Determinants of inpatient rehabilitation length of stay and discharge modality after hip and knee replacement surgery in Switzerland
DOI: https://doi.org/10.4414/smw.2013.13832
Amir
Tal-Akabi, Stefan
Schmid, Jan
Taeymans
Summary
QUESTIONS UNDER STUDY / PRINCIPLES: The aims of this study were to identify the determinants influencing the inpatient rehabilitation length of stay (LoS) and discharge modality (DisMod) after hip or knee replacement surgery.
METHODS: Data were retrieved for 306 patients (185 females, 121 males) who were admitted to a Swiss orthopaedic rehabilitation facility between 2007 and 2008 after hip or knee replacement surgery. LoS and DisMod were extracted from the medical files along with an additional seven binary and six continuous variables (including scores of timed-get-up-and-go [TUG], walking distance [WDT] and stair climbing tests [FIM_St]). Nonparametric procedures were used to detect differences between the gender groups. For the analysis of the LoS determinants, a linear regression model was used. The nonmotor performance test determinants of DisMod were analysed using a logistic regression model, whereas the motor performance test determinants were examined using binary classification. For both regression models, a backward procedure was used.
RESULTS: Unlike DisMod, LoS calculations were conducted after stratification for gender. The simplified regression models explained 22% (females) and 31% (males) of the LoS variance and 20% (both genders) of the DisMod variance. TUG, WDT and FIM_St were all important predictors for LoS, whereas DisMod could be best predicted by WDT.
CONCLUSIONS: Patients with good motor ability at admission were discharged earlier and more frequently to home. These findings might be of importance for preoperative physiotherapeutic care and might help to improve care planning as well as more accurately predict the access to inpatients beds and the allocation of resources.
A retrospective observational study
Introduction
Total hip and knee replacements (THR and TKR, respectively) rank amongst the most frequently performed surgeries worldwide. Based on the 2009 OECD prevalence data, the amount of THR surgeries in Switzerland (287 per 100,000 citizens) was the second highest after Germany (296 per 100,000 citizens) with an OECD-mean of 154 per 100,000 citizens [1]. The Geneva University Hospitals alone reported more than 4,500 THR surgeries (4,141 primary and 381 revision surgeries) between March 1996 and December 2009 [2]. The prevalence of TKR surgeries in Switzerland (200 per 100,000 citizens) ranked third following the United States and Germany (both countries 213 per 100,000 citizens) with an OECD-mean of 118 per 100,000 citizens [1].
The demand for hip and knee replacements has increased dramatically in recent years. Studies from the United States reported that the number of patients undergoing THR or TKR surgery between 1993 and 2006 increased significantly from approximately 350,000 to 800,000 individuals [3, 4]. This trend was also observed in Europe, along with a shorter length of stay (LoS) in acute care hospitals and a more frequent discharge to postacute facilities with consequent concerns about the cost-efficiency of such postacute rehabilitation programmes [4]. In Swiss hospitals, for instance, the LoS after all kinds of surgery decreased from 9.3 days in 2009 to 8.9 days in 2011 [5].
Theurl and Winner [6] investigated whether the introduction of the diagnosis-related groups (DRG) system in the nine Austrian provinces (Bundesländer) influenced the hospital LoS. They used data from 20 diagnostic groups (based on the ICD-10) between 1989 and 2003. Their findings suggested that the change of the hospital financing system had induced a substantial decrease in the average hospital LoS. The introduction of the new inpatient rehabilitation reimbursement system in Switzerland, using the DRGs with a reduction of the LoS as a primary aim, might lead to false incentives with the risk of a premature discharge of patients resulting in changes in the quality of care and affecting rehabilitation outcomes. Based on epidemiological data and the growing prevalence of these interventions, one can argue that inpatient rehabilitation following THR/TKR surgery will further increase. If rehabilitation should be financed by case-based reimbursement, a quality insurance programme would be needed and the question of LoS and discharge modality (i.e. discharge to home or discharge to other rehabilitation facility) following inpatient rehabilitation should be investigated. It is expected that due to economical restrictions, rehabilitation programmes have to start early after surgery and the inpatient programmes’ duration has to be kept as short as possible.
