellers (2.2%). Herein we see two main reasons: one is the loss of independence caused by functional impairment due to the injury. For this purpose care in a nursing home is often sufficient whereas patients coming from their own home need at least temporary institutionalised care. A second point is that for nursing home patients the decision where they are transferred to (back to a nursing home versus admission to an acute hospital) is rather based on insurance reasons (the Swiss healthcare system in general does not fund rehabilitation for patients who were institutionalised before the injury) rather than on a clinical algorithm.
Severe weaknesses of this study are the missing data of geriatric assessment (i.e., mobility status, functional status, evaluation of bone biology) and measure of complications (i.e., respiratory infection, urinary tract infection). On the other hand, we believe that our inclusion criteria focusing on pubic rami fracture in patients older than 65 years and low-energy trauma only, are strengths of this study, as is a loss of follow-up of only two patients. Including 132 patients our study represents one of the larger cohorts focusing on osteoporotic pelvic ring fractures due to low-energy trauma and is therefore a useful contribution to the very low number of studies available in the literature.
A coexistent posterior lesion of the pelvic ring in pubic rami fracture is frequent. On standard pelvic X-ray posterior lesions are commonly missed and hence pelvic ring fractures tend to be underdiagnosed and undertreated. Regarding fracture healing these injuries in general show good results with non-operative treatment, but the time for recovery is longer than generally assumed.
Baseline characteristics of elderly patients with pelvic ring fractures are comparable to patients with proximal femur fractures. In contrast to the latter which are extensively discussed in literature, pelvic ring fractures in geriatric patients lacks observance.
With respect to the results of this study, a more aggressive approach for the treatment of geriatric patients with pelvic ring fractures may be appropriate. One possibility is the use of new drugs with the with the aim of accelerated fracture healing like parathyroid hormone 1‒84 as presented by Peichl et al. [36]. Early surgical therapy by minimal invasive techniques that have low morbidity and are based on the results of systematically deployed CT-scans may be considered as well. To further compare these treatment options, a prospective randomised study with adequate geriatric assessment, osteoporosis work-up and well defined functional outcome parameters would be necessary.
1 Kannus P, Palvanen M, Parkkari J, Niemi S, Järvinen M. Osteoporotic pelvic fractures in elderly women. Osteoporosis Int. 2005;16(10):1304–5.
2 Schapira D, Militeanu D, Israel O, Scharf Y. Insufficiency fractures of the pubic ramus. Semin Arthritis Rheum. 1996;25(6):373–82.
3 Alost T, Waldrop RD. Profile of geriatric pelvic fractures presenting to the emergency department. Am J Emerg Med. 1997;15(6):576–8.
4 Boufous S, Finch C, Lord S, Close J. The increasing burden of pelvic fractures in older people, New South Wales, Australia. Injury. 2005;36(11):1323–9.
5 Melton LJ 3rd, Sampson JM, Morrey BF, Ilstrup DM. Epidemiologic features of pelvic fractures. Clin Orthop Relat Res. 1981;(155):43–7.
6 Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970–1997 and alarming projections for the new millennium. Osteoporos Int. 2000;11(5):443–8.
7 Suhm N, Lamy O, Lippuner K, Reto B, Marc-Antoine K, Olivier L, et al. Management of fragility fractures in Switzerland: results of a nationwide survey. Swiss Med Wkly. 2008;138(45-46):674–83.
8 Callaway DW, Wolfe R. Geriatric trauma. Emerg Med Clin North Am. 2007;25(3):837–60.
9 Lippuner K. The future of osteoporosis treatment – a research update. Swiss Med Wkly. 2012;142:w13624.
10 Rizzoli R, Kraenzlin M, Krieg MA, Mellinghoff HU, Lamy O, Lippuner K. Indications to teriparatide treatment in patients with osteoporosis. Swiss Med Wkly. 2011;141:w13297.
11 Pennal GF, Tile M, Waddell JP, Garside H. Pelvic disruption: assessment and classification. Clin Orthop Relat Res. 1980;(151):12–21.
12 Gertzbein SD, Chenoweth DR. Occult injuries of the pelvic ring. Clin Orthop Relat Res. 1977;(128):202–7.
13 Isler B, Ganz R. Classification of pelvic ring injuries. Injury. 1996;27(Suppl 1):S-A3–12.
14 Shuler TE, Boone DC, Gruen GS, Peitzman AB. Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions. J Trauma. 1995;38(3):453–8.
