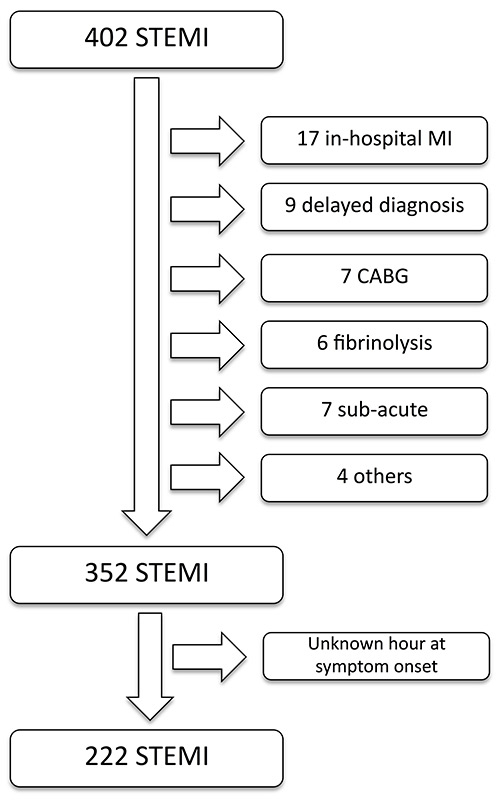
Figure 1
Study flow chart.
DOI: https://doi.org/10.4414/smw.2013.13817
Primary percutaneous coronary intervention (pPCI) for ST-elevation myocardial infarction (STEMI) is considered a life-saving procedure with a class 1A recommendation according to international scientific guidelines [1]. Moreover, it is well-known that in the management of STEMI, time from symptom onset to reperfusion therapy strongly affects the prognosis [2–5].
Large international clinical trials from the last decade demonstrate that although door-to-needle times have decreased [6], the time between symptom onset and first medical contact has hardly changed. The Swiss AMIS (Acute Myocardial Infarction in Switzerland) registry of acute coronary syndrome (ACS) has collected data since 1977 from 106 hospitals treating ACS. At the end of the year 2010, the registry contained 33,040 patients’ data. During the last decade, the door-to-balloon time for patients with STEMI in Switzerland decreased by 59.32% (from a median of 118 minutes in 1999 to 48 minutes in 2009), but the time between symptom onset and admission was only reduced by 15.77% (from a median of 260 minutes in 1999 to 219 minutes in 2009) [7].
A recent Swiss study showed that campaigns to raise patients’ awareness are an efficient way to reduce the prehospital delay [7]. In fact, a nation-wide public campaign was followed by a reduction of 10% in the prehospital delay amongst patients with STEMI.
In this study we sought to identify the impact of socioeconomic factors on time delays, STEMI management and outcome in a well-defined region of the French part of Switzerland.
Between 01 January 2009 and 30 June 2010, 402 consecutive patients underwent pPCI for STEMI in a large tertiary hospital in the French part of Switzerland. This hospital is the only site in charge of pPCI in the canton of Vaud, which has approximately 700,000 inhabitants. Patients with “symptom-to-first-medical-contact” time longer than 12 hours, patients previously treated with fibrinolysis or patients directly referred for coronary artery bypass graft (CABG) were excluded (50 patients). Amongst the remaining patients, symptom-to-first-medical-contact time was known for 222 (fig. 1). Laboratory, clinical, haemodynamic and demographic data were retrospectively collected from detailed hospital and catheter laboratory databases.
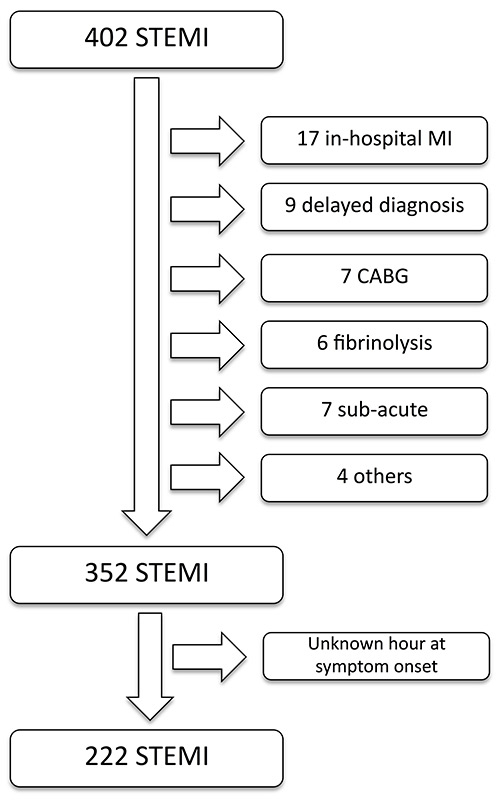
Figure 1
Study flow chart.
