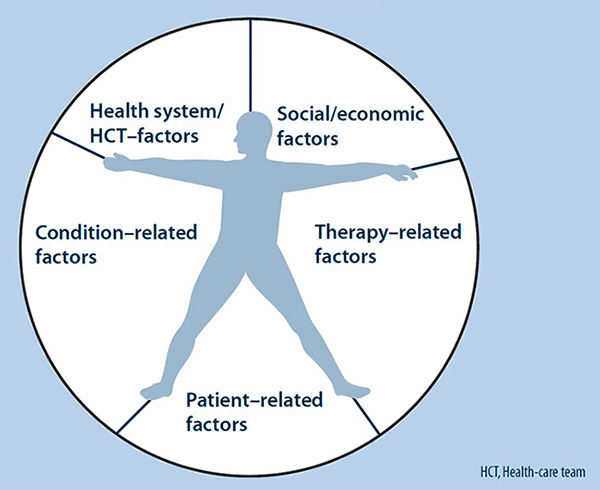
Figure 1
The five dimensions of adherence (reproduced with the permission of the WHO from Sabaté E (2003) [13]).
DOI: https://doi.org/10.4414/smw.2013.13827
Internet and communication technologies, such as personal computers, smartphones or tablets, have rapidly and drastically changed the ways by which human beings communicate with each other socially and professionally (e-mails, social media), as well as the flow of information (dissemination, quantity and quality of information). Past boundaries have all but disappeared, and time and geography matter increasingly less. All strata of life, including education and health, have been deeply affected. According to recent estimates, 63% of the population in Europe uses the Internet [1]. Evidence has shown that healthcare cannot continue being dissociated from the Internet. Hence, some journals, such as the Journal of Medical Internet Research, Telemedicine and eHealth and the International Journal of Telemedicine and Applications, have begun to address this topic.
Healthcare professionals know how much the Internet has positively changed their activities regarding, for example, knowledge (open access to medical journals, medical guidelines and online conferences) or professional networking (for continuing education and sharing professional experiences, crowdsourcing* for sharing and solving problems). (*Jeff Howe defined the neologism crowdsourcing in 2006 in Wired Magazine as “a process that involves outsourcing tasks to a distributed, undefined and large network of people in the form of an open call through the internet’ with the aim, for example, of generating knowledge”.) Healthcare professionals use what is relevant to their own activities, which implies that they are able to develop specific abilities to ensure the usefulness and quality of data while regulating its flow and storage (also called digital curation). In a similar fashion, the Internet is definitely changing patients’ attitudes toward health management.
The World Health Organization (WHO) defines eHealth as the transfer of health resources and health care by electronic means [2]. Cyberhealth is defined as the provision of care through the Internet [3]. More specifically, health 2.0 is the use of a specific set of Internet tools (such as blogs, podcasts and tagging searches) by healthcare providers and patients, who together use open sources to generate information, collaborate, promote health education and personalise healthcare [4]. Thanks to the Internet era, medical information is more readily available than it used to be. The Internet is powerful, but it can also be risky, as its information might be biased or even false. Healthcare professionals often complain about the poor quality of information patients get on the Internet related to their health state, disease or treatment options. Either the quality of information is poor, or the information does not make sense; thus, often patients have a hard time making an informed decision, especially when their health literacy is low [5]. At the same time, e-patients (also known as Internet patients) are increasingly active participants in their care and report increasingly accurate health information and a more autonomous – but not always improved – relationship with their healthcare providers [6].
Computer- and now Internet-tailored strategies have become common and efficient for altering certain health-risk behaviours, for example smoking [7]. However, thus far some results have been controversial and inconclusive, for example regarding changing dietary behaviours [8]. Based on this fact, the potential of Internet strategies must be considered for altering and supporting drug intake behaviour during long-term treatments, such as human immunodeficiency virus (HIV) infection, cancer, cardiovascular diseases, asthma or epilepsy. The present work tries to evaluate the possibility that cyberhealth, via the development of population-wide easy access to wireless personal computers, tablets and smartphones, can effectively influence the intake of medication and long-term medication adherence.
