ABC versus CAB for cardiopulmonary resuscitation: a prospective, randomized simulator-based trial
DOI: https://doi.org/10.4414/smw.2013.13856
Stephan
Marsch, Franziska
Tschan, Norbert K
Semmer, Roger
Zobrist, Patrick
Hunziker, Sabina
Hunziker
Summary
QUESTIONS UNDER STUDY: After years of advocating ABC (Airway-Breathing-Circulation), current guidelines of cardiopulmonary resuscitation (CPR) recommend CAB (Circulation-Airway-Breathing). This trial compared ABC with CAB as initial approach to CPR from the arrival of rescuers until the completion of the first resuscitation cycle.
METHODS: 108 teams, consisting of two physicians each, were randomized to receive a graphical display of either the ABC algorithm or the CAB algorithm. Subsequently teams had to treat a simulated cardiac arrest. Data analysis was performed using video recordings obtained during simulations. The primary endpoint was the time to completion of the first resuscitation cycle of 30 compressions and two ventilations.
RESULTS: The time to execution of the first resuscitation measure was 32 ± 12 seconds in ABC teams and 25 ± 10 seconds in CAB teams (P = 0.002). 18/53 ABC teams (34%) and none of the 55 CAB teams (P = 0.006) applied more than the recommended two initial rescue breaths which caused a longer duration of the first cycle of 30 compressions and two ventilations in ABC teams (31 ± 13 vs.23 ± 6 sec; P = 0.001). Overall, the time to completion of the first resuscitation cycle was longer in ABC teams (63 ± 17 vs. 48 ± 10 sec; P <0.0001).
CONCLUSIONS: This randomized controlled trial found CAB superior to ABC with an earlier start of CPR and a shorter time to completion of the first 30:2 resuscitation cycle. These findings endorse the change from ABC to CAB in international resuscitation guidelines.
Abbreviations
ABC Airway-Breathing-Circulation
CAB Circulation-Airway-Breathing
CPR cardiopulmonary resuscitation
Introduction
The acronym ABC stands for Airway-Breathing-Circulation while the acronym CAB stands for Circulation-Airway-Breathing. ABC has been the recommended approach to victims of cardiac arrests for decades [1–5]. In 2005, the guidelines of the European Resuscitation Council recommended the initiation of chest compressions before ventilation (i.e. CAB) [6, 7] while the guidelines of the American Heart Association continued to recommend the ABC approach with two rescue breaths preceding cardiac massage [8]. In the current 2010 version, both European and American guidelines jointly recommend CAB [9, 10].
The rationale for changing from ABC to CAB was to emphasize the priority of chest compressions and minimise delays to their execution [6, 7, 10]. As time consuming manoeuvres to facilitate ventilation such as positioning of the head and achieving a tight seal of a bag mask apparatus can be carried out in parallel to cardiac massage, the delay in ventilation due to CAB was hypothesized to be minimal [10].
No published human or animal data demonstrate that choosing ABC or CAB has an impact on outcome. Moreover, there is only limited evidence that CAB actually has the intended effect of minimising the delay to chest compression at the cost of a minimal delay in ventilation [11].
The difference between ABC and CAB is limited to the very beginning of cardiopulmonary resuscitation (CPR) efforts. A clinical study assessing this phase would be extremely difficult to conduct as monitoring equipment should be functional or an observer present at the very onset of a cardiac arrest. As medical simulation allows the recording of data from both “patient” and first responders right from the start of an event [11, 12], this technology is perfectly suited to investigate the very early phase of a cardiac arrest.
Accordingly, the aim of the present randomized controlled trial was to compare ABC with CAB in simulated cardiac arrests.
Methods
Participants
The study was approved by the regional ethical committee and all participants gave written informed consent. Participants were general practitioners and hospital physicians from all over Switzerland participating in workshops at the simulator centre at the University Hospital of Basel.

Figure 1
Instruction of the ABC algorithm corresponding to the 2005 guidelines of the American Heart Association [8]. The instruction includes illustrations from the electronic version of the 2005 guidelines of the American Heart Association [8] and the European Resuscitation Council [6]. Reprint with permission of the publishers.

Figure 2
Instruction of the CAB algorithm corresponding to the 2005 guidelines of the European Resuscitation Council [6]. The instruction includes illustrations from the electronic version of the 2005 guidelines of the American Heart Association [8] and the European Resuscitation Council [6]. Reprint with permission of the publishers.