In order to better plan and optimise the management of an inpatient rehabilitation regimen for patients following lower extremity surgery, a deeper understanding of the determinants influencing the LoS and the discharge modality is required. An identification of these determinants could improve the rehabilitation processes as well as the quality of care through an improved care planning and a more effective allocation of resources. For example, when a patient entering the rehabilitation facility following THR/TKR surgery showed characteristics that might predict a longer duration of stay, the facility management as well as the rehabilitation and care teams could anticipate more accurately and better plan access to inpatient beds or resource allocation such as staffing [7].
Some authors have evaluated factors that influence inpatient rehabilitation LoS after primary or revision THR. For instance, Yeung et al. [8] investigated LoS of 275 inpatients following revision THR. The mean age in their study was 69 years with 62% female patients and the mean LoS was 29.6 days. Interestingly, the authors found statistically significant predictors for a longer LoS such as a low Functional Independence Measure (FIM) score at admission, female sex, revision of only the femoral component, two or more prior lower limb surgeries and two or more hip revisions. Walker et al. [9] found the same average LoS (10.5 days) for primary and revision THR patients whereas Vincent et al. [10] observed shorter LoS in primary (10 days) than in revision patients (13.1 days) and the longest LoS in patients aged more than 70 years. In addition, the authors found shorter LoS in primary compared to revision TKR patients. Other authors claimed that discharge destination for TKR patients depends on several different factors, including age, number of co-morbidities, post-operative functional ability, availability of home help, surgeon’s habits and patient’s wishes [11–13]. However, these findings were rejected by Dauty et al. [14], who doubted the predictability of such factors alone.
The aims of this study were to identify the determinants influencing the inpatient rehabilitation length of stay (LoS) and discharge modality (DisMod) following THR or TKR surgery. Identifying such determinants might help to improve the availability of inpatient beds, and improve the allocation of resources as well as the rehabilitation outcomes.
Patients and methods
Data retrieval
For this retrospective observational study, data were retrieved for all the 458 patients who were admitted to an orthopaedic rehabilitation facility in the German-speaking part of Switzerland between April 2007 and May 2008 following lower extremity surgery. To reduce the risk of bias when comparing different subgroups, however, the study was based only on patients following elective or trauma-related total or partial knee and hip replacement surgeries, leaving a study population of 306 patients.
As a standard procedure within 24 hours of admission to the rehabilitation facility, all patients were examined by trained physiotherapists. This included the following motor performance tests: timed-get-up-and-go test (TUG) [15], walking distance test (WDT) and item M (stairs) of the functional independence measures test (FIM_St) [16]. In addition, patients were screened for additional gait disorders (AGD). For the TUG, the time (in seconds) that the patients needed to stand up from a chair, walk three metres, turn around, walk back to the chair and sit back down on the chair was measured. Hence, the lower the score, the better the patients performed in the test. For the WDT, the patients were instructed to walk as far as possible without stopping and without time limitation but not longer than one 20-minute physiotherapy session, whereby the distance (in metres) was measured. Hence, the longer the distance, the better the patients performed in this test. Distances of over 400 m were defined as “unlimited distance” and the test was stopped. The FIM_St test was scored from one to seven, with higher scores representing a more independent ability to climb the stairs.
All other clinical parameters were extracted from the patients’ medical files (see tables 1 and 2 below).
Data analysis
All statistical calculations were conducted using SPSS 20 (IBM Corp., Armonk, NY, USA). The Kolmogorov-Smirnov goodness-of–fit test revealed statistically significant skewness for the continuous variables (p <0.01) and therefore the continuous variables were log-transformed before imputation in further analyses.
Nonparametric descriptive statistics and frequency analyses were used to present the results of the continuous and binary data, respectively. Mann-Whitney U tests were used to test for between-gender group differences of the continuous variables before log-transformation and the Pearson chi-squared test was used to test the between group frequencies. The same analyses were conducted for continuous and binary variables to test for discrepancies in group characteristics among those patients who were able and those who were not able to participate in the stair test (missing values for FIM_St).
Before starting the regression analyses, a correlation matrix was established using Pearson correlation coefficients, to obtain a first “picture” of the associations among the variables under investigation. As gender was associated with LoS (r = –0.119; p = 0.037; n = 306) but not with discharge modality (r = –0.042; p = 0.464; n = 306), all variables were stratified for gender in the LoS analysis, whereas gender was included as a predictor variable in the discharge modality analysis.