Worldwide, the interactions between patients and healthcare professionals have evolved during the last two decades towards a more balanced partnership. An increasing number of patients participate in their own medical decisions. Health literacy and patient empowerment support the patients’ abilities and competencies in engaging with this relationship. Supporting the self-management of medication intake implies person-centred interventions, and the Internet could represent a powerful technology for embracing this new orientation in care. However, the impact of providing such intervention through the Internet must be assessed to determine whether it is effective in improving autonomous and safe intake of medication.
As a fundamental prerequisite, it seems obvious that cyberhealth cannot replace the continuous interprofessional collaboration among patients, physicians, pharmacists, nurses and other healthcare providers. However, thanks to its attempts at a constructive human relationship, cyberhealth could become an interesting facilitator to meet patients’ needs during the time between visits with the healthcare providers. However, healthcare providers, as well as patients, must master new complex skills and specific competences, called eHealth Literacy 2.0, to integrate cyberhealth into their relationship and to benefit from its potential use [9, 10].
The intake of medication and specifically medication adherence are dynamic and complex human behaviours that are influenced by many factors (see fig. 1). Some factors relate to the healthcare system and how much it addresses and supports patient adherence. The prevalence and consequences of nonadherence affect the quality of care, and there is an urgent need to develop effective intervention programs to support the responsible and safe use of medication.
There is a popular phrase summing up nonadherence: "Drugs don’t work if patients don’t take them". In 2003, the WHO published a report recognising the poor adherence to chronic disease treatments as a worldwide problem of striking magnitude. Nevertheless, the evaluation of the prevalence of nonadherence is inherently susceptible to bias, as it relies on the quality of measurement as well as the chosen cut-offs (adherence vs nonadherence) [11, 12]. However, the WHO estimates that 50% of patients in developed as well as developing countries are nonadherent. The number of nonadherent patients is expected to grow over the coming years as the burden of chronic disease grows worldwide [13]. Blaschke mentioned that a mean of 60% of patients were still adherent 1 year after having started a chronic therapy [14]. As well, Briesacher reported that 72% of patients treated for hypertension, 68% for hypothyroidism, 65% for type 2 diabetes, 61% for seizure disorders, 55% for hypercholesterolaemia, 51% for osteoporosis and 37% for gout still took their medicine at the 1-year follow-up [15].
Recently, the ABC expert team* has reviewed the taxonomy defining adherence to medication. (*The ABC Project aimed to produce evidence-based recommendations for European policymakers to improve patient adherence and thereby promote more efficient use of medicines. The ABC team is a collaboration of experts from the Medical University of Lodz, Poland, Bangor University, UK, AARDEX Group, Switzerland,Keele University, UK andKatholieke Universiteit Leuven, Belgium.) They define it as “the process by which patients take their medications as prescribed, composed of initiation, implementation and discontinuation. Persistence is the length of time between initiation and the last dose, which immediately precedes discontinuation” [12]. Medication adherence has been recognised as a dynamic process that is influenced not only by the patient but also by significant others, prescribers, providers, community, institutions and healthcare policies [16]. Different determinants of medication adherence have been described. The WHO proposed a five-dimension classification system composed of socioeconomic factors, healthcare team- and system-related factors, condition-related factors, therapy-related factors and patient-related factors (fig. 1) [13]. A recent systematic review identified 771 individual determinants of patient nonadherence across all the dimensions of the classification. Patients’ attitudes and beliefs appear to be the factors most closely associated with nonadherence [12]. Osterberg outlines the major predictors of poor adherence as psychological problems, cognitive impairments, treatment of asymptomatic diseases, inadequate follow-up planning, treatment side effects, patient’s lack of belief in the benefit of treatment, patient’s lack of insight into the illness, poor provider-patient relationships, practical and economic barriers to care or medication, missed appointments and the complexity of treatment [17].