15 Beall DP, D'Souza SL, Costello RF, Prater SD, Van Zandt BL, Martin HD, et al. Percutaneous augmentation of the superior pubic ramus with polymethyl methacrylate: treatment of acute traumatic and chronic insufficiency fractures. Skeletal Radiol. 2007;36(10):979–83.
16 Frey ME, Depalma MJ, Cifu DX, Bhagia SM, Carne W, Daitch JS. Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J. 2008;8(2):367–73.
17 Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5);373–83.
18 Dechert TA, Duane TM, Frykberg BP, Aboutanos MB, Malhotra AK, Ivatury RR. Elderly patients with pelvic fracture: interventions and outcomes. Am Surg. 2009;75(4):291–5.
19 Hill RM, Robinson CM, Keating JF. Fractures of the pubic rami. Epidemiology and five-year survival. J Bone Joint Surg Br. 2001;83(8):1141–4.
20 Koval KJ, Aharonoff GB, Schwartz MC, Alpert S, Cohen G, McShinawy A, et al. Pubic rami fracture: a benign pelvic injury? J Orthop Trauma. 1997;11(1):7–9.
21 Leung WY, Ban CM, Lam JJ, Ip FK, Ko PS. Prognosis of acute pelvic fractures in elderly patients: retrospective study. Hong Kong Med J. 2001;7(2):139–45.
22 Morris RO, Sonibare A, Green DJ, Masud T. Closed pelvic fractures: characteristics and outcomes in older patients admitted to medical and geriatric wards. Postgrad Med J. 2000;76(900):646–50.
23 O’brien DP, Luchette FA, Pereira SJ, Lim E, Seeskin CS, James L, et al. Pelvic fracture in the elderly is associated with increased mortality. Surgery. 2002;132(4):710–14.
24 Krappinger D, Kammerlander C, Hak DJ, Blauth M. Low-energy osteoporotic pelvic fractures. Arch Orthop Trauma Surg. 2010;130(9):1167–75.
25 Kenzora JE, McCarthy RE, Lowell JD, Sledge CB. Hip fracture mortality. Relation to age, treatment, preoperative illness, time of surgery, and complications. Clin Orthop Relat Res. 1984;(186):45–56.
26 Zuckerman JD, Sakales SR, Fabian DR, Frankel VH. Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program. Clin Orthop Relat Res. 1992;(274):213–25.
27 Fitzgerald JF, Moore PS, Dittus RS. The care of elderly patients with hip fracture. Changes since implementation of the prospective payment system. N Engl J Med. 1988;319(21):1392–7.
28 Sexson SB, Lehner JT. Factors affecting hip fracture mortality. J Orthop Trauma. 1987;1(4):298–305.
29 Keller JM, Sciadini MF, Sinclair E, OʼToole RV. Geriatric trauma: demographics, injuries, and mortality. J Orthop Trauma. 2012;26(9):161–5.
30 Scheyerer MJ, Osterhoff G, Wehrle S, Wanner GA, Simmen HP, Werner CM. Detection of posterior pelvic injuries in fractures of the pubic rami. Injury. 2012;43(8):1326–9.
31 Wetzel E, Strauss LR, Göpfrich M, Oellers B. Potentialities of radiological diagnosis of injuries to the dorsal pelvic ring. Rofo. 1985;142(3):291–5.
32 Schädel-Höpfner M, Celik I, Stiletto R, Giannadakis K, Froehlich JJ, Gotzen L. Computed tomography for the assessment of posterior pelvic injuries in patients with isolated fractures of the pubic rami in conventional radiography. Chirurg. 2002;73(10):1013–8.
33 Hoffmeyer P, Seigne JM, Garcia J, Vasey H. The value of computerized tomography in fractures of the pelvic ring. Int Orthop. 1984;8(1):1–8.
34 Alnaib M, Waters S, Shanshal Y, Caplan N, Jones S, St Clair Gibson A, et al. Combined pubic rami and sacral osteoporotic fractures: a prospective study. J Orthop Traumatol. 2012;13(2):97–103.
35 Henes FO, Nüchtern JV, Groth M, Habermann CR, Regier M, Rueger JM, et al. Comparison of diagnostic accuracy of Magnetic Resonance Imaging and Multidetector Computed Tomography in the detection of pelvic fractures. Eur J Radiol. 2012;81(9):2337–42.
36 Peichel P, Holzer LA, Maier R, Holzer G. Parathyroid hormone 1-84 accelerates fracture-healing in pubic bones of elderly osteoporotic women. J Bone Joint Surg Am. 2011;93:1583–7.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.