To evaluate the determinants influencing the length of stay (LoS), a linear regression model was used. The use of box-and-whisker plots revealed five outliers with extreme LoS values up to 90 days. To explore the sensitivity of the LoS regression model to the effect of such outliers, the procedure was repeated after excluding these extreme values. After forcing all abstracted variables in the exploratory models, a backward procedure was used, which meant that predictors with p-values of more than 0.25 were excluded from the models during the consecutive steps.
Due to a classification problem of the FIM_St variable, only the nonmotor performance test determinants of discharge modality (DisMod) were analysed using logistic regression with the same backwards procedure as described above.
To gain a better knowledge about the association between the motor performance tests at admission and DisMod, receiver operating characteristic (ROC) curves were established. Based on the optimal cut-off value of the most accurate motor performance test, its data distribution was dichotomised in order to calculate the odds ratio (OR) as well as the positive (PPV) and negative predictive values (NPV). While sensitivity and specificity are test characteristics, the PPV and NPV are of more clinical interest in context of this study.
The significance level for several statistical analyses was set at the 5% probability of error level.
|
Table 1: Descriptive statistics and between gender group comparisons (Mann-Whitney U test) for the nonlog-transformed continuous variables. |
|
Variables
|
Units
|
Female
|
Male
|
p-value
|
|
n
|
Median
|
P25
|
P75
|
n
|
Median
|
P25
|
P75
|
| Age at admission (Age)1
|
Years |
185 |
78.5 |
71.2 |
83.7 |
121 |
75.8 |
66.8 |
81.0 |
0.049* |
| Length of stay at the rehabilitation facility (LoS)1
|
Days |
185 |
20.4 |
15.0 |
22.0 |
121 |
19.0 |
15.0 |
22.0 |
0.019* |
| Time between surgery and admission to rehabilitation facility (TtoA)1
|
Days |
185 |
10.0 |
8.0 |
13.0 |
121 |
10.0 |
8.0 |
13.0 |
0.969 |
| Number of comorbidities (COM)1
|
– |
185 |
5.0 |
4.0 |
6.0 |
121 |
6.0 |
4.0 |
7.0 |
0.238 |
| Walking distance at admission (WDT)1
|
Metres |
182 |
50.0 |
20.0 |
100.0 |
117 |
60.0 |
30.0 |
120.0 |
0.270 |
| Timed-up-and-go test at admission (TUG)1
|
Seconds |
166 |
34.0 |
23.0 |
47.0 |
107 |
28.0 |
20.0 |
42.0 |
0.011* |
| Functional independence measures score for stair climbing (FIM_St)1
|
– |
146 |
1.0 |
1.0 |
5.0 |
98 |
2.0 |
1.0 |
5.8 |
0.078 |
|
1 indicates variables that were log-transformed for further analyses;
* indicates statistically significant differences (p <0.05) |
|
Table 2: Frequencies and between group comparisons (Pearson’s chi-squared test) for the binary variables that were valued “1”. |
|
Variables
|
Values
|
Frequency (%)
|
p-Value
|
|
Females
|
Males
|
| Discharge modality (DisMod) |
1 = discharge to home; 0 = discharge to supported living setting |
90.3 |
87.6 |
0.463 |
| Surgery due to trauma (TRAU) |
1 = yes; 0 = no |
23.2 |
14.9 |
0.074 |
| Multitrauma (MTRAU) |
1 = yes; 0 = no |
2.7 |
1.7 |
0.544 |
| Revision surgery (REV) |
1 = yes; 0 = no |
16.8 |
20.7 |
0.401 |
| Elective total knee replacement (ETKR) |
1 = yes; 0 = no |
36.8 |
35.5 |
0.829 |
| Elective total hip replacement (ETHR) |
1 = yes; 0 = no |
39.5 |
49.6 |
0.081 |
| Emergency total hip replacement (EmTHR) |
1 = yes; 0 = no |
23.8 |
14.9 |
0.058 |
| Additional gait disorders (AGD) |
1 = yes; 0 = no |
13.5 |
11.6 |
0.619 |
| * indicates statistically significant differences (p <0.05) |
Results
Descriptive statistics and between gender group comparisons
The median age of the 185 female patients was 2.7 years higher than the 121 male patients (p = 0.049). In addition, the male patients were discharged 1.5 days earlier from the rehabilitation facility (p = 0.019), performed significantly better in the TUG (p = 0.011) at admission and tended to perform better on the FIM_St (p = 0.078) compared with the female patients (table 1). There were no gender differences in participation rates for the motor performance tests at admission to the rehabilitation facility (WDT = 97.5%; TUG = 89%; FIM_St = 79%). No discrepancies in group characteristics were found among females with (n = 146) and without (n = 39) FIM_St values. Among males with (n = 98) and without (n = 23) FIM_St values, significant differences were found for the characteristics TRAUMA (p = 0.038), EmTHR (p = 0.038) and REV (p = 0.007).