Adherence fades with time for different reasons (lack of priority, fear of long-term use, pill fatigue, lack of personal benefit, little feedback from the prescriber, etc.). The timing of the intake becomes more erratic, and dose omissions occur more frequently. However, adherence frequently improves just before or after a medical appointment [17]. The consequences of nonadherence vary from major to trivial, spanning its effects on pharmacodynamic and pharmacokinetic parameters, as well as its short- and long-term effects on the disease [18].
Increasing and sustaining individually regulated drug management and medication adherence over time are difficult tasks. The need for efficient interventions is increasing along with newly complex and costly long-term treatments and the increasing number of long-term and aging patients.
The following was one of the take-home messages of the 2003 report of the WHO: “the consequences of poor adherence to long-term therapies are poor health outcomes and increased health care costs” [13]. We can evaluate the potential impact of nonadherence knowing that fewer than 25% of hypertensive patients achieve optimum blood pressure [13] and that, as shown by Burnier et al., 50% of nonresponders were in fact nonadherent [19]. In the USA, more than 100 billion US-dollars a year are spent on hospitalisations due to poor adherence [20]. In diabetes, a 10% increase in medication possession ratio was associated with an 8.6% decrease of global annual healthcare costs [21, 22]. Similarly, in schizophrenia, a 10% increase in this ratio was associated with a 12.6% decrease of semiannual healthcare costs [23, 24]. Hopefully, these reported outcomes will motivate researchers and healthcare providers to request that governments and insurers support new, data-driven medication adherence programmes.
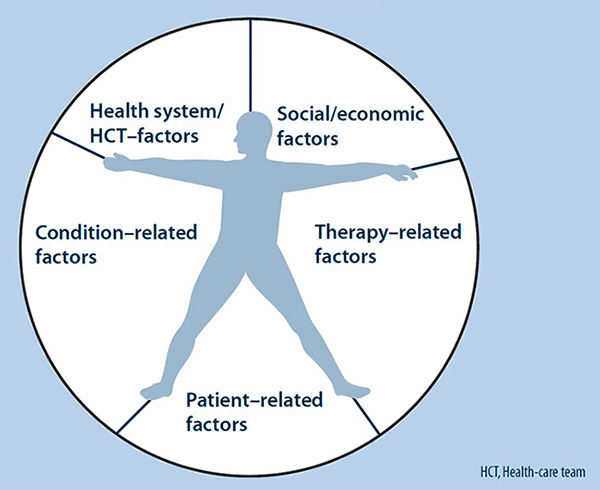
Figure 1
The five dimensions of adherence (reproduced with the permission of the WHO from Sabaté E (2003) [13]).
Nonadherence could lead to failed treatment, poor clinical outcomes, misdiagnosis, inappropriate dose escalation, emergence of drug resistance, rebounding or recurrent first-dose effects, increasing hospitalisation and practitioner visits, and a poorer quality of life. At a societal level, nonadherence may cause deleterious consequences for workforce productivity and the transmission of infectious diseases. These factors can bias the efficacy of clinical studies or adversely affect the results of the drug, ultimately influencing healthcare policy [17, 25–27]. The WHO and the Institute of Healthcare Informatics estimate that nonadherence contributes to 57% of the world’s total avoidable cost due to suboptimal medicine use [28].
Roebuck questioned why, given the widespread debate over healthcare costs, medication adherence in patients with chronic diseases does not feature more prominently in these discussions. He recognises that “research into medication compliance (adherence) suffers from methodological challenges that may call the validity of the results into question” [29].
In a recent systematic review on the cost-effectiveness of adherence-enhancing interventions, the ABC project team underlined the paucity of evidence and the need for more and better research. Their work is based on Elliott’s review in 2005 [30], updated by the UK National Institute for Health and Care Excellence (NICE) in 2009 [31]. They were not able to draw conclusions because of study heterogeneity [12].
To change a suboptimal adherence behaviour to more persistent and accurate drug intake behaviours, the patient must be involved in the decision-making process. To fully engage in such a process, patients also require both time and sound theory-based interventions to be conventionally transmitted by educated healthcare providers. However, web-based interventions could play an increasing role in changing patient behaviours by sustaining the healthcare provider’s messages, providing continuous monitoring and building collective intelligence.