STEMI was defined in accordance with the European Society of Cardiology definition [1].
Symptom-to-first-medical-contact time was defined as the time between symptom onset, as reported by the patient, and the first contact with a medical doctor.
Different socioeconomic factors that might affect symptom-to-first-medical-contact time were identified and investigated: “level of education” [8, 11], “origin” [9–12] and “marital status” [11, 13]. The impact of these factors on STEMI management and outcome was analysed.
Level of education. Patients were sent a written questionnaire in order to report their level of schooling. If needed, patients and/or their general practitioners were contacted by telephone for additional information. The Swiss official education grading system was then used to classify patients into two educational levels: high education level (HEL) and low education level (LEL) in accordance with the official website of the “Swiss centre for professional education services, career counselling, academic and career”.
HEL-LEL. Patients who achieved a university entrance qualification or an equivalent education level were considered to be patients with a high education level. For patients from a non-Swiss education system, we compared the number of study years and the ability to go to university with their education level, to make it comparable with the Swiss grading system.
Origin and marital status. These variables where derived from the administrative records at admission. In terms of origin, patients were classified as Swiss or non-Swiss citizens depending on their nationality. For the variable marital status, we classified the patients into two groups: “married” or “not married” (single, divorced or widowed).
One-year mortality was defined as the cumulative all-cause mortality, including in-hospital mortality.
Door-to-needle time was defined as the time between hospital admission and start of the angiographic procedure.
The GraphPad Prism software 5.0d version was used to perform statistical analysis. Normally distributed data are presented as mean ± standard deviation (SD) and non-normally distributed data as median with interquartile range (P25; P75).
Discrete variables are presented as frequencies and percentages. Group differences were tested using an unpaired t-test for continuous variables with a normal distribution and nonparametric tests such as the Mann-Whitney U test was used for continuous variables with a non-Gaussian distribution.
This study complied with the Declaration of Helsinki regarding investigations in humans and was approved by the Institutional Ethics Committee. The authors had full access to the data and are solely responsible for the design and conduct of this study, all study analyses and drafting and editing of the paper.
The characteristics of the 222 patients enrolled in this study are summarised in table 1. The median age was 68.6 years. Median symptom-to-first-medical-contact time was 109 minutes and median door-to-needle time was 55 minutes. A total of 72.1% of patients were male, 49.7% had a high education level, 36.9% were not married and 67.7% were Swiss citizens.
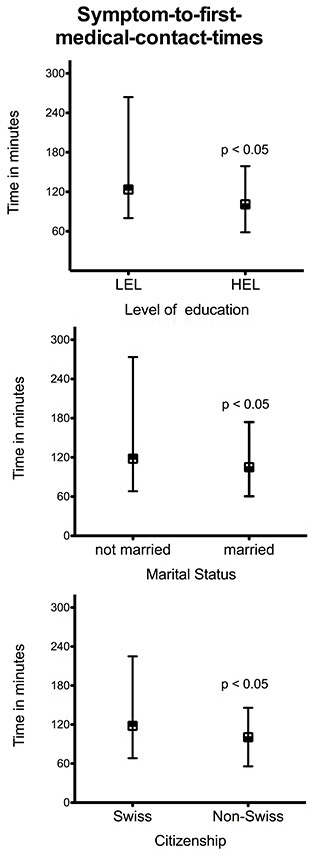
Figure 2
Median symptom-to-first-medical-contact times with interquartile ranges for the different socioeconomic groups. Patients with a low level of education, unmarried patients and Swiss citizens had significantly longer symptom-to-first-medical-contact times (p <0.05).
The symptom-to-first-medical-contact times were calculated for each of the sub-groups (fig. 2). A statistically significant difference was found in the median symptom-to-first-medical-contact time for the factors “level of education”, “origin” and “marital status”. People with a high level of education had a median symptom-to-first-medical-contact time of 101.0 (58.5; 159.0) minutes compared with 123.5 (80.0; 264.0) minutes for people with a low level of education (p <0.05). Non-Swiss citizens had a median symptom-to-first-medical-contact time of 100.5 (55.8; 145.8) minutes compared with 118.0 (68.3; 225.0) minutes for Swiss citizens (p <0.05). Married people had a median symptom-to-first-medical-contact time of 105.0 (60.5; 174.0) minutes compared with 118.0 (68.25; 273.5) minutes for unmarried people (p <0.05). In contrast, gender did not influence symptom-to-first-medical-contact time (median120.0 min for men vs 100.5 min for women; p = 0.35). Linear regression was then performed in order to study the relationship between age and symptom-to-first-medical-contact time. Here again, no association was found with a goodness of fit (R-square) <0.001. To avoid any selection bias, the proportion of every socioeconomic factor in patients with unknown symptom-to-first-medical-contact time (n = 130) was calculated. No statistically significant difference was found.