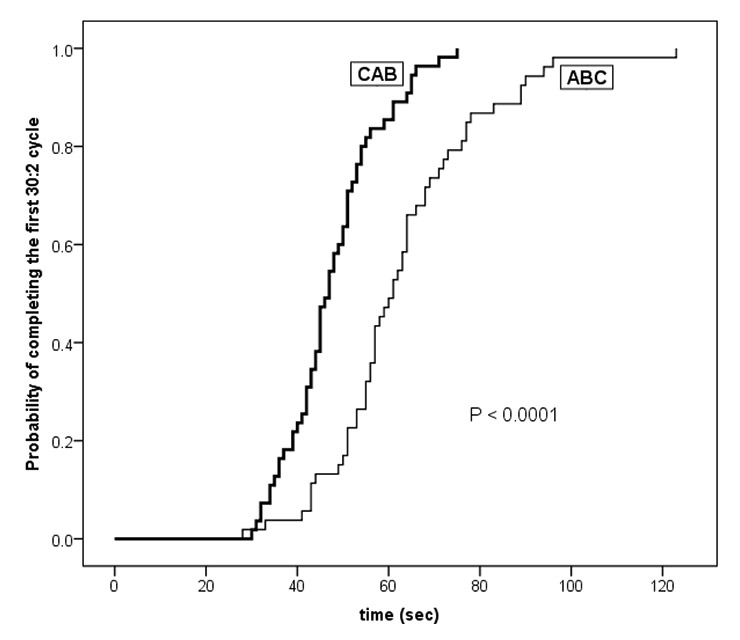
Figure 3
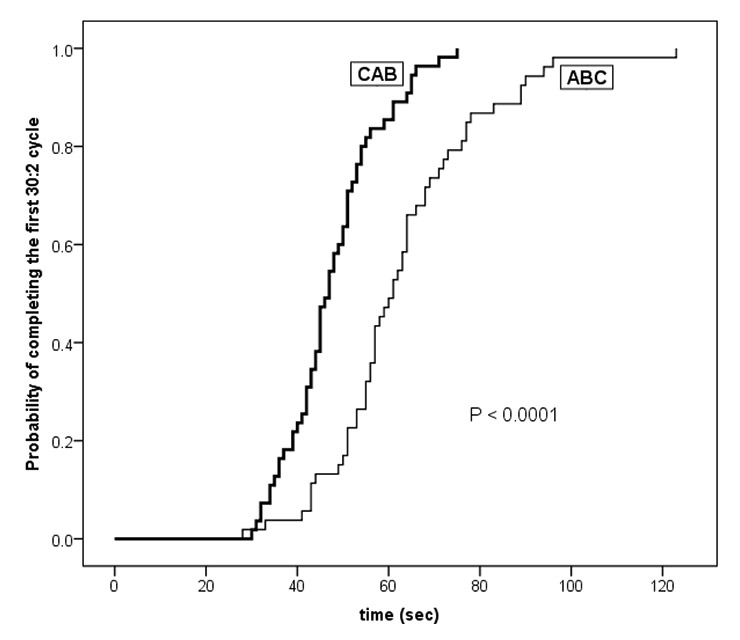
Kaplan-Meier diagram displaying the probability of completing the first resuscitation cycle consisting of 30 compressions and 2 ventilations over time. Teams were randomized to apply either ABC or CAB as initial approach to CPR. Time 0 is defined as first touch of the patient by one of the rescuers. Curves differ significantly (log-rank test).
Study design
This is a prospective randomized controlled single-blind study, the participants not being aware of the purpose of the study. The rationale for designing this study was the lack of controlled data comparing ABC and CAB for the initial phase of CPR advocated in international resuscitation guidelines published in 2005 [6, 8]. The study was conducted from 2007 to 2010. After the publication of the 2010 guidelines jointly advocating the CAB approach the investigators unanimously agreed that it would not be appropriate to draw our participants’ attention to an algorithm no longer recommended and, therefore, decided to terminate the study.