During the last decade, the number of websites allowing patients to manage medical information has increased, for example a number of sites allow diabetic patients to upload sugar levels. Lately, more complex websites are emerging that allow patients to upload and/or share additional information such as personal and medical information.
Because of its novelty, the impact of cyberhealth on drug intake has not yet been well explored. However, early results have provided some evidence. Linn et al. published a systematic review on effects of cyberhealth interventions on medication adherence. Thirteen studies met the inclusion criteria. They found that 11 (85%) studies showed a moderate to significant impact from Internet interventions on adherence to treatment. Evidence came especially from three studies of good quality, the main results of which are as follows. Joseph et al. showed in a randomised clinical trial (RCT) that, compared with generic asthma websites, a web-based, 6-month tailored approach to changing negative asthma behaviours was effective and economical in improving asthma outcomes at 12 months in the hard-to-reach African-American teenage population. Notably, access to the Internet was provided through school computers [32]. DeVito et al. showed in a pilot RCT conducted in the USA that lung transplant patients using an electronic pocket device were, compared with standard care protocols, more engaged in self-care behaviours for the first 2 months after hospital discharge [33]. Unfortunately, long-term results are unavailable. Jan showed that a Taiwanese Internet-based asthma telemonitoring programme increased children’s and caregivers’ self-management skills at 12 weeks and decreased negative clinical outcomes compared with standard care protocols [34]. However, long-term results are also lacking. Obviously, more research is needed to confirm these early results.
The number of available Internet websites is increasing, including webEase in Epilepsia [35], Puff City in Asthma [36] and prochange behaviour systems, a generic website for long-term patients [37]. Such interactive websites provide several levels of intervention programmes on drug intake, including the following: (1) basic one-way drug information and education on drug use to increase patient knowledge; (2) encouragement to upload personal data and self-monitor one’s own drug intake and clinical data; and (3) tailored web-based interventions and individualised feedback, depending on the patient’s profile, health, beliefs, attitudes, barriers and needs, all of which are assessed online. Typically assessed dimensions include symptoms, control of disease, medication use (name of medication, dosage and frequency of use), knowledge, motivation, self-efficacy, self-regulatory strategies, goals, social support, mental health, frequency of medical visits, emergency visits and hospitalisations.
Moreover, importantly, recent literature on adherence has shown that interventions providing feedback to patients on their recent drug intake enhances patient adherence [38, 39]. Internet programmes could provide such individual feedback with suitable, personalised timing. However, the literature is not yet conclusive on the relation between the extent of customisation and the impact on medication behaviours [7, 40]. It also seems that frequency of using the interactive website is determinant [40].
Little is known about the profiles of patients who could benefit from such cyberhealth programmes. Intuitively, teenagers seem to be likely targets, as they are both frequent Internet users and difficult to retain in care. Indeed, many teenagers with chronic diseases are reluctant to visit their healthcare providers on a regular basis [41]. The Internet could also be useful for long-term patients living in remote, isolated areas or for frequent travellers. Unfortunately, we do not know yet whether online benefits apply mostly to new patients engaging in new treatments, experienced patients, or both. We also lack information on the relevant determinants of the level of health literacy and eHealth Literacy 2.0.
The methods used to measure adherence in studies that have evaluated the impact of cyberhealth on drug intake or drug management were often poor and relied mostly on patient self-reports. However, electronic pill containers are now available to monitor and support patient adherence [38]. Reading of such devices could be performed remotely instead of at a pharmacy visit. The frequency of these remote readings can be scheduled according to patient needs, and healthcare providers could intervene promptly in the case of a cluster of unusual drug omissions [42]. Patients and their caregivers could benefit from such a monitoring system, which could reinforce the alliance between the patient encountering major issues with drug intake and the healthcare system.
Preliminary results have also shown that the effects of these programmes decrease after their termination, which is consistent with most traditional interventions as well [7]. There is a need to develop tailored programmes that could be used iteratively over time according to a patient’s evolving needs. Such needs have to be identified and discussed with healthcare providers.