Clinical outcome and follow-up are summarised in table 2. Mean peak creatine kinase level was 2511 ± 2506 U/l and mean left ventricular ejection fraction (LVEF) assessed by means of echocardiography at discharge was 48.5% ± 11.4%. Clinical follow-up data were obtained for 86% of the patients. At 1-year follow-up, the all-cause mortality rate was 3.7%.
Management characteristics are summarised in table 3. For the socioeconomic factors studied, no statistically significant difference was found in terms of door-to-needle time, procedure time, number of stents, stent length or stent diameter. Clinical outcomes are summarised in table 4. No statistically significant difference was found in terms of mortality at one year, mean peak creatine kinase level or mean LVEF at discharge.
| Table 1: Baseline demographic characteristics (n = 222). | |
| General and socioeconomic factors | |
| Male gender (%) | 72.10% |
| Age (mean ± SD) | 68.6 ± 12.9 |
| High level of education (%) | 49.70% |
| Not married (%) | 36.90% |
| Swiss citizen (%) | 67.70% |
| Cardiovascular risk factors (%) | |
| Dyslipidaemia | 54.5% |
| Diabetes | 22.9% |
| Hypertension | 53.6% |
| Family history | 12.2% |
| Obesity | 23.4% |
| Smoking | 52.3% |
| Delays | |
| Symptom-to-first-medical-contact time; median (P25; P75) | 108.5 (65.8; 191.3) |
| Door-to-needle time; median (P25; P75) | 54.5 (38.3; 76.0) |
| Previous cardiovascular history (%) | |
| Prior percutaneous coronary intervention | 12.2% |
| Prior myocardial infarction | 7.2% |
| P25; P75 = interquartile range; SD = standard deviation | |
| Table 2: Myocardial infarction and percutaneous intervention characteristics, and outcomes (n = 222). | |
| Myocardial infarction characteristics | |
| Inferior (%) | 49.3% |
| Anterior (%) | 47.8% |
| Lateral (%) | 2.9% |
| Peak creatine kinase concentration (U/l) mean ± SD | 2511 ± 2506 |
| Percutaneous coronary intervention characteristics | |
| Procedure time (min) mean ± SD | 68.8 ± 109.4 |
| Stent length (mm) mean ± SD | 25.2 ± 11.5 |
| Stent diameter (mm) mean ± SD | 3.4 ± 0.6 |
| Number of stents (mean ± SD) | 1.2 ± 0.4 |
| Outcome | |
| Left ventricular ejection fraction (%) mean ± SD | 48.5 ± 11.4 |
| Mortality at 1 year (%) | 3.7 |
| SD = standard deviation | |
| Table 3: Management characteristics and socioeconomic factors (n = 222). | |||
| Level of education: | Low level of education | High level of educational | p-value |
| Door-to-needle time (min) median (P25; P75) | 50 (35; 77) | 54 (37; 72.5) | 0.45 |
| Procedure time (min) mean ± SD | 61 ± 22.9 | 62.8 ± 26.1 | 0.88 |
| Number of stents (mean ± SD) | 1.2 ± 0.4 | 1.2 ± 0.4 | 0.58 |
| Stent length (mm) mean ± SD | 24.9 ± 12.1 | 26.6 ± 12.2 | 0.30 |
| Stent diameter (mm) mean ± SD | 3.3 ± 0.6 | 3.3 + 0.6 | 0.85 |
| Citizenship: | Swiss | Non-Swiss | p-value |
| Door-to-needle time (min) median (P25; P75) | 54 (35; 75) | 51 (35.8; 72.3) | 0.71 |
| Procedure time (min) mean ± SD | 68.3 ± 68.2 | 58.8 ± 36 | 0.41 |
| Number of stents (mean ± SD) | 1.2 ± 0.4 | 1.2 ± 0.5 | 0.37 |
| Stent length (mm) mean ± SD | 25.5 ± 11.5 | 26.3 ± 13.8 | 0.91 |
| Stent diameter (mm) mean ± SD | 3.3 ± 0.6 | 3.3 ± 0.6 | 0.95 |
| Marital status: | Married | Not married | p-value |
| Door-to-needle time (min) median (P25; P75) | 51 (36; 71.75) | 54 (35; 82) | 0.48 |
| Procedure time (min) mean ± SD | 62.4 ± 56.1 | 71.3 ± 67.8 | 0.35 |
| Number of stents (mean ± SD) | 1.2 ± 0.4 | 1.2 ± 0.4 | 0.79 |
| Stent length (mm); mean ± SD | 26.3 ± 12.9 | 24.6 ± 11.0 | 0.52 |
| Stent diameter (mm) mean ± SD) | 3.3 ± 0.6 | 3.3 ± 0.6 | 0.38 |
| P25; P75 = interquartile range; SD = standard deviation | |||
| Table 4: Outcome characteristics and scioecenomic factors (n = 222). | |||
| Level of education: | Low level of education | High level of educational | p-value |
| Creatine kinase concentration (U/l) mean ± SD | 2777 ± 3032 | 2177 ± 1910 | 0.28 |
| Left ventricular ejection fraction (%) mean ± SD | 47.5 ± 11.8 | 50.6 ± 9.6 | 0.24 |