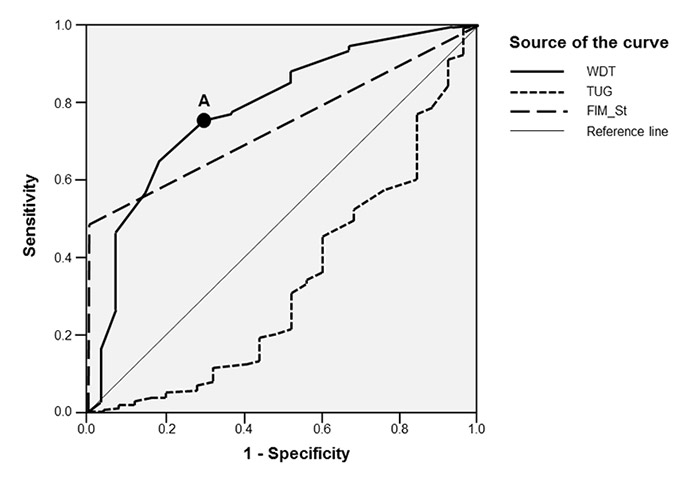
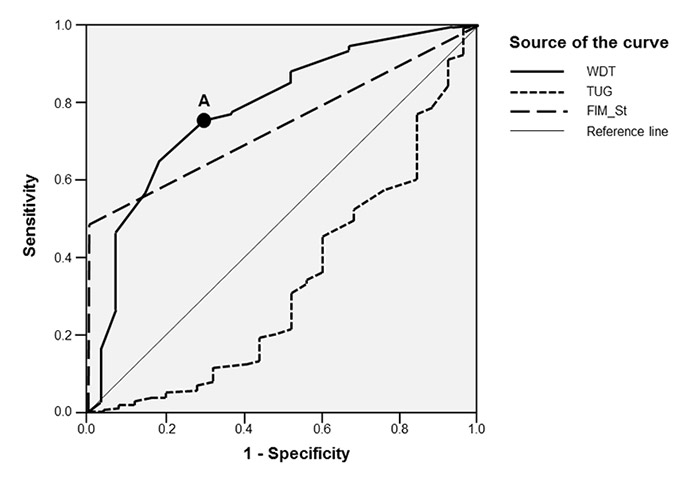
Figure 1
Receiver operating characteristic (ROC) curves for the motor tests at admission. Point “A” depicts the optimal cut-off value of 27 metres for dichotomisation of WDT.
FIM_St = functional independence measures score for stair climbing; TUG = timed-get-up-and-go test at admission; WDT = walking distance at admission
Table 2 shows the frequencies (in %) of the binary data for the female and male groups. The frequency of the “discharged to home” modality after inpatient rehabilitation was similar in both gender groups (p = 0.463).
Analysis of the determinants influencing length of stay (LoS)
When all 12 variables were forced into the explorative regression analysis, significant models (p <0.001) were obtained with R2= 0.24 (SE = 0.24) and R2 = 0.32 (SE = 0.27) in female and male samples, respectively.
The backward procedure, eliminating predictors with p-values of more than 0.25 from the forced explanatory regression equations resulted after seven and six steps, respectively, in simplified models (table 3). Several motor performance tests conducted at the time of admission were important predictors in the female and male simplified models. A sensitivity analysis to test the robustness of the models against outliers revealed no changes after excluding the extreme values.