Such web-based and easily accessible programmes aim at promoting self-care management by involving patients in active care and hence by giving them new means to play a major role in managing their own health (e-patients). Web-based programmes could bridge a time-gap and give patients a chance of interaction during daily life, in parallel with chronic medication intake. They provide the unique opportunity to integrate health and social care by guiding patients in their own thinking, decisions and action plan, by identifying their individual needs, by giving up-to-date information and by empowering them to discuss openly their unsolved issues with their healthcare providers. Accessing information in an iterative way and combining diverse media (written information, audio and video) can also enhance the patient’s memorisation process. Patients could gain control over their disease, which should be beneficial to their quality of life.
Tailored messages and customised health programmes, in which patients can choose which the components they would like to use, are theoretically more adapted to patients’ needs. They have the potential for supporting patients in changing behaviours and attitudes towards an improved intake of medication in the long term with increased relevance and depth of support [7]. In fact, web-based programmes are less biased by the patient’s memory recall issues than standard care, provided relevant data are updated on a regular basis. They might also enhance the patient’s awareness of personal attitudes, and clarify misconceptions or misunderstandings.
Patients can upload in real time information on the way they deal with their treatment on daily basis (for example, date of clinical event, date and time of a missed dose and circumstances when the dose was missed), consult and get feedback as visual graphs of uploaded data, and explore changes over time on their own, or with their family or healthcare giver. Indeed, feedback generates sustained motivation and cements a positive drug intake habit [38, 39]. For example, on http://www.webease.org , epileptic patients can upload self-reported data on their medication-taking behaviour over the last 3 days, including how many prescribed doses were missed. Patients may then generate graphs connecting, for example, medication adherence to seizures. Insights gained by such visualisations may motivate patients to be more adherent.
Furthermore, when linked to empathic follow-ups with healthcare providers, such programmes are likely to promote the emergence of novel, patient-friendly solutions. For example, a patient could benefit from filling out a self-efficacy scale when experiencing the first symptoms of pill fatigue; when detecting pill fatigue, the programme should engage the patient in scheduling a new appointment with his or her healthcare provider, who could be the patient’s physician or pharmacist. The same could happen when side-effects emerge or worsen (using an online pain analogue scale); the programme should recommend that the patient contacts his or her physician.
Hence, the purpose of such Internet programmes is not to take over the role of healthcare givers. On the contrary, they should reinforce provider’s messages, maintain access to tailored information during the time between medical visits and encourage patients to disclose their treatment issues to healthcare providers. The alliance between the patient and the healthcare providers has to benefit from it [43, 44]. Quality of communication and assessment of the patient’s needs might be enhanced through the right integration of cyberhealth into clinical practice. If cyberhealth adequately addresses e-patients’ needs, it could drive improved continuity of care.
In sum, to get full benefit out of such personal self-administered health records, data should be shared with healthcare providers. Patients and healthcare providers must agree on: (1) the material they would like to exchange and discuss, and (2) the frequency and means by which this exchange can be made most effectively. For example, the provider has to intervene when data have worsened [45]. In such a case, an alarm should encourage the patient to visit healthcare providers soon.