| Mortality at 1 year; n (%) | 4 (3.1%) | 2 (1.8%) | 0.55 |
| Citizenship: | Swiss | Non-Swiss | p-value |
| Creatine kinase concentration (U/l) mean ± SD | 2399 ± 2313 | 3068 ± 3306 | 0.25 |
| Left ventricular ejection fraction (%) mean ± SD | 47.9 ± 11.1 | 49.76 ± 11.4 | 0.31 |
| Mortality at 1 year; n (%) | 6 (3.4%) | 2 (2.7%) | 0.76 |
| Marital status: | Married | Not married | p-value |
| Creatine kinase concentration (U/l) mean ± SD | 2598 ± 2721 | 2617 ± 2572 | 0.78 |
| Left ventricular ejection fraction (%) mean ± SD | 48.6 ± 11.5 | 48.5 ± 10.8 | 0.87 |
| Mortality at 1 year; n (%) | 6 (3.7%) | 2 (2.35%) | 0.57 |
This study was conducted in 402 consecutive patients with STEMI undergoing pPCI in accordance with guidelines from The Task Force on Myocardial Revascularisation of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) [1] in a well-defined region of the French part of Switzerland. A significant impact of different socioeconomic factors on symptom-to-first-medical-contact times was observed. People with a higher educational level, non-Swiss citizens and married people had significantly shorter symptom-to-first-medical-contact times, with median differences of 23 minutes, 18 minutes and 13 minutes, respectively. This delay could be expected to result in adverse outcomes for this group of patients, but we did not observe this in our group of patients, with no difference in mortality at 1 year.
A number of studies have analysed the impact of socioeconomic factors on the pPCI treatment of patients with STEMI [7–16]. Contrary to previous publications, where the level of education was analysed qualitatively only [15], our study also shows the existence of a quantitative difference: people with a high level of education had significantly shorter symptom-to-first-medical-contact times. Furthermore, in contrast to several observations in the USA population, where differences between residents and nonresidents were investigated, the present paper shows that Swiss citizens had significantly longer symptom-to-first-medical-contact times than non-Swiss citizens [9, 15, 17]. Finally, this study confirmed that married people have significantly shorter symptom-to-first-medical-contact times.
Various publications have demonstrated the existence of a strong correlation between the patients’ subjective feeling of symptom severity and delay in seeking medical treatment [14]. We hypothesise that a high level of education may allow better awareness of symptoms and better knowledge of myocardial infarction, and therefore reduces symptom-to-first-medical-contact time, thus explaining our results.
Switzerland is a multicultural country with approximately 20% of the population being foreign inhabitants. It is surprising that Swiss citizens, who are supposed to be well acquainted with their health system, have a higher symptom-to-first-medical-contact time than non-Swiss citizens. However, in the study population area, multinational and start-up companies predominate and the proportion of people with a high education level was not statistically different between Swiss citizens and non-Swiss citizens; therefore, it may be assumed that the health awareness of these employees is high. On the other hand, different studies in Western countries have shown a higher rate of emergency room visits for vulnerable socioeconomic groups [16], such as migrants. The observations in Europe contrast with findings in the USA, where racial and ethnic disparities exist that put parts of the black and Hispanic populations at risk.
In our study, married people had shorter symptom-to-first-medical-contact time than unmarried. This difference has previously been reported and was found in miscellaneous studies such as the REACT trial [18]. Most logically it is due to the presence of the husband/wife accelerating the decision to call an ambulance or to go to the hospital.
