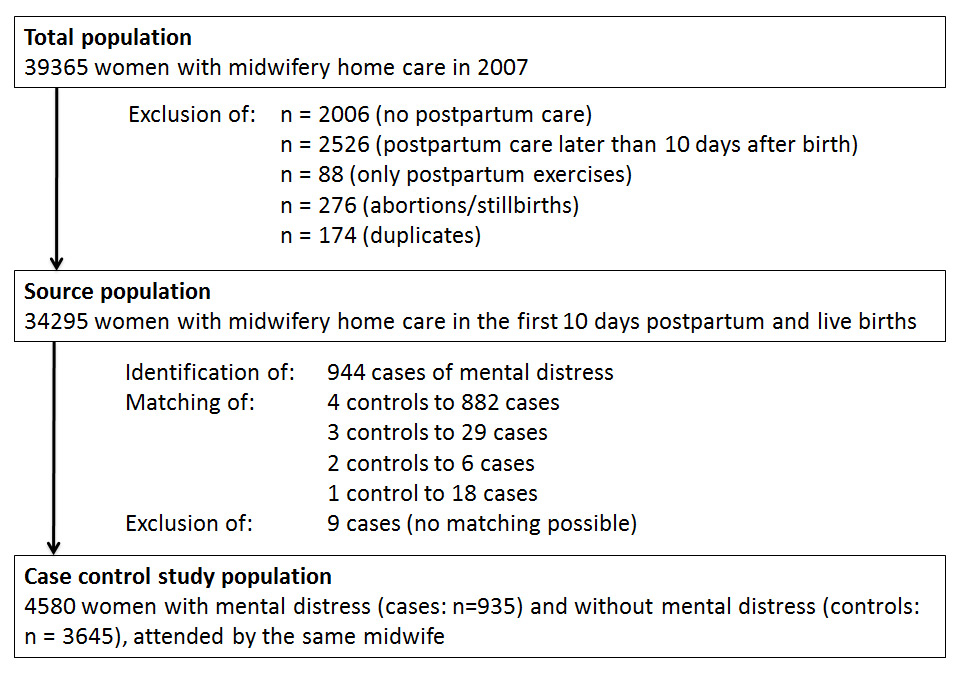
Figure 1
Study population.
DOI: https://doi.org/10.4414/smw.2013.13862
Transition to motherhood is a time of heightened vulnerability to emotional problems. New mothers are faced with multiple biological, psychological and social changes and demands requiring adjustments and often involving difficulties and concerns [1–4]. Against the background of possible underlying genetic or dynamically evolved vulnerabilities, these changes may trigger mental health problems [5]. Up to 50% of all mothers are confronted with mental health problems in the first postpartum year [6–9]. Separate conditions such as the baby blues, postpartum depression, postpartum psychoses, anxiety, posttraumatic stress disorder and disorders of the mother-infant relationship have been described [6–8, 10]. Other authors define mental health problems more broadly as mental distress including all conditions that affect emotional status of women around childbirth such as anxiety, depression, worry, control, quality of life, sleep disturbances, and low self-esteem [4, 7, 9, 11].
Despite of the high occurrence of these mental conditions, they often remain unrecognised and untreated, which can have pernicious short- and long-term effects for the mother, the child and the family ([8, 12]. Since mothers tend to see themselves as suffering from a “normal” condition, they often do not pro-actively seek help for treatment [13–15]. The involvement of midwives or other health care professionals, who visit women at home, may facilitate early identification of mental health problems [8, 16]. Actually, the first phase after hospital discharge may be a particularly sensitive period with respect to the development of mental distress [17]. This period is a trying time, often without professional stand-by, when the mother returns home with the newborn and is confronted with the responsibility for infant care, breastfeeding and recovery from birth in her social environment [18].
In Switzerland, standard care for childbirth is provided by obstetricians. However, many women engage the additional care of independent midwives. In 2007, approximately 50% of all child-bearing women had midwifery home-care after childbirth, 9% antenatal care and 4% intrapartum care (midwife-led births at home or in birthplaces) [19]. Continuous care by the same independent midwife during pregnancy, delivery and in the postpartum period was delivered to 3.8% of all child-bearing women. Postnatal visits of midwives mostly begin after hospital discharge, at around the 5 th day postpartum. Until 10 days after childbirth these consultations are reimbursed by the mandatory health insurance. On average, 3.8 visits take place in the first 10 days postpartum [19].
In recent years, the length of stay in hospital after childbirth has steadily decreased from an average stay of 5.9 days in 2000 to 5.03 days in 2011 for vaginal deliveries without complications [20, 21]. Annual statistics of a large hospital in Zurich shows even shorter hospital stays with an average of 5.4 days in 2007 and 4.2 days in 2010, being lowest in mothers with single infants delivered vaginally and at term (4.7 days in 2007 and 3.6 in 2010) [22, 23]. With the introduction of the diagnose-related groups (DRGs) in Switzerland in 2012 a further decrease is expected, because it becomes more lucrative for a hospital to release a patient as soon as possible, while the old system with daily rates for a hospital bed provided rather an incentive to extend hospital stays [24]. Against this background, the need for home-visiting midwives in the first days postpartum may rise in forthcoming years. Midwives therefore will probably be more commonly confronted with the very early problems of mental health.