| Table 1: Examples of potential benefits and risks of cyberhealth in supporting the intake of medication. | |
| Potential benefits | Potential risks |
| Empowerment of patients by giving them new means to play a major role in managing their own health Enhanced assessment of patient’s needs in real time Sustained healthcare provider’s messages, provision of continuous monitoring and bridging of the time-gap between scheduled visits with providers Promotion of the “e-patient” concept: enhancement of a 24-hours-a-day, multidirectional flow of information (patient-healthcare providers-online communities) Decrease in the patient’s feeling of isolation Capacity to reach patients who are difficult to retain in care (e.g. teenagers, or socially or geographically isolated patients) Provision of tailored interventions and individualised feedback to sustain patient’s motivation (person-centred care) Provision of up-to-date information; increase in patient knowledge on responsible use of medicines Capacity to trigger adapted alarm messages in case situation worsens and facilitated relationship with healthcare providers | Poor control of quality of websites content (evidence- and theory-based, independency) Lack of customisation of websites (lack of adaptation to age, culture, language, computer skills, health literacy, etc.) Keeping patients away from healthcare providers Lack of uptake and insufficient frequency of use by patients in daily life Lack of patients and healthcare providers’ readiness and e-Health literacy 2.0 Fostering inequalities in healthcare (digital divide) Confidentiality and patient data use issues Cost and reimbursement issues |
Importantly, the potential benefits of Cyberhealth must be balanced against its risks (table 1). Although interactive tools and collaborative software permit a new orientation to clinical care, there is no one solution that fits everyone; thus, such programmes should apply to patients willing and with the skills to use them. These programmes should be adapted to the age, culture, language (most of them are available in English only), needs and social levels of the targeted populations, and they should be kept up-to-date. Their content must be theory-based and independent and should reflect evidence-based practices. Functionality and usability are as important as content and must be just as well-tested [43]. Monitoring the attrition rate should show whether patients persist in using cyberhealth, which is an important quality measure of the programme. If patients lack interest in a cyberhealth programme, they will not benefit from it; thus, the healthcare provider must adapt care accordingly.
We cannot dismiss the risk that cyberhealth could keep patients away from healthcare providers, increasing their distance and decreasing their quality of care. With this in mind, healthcare providers could better adjust care to patients’ needs by using the feedback provided by cyberhealth to discuss empathically relevant determinants of medication intake during in-person appointments. We should also keep in mind that this system may create a risk of fostering inequalities in healthcare between those who can access the Internet and those who cannot, through lack of skill with or availability of technology (risk of a digital divide). Thus, adjustment to the needs of a patient or a population is important (for example, using school computers for teenagers).
We also need more data on the cost-effectiveness and applicability to standard care of such cyberhealth programmes to create financial models and determine whether public health funding should support such developments. Additionally, ethical considerations should pave the way for successful implementations. One must also think of a competent authority to control the scientific quality of the content of such programmes and their user-friendliness (Health On the Net Foundation [HON] and others). Finally, health authorities must also devise methods through which healthcare providers will be reimbursed for integrating these tools into their practice [3].
Cyberhealth programmes must be confidential and secure, especially when patients upload personal data on their drug intake. Healthcare authorities must take responsibility for insuring the appropriate storage of personal data, according to national laws and local institutional requirements [45]. They must also regulate the scientific and commercial properties of uploaded data, as the richness of such available data represents a substantial new opportunity for research.
Well-designed studies will be needed to assess the effectiveness of these comprehensive websites when integrated into practice by both patients and their healthcare providers. Furthermore, identifying the factors likely to drive the acceptance and adoption of these sites by both patients and healthcare providers will be key to their success.
Cyberhealth is already undoubtedly modifying healthcare and long-term patient follow-up. Although cyberhealth seems to represent a promising method of supporting patient drug intake, we need more evidence to determine its (cost-) effectiveness and feasibility. Ultimately, we must determine the impact of cyberhealth tools on long-term adherence and health outcomes. Further research is required to evaluate strategies for the integration of cyberhealth programmes into clinical practice in order to avoid major pitfalls. This represents a huge shift that can be difficult to manage for healthcare systems; however, the potential opportunities are inescapable. One benefit is to move with patients into the Internet world instead of stranding patients in a web of misinformation on their own. Entering this generation of digital humanity, healthcare cannot stay on the side any longer [46]. Therefore, we urgently need high-quality research that promotes the safe use of cyberhealth to foster safe, efficient and economical drug intake. Aside from drug intake, cyberhealth comprehensive care management programmes should monitor simultaneously a series of health behaviours, such as smoking, alcohol consumption, weight loss and physical exercise. In this sense, cyberhealth might facilitate better integrated care in the future.
Last but not least, crowd-sourced cohorts on drug intake represent a new reservoir of research data alongside institutional research. These cohorts have the potential to complement traditional research and generate new data on patients’ habits and needs regarding drugs [45].
Acknowledgment:The authors would like to thank Matthias Reymermier and Sebastian Amico, pharmacists, for their help in managing the references and reading the manuscript as well as Dr John Wagg for his useful comments.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.