Analysis of the determinants influencing discharge modality (DisMod)
When all non-motor performance test variables were forced into the explorative logistic regression analysis, a significant model (p <0.001) was obtained with Nagelkerke R2= 0.21 and an ability to correctly classify the cases in 90%. The simplified model, established after the backward procedure in 2 steps, was able to keep the classification capacity of 90% (table 3).
Figure 1 depicts the ROC curves for the motor performance test variables in relation to DisMod. From the three motor performance tests, the walking distance test (WDT) appeared to have the best predictive characteristics for DisMod (area under curve = 0.822; p <0.001). Therefore, the WDT data were dichotomised into the categories “poor” and “good” using a cut-off value of 27 metres (point “A”) and expressed as a new variable (WDT_dich).
Table 4 displays the frequency distribution for the variables WDT_dich and DisMod. Sensitivity and specificity for WDT_dich were 73.2% (95%CI = 67.4%–78.2%) and 70.3% (95%CI = 49.7%–85.5%) respectively. The OR for WDT_dich was 6.47 (95%CI = 5.60–7.34) and the PPV and NPV were 96% (95%CI = 92.3%–98.2%)and 21% (95%CI = 13.2%–30.6%) respectively. Test accuracy, defined as the ratio of the sum of the true positives and true negatives to the grand total, was 73% for the walking distance test.
|
Table 3: Explorative regression formulae to predict length of stay (LoS) in female and male patients and discharge modality (DisMod) in both genders. |
|
Variable
|
Gender
|
Regression formulae
|
R2
|
SE
|
p-value
|
| Length of stay at the rehabilitation facility (LoS) |
Female |
Ln(LoS) = 2.51 + 0.09xEmTHR + 0.09xLn(TtoA) + 0.10xLn(TUG) – 0.04xLn(WDT) – 0.05xLn(FIM_St) |
0.22 |
0.23 |
<0.001* |
| Male |
Ln(LoS) = 0.96 + 0.92xAGD + 0.29xMTRAU + 0.44xLn(AGE) + 0.09xLn(TUG) – 0.05xLn(WDT) – 0.08xLn(FIM_St) |
0.31 |
0.27 |
<0.001* |
| Discharge modality (DisMod) |
Both |
DisMod = 3.18 – 1.30xLn(COM) – 1.07xAGD + 1.39xREV + 1.59xETHR + 1.06xETKR |
Nagelkerke R2 = 0.20 |
– |
<0.001* |
| * indicates statistically significant model (p <0.001);
EmTHR = emergency total hip replacement; TtoA = time between surgery and admission to rehabilitation facility; TUG = timed-get-up-and-go test at admission; WDT = walking distance at admission; FIM_St = functional independence measures score for stair climbing; AGD = additional gait disorders; MTRAU = multitrauma; AGE = age at admission; COM = number of comorbidities; REV = revision surgery; ETHR = elective total hip replacement; ETKR = elective total knee replacement |
|
Table 4: Contingency table of the dichotomised walking distance at admission (WDT_dich) and discharge modality (DisMod). |
|
|
Discharge to “home”(DisMod = 1)
|
Discharge to “other setting”(DisMod = 0)
|
Total
|
| Walking distance at admission categorised as “good” (WDT_dich = 1) |
199 |
8 |
207 |
| Walking distance at admission categorised as “poor” (WDT_dich = 0) |
73 |
19 |
92 |
| Total |
272 |
27 |
299 |
Discussion
The aims of this retrospective study were to identify determinants influencing the inpatient rehabilitation length of stay (LoS) and discharge modality (DisMod) following THR or TKR surgery.
It was demonstrated that male patients tended to be discharged 1.5 days earlier from the rehabilitation facility and performed better overall in the motor performance tests at admission (WDT, TUG and FIM_St) than their female counterparts. Trauma and emergency THR surgery tended to be more frequent in females, whereas elective THR surgery tended to be more frequent in males. The frequency of patients that were discharged to home after inpatient rehabilitation was similar in both gender groups (about 90%).
Motor performance test scores were available from 146 (FIM_St) to 182 (WDT) female patients and from 98 (FIM_St) to 117 (WDT) male patients (see table 1). Due to the large number of missing values for FIM_St, this variable was used to control for possible discrepancies in the predictive characteristics among the patients who were able to participate and those who were not able to participate in the FIM_St test at admission. No group differences were found for the females, while only three of the twelve characteristics were found to be different for the males, suggesting that the missing values did not bias the current analyses.