Research on predictors of postpartum maternal mental health problems, so far, has paid little attention to the period immediately after hospital discharge and on midwifery care. Previous studies mostly were conducted later than four weeks after childbirth [25–34]. The few studies performed in the first days after childbirth were undertaken, when women were still in hospital [6, 35–42]. They identified the following predictors of maternal distress: psychological factors (history of depression, elevated trait anxiety, vulnerable personality style, stressful life events, low life satisfaction, low self-esteem) [35, 38, 39], socio-demographic factors (young age, being a single parent, lower social class, lower educational level, immigration, lack of perceived support) [38, 40–42], maternal factors (primiparity, multiparity, negative experience of labor, short inter-pregnancy interval, dissatisfaction with infant feeding method) [35, 38, 40–42] and infant-related factors (serious health problems of the infant, low birthweight) [35, 40].
The aim of this study was to provide information about socio-demographic, maternal, and infant-related predictors of postpartum maternal mental distress in the first ten days after childbirth, making use of the data from the Swiss national statistical database of independent midwives, which collects data in the home care setting.
Our study is based on the Swiss national statistical database of independent midwives, a compulsory, annually updated administrative-clinical database. It holds standardised data about the services and all care provided by independent midwives in Switzerland, collected during home visits. The questionnaire comprises all relevant information related to pregnancy, birth and the postpartum period (e.g. socio-demographic situation of the mother, number of midwifery consultations, location and course of delivery, birth outcomes, reasons for postnatal visits). The rates of missing data are low (at most 5%, depending on the question).
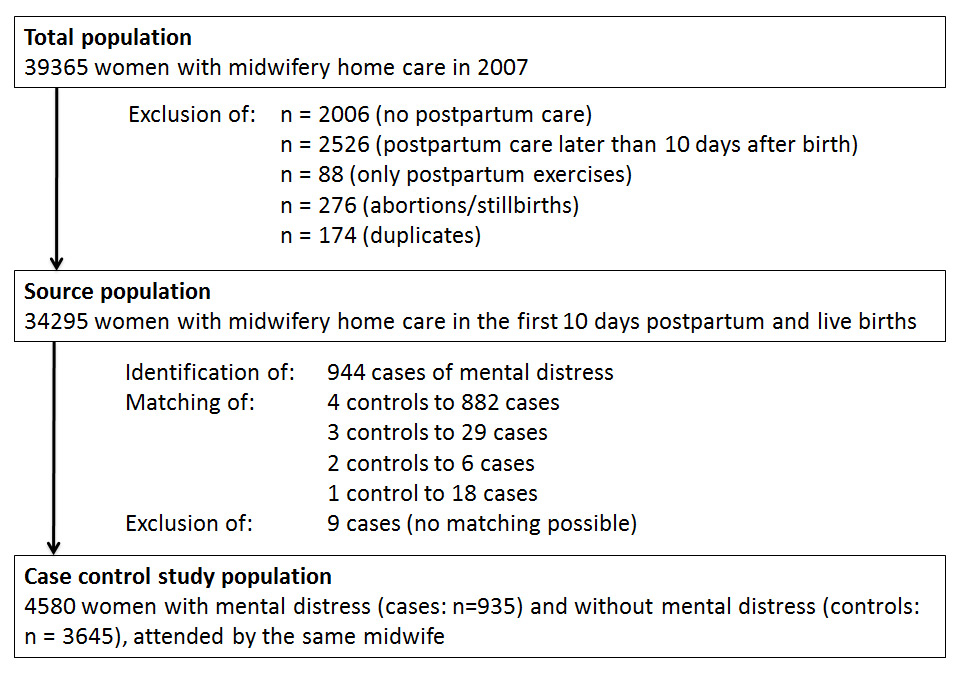
Figure 1
Study population.
We used the 2007 data, covering all mothers whose midwifery home care was completed between 1 January and 31 December 2007. Overall, 722 independent midwives provided care for 39,365 women [19]. For the present study, we included only mothers with live births and with midwifery care in the first 10 days after childbirth (N = 34,295) (fig. 1). From this source population, both cases and controls were sampled for the present nested case-control study to analyse a range of exposures potentially associated with maternal distress.
Eligible cases of maternal distress were all mothers in the source population, for whom the attending midwife had documented an entry of “postpartum depression” and/or “maternal decompensation” in the data form (n = 944). Decompensation – a term commonly used in Switzerland – describes a high level of distress and generally indicates that a person can no longer manage his/her daily life without getting (professional) support. Maternal distress in our study therefore not only encompasses postpartum depression, but is considered to be an indicator of a broad spectrum of mental health conditions as also defined by Jomeen [4]. The reporting of the outcome depended on each midwife’s professional assessment and clinical judgement. Hence, it was not standardised, nor were screening instruments used. Therefore, the documentation of postpartum depression does not necessarily indicate the existence of postpartum depression according to the DSM-IV definition. However, in order to account for the possibility of a differential reporting of maternal distress between midwives, a matched case-control approach was chosen with matching by midwife, assuming that each midwife adopted a consistent assessment for the women she cared for. For each case, up to four controls were selected among mothers who were attended by the same midwife but had no documentation of maternal distress (fig. 1).
The study was approved by the Swiss Federation of Midwives and the cantonal ethics committee.