Participants from single workshops were randomly assigned to teams of two. Each team was completed by a registered nurse. The nurse played the role of a policeman called to the scene carrying emergency equipment including a bag mask apparatus and a defibrillator. Teams were randomly allocated (sealed envelopes) to receive one of two versions of a graphical instruction of the resuscitation algorithm (fig. 1 and 2): ABC (corresponding to the 2005 guidelines of the American Heart Association [8]) or CAB (corresponding to the 2005 guidelines of the European Resuscitation Council [6]). Instructions consisted of one single sided A4 size page and included: (1) a flowchart displaying the resuscitation algorithm in German language; and (2) graphical illustrations of the sequence of crucial steps (diagnosis, cardiac massage, ventilation, and defibrillation). Flowchart and illustrations were copied from the electronic versions of the 2005 resuscitation guidelines. Except for the initial measure (two rescue breaths or immediate cardiac massage) advocated after the diagnosis of cardiac arrest, both versions of the instructions were identical.
Scenario
All participants received a 15 min standardised instruction of the patient simulator (Human Patient Simulator, METI, Sarasota, FL, USA). Features of this simulator include palpable pulses, spontaneous breathing with visible thoracic excursion, eyes with spontaneous lid movements and a speaker in the mannequin’s head that broadcasts the voice of an operator to give the illusion that the “patient” can talk.
Prior to the simulation the two participants allocated to form a team were led to a separate room and were briefed that: (1) their roles were that of physicians volunteering to cover a first aid post at a large sports event; (2) the room they had just entered was supposed to be the physicians’ resting room of the first aid post; (3) in case of a medical emergency a policeman would arrive and lead them to the patient; (4) the policeman would carry emergency equipment and was trained in its use; and (5) they had now the possibility to refresh their knowledge on current algorithms of CPR. Participants then received the graphical instruction of their allocated algorithm and were asked to read it carefully. 10 minutes after the participants had received these instructions the policeman entered the room and led them to the patient.
The patient (simulator) was a middle aged man, dressed as a sports fan, presenting with an out of hospital unwitnessed cardiac arrest due to ventricular fibrillation. The patient was pulseless, apnoeic, had his eyes closed and did not react to verbal commands or painful stimuli. Ventricular fibrillation could be diagnosed on the display of the defibrillator. Provided that a least one complete cycle of 30 compressions and two ventilations (primary outcome) had been performed, the patient converted to sinus rhythm and regained consciousness following the second defibrillation.
After the simulation the participants were handed a questionnaire and asked to rate the algorithm previously received on a 10 point Likert scale with regard to: (1) the perceived helpfulness of the algorithm in handling the scenario experienced (0 = completely useless, 10 = extremely helpful); and (2) the perceived simplicity of following the algorithm in the scenario experienced (0 = extremely easy, 10 = extremely difficult).
Data analysis
Data analysis was performed using video recordings obtained during simulations by two independent observers (one nurse and one physician, both working in intensive care with regular exposition to CPR in real cases and teaching scenarios). Inter-observer differences in timing of events of ≤5 seconds were considered as agreement, and the shorter of the two readings was used for further analysis. Inter-observer differences in timing of events of >5 seconds were solved by jointly reviewing the video recordings. The first touch of the patient by one of the participants was defined to be the starting point for the timing of all events.
Statistics
The primary endpoint was the time to completion of the first resuscitation cycle of 30 compressions and two ventilations. We assumed that if ABC and CAB were started simultaneously and both carried out correctly, the time to completion of the first resuscitation cycle should be identical. Secondary endpoints were timings of other resuscitation events in the initial phase (check of airway and pulse, positioning of a face mask, first defibrillation) and the results of the post-simulation questionnaire. A difference of ≥10 seconds in the primary outcome was considered to be of clinical significance. In the absence of data relating patient outcomes with the timeliness of cardiac massage, this 10 second difference had to be arbitrarily chosen. We had two lines of reasoning: (1) if performed properly, a 30:2 cycle lasts approximately 20 seconds so that a 10 second difference represents a 50% difference; (2) in previous simulator-based studies we observed that those participants that followed the CPR algorithm exactly required approximately 50 seconds to diagnose the arrest, initiate CPR and complete the first 30:2 cycle. In this context a 10 second difference represents a 20% difference.
A power analysis, based on data of a previous study [13] revealed that approximately 60 teams had to be studied in each group to detect this difference with significance levels of 0.05 and 90% power. Anticipating a 10% rate of technical difficulties or major protocol deviations we planned to include 66 teams in each group and anticipated a study period of four to five years. All data were analysed on an intention to treat basis. Data are means ± SD unless otherwise stated. Statistical analysis was performed using SPSS (version 19.0). Student’s t-test, chi-square test, and log-rank test were applied as appropriate. A P <0.05 was considered to represent statistical significance.