The first-step linear regression model was based on all predictor variables, whereas the logistic regression model was solely based on the clinical parameters that were extracted from the patients’ medical files (i.e. no motor performance test scores were imputed in this model). The large number of participants guaranteed that the models were in agreement with the recommendations for good practice in regression analysis, in that less than 10% of the number of subjects might be predictors in the linear model while the number of predictors in the logistic equation should not be more than 10% of the cases [17].
Length of stay (LoS) and discharge modality (DisMod)
Female gender was previously shown to be an important confounder when modelling the LoS of inpatient rehabilitation following revision THR surgery [8]. In the current study, LoS was significantly correlated with gender and, therefore, modelling was stratified for female and male patients.
The motor performance tests at admission to the rehabilitation facility were found to be important predictors for LoS in both gender groups, suggesting that performing well on these tests was associated with a shorter LoS.
Females who required more time between surgery and admission to the rehabilitation facility as well as females who had emergency THR surgery were shown to be at risk for a longer LoS. Predictors for a longer LoS among male patients were a higher age at admission and whether they were suffering from multi-trauma or presented additional gait disorders.
The predictability of the model for LoS established in the present study was comparable with the results of Yeung et al. [8]. In their retrospective study on factors influencing inpatient rehabilitation LoS following revision THR surgery, data for 275 patients were included (mean LoS = 29.6 days). The researchers used linear regression models with forward including of the variables that were significant at the 10% level of probability of error. Their final model explained 28% of variance in inpatient LoS, including the following eight predictors: gender, revision surgery, motor FIM scores at admission, age, weight bearing restriction at admission, haemoglobin level at admission, complications and days after surgery at the time of admission. The mean LoS in the current study was 19.8 ± 7.6 days and the models explained 22% of the LoS variance in the female and 31% in the male groups. Moreover, similar predictor variables were included such as motor performance tests, complications (e.g. additional gait disorders, number of comorbidities) and the time between surgery and admission to the rehabilitation facility.
The most important predictor in the model by Yeung et al. [8] was the motor FIM score at admission (standardised beta = –0.31). Lower FIM scores indicated lower functional motor capacity and more dependence in basic functional activities. Hence, on average the patients with higher motor FIM scores had a shorter LoS. This finding is consistent with the important influence of the WDT, TUG and FIM_St (with standardised beta’s ranging from –0.20 to 0.18 in females and –0.22 to 0.14 and males respectively) in the current models for both gender groups. The observation that a good motor performance capacity at admission to the rehabilitation facility was associated with a reduced LoS might be of uppermost importance. Therefore, it could be argued that an intensive physiotherapy intervention prior to a THR or TKR surgery might lead to an increased post-operative motor performance condition and hence in a decreased LoS at the rehabilitation facility and in significant savings of different resources.
The functional benefit of a comprehensive 3-week inpatient rehabilitation programme was previously demonstrated using the Western Ontario and McMaster Universities Arthritis Index (WOMAC) for pain, stiffness and function [18, 19]. Further research should examine whether different intervention strategies in patients with low motor performance capacity at admission would shorten the LoS of inpatient rehabilitation following THR or TKR surgery.
Along with Yeung et al.’s LoS prediction model [8], the current study also included age as a predictor in the male LoS equation, suggesting that substantially slower bed flow and higher costs might be expected in rehabilitation facilities with a higher number of older males.
The logistic regression model showed that there were important non-motor performance test based predictors for DisMod. The number of co-morbidities and the presence of additional gait disorders were suggested to be risk factors for a discharge to a supported living setting. Patients following elective or revision THR/TKR surgery had on average a more positive prognosis to be discharged to home.
The calculation of the OR for the categorised walking distance test at admission (WDT_dich) indicated that patients who performed “good” on the test (>27 metres) had about 6.5 times higher odds to discharge to home as compared to those who scored “poor”.