The investigated predictors were selected from findings in previous research [6, 35–42]. They were defined as follows. Vocational education: years of education obtained after mandatory education, reported in three categories (<2 years, 2-4 years, >4 years). Midwife-led births: deliveries with independent midwives being the main responsible person (home deliveries or in birthplaces) versus other births (in hospitals with a medical doctor as main responsible provider). Small for date: weight below the 10th percentile for the respective gestational age according to the Fenton growth chart [43]. Gestational age of less than 37 weeks was considered as preterm birth. Pathologicalcourse of delivery: reported dystocia, induction of labor, haemorrhage, meconium-stained amniotic fluid and foetal distress. Summary indicators were constructed for the following conditions: maternal postpartum pathologies (including wound healing difficulties of the episiotomy or caesarean section cicatrice, problems with uterus involution, infection); breast or breastfeeding problems (sore nipples, skin fissures, engorgement, mastitis); infant weight gain concerns (not enough milk, insufficient weight gain); neonatal pathologies (infection, malformation, congenital heart defect, acute respiratory distress syndrome, meconium aspiration). Crying problems were also based on the midwife’s documentation. Consequently, a report of excessive crying could have been based on the midwife’s direct observation of the infant or on maternal report.
The prevalence of maternal distress was calculated for the whole source population (n = 34,295). In the case control study population (n = 4,580), the distribution of the predictors among cases and controls were compared. Simple and multivariable conditional logistic regression models were performed to calculate unadjusted and adjusted odds ratios and p-values in order to determine statistically significant differences between cases and controls (p-values <0.05) and to account for the matching [44].
For maternal age, linear association with maternal distress was tested by inserting a quadratic and cubic term into the model. Since they were not statistically significant (p >0.05), only the linear term was included in the final model. For parity, three categories were used (one, two, three and more children). The variables small for date and preterm birth were tested for interaction, yielding no statistically significant result. Thus, both variables were included in the final model.
Among 34,295 mothers with midwifery home care in the first 10 days after birth, 944 cases of maternal distress were identified. This represents a prevalence rate of 2.75% in the source population.
After excluding nine cases (no matching possible), the final sample for the case-control study included 935 cases and 3,645 controls (total: 4,580 mothers). These mothers were seen by 332 different midwives. The number of mothers attended by one midwife ranged from 3 to 125 (mean 29, SD = 25.53). Postpartum depression was documented for 546 cases (58.40% of all cases) and maternal decompensation for 412 cases (44.06%); both conditions were documented for 23 women.
Table 1 shows the distribution of the predictors among cases and controls. Case mothers were significantly older, more often of Swiss nationality, less often living with a partner and intended less frequently to return to work after birth. Other socio-demographic characteristics were similarly distributed among cases and controls.
Almost all maternal factors showed statistically significant differences between cases and controls. Women with maternal distress were more often primiparous and more likely to have attended prenatal classes compared to controls. Midwifery care during pregnancy was more frequent among the cases, whereas midwife-led births were less prevalent among the cases. Case mothers more often had undergone vaginally operative deliveries and caesarean sections and more often had a pathologic course of delivery. Concerns about infant weight gain were also more often documented in cases compared to controls.
Regarding the neonatal factors, infants with medical pathologies and crying problems were more frequently documented in cases compared to controls.
| Table 1:Distribution ofsocio-demographic, maternal and neonatal factors among cases (women with maternal distress) and controls. | |||
| Casesn = 935 n (%) | Controlsn = 3645 n (%) | P-value | |
| Socio-demographic factors | |||
| Maternal age (in years) | |||
| maternal age, mean (SD) | 32.35 (5.03) | 31.45 (5.08) | <0.001 |
| missing data | 1 | 4 | |
| Nationality | |||
| Swiss | 630 (67.38) | 2272 (62.33) | |
| European | 230 (24.60) | 1008 (27.65) | |
| non-European | 76 (8.02) | 365 (10.01) | 0.004 |
| Living with a partner | |||
| yes | 866 (92.62) | 3555 (97.53) | |