Results
During the study period a total of 109 consecutive teams were assessed for eligibility and all 109 teams were included in the trial. Fifty four teams were randomized to ABC and 55 teams were randomized to CAB. All teams received the algorithm according to their randomization arm and no protocol violation occurred. Since video recording was erroneously started too late to capture the initial phase of the scenario in one team of the ABC group, this team was excluded from further analysis. Thus, 53 ABC teams and 55 CAB teams were analysed. Twenty one of the 53 ABC teams and 23 of the 55 CAB teams were composed of two general practitioners each while the remaining teams were composed of two hospital physicians each. All hospital physicians were working in internal medicine or in a sub-speciality of internal medicine. Gender distribution (36 women: 70 men vs. 36 women: 74 men) and age (39 ± 9 vs.41 ± 11 years) did not differ between the groups.
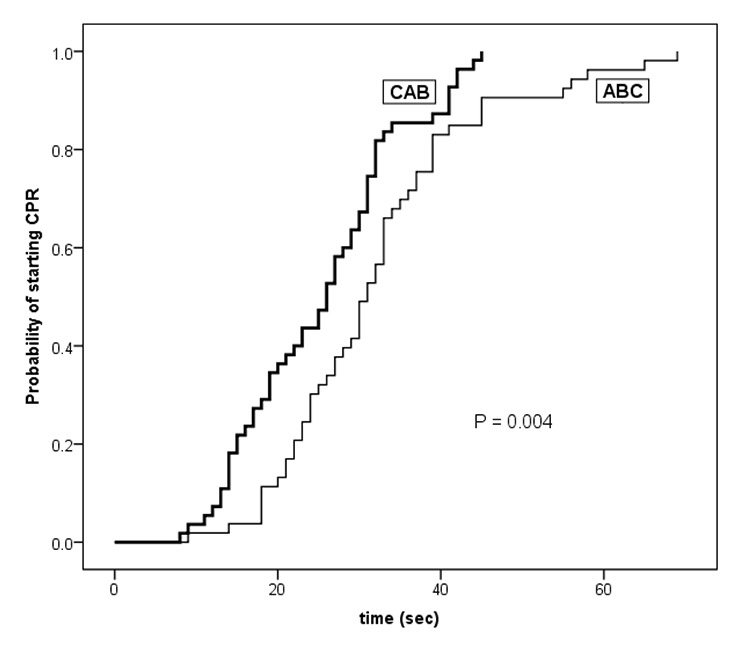
Figure 4
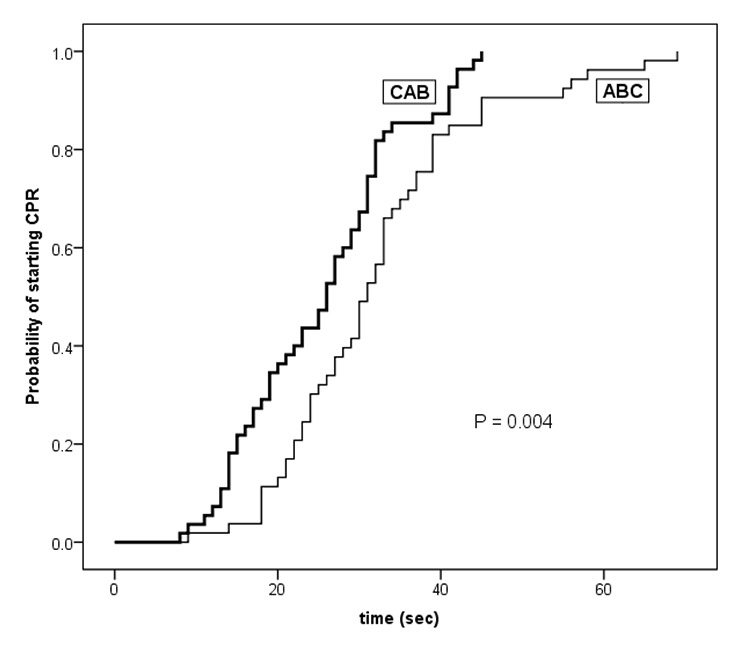
Kaplan-Meier diagram displaying the probability of executing a first initial measure of CPR over time. Teams were randomized to apply either ABC or CAB as initial approach to CPR. Time 0 is defined as first touch of the patient by one of the rescuers. Curves differ significantly (log-rank test).