About 10% of the patients that were admitted to the rehabilitation facility following THR/TKR surgery did not discharge to home. To be discharged to a supported living setting might be a drastic change in the way of living for these patients. Therefore, the possibility to predict the discharge modality based on the outcome of a motor performance test might be of high importance. The PPV for WDT_dich, predicting a discharge to home given the condition that the patient scored “good” on the test at admission was 96%. The NPV, predicting a discharge to a supported living setting given a “poor” test result at admission, was 21%. Such information could be important from a patient’s perspective. In the context of patient communication, a statement such as “from 100 patients who were able to walk more than 27 metres at admission, about 96 were likely to discharge to home after rehabilitation” could be motivating. The walking distance test accuracy (73%) and its area under the ROC curve (0.822) suggested good to very good discrimination power of this test.
Sensitivity and specificity represent specific test characteristics and might therefore be of minor interest for the clinical interpretation of the current results.
Costs-efficiency comparisons between rehabilitation programmes at nursing facilities, inpatient rehabilitation facilities and at home revealed higher costs for inpatient rehabilitation facilities but a shorter duration and better outcomes [4, 20–22]. The question, however, of whether decreasing LoS would lead to overall cost savings, remains unclear and is beyond the scope of this paper.
Furthermore, in the Swiss healthcare context, discharging home might not lead to savings of resources per se. The costs for professional nursing support at home might outweigh the cost savings of living at home. For instance, from the perspective of a Swiss health insurance company, it might be preferable to discharge an older THR/TKR patient with severe additional gait disorders and comorbidities to a supported living setting.
Strengths and limitations
The strengths of this paper are the inclusion of a large sample, validity-proven and easy-to-conduct motor performance tests as predictors, the standardisation of the setting (same rehabilitation facility and same (trained) observers) and the possible practical implications of the results. However, the following limitations have to be considered. By focusing on length of stay and discharge modality (important factors in the context of resource allocation), other potential outcomes such as functionality, pain or quality of life were not considered in this study. Although this study describes a sample with a rather homogenous condition (i.e. THR or TKR), the observed standard errors of the predictions point to uncertainty. This could be partially explained by the fact that LoS and DisMod seemed to be related to many patient and nonpatient factors. The retrospective nature of the study design was considered another limitation, making it impossible to include additional interesting variables in the analysis. For example, the impact of body-mass index, socioeconomic status or types of comorbidities such as osteoporosis and upper limb impairments was not controlled for. Other limitations include the facts that all measurements were conducted before the introduction of the DRGs in Switzerland and that several data were collected from only one inpatient rehabilitation facility. Although there were no geographical limitations for the patients admitted to the facility, the majority stemmed from the German-speaking part of Switzerland. These factors might limit the external validity of this study. However, although multiple factors might affect LoS and DisMod, the models presented explained between 20% and 31% of the dependent variables’ variances, reflecting the depth of the predictors included in the exploratory regression equations. These results add valuable information to the existing knowledge on designing prospective studies to investigate the determinants of LoS and DisMod in the future.
Conclusion
In conclusion, predictors influencing length of stay and discharge modality of inpatient rehabilitation following knee and hip replacement surgery were investigated. Using simplified models including five to six easy-to-gather and noninvasive variables, 22% (in females) and 31% (in males) of the variance of LoS and 20% (both females and males) of the variance of discharge modality could thereby be explained. Patients with good motor performance ability (i.e. high WDT and/or low TUG and/or high FIM_St scores) at admission to inpatient rehabilitation discharged earlier compared with patients with lower motor ability at admission. Similarly, based on the calculated OR, it can be concluded that “good” performers on the walking distance test at admission were more likely to be discharged home. These findings might be of interest for preoperative physiotherapeutic interventions and might help to improve the care planning and more accurately predict the access to inpatient beds as well as the allocation of resources.
Acknowledgment:The authors would like to thank Prof. Marcel Zwahlen, PhD from the Institute of Social and Preventive Medicine (ISPM) at the University of Bern in Switzerland for his statistical advice and Leila Sadeghi, PhD from the Section of Health at the Bern University of Applied Sciences for proof-reading and U. Steiger, MD, of the Berne Rehabilitation Centre (BRH) for providing the data.
References
1 OECD. Hip and knee replacement. Health at a Glance 2011: OECD Indicators: OECD Publishing; 2011.
2 Lübbeke A, Garavaglia G, Barea C, Hoffmeyer P. Why do we need hospital-based registries? The Geneva Hip Arthroplasty Registry Geneva: Division of Orthopaedics and Trauma Surgery, Geneva University Hospitals, Geneva, Switzerland; 2010.