| no | 69 (7.38) | 90 (2.47) | <0.001 |
| Vocational education | |||
| >4 years | 232 (24.81) | 1029 (28.23) | |
| 2–4 years | 521 (55.72) | 1935 (53.09) | |
| <2 years | 180 (19.25) | 676 (18.55) | |
| missing data | 2 (0.21) | 5 (0.14) | 0.088 |
| Paid employment before birth | |||
| no | 302 (32.30) | 1105 (30.32) | |
| yes, part-time | 359 (38.40) | 1480 (40.60) | |
| yes, full-time | 269 (28.77) | 1044 (28.64) | |
| missing data | 5 (0.53) | 16 (0.44) | 0.433 |
| Intend to return to work after birth | |||
| no | 474 (50.70) | 1695 (46.50) | |
| yes | 461 (49.30) | 1946 (53.39) | |
| missing data | 0 (0.00) | 4 (0.11) | 0.015 |
| Maternal factors | |||
| Parity | |||
| 1 child | 580 (62.03) | 1983 (54.40) | |
| 2 children | 262 (28.02) | 1211 (33.22) | |
| 3 or more children | 93 (9.95) | 451 (12.37) | <0.001 |
| Attendance of childbirth classes | |||
| no | 412 (44.06) | 1815 (49.79) | |
| unclear | 78 (8.34) | 331 (9.08) | |
| yes | 445 (47.59) | 1496 (41.04) | |
| missing data | 0 (0.00) | 3 (0.08) | <0.001 |
| Multiple birth | |||
| no | 925 (98.93) | 3589 (98.46) | |
| yes | 10 (1.07) | 56 (1.54) | 0.247 |
| Midwifery care during pregnancy | |||
| no | 805 (86.10) | 3229 (88.59) | |
| yes | 130 (13.90) | 416 (11.41) | 0.006 |
| Midwife-led birth | |||
| no | 885 (94.65) | 3374 (92.57) | |
| yes | 50 (5.35) | 269 (7.38) | |
| missing data | 0 (0.00) | 2 (0.05) | 0.009 |
| Mode of delivery | |||
| spontaneous | 469 (50.16) | 2140 (58.71) | |
| vaginally operative | 137 (14.65) | 446 (12.24) | |
| caesarean section | 327 (34.97) | 1035 (28.40) | |
| missing data | 2 (0.21) | 24 (0.66) | <0.001 |
| Course of delivery | |||
| physiological | 370 (39.57) | 1793 (49.19) | |
| pathological | 565 (60.43) | 1849 (50.73) | |
| missing data | 0 (0.00) | 3 (0.08) | <0.001 |
| Maternal postpartum pathologies | |||
| no | 827 (88.45) | 3216 (88.23) | |
| yes | 108 (11.55) | 429 (11.77) | 0.371 |
| Breast or breastfeeding problems | |||
| no | 760 (81.28) | 2998 (82.25) | |
| yes | 175 (18.72) | 647 (17.75) | 0.418 |
| Infant weight gain concerns | |||
| no | 780 (83.42) | 3236 (88.78) | |
| yes | 155 (16.58) | 409 (11.22) | <0.001 |
| Neonatal factors | |||
| Small for date | |||
| no | 912 (97.54) | 3557 (97.59) | |
| yes | 18 (1.93) | 75 (2.06) | |
| missing data | 5 (0.53) | 13 (0.36) | 0.856 |
| Preterm birth | |||
| no | 898 (96.04) | 3496 (95.91) | |
| yes | 35 (3.74) | 143 (3.92) | |
| missing data | 2 (0.21) | 6 (0.16) | 0.718 |
| Neonatal pathologies | |||
| no | 887 (94.87) | 3516 (96.46) | |
| yes | 48 (5.13) | 129 (3.54) | 0.033 |
| Documented crying problems | |||
| no | 834 (89.20) | 3499 (95.99) | |
| yes | 101 (10.80) | 146 (4.01) | <0.001 |
The associations of the predictors with maternal distress from unadjusted and adjusted multivariable analyses are presented in table 2. In the full model, midwife-documented crying problems (Odds Ratio 3.62 [95% Confidence interval 2.64–4.97]) and not living with a partner (OR 3.06 [95% CI 2.14–4.37]) were the strongest predictors for maternal distress. Also the following conditions were significantly associated with a higher likelihood for maternal distress: older age (OR per year of age 1.06 [95% CI 1.04–1.07]), lower educational levels (OR 1.29 [95% CI 1.06–1.57] and OR 1.56 [95% CI 1.17–2.06]), midwifery care during pregnancy (OR 1.69 [95% CI 1.23–2.32]), breast or breastfeeding problems (OR 1.28 [95% CI 1.03–1.59]), concerns about infant weight gain (OR 1.54 [95% CI 1.22–1.94]), and neonatal pathologies (OR 1.49 [95% CI 1.03–2.16]).
The strongest protective factor against maternal distress was higher parity. Having had two or more than two children in comparison to having had one child was associated with a lower likelihood of maternal distress (OR 0.72 [95% CI 0.58-0.89] and OR 0.58 [95% CI 0.42–0.79], respectively). Lower risks were also seen for non-Swiss mothers compared to Swiss mothers (OR 0.79 [95% CI 0.65–0.96] for Europeans and OR 0.58 [95% CI 0.42–0.79] for non-Europeans). Furthermore, employment-related factors appear to be protective: full-time employment before birth (OR 0.74 [95% CI 0.56–0.98]) and intending to return to work after birth (OR 0.80 [95% CI 0.65–0.99]) were both associated with a lower likelihood of maternal distress.
There were only a few differences between unadjusted and adjusted odds ratios. Associations of lower educational levels, full time employment before birth and breast or breastfeeding problems with maternal distress were statistically significant only in the multivariable analysis. On the other hand, maternal factors tended to have weaker associations in the multivariable model: attending childbirth classes, mode of delivery, and course of delivery were significantly associated with maternal distress in the unadjusted models, but not in the full model.