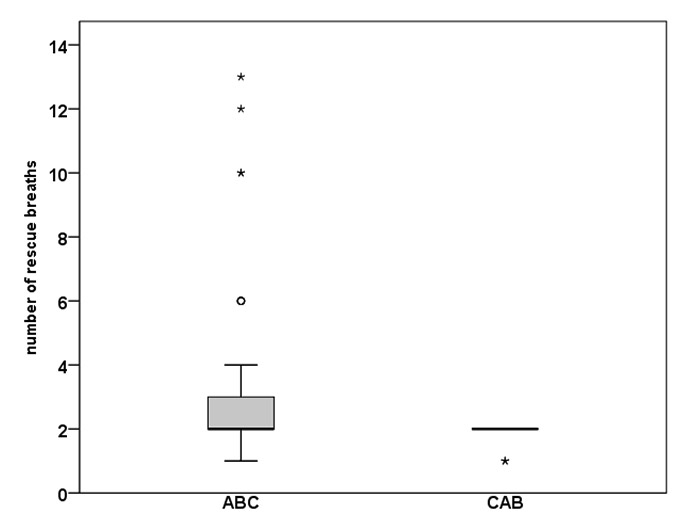
Figure 5
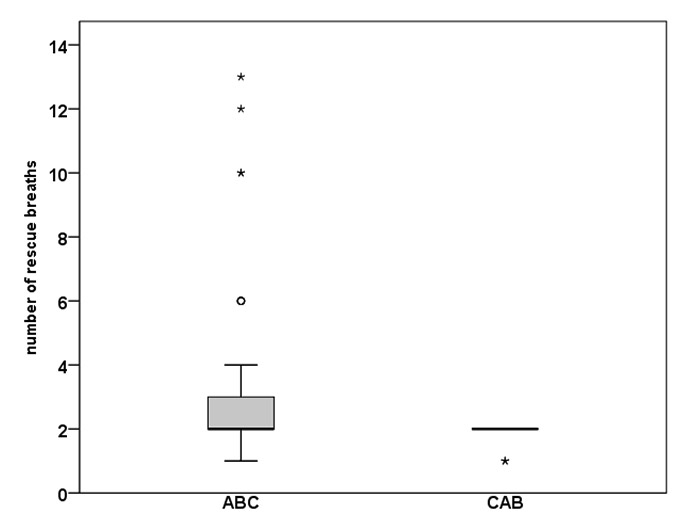
Box and whisker plot displaying the number of rescue breaths applied in the initial cycle consisting of 30 compressions and 2 ventilations. Teams were randomized to use either ABC or CAB as initial approach to CPR. Groups differ significantly (P = 0.006; chi-square test). * = one group; º = 3 groups.
Seven of the 53 teams allocated to the ABC algorithm started CPR with cardiac massage rather than rescue breaths: five of these seven teams took an active decision to start cardiac massage while experiencing technical problems with the bag mask apparatus; one team started with cardiac massage without apparent reason; in the remaining team a participant falsely announced that he had just performed the rescue breaths, which prompted his partner to start cardiac massage.
Two of the 55 teams allocated to the CAB algorithm started CPR with rescue breaths rather than with cardiac massage, both doing so without apparent reason. An additional four CAB teams took an active decision to continue cardiac massage during the first cycle beyond the recommended 30 strokes until they had solved their technical problems with the bag mask apparatus.
Primary endpoint (fig. 3): The time to completion of the first resuscitation cycle of 30 compressions and two ventilations was 63 ± 17 sec in the ABC group and 48 ± 10 sec in the CAB group (P <0.0001). Further analysis revealed that this difference was due to a combination of a later start and a longer duration of the first cycle in ABC teams (fig. 4, table 1).
Secondary endpoints: 18/53 ABC teams (34%) and none of the 55 CAB teams (P = 0.006) applied more than the recommended two initial rescue breaths (fig. 5). Accordingly, the time necessary to deliver the initial rescue breaths differed between the groups (6 ± 8 vs. 3 ± 2 sec; P = 0.03). As expected, this time did not differ between the 37 ABC teams delivering the recommended two rescue breaths exactly and the CAB teams (3 ± 1 vs. 3 ± 2 sec; P = 0.88). In all subsequent cycles, all teams consistently applied two breaths.