3 Tian W, DeJong G, Brown M, Hsieh CH, Zamfirov ZP, Horn SD. Looking upstream: factors shaping the demand for postacute joint replacement rehabilitation. Arch Phys Med Rehabil. 2009;90(8):1260–8.
4 Tian W, DeJong G, Horn SD, Putman K, Hsieh CH, DaVanzo JE. Efficient rehabilitation care for joint replacement patients: skilled nursing facility or inpatient rehabilitation facility? Med Decis Making. 2012;32(1):176–87.
5 OECD. Average length of stay in hospitals. Health at a Glance 2011: OECD Indicators: OECD Publishing; 2011.
6 Theurl E, Winner H. The impact of hospital financing on the length of stay: evidence from Austria. Health Policy. 2007;82(3):375–89.
7 Capuano T, MacKenzie R, Pintar K, Halkins D, Nester B. Complex adaptive strategy to produce capacity-driven financial improvement. J Healthc Manag. 2009;54(5):307–18; discussion 318-309.
8 Yeung SM, Davis AM, Soric R. Factors influencing inpatient rehabilitation length of stay following revision hip replacements: a retrospective study. BMC Musculoskelet Disord. 2010;11:252.
9 Walker WC, Keyser-Marcus LA, Cifu DX, Chaudhri M. Inpatient interdisciplinary rehabilitation after total hip arthroplasty surgery: a comparison of revision and primary total hip arthroplasty. Arch Phys Med Rehabil. 2001;82(1):129–33.
10 Vincent KR, Vincent HK, Lee LW, Weng J, Alfano AP. Outcomes after inpatient rehabilitation of primary and revision total hip arthroplasty. Arch Phys Med Rehabil. 2006;87(8):1026–32.
11 Fisher DA, Trimble S, Clapp B, Dorsett K. Effect of a patient management system on outcomes of total hip and knee arthroplasty. Clin Orthop Relat Res. 1997(345):155–60.
12 Mahomed NN, Koo Seen Lin MJ, Levesque J, Lan S, Bogoch ER. Determinants and outcomes of inpatient versus home based rehabilitation following elective hip and knee replacement. J Rheumatol. 2000;27(7):1753–8.
13 Oldmeadow LB, McBurney H, Robertson VJ. Hospital stay and discharge outcomes after knee arthroplasty: implications for physiotherapy practice. Aust J Physiother. 2002;48(2):117–21.
14 Dauty M, Smitt X, Menu P, Dubois C. Which factors affect the duration of inpatient rehabilitation after total knee arthroplasty in the absence of complications? Ann Phys Rehabil Med. 2009;52(3):234–45.
15 Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
16 Ravaud JF, Delcey M, Yelnik A. Construct validity of the functional independence measure (FIM): questioning the unidimensionality of the scale and the “value” of FIM scores. Scand J Rehabil Med. 1999;31(1):31–41.
17 Kirkwood B, Sterne J. Essential Medical Statistics (Essentials). 2nd ed. Malden, MS, USA: Blackwell Science Inc.; 2003.
18 Tal-Akabi A, Steiger U. Long-Term Functional Effects of High Intensity Resistance Training of Nonoperated Limb in Elderly after Hip or Knee Surgery. physioscience. 2010;6:21–6.
19 Tal-Akabi A, Steiger U, Villiger PM. Neuromuscular adaptation to early post-operative, high-intensity, short resistance training of non-operated lower extremity in elderly patients: a randomized controlled trial. J Rehabil Med. 2007;39(9):724–9.
20 Herbold JA, Bonistall K, Walsh MB. Rehabilitation following total knee replacement, total hip replacement, and hip fracture: a case-controlled comparison. J Geriatr Phys Ther. 2011;34(4):155–60.
21 Munin MC, Putman K, Hsieh CH, et al. Analysis of rehabilitation activities within skilled nursing and inpatient rehabilitation facilities after hip replacement for acute hip fracture. Am J Phys Med Rehabil. 2010;89(7):530–40.
22 DeJong G, Tian W, Smout RJ, et al. Long-term outcomes of joint replacement rehabilitation patients discharged from skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90(8):1306–16.