1 European Internet Statistics. 2012 updated June 30, 2012 [cited 21.11.2012]; Available from: http://www.internetworldstats.com/
2 World Health organisation. E-Health. Glossary of globalization, trade and health terms Web [Internet]. Geneva: Department of Ethics, Equity, Trade and Human Rights ; 2012 [updated 2012; cited 2012 Nov 21]. Available from: http://www.who.int/trade/glossary/story021/en/index.html
3 Stroetmann KA, Kubitschke L, Robinson S, Stroetmann V, Cullen K, McDaid D. How can telehealth help in the provision of integrated care? Copenhagen: WHO Regional Office for Europe 2010:1–39.
4 Council for public health and health care. Health 2.0: It’s up to you. The Hague; 2010.
5 Allam A, Schulz PJ, Nakamoto K.: Between bad literacy and guided navigation. paper presented at: 5th World Congress on Social media, Mobile Apps and, and Internet/Web2.0.; 2012 Sept 9; Boston (USA)
6 Participatorymedicine.org [Internet]. Newburyport (USA): Society for Participatory Medicine; c2009–2012 [cited 2012 Nov 28]; Available from: http://participatorymedicine.org
7 Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51(3-4):214–21.
8 Harris J, Felix L, Miners A, Murray E, Michie S, Ferguson E, et al. Adaptive e-learning to improve dietary behaviour: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2011;15(37):1–160.
9 Norman C. eHealth literacy 2.0: problems and opportunities with an evolving concept. J Med Internet Res. 2011;13(4):e125.
10 Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res. 2006;8(2):e9.
11 Buscher A, Hartman C, Kallen MA, Giordano TP. Validity of self-report measures in assessing antiretroviral adherence of newly diagnosed, HAART-naive, HIV patients. HIV clinical trials. 2011;12(5):244–54.
12 Team AP. Ascertaining Barriers for Compliance:policies for safe, effective and cost-effective use of medicines in Europe, Final Report of the ABC Project (Deliverable 7.1): ABC Project; 2012 juin 2012.
13 Sabaté E, World Health O. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization 2003.
14 Blaschke TF, Osterberg L, Vrijens B, Urquhart J. Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol. 2012;52:275–301.
15 Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy. 2008;28(4):437–43.
16 Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705.
17 Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
18 Osterberg LG, Urquhart J, Blaschke TF. Understanding forgiveness: minding and mining the gaps between pharmacokinetics and therapeutics. Clin Pharmacol Ther. 2010;88(4):457–9.
19 Burnier M, Schneider MP, Chiolero A, Stubi CL, Brunner HR. Electronic compliance monitoring in resistant hypertension: the basis for rational therapeutic decisions. J Hypertens. 2001;19(2):335–41.
20 Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
21 Balkrishnan R, Rajagopalan R, Camacho FT, Huston SA, Murray FT, Anderson RT. Predictors of medication adherence and associated health care costs in an older population with type 2 diabetes mellitus: a longitudinal cohort study. Clin Ther. 2003;25(11):2958–71.
22 Salas M, Hughes D, Zuluaga A, Vardeva K, Lebmeier M. Costs of medication nonadherence in patients with diabetes mellitus: a systematic review and critical analysis of the literature. Value Health. 2009;12(6):915–22.
23 Dilla T, Ciudad A, Alvarez M. Systematic review of the economic aspects of nonadherence to antipsychotic medication in patients with schizophrenia. Patient Prefer Adherence. 2013;7:275–84.
24 Peng X, Ascher-Svanum H, Faries D, Conley RR, Schuh KJ. Decline in hospitalization risk and health care cost after initiation of depot antipsychotics in the treatment of schizophrenia. ClinicoEconomics and outcomes research: CEOR. 2011;3:9–14.
25 Urquhart J. Pharmacoeconomic consequences of variable patient compliance with prescribed drug regimens. Pharmacoeconomics. 1999;15(3):217–28.