| Table 2: Odds ratios for maternal distress, unadjusted and adjusted for all predictors. | ||||
| Unadj. Odds Ratio (95%-CI) n = 4542 | P-value | Adj. Odds Ratio (95%-CI) n = 4461 | P-value | |
| Socio-demographic factors | ||||
| Maternal age (in years) | ||||
| maternal age | 1.04 (1.02–1.05) | <0.001 | 1.06 (1.04–1.07) | <0.001 |
| Nationality | ||||
| Swiss | 1 | 1 | ||
| European | 0.81 (0.68–0.97) | 0.020 | 0.79 (0.65–0.96) | 0.020 |
| non-European | 0.73 (0.56–0.96) | 0.024 | 0.58 (0.42–0.79) | 0.001 |
| Living with a partner | ||||
| yes | 1 | 1 | ||
| no | 3.22 (2.31–4.48) | <0.001 | 3.06 (2.14–4.37) | <0.001 |
| Vocational education | ||||
| >4 years | 1 | 1 | ||
| 2–4 years | 1.22 (1.02–1.47) | 0.033 | 1.29 (1.06–1.57) | 0.013 |
| <2 years | 1.20 (0.96–1.50) | 0.116 | 1.56 (1.17–2.06) | 0.002 |
| Paid employment before birth | ||||
| no | 1 | 1 | ||
| yes, part-time | 0.88 (0.74–1.05) | 0.160 | 0.83 (0.65–1.05) | 0.125 |
| yes, full-time | 0.93 (0.77–1.13) | 0.472 | 0.74 (0.56–0.98) | 0.033 |
| Intend to return to work after birth | ||||
| no | 1 | 1 | ||
| yes | 0.83 (0.71–0.96) | 0.015 | 0.80 (0.65–0.99) | 0.036 |
| Maternal factors | ||||
| Parity | ||||
| 1 child | 1 | 1 | ||
| 2 children | 0.73 (0.62–0.86) | <0.001 | 0.72 (0.58–0.89) | 0.003 |
| 3 or more children | 0.69 (0.54–0.88) | 0.003 | 0.58 (0.42–0.79) | 0.001 |
| Attendance of childbirth classes | ||||
| no | 1 | 1 | ||
| unclear | 1.01 (0.75–1.38) | 0.929 | 0.95 (0.68–1.32) | 0.740 |
| yes | 1.32 (1.13–1.55) | <0.001 | 1.14 (0.93–1.38) | 0.202 |
| Multiple birth | ||||
| no | 1 | 1 | ||
| yes | 0.67 (0.34–1.32) | 0.247 | 0.54 (0.26–1.15) | 0.111 |
| Midwifery care during pregnancy | ||||
| no | 1 | 1 | ||
| yes | 1.47 (1.12–1.93) | 0.006 | 1.69 (1.23–2.32) | 0.001 |
| Midwife-led birth | ||||
| no | 1 | 1 | ||
| yes | 0.60 (0.41–0.88) | 0.009 | 0.61 (0.39-0.96) | 0.031 |
| Mode of delivery | ||||
| spontaneous | 1 | 1 | ||
| vaginally operative | 1.44 (1.16–1.79) | 0.001 | 1.13 (0.83–1.53) | 0.440 |
| caesarean section | 1.47 (1.25–1.73) | <0.001 | 1.12 (0.86–1.46) | 0.405 |
| Course of delivery | ||||
| physiological | 1 | 1 | ||
| pathological | 1.51 (1.30–1.76) | <0.001 | 1.23 (0.95–1.59) | 0.115 |
| Maternal postpartum pathologies | ||||
| no | 1 | 1 | ||
| yes | 0.90 (0.71–1.14) | 0.371 | 0.78 (0.61–1.01) | 0.062 |
| Breast or breastfeeding problems | ||||
| no | 1 | 1 | ||
| yes | 1.08 (0.89–1.32) | 0.418 | 1.28 (1.03–1.59) | 0.025 |
| Infant weight gain concerns | ||||
| no | 1 | 1 | ||
| yes | 1.57 (1.27–1.94) | <0.001 | 1.54 (1.22–1.94) | <0.001 |
| Neonatal factors | ||||
| Small for date | ||||
| no | 1 | 1 | ||
| yes | 0.95 (0.57–1.60) | 0.856 | 0.75 (0.43–1.31) | 0.316 |
| Preterm birth | ||||
| no | 1 | 1 | ||
| yes | 0.93 (0.64–1.36) | 0.718 | 0.92 (0.60–1.39) | 0.685 |
| Neonatal pathologies | ||||
| no | 1 | 1 | ||
| yes | 1.45 (1.03–2.05) | 0.033 | 1.49 (1.03–2.16) | 0.034 |
| Documented crying problems | ||||
| no | 1 | 1 | ||
| yes | 3.60 (2.67–4.85) | <0.001 | 3.62 (2.64–4.97) | <0.001 |
Based on a midwifery home care setting, the present study provides evidence of predictors of maternal distress immediately after childbirth: midwife-documented infant crying problems and not living with a partner were strong predictors of maternal distress, whereas higher parity seems to be protective against maternal distress. Additional factors associated with a higher likelihood of maternal distress included older age, lower educational levels, breast and breastfeeding problems, infant weight gain concerns, neonatal pathologies, and midwifery care during pregnancy. A lower likelihood for maternal distress was seen for women with foreign nationality, women who worked full-time before birth, women who intended to return to work after birth and women who gave birth in a midwife-led setting. Mode of delivery, course of delivery and preterm birth were not significantly related to maternal distress.