The absence of difference in management characteristics is not surprising in the setting of a large tertiary referral centre with an organised STEMI programme. The overall mortality at 1-year follow-up was only 3.7% (including in-hospital mortality due to life-threatening arrhythmias occurring after revascularisation [19]) and therefore no impact of these socioeconomic factors on late clinical outcome was found.
The number of patients included in this study is relatively small; however, the hospital where this study was performed is the only centre for pPCI after STEMI in this well-defined region of the French part of Switzerland, with excellent data quality. Although our findings are likely to be applicable to other western countries, different ethnic mixes, socioeconomic settings and healthcare systems produce different sources of treatment differences. It would have been interesting to have the information “living alone” versus “living with someone” instead of married versus not married, which would have been more accurate. Furthermore, it would have been interesting to know patient’s exact locality at symptom onset, to allow us to rule out any bias due to geographical position and to distance from the hospital.
This retrospective study shows that symptom-to-first-medical-contact time amongst STEMI patients undergoing pPCI relates significantly to various socioeconomic factors including level of education, origin and marital status. In particular, unmarried Swiss citizens with a low level of education seem to be particularly vulnerable, and tertiary prevention campaigns should focus on this group of patients.
1 Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31(20):2501–55.
2 Gibson CM. Time is myocardium and time is outcomes. Circulation. 2001;104(22):2632–4.
3 Gibson CM, de Lemos JA, Antman EM. Time is muscle in primary PCI: the strength of the evidence grows. Eur Heart J. 2004;25(12):1001–2.
4 De Luca G, van ’t Hof AWJ, de Boer M-J, et al. Time-to-treatment significantly affects the extent of ST-segment resolution and myocardial blush in patients with acute myocardial infarction treated by primary angioplasty. Eur Heart J. 2004;25(12):1009–13.
5 Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941–7.
6 Schiele F, Hochadel M, Tubaro M, et al. Reperfusion stategy in Europe: temporal trends in performance measures for reperfusion therapy in ST-elevation myocardial infarction. Eur Heart J. 2010;31(21):2614–24.
7 Naegeli B, Radovanovic D, Rickli H, et al. Impact of a nationwide public campaign on delays and outcome in Swiss patients with acute coronary syndrome. Eur J Cardiovasc Prev Rehabil. 2011;18(2):297–304.
8 Berton G, Cordiano R, Palmieri R, et al. Clinical features associated with pre-hospital time delay in acute myocardial infarction. Ital Heart J. 2001;2(10):766–71.
9 Cohen MG, Fonarow GC, Peterson ED, et al. Racial and ethnic differences in the treatment of acute myocardial infarction: findings from the Get With the Guidelines-Coronary Artery Disease program. Circulation. 2010;121(21):2294–301.
10 Sheifer SE, Rathore SS, Gersh BJ, et al. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000;102(14):1651–6.
11 Brown AL, Mann NC, Daya M, et al. Demographic, belief, and situational factors influencing the decision to utilize emergency medical services among chest pain patients. Rapid Early Action for Coronary Treatment (REACT) study. Circulation. 2000;102(2):173–8.
12 Bradley EH, Herrin J, Wang Y, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004;292(13):1563–72.
13 Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114(2):168–82.
14 Johansson I, Strömberg A, Swahn E. Factors related to delay times in patients with suspected acute myocardial infarction. Heart Lung. 2004;33(5):291–300.
15 Fang J, Gillespie C, Keenan NL, et al. Awareness of heart attack symptoms among US adults in 2007, and changes in awareness from 2001 to 2007. Future Cardiol. 2011;7(3):311–20.
16 Byrne M, Murphy AW, Plunkett PK, et al. Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med. 2003;41(3):309–18.
17 McGruder HE, Greenlund KJ, Malarcher AM, et al. Racial and ethnic disparities associated with knowledge of symptoms of heart attack and use of 911: National Health Interview Survey, 2001. Ethn Dis. 2008;18(2):192–7.
18 Hedges JR, Feldman HA, Bittner V, Goldberg RJ, Zapka J, Osganian SK, et al. Impact of community intervention to reduce patient delay time on use of reperfusion therapy for acute myocardial infarction: rapid early action for coronary treatment (REACT) trial. REACT Study Group. Acad Emerg Med. 2000;7(8):862–72.
19 Cricri P, Trachsel L, Müller P, Wäckerlin A, Reinhart W, Bonetti P. Incidence and time frame of life-threatening arrhythmias in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Swiss Med Wkly. 2012;142:w13604.
Funding / potential competing interests:University Hospital Centre (Lausanne, Switzerland), Cardiology’s research funds. The authors have no conflict of interest to declare.