Table 1 displays the timing of events while table 2 shows the adherence to algorithm in the further course of resuscitation. Though teams performed, as recommended, a median of five consecutive 30:2 cycles prior to the first defibrillation and between the first and second defibrillation respectively, there was a surprisingly high variance in the number of cycles performed (range 2–8, interquartile range 2) with no significant difference between the groups. While 49/53 ABC teams and 51/55 CAB teams consistently counted the massage strokes within a given cycle aloud, only 29/53 ABC teams and 32/55 CAB teams made any statement regarding the number of cycles already performed or still to be performed, and only 5/53 ABC teams and 6/55 CAB teams systematically counted the cycles aloud.
The perceived helpfulness of the algorithm was rated with a median of 8 in both groups, with an interquartile range of 6-9 in the ABC group and 7-9 in the CAB group (P = 0.46). The perceived simplicity of following the algorithm was rated with a median of 3 (interquartile range 2–6) in the ABC group and with a median of 2.5 (interquartile range 1–5) in the CAB group (P = 0.13).
|
Table 1: Timing of events. |
| |
ABC(n = 53)
|
CAB(n = 55)
|
P
|
| Check airway (sec) |
8 ± 6 |
7 ± 8 |
0.79 |
| Check pulse (sec) |
16 ± 13 |
8 ± 6 |
0.0001 |
| Mask positioned on face (sec) |
36 ± 16 |
38 ± 13 |
0.56 |
| Start of rescue breaths (sec) |
37 ± 15 |
43 ± 10 |
0.005 |
| Start of cardiac massage (sec) |
43 ± 16 |
25 ± 9 |
0.0001 |
| Start of first 30:2 cycle (sec) |
32 ± 12 |
25 ± 10 |
0.002 |
| Length of first 30:2 cycle (sec) |
31 ± 13 |
23 ± 6 |
0.0001 |
| End of first 30:2 cycle (sec) |
63 ± 17 |
48 ± 10 |
0.0001 |
| 1st Defibrillation (sec) |
154 ± 77 |
138 ± 43 |
0.18 |
| Data (means ± SD) are time intervals between time 0, defined as first touch of the patient by one of the rescuers and the occurrence of the event specified. |
|
Table 2: Adherence to algorithm after the first cycle. |
| |
ABC(n = 53)
|
CAB(n = 55)
|
| 30 massage strokes per cycle |
52/53 |
54/55 |
| Chest compression rate ≥100/min* |
44/53 |
40/55 |
| 2 breaths per cycle |
53/53 |
55/55 |
| 5 cycles until 1st defibrillation |
20/53 |
16/55 |
| Defibrillation with one shock only |
51/53 |
54/55 |
| 5 cycles until 2nd defibrillation |
21/53 |
29/55 |
| * measured in the 2nd cycle performed.
No significant differences between the groups |
Discussion
The present study demonstrates that starting CPR using the CAB approach leads to a shorter time interval to complete the first 30:2 resuscitation cycle than using the ABC approach. This difference is due to a combined effect of a shorter initial delay to start resuscitation measures in the first place and a shorter duration of the 30:2 resuscitation cycle itself.
After decades of advocating ABC, the 2010 resuscitation guidelines universally advocate CAB [9, 10, 14, 15]. Briefly, current guidelines recommend: 1) starting CPR with cardiac massage (CAB), 2) performing high-quality CPR (compression to ventilation ratio of 30:2, compression rate of at least 100/min, compression depth of at least 5cm, full chest recoil between compressions); 3) rapid defibrillation if indicated; and 4) two minute cycles of cardiac massage and ventilation between subsequent defibrillations [10].
The change from ABC to CAB was primarily based on the theoretical consideration that in non-asphyxial cardiac arrest ventilation is initially less important than chest compression, and that delays in, and interruptions of, chest compressions should be minimized [6, 7, 10]. These considerations were endorsed by observational data [16–19]. In addition, the accumulation of evidence that the outcome after CPR with chest compressions only is not worse than after conventional CPR may have contributed to the change [20, 21].
The key findings of the present study are in agreement with the results of a recent manikin-based study in the paediatric settings [11] and empirically confirm two major theoretical rationale for the change from ABC to CAB in resuscitation guidelines: 1) CAB leads to a shorter delay in chest compressions [10]; and 2) CAB leads only to a minimal delay in ventilation, as time consuming manoeuvres necessary to allow ventilation to be performed can be carried out during on-going chest compressions [10]. Moreover, our findings highlight that bag mask ventilation is a technically demanding task that may prove to be difficult to perform correctly and in a timely fashion.