Previous findings on the relation between infant crying and maternal distress support our results [45–47]. Also being a single parent has been found to be a risk factor for early postpartum maternal distress [40, 42]. The results are less clear with regard to parity; primiparity as well as multiparity have been found to be associated with a higher likelihood for maternal distress [40–42]. Work-related factors have barely been investigated in the early postpartum time. Findings obtained later after childbirth show, that women who work full-time are less likely to have moderate-to-severe depressive symptoms [28]. Furthermore, unemployment has been shown to be associated with poorer maternal mental health [9]. Also in line with our results, lower educational levels and infant health problems have been described to be associated with early postpartum maternal distress [35, 40, 41], as well as maternal concerns about the babies’ health and infant care have been found to be the main subjective stressors of mothers in the early postpartum period [48]. Research covering the initial phase after childbirth has shown a higher likelihood for maternal distress at young age and with immigration status [38–40], whereas investigations performed later after childbirth have found that older age was associated with a higher risk for maternal distress but not foreign nationality [9, 49].
The present study allows a broad view on early postpartum maternal distress immediately after hospital discharge. Most studies with similar questions used screening instruments on specific mental health outcomes and usually were performed when women were still in hospital [35–42, 50]. To our knowledge, no study so far has investigated maternal distress in such a large population and examining as well as including simultaneously such a broad range of predictors (neonatal, socio-demographic, maternal). Furthermore, we can rule out selection bias because the Swiss national statistical database of independent midwives corresponds to the whole source population.
The results of our study have to be interpreted in the light of the following limitations. The data originate from the annual statistics of the services provided by independent midwives in Switzerland. The definition of the outcome was therefore not documented according to a standard definition, but depended on the clinical judgement and assessment of each midwife and on the reporting behaviour of the mother. Accordingly, a differential reporting of maternal distress between midwives is possible. To minimise this problem, a midwife-matched case-control approach was chosen, assuming that each midwife adopted a consistent assessment for the women she cared for. In addition, it has to be considered that the definition used in the present study is a broad indicator of mental health problems [4]. Nevertheless, because of the lack of standardised outcome measurement, we ran additional analyses separately for midwife-reported “maternal decompensation” and “depression” (data not shown). They yielded a very similar pattern of predictors. A further limitation is the lack of information about the previous history of the mothers’ mental health. Pre-existing psychological or psychiatric disorders have been shown to be a strong predictor for postpartum mental health problems [6, 35, 36, 38, 39, 50] and therefore could have confounded our results: Because pre-existing mental disorders or premorbid psychological traits may lower the chance of having several children or of working full-time, case mothers are possibly underrepresented in these groups. In our study, this could have resulted in a seemingly protective effect of these two conditions for mental distress. In fact, being integrated in the work force or having children is more likely in women with good health [51, 52].
Because of the cross-sectional design of the present study, we did not have any information about the duration of maternal distress, nor the direction of the association. Crying problems may lead to exhaustion and maternal distress, but depressed mothers also may interact less with their infants, thereby possibly favouring crying problems [47, 53].
Because our study only included women with midwifery home care covering only 50% of all child-bearing women in Switzerland, the sample is not representative for the whole population of new mothers. Compared to all women with live births in Switzerland, women with midwifery home care tend to be older, to be primiparous, to live with a partner and to be of non-Swiss nationality [46]. Furthermore, underprivileged mothers may not be informed about independent midwives’ postnatal home services.
Compared to other studies about maternal distress in the first week postpartum, the prevalence rate in the present survey is low (2.75%) [35–38, 40–42]. Our study is a clinical survey on maternal distress, not a prevalence study based on systematic screening. Maternal distress therefore may be underdiagnosed with possible lower detection of milder levels of maternal distress and of psychological dimensions other than depression and decompensation. This assumption is supported by the fact, that baby blues have barely been documented in our study. Furthermore, mental health does not usually constitute the main focus of the midwives’ home visits and women often do not talk about their mental health problems. Therefore, cases in our sample most likely relate to noticeable and obvious situations of elevated maternal distress. Another explanation for the low prevalence may be that the midwife’s visit per se already constitutes an intervention with a beneficial effect on mental health, which would support the importance of postnatal home care [54].
The findings of our study suggest a profile of women at risk for early maternal distress. Particular attention should be paid to mothers with excessively crying infants, to single mothers and to primipara. Postnatal home care by midwives or other health care professionals provides a unique opportunity to identify these mothers early [17], and to address possible underlying reasons for their elevated risk of maternal distress: additional demands, low perceived level of support, few possibilities to rest and low confidence in maternal competencies [5, 55]. Midwives or other health care professionals can support mothers by informing and counseling them about infant crying, breastfeeding, infant weight and infant health problems. Such support may increase mothers’ feeling of being efficacious in their role as mother, thereby reducing the risk for maternal distress [56]. Furthermore, mothers can be linked to available healthcare services and can be advised how to best draw on support from their social network to get the necessary rest, a matter of particularly urgency when infants are crying excessively and for mothers who are not living with a partner. In fact, individualised postpartum care by midwives that incorporates the assessment of predictors and that provides intensive, professionally based postpartum support has been shown to be effective in the prevention of postpartum depression [54].
Additional research is needed to clarify the association of maternal distress with nationality and midwifery care. The lower likelihood of foreign women to experience maternal distress could be caused by an underassessment of maternal distress given that midwives did not work with interpreters. Furthermore, cultural differences in perceptions and expression of mental health problems and the reporting style of foreign women can also have lead to underassessment [57].