26 Bosworth HB, Granger BB, Mendys P, Brindis R, Burkholder R, Czajkowski SM, et al. Medication adherence: a call for action. Am Heart J. 2011;162(3):412–24.
27 Cutler DM, Everett W. Thinking outside the pillbox – medication adherence as a priority for health care reform. N Engl J Med. 2010;362(17):1553–5.
28 IMS Institute for Healthcare Informatics. Advancing the responsible Use of Medecines: Applying levers for change. 2012.
29 Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff (Millwood). 2011;30(1):91–9.
30 Elliott RA, Barber N, Horne R. Cost-effectiveness of adherence-enhancing interventions: a quality assessment of the evidence. Ann Pharmacother. 2005;39(3):508–15.
31 Urquhart J. Some economic consequences of noncompliance. Curr Hypertens Rep. 2001;3(6):473–80.
32 Joseph CL, Peterson E, Havstad S, Johnson CC, Hoerauf S, Stringer S, et al. A web-based, tailored asthma management program for urban African-American high school students. American journal of respiratory and critical care medicine. 2007;175(9):888–95.
33 DeVito Dabbs A, Dew MA, Myers B, Begey A, Hawkins R, Ren D, et al. Evaluation of a hand-held, computer-based intervention to promote early self-care behaviors after lung transplant. Clinical transplantation. 2009;23(4):537–45.
34 Jan RL, Wang JY, Huang MC, Tseng SM, Su HJ, Liu LF. An internet-based interactive telemonitoring system for improving childhood asthma outcomes in Taiwan. Telemedicine journal and e-health: the official journal of the American Telemedicine Association. 2007;13(3):257–68.
35 Epilepsy Foundation of America. [Internet]. Landover (USA): Epilepsy Foundation of America; 1999–2012 [cited 2012 Nov]; Available from: http://www.epilepsyfoundation.org/
36 Puffcity.org. Puff city Asthma management programm [Internet]. the Michigan Public Health Institute [cited November 2012]; Available from: https://puffcity.org
37 Pro-Change Behavior Systems [Internet]. Kingstown: Pro-Change Behavior Systems; c2010–2012 [cited November 2012]; Available from: http://www.prochange.com/
38 Krummenacher I, Cavassini M, Bugnon O, Schneider MP. An interdisciplinary HIV-adherence program combining motivational interviewing and electronic antiretroviral drug monitoring. AIDS Care. 2011;23(5):550–61.
39 De Bruin M, Hospers HJ, van den Borne HW, Kok G, Prins JM. Theory- and evidence-based intervention to improve adherence to antiretroviral therapy among HIV-infected patients in the Netherlands: a pilot study. AIDS PatientCare STDS. 2005;19(6):384–94.
40 Linn AJ, Vervloet M, van Dijk L, Smit EG, Van Weert JC. Effects of eHealth interventions on medication adherence: a systematic review of the literature. J Med Internet Res. 2011;13(4):e103.
41 Fredericks EM, Dore-Stites D. Adherence to immunosuppressants: how can it be improved in adolescent organ transplant recipients? Current opinion in organ transplantation. 2010;15(5):614–20.
42 Schneider M-P, Despland P-A, Buclin T, Burnier M. Evaluation of online telemonitoring of drug adherence: a pilot randomised, controlled study in patients with epilepsy. The Journal on Information Technology in Healthcare. 2003;1(6):419–35.
43 Fleisher L, Buzaglo J, Collins M, Millard J, Miller SM, Egleston BL, et al. Using health communication best practices to develop a web-based provider-patient communication aid: the CONNECT study. Patient Educ Couns. 2008;71(3):378–87.
44 Christensen H, Griffiths KM, Farrer L. Adherence in internet interventions for anxiety and depression. J Med Internet Res. 2009;11(2):e13.
45 Swan M. Health 2050: The Realization of Personalized Medicine through Crowdsourcing, the Quantified Self, and the Participatory Biocitizen. J Pers Med. 2012;2(3):93–118.
46 Svensson P. Envisioning the Digital Humanities. Digital humanities quarterly Alliance of Digital Humanities Organizations 2012.