If the ABC and CAB approach were to be carried out correctly, the time to completion of the first resuscitation cycle of 30 compressions and two ventilations should be identical. Our results demonstrate that this is not the case: the ABC approach is associated with a longer delay in initiating the first resuscitation measure. Moreover, starting CPR with ventilation apparently carries the risk of substantially more than the recommended two initial rescues breaths being applied, thereby further delaying chest compressions. Although the difference between ABC and CAB consists of a mere change in the initial sequence of two resuscitation measures, ABC is obviously more difficult to perform correctly and in timely fashion than CAB. To the best of our knowledge, this is the first study demonstrating that in designing an algorithm the sequencing of events may have a profound effect on the quality of execution. Thus, the design of future algorithms in the medical field should be guided by empirical research on how easily the algorithm can be followed by healthcare workers [22].
We observed a remarkable variance in the adherence to individual components of the CPR algorithm [23]. While almost all teams performed the recommended 30 chest compressions in each compression-ventilation cycle, less than half of the teams performed the recommended five compression-ventilation cycles between defibrillations. This appears to result from the fact that chest compressions within cycles were systematically counted aloud, whereas compression-ventilation cycles were only rarely counted. Keeping track of quantitative information poses a major problem for working memory, especially if the numbers change over time [24]; it therefore requires additional support, for instance by counting aloud. In the case of resuscitation, the perspective needs to change back and forth between attending to a lower task level (compression within cycles) and to a higher level (cycles between defibrillations). Such a change of perspective is difficult, similar to the difficulties encountered when attending to individual actions as well as the wider team context [25, 26]. In the present case, a solution might involve having one team member count compressions, thus focusing on the lower level, while the other one counts cycles, thus focusing on the higher level. This observation therefore has implications for teaching medical algorithms, most notably in terms of attending to team coordination as a task in its own right [27–30].
No randomised trial has ever compared ABC and CAB with regard to hard patient outcomes. As the available evidence, including the present study, almost exclusively favours CAB [16–19], it appears highly unlikely that such a trial will be conducted in the near future. However, the comparison of registry-based patient data from the time, where ABC and CAB were simultaneously recommended might reveal differences, if any, in patient outcomes.
The present study included Swiss physicians. Curricula of all Swiss medical schools encompass education in basic and advanced life support. Postgraduate training in CPR and exposition to cardiac arrests depend on speciality and institution chosen and may vary substantially. Training courses in resuscitation including the ACLS course (advanced cardiac life support) are available on a commercial basis. The successful completion of such courses is a prerequisite for the access to the final Swiss board exam in only a small minority of specialties
Limitations of simulator-based studies include the absence of real patients. However, when performance markers such as hands-on time and technical quality of CPR are assessed, findings in simulator-based studies show a high agreement with findings in real cases [12, 27]. A particular strength of simulation is the possibility of recording objective data from both “patient” and participants right from the start of a cardiac arrest. Thus, simulation enabled us to investigate a topic that for a variety of medical, practical and ethical reasons is very difficult to investigate in situations involving real patients. Further strengths of the present study include the sample size and the identical conditions for all participants.
In conclusion, the present study demonstrates that the CAB approach is easier to perform correctly and in a timely fashion than the ABC approach. CAB is associated with a shorter delay in starting resuscitation and a shorter duration of the first resuscitation cycle of 30 compressions and two ventilations. These findings endorse the change from ABC to CAB in international resuscitation guidelines.
References
1 Cardiopulmonary resuscitation: Statement by the ad hoc committee on cardiopulmonary resuscitation of the division of medical sciences, national academy of sciences-national research council. JAMA. 1966;198:372–9.
2 Standards for cardiopulmonary resuscitation (CPR) and emergency cardiac care (ECC). JAMA. 1974;227:833–68.
3 Standards and guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiac Care (ECC). National Academy of Sciences – National Research Council. JAMA. 1986;255:2905–89.
4 Standards and guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiac care (ECC). JAMA. 1980;244:453–509.
5 Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Resuscitation. 2000;46:1–448.