In our study, women who had used midwifery antenatal care were at a higher risk for postpartum maternal distress, whereas intrapartum care was a protective factor. Since only about half of all women, who engage midwifery home care during pregnancy also have a midwife-led birth, these two groups are not an identical selection of women [19]. In the group with antenatal care, women with health problems, with high concerns about their own and their babies’ health, or with a greater underlying vulnerability for maternal distress may be overrepresented. On the other hand, women giving birth in a midwife-led setting are a selection of healthy, highly motivated and well educated women with a low risk medical history [58]. These differences may explain their different risk for maternal distress.
The present study provides evidence of predictors of maternal distress in a home care setting immediately after childbirth. Women with crying infants, single mothers, and primipara may need particular attention with respect to mental distress. These findings are important against the background that women with mental health problems often do not proactively seek help and that the length of hospital stay is decreasing. Midwives or other health care professionals who visit new mothers at home can play an important role in identifying, supporting and advising these women at risk.
Acknowledgement:We thank the Swiss Federation of Midwives for providing the data.
Funding / potential competing interests: The study was conducted independently of any funding sources.
1 Luyben AG, Kinn SR, Fleming VEM. Becoming a mother: women’s journeys from expectation to experience in three european countries. International Journal of Childbirth. 2011;1(1):13–26.
2 Halbreich U. The association between pregnancy processes, preterm delivery, low birth weight, and postpartum depressions – the need for interdisciplinary integration. Am J Obstet Gynecol. 2005;193(4):1312–22.
3 Beck CT. Postpartum depression: a metasynthesis. Qual Health Res. 2002;12(4):453–72.
4 Jomeen J. The importance of assessing psychological status during pregnancy, childbirth and the postnatal period as a mulidimensional construct: A literature review. Clin Eff Nurs. 2004;8:143–55.
5 Halbreich U. Postpartum disorders: multiple interacting underlying mechanisms and risk factors. J Affect Disord. 2005;88(1):1–7.
6 Henshaw C. Mood disturbance in the early puerperium: a review. Arch Womens Ment Health. 2003;6(Suppl 2):S33–42.
7 Miller RL, Pallant JF, Negri LM. Anxiety and stress in the postpartum: is there more to postnatal distress than depression? BMC Psychiatry. 2006;6:12.
8 Brockington I. Postpartum psychiatric disorders. Lancet. 2004;363(9405):303–10.
9 Romito P, Saurel-Cubizolles MJ, Lelong N. What makes new mothers unhappy: psychological distress one year after birth in Italy and France. Soc Sci Med. 1999;49(12):1651–61.
10 Austin MP. Antenatal screening and early intervention for “perinatal” distress, depression and anxiety: where to from here? Arch Womens Ment Health. 2004;7(1):1–6.
11 Fisher JR, Feekery CJ, Rowe-Murray HJ. Nature, severity and correlates of psychological distress in women admitted to a private mother-baby unit. J Paediatr Child Health. 2002;38(2):140–5.
12 Brand SR, Brennan PA. Impact of antenatal and postpartum maternal mental illness: how are the children? Clin Obstet Gynecol. 2009;52(3):441–55.
13 Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323–31.
14 Hall PL, Wittkowski A. An exploration of negative thoughts as a normal phenomenon after childbirth. J Midwifery Womens Health. 2006;51(5):321–30.
15 Foulkes M. Enablers and barriers to seeking help for a postpartum mood disorder. J Obstet Gynecol Neonatal Nurs. 2011;40(4):450–7.
16 Nagel-Brotzler A, Bronner J, Hornstein C, Albani C. Mental disorders in the peripartum period – early detection and multi-professional cooperation. Z Geburtshilfe Neonatol. 2005;209(2):51–8.
17 Logsdon MC, Tomasulo R, Eckert D, Beck C, Dennis CL. Identification of mothers at risk for postpartum depression by hospital-based perinatal nurses. MCN Am J Matern Child Nurs. 2012;37(4):218–25.
18 Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O, Epiney M. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery. 2011;27(2):237–42.
19 Schweizerischer Hebammenverband. Tätigkeitserfassung der freipraktizierenden Hebammen der Schweiz 2007 [Statistical Database of Independent Midwives’ Services in Switzerland 2007] 2008. Available from: http://www.hebamme.ch/x_dnld/stat/Statistikbericht_2007_d.pdf.
20 Bundesamt für Statistik. Medizinische Statistik der Krankenhäuser 2011 Neuchâtel. Bundesamt für Statistik; 2013. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/04/01/data/01/05.html
21 Bundesamt für Statistik. Medizinische Statistik der Krankenhäuser 2000 Neuchâtel. Bundesamt für Statistik; 2002. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/04/01/data/01/04.html.
22 UniversitätsSpital Zürich. Jahresstatistik der Geburtshilfe 2007. Klinik für Geburtshilfe. Available from: http://www.geburtshilfe.usz.ch/UeberUns/ZahlenUndFakten/Jahresstatistik/Seiten/default.aspx .
23 UniversitätsSpital Zürich. Jahresstatistik der Geburtshilfe 2010. Klinik für Geburtshilfe. Available from: http://www.geburtshilfe.usz.ch/UeberUns/ZahlenUndFakten/Jahresstatistik/Seiten/default.aspx .
24 Bartkowski R. Length of hospital stay due to DRG reimbursement. Ther Umsch. 2012;69(1):15–21.
25 Beck CT. A meta-analysis of predictors of postpartum depression. Nurs Res. 1996;45(5):297–303.
26 Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50(5):275–85.
27 Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. 2008;8:24.