6 European Resuscitation Council Guidelines for Resuscitation 2005. Resuscitation. 2005;67S1:S1–S189.
7 Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L. European Resuscitation Council Guidelines for Resuscitation 2005: Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2005; 67(Supplement 1):S7–S23.
8 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV1–203.
9 Koster RW, Baubin MA, Bossaert LL, Caballero A, Cassan P, Castr+®n M, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2010;81:1277–92.
10 Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: Adult Basic Life Support. Circulation. 2010;122:S685–S705.
11 Lubrano R, Cecchetti C, Bellelli E, Gentile I, Loayza Levano H, Orsini F, et al. Comparison of times of intervention during pediatric CPR maneuvers using ABC and CAB sequences: A randomized trial. Resuscitation. 2012;83:1473–7.
12 Marsch SC, Tschan F, Semmer N, Spychiger M, Breuer M, Hunziker PR. Performance of first responders in simulated cardiac arrests. Crit Care Med. 2005;33:963–7.
13 Hunziker S, Tschan F, Semmer NK, Zobrist R, Spychiger M, Breuer M, et al. Hands-on time during cardiopulmonary resuscitation is affected by the process of teambuilding: a prospective randomised simulator-based trial. BMC Emerg Med. 2009;9:3.
14 Australian Resuscitation Council NZRC. Basic Life Support: Cardiopulmonary Resuscitation. ARC and NZRC Guideline 2010. Emergency Medicine Australasia. 2011;23:259–60.
15 Klemmer U. Reanimationsrichtlinien 2010. Schweizerische Arztezeitung 2011;92:62–3.
16 Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of Continuous Chest Compressions During Cardiopulmonary Resuscitation: Improved Outcome During a Simulated Single Lay-Rescuer Scenario. Circulation. 2002;105:645–9.
17 Assar D, Chamberlain D, Colquhoun M, Donnelly P, Handley AJ, Leaves S, et al. Randomised controlled trials of staged teaching for basic life support: 1. Skill acquisition at bronze stage. Resuscitation. 2000;45:7–15.
18 Heidenreich JW, Higdon TA, Kern KB, Sanders AB, Berg RA, Niebler R, et al. Single-rescuer cardiopulmonary resuscitation: “two quick breaths” – an oxymoron. Resuscitation. 2004;62:283–9.
19 Kobayashi M, Fujiwara A, Morita H, Nishimoto Y, Mishima T, Nitta M, et al. A manikin-based observational study on cardiopulmonary resuscitation skills at the Osaka Senri medical rally. Resuscitation. 2008;78:333–9.
20 Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. The Lancet. 369:920–6.
21 Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, et al. Effectiveness of Bystander-Initiated Cardiac-Only Resuscitation for Patients With Out-of-Hospital Cardiac Arrest. Circulation. 2007;116:2900–7.
22 Dainty KN, Brooks SC, Morrison LJ. Are the 2010 guidelines on cardiopulmonary resuscitation lost in translation? A call for increased focus on implementation science. Resuscitation 2012.
23 Osterwalder JJ, Braun D. Strengths and weaknesses of chest compression training: a preliminary retrospective study. Swiss Med Wkly. 2011;141:w13221.
24 Bogenstatter Y, Tschan F, Semmer NK, Spychiger M, Breuer M, Marsch S. How accurate is information transmitted to medical professionals joining a medical emergency? A simulator study. Hum Factors. 2009;51:115–25.
25 Driskell JE, Salas E, Johnston J. Does stress lead to a loss of team perspective? Group Dynamics: Theory, Research, and Practice 1999;3:291–302.
26 Tschan F, Vetterli M, Semmer NK, Hunziker S, Marsch SC. Activities during interruptions in cardiopulmonary resuscitation: a simulator study. Resuscitation. 2011;82:1419–23.
27 Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O’Hearn N, Wigder HN, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428–34.
28 Hunziker S, Johansson AC, Tschan F, Semmer NK, Rock L, Howell MD, et al. Teamwork and leadership in cardiopulmonary resuscitation. J Am Coll Cardiol. 2011;57:2381–8.
29 Hunziker S, Tschan F, Semmer NK, Marsch SC. Importance of leadership in cardiac arrest situations: from simulation to real life and back. Swiss Med Wkly. 2013;143:w13774.
30 Tschan F, Semmer NK, Gautschi D, Hunziker P, Spychiger M, Marsch SU. Leading to recovery: Group performance and coordinative activities in medical emergency driven groups. Human Performance. 2006;19:277–304.