28 Mayberry LJ, Horowitz JA, Declercq E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. J Obstet Gynecol Neonatal Nurs. 2007;36(6):542–9.
29 Nielsen Forman D, Videbech P, Hedegaard M, Dalby Salvig J, Secher NJ. Postpartum depression: identification of women at risk. BJOG. 2000;107(10):1210–7.
30 Righetti-Veltema M, Conne-Perreard E, Bousquet A, Manzano J. Risk factors and predictive signs of postpartum depression. J Affect Disord. 1998;49(3):167–80.
31 Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, et al. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. 2008;108(1–2):147–57.
32 Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95.
33 Patel M, Bailey RK, Jabeen S, Ali S, Barker NC, Osiezagha K. Postpartum depression: a review. J Health Care Poor Underserved. 2012;23(2):534–42.
34 Horowitz JA, Murphy CA, Gregory KE, Wojcik J. A community-based screening initiative to identify mothers at risk for postpartum depression. J Obstet Gynecol Neonatal Nurs. 2011;40(1):52–61.
35 Bergant AM, Heim K, Ulmer H, Illmensee K. Early postnatal depressive mood: associations with obstetric and psychosocial factors. J Psychosom Res. 1999;46(4):391–4.
36 Bloch M, Rotenberg N, Koren D, Klein E. Risk factors for early postpartum depressive symptoms. Gen Hosp Psychiatry. 2006;28(1):3–8.
37 Britton JR. Maternal anxiety: course and antecedents during the early postpartum period. Depress Anxiety. 2008;25(9):793–800.
38 Dennis CL, Janssen PA, Singer J. Identifying women at-risk for postpartum depression in the immediate postpartum period. Acta Psychiatr Scand. 2004;110(5):338–46.
39 Dennis CL, Ross LE. Depressive symptomatology in the immediate postnatal period: identifying maternal characteristics related to true- and false-positive screening scores. Can J Psychiatry. 2006;51(5):265–73.
40 Giakoumaki O, Vasilaki K, Lili L, Skouroliakou M, Liosis G. The role of maternal anxiety in the early postpartum period: screening for anxiety and depressive symptomatology in Greece. J Psychosom Obstet Gynaecol. 2009;30(1):21–8.
41 Gurel S, Gurel H. The evaluation of determinants of early postpartum low mood: the importance of parity and inter-pregnancy interval. Eur J Obstet Gynecol Reprod Biol. 2000;91(1):21–4.
42 Skari H, Skreden M, Malt UF, Dalholt M, Ostensen AB, Egeland T, et al. Comparative levels of psychological distress, stress symptoms, depression and anxiety after childbirth – a prospective population-based study of mothers and fathers. BJOG. 2002;109(10):1154–63.
43 Fenton TR. A new growth chart for preterm babies: Babson and Benda's chart updated with recent data and a new format. BMC Pediatr. 2003;3:13.
44 Hosmer DW, Lemeshow S. Logistic regression for matched case-control studies. In: Hosmer DW, Lemeshow S, editors. Applied Logistic Regression, second edition. New York: John Wiley & Sons; 2000. p. 223–59.
45 Miller AR, Barr RG, Eaton WO. Crying and motor behavior of six-week-old infants and postpartum maternal mood. Pediatrics. 1993;92(4):551–8.
46 Kurth E, Spichiger E, Cignacco E, Kennedy HP, Glanzmann R, Schmid M, et al. Predictors of crying problems in the early postpartum period. J Obstet Gynecol Neonatal Nurs. 2010;39(3):250–62.
47 Kurth E, Kennedy HP, Spichiger E, Hosli I, Zemp Stutz E. Crying babies, tired mothers: what do we know? A systematic review. Midwifery. 2011;27(2):187–94.
48 Hung CH. Correlates of first-time mothers’ postpartum stress. Kaohsiung J Med Sci. 2006;22(10):500–7.
49 Edge D. Ethnicity, psychosocial risk, and perinatal depression – a comparative study among inner-city women in the United Kingdom. J Psychosom Res. 2007;63(3):291–5.
50 Moayedoddin A, Moser D, Nanzer N. The impact of brief psychotherapy centred on parenthood on the anxio-depressive symptoms of mothers during the perinatal period. Swiss Med Wkly. 2013 doi: 10.4414/smw.2013.13769.
51 Cook JA. Employment barriers for persons with psychiatric disabilities: update of a report for the President’s Commission. Psychiatr Serv. 2006;57(10):1391–405.
52 Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: a population-based register study. JAMA. 2006;296(21):2582–9.
53 Reck C, Hunt A, Fuchs T, Weiss R, Noon A, Moehler E, et al. Interactive regulation of affect in postpartum depressed mothers and their infants: an overview. Psychopathology. 2004;37(6):272–80.
54 Dennis CL. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. BMJ. 2005;331(7507):15.
55 Beck CT. Theoretical perspectives of postpartum depression and their treatment implications. MCN Am J Matern Child Nurs. 2002;27(5):282–7.
56 Fish M, Stifter C. Mother parity as a main and moderating influence on early mother-infant interaction. J Appl Dev Psychol. 1993;14:557–72.
57 Halbreich U, Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J Affect Disord. 2006;91(2-3):97–111.
58 Cignacco E, Buchi S, Oggier W. Midwife-led labour in a Swiss hospital. Pflege. 2004;17(4):253–61.