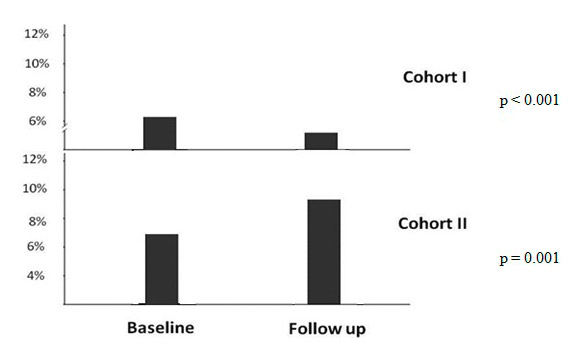
Figure 1
Proportion of patients with LDL cholesterol <70 mg/dl in both cohorts.
DOI: https://doi.org/10.4414/smw.2013.13828
BACKGROUND: Low density lipoprotein (LDL) cholesterol is a causative factor in coronary artery disease, and LDL cholesterol lowering by statins is a cornerstone in cardiovascular risk management. Current guidelines recommend serum LDL cholesterol <70 mg/dl for patients at very high risk, in particular for those with coronary arterial disease (CAD) or type 2 diabetes (T2DM). We aimed to investigate the proportion of patients achieving current lipid goals in two high-risk cohorts of CAD patients.
MATERIAL AND METHODS: We obtained lipid profiles for two cohorts of patients who underwent coronary angiography for the evaluation of previously (>1 month) established CAD in 1999–2000 (n = 346) and in 2005–2007 (n = 850), at baseline and after 2 years of follow-up.
RESULTS: Overall, the proportion of patients with baseline LDL cholesterol <70 mg/dl was 6.1% in the first and 7.3% in the second cohort (p = 0.236). In logistic regression analysis, male gender (odds ratio [OR] 1.33, 95% confidence interval [CI] 1.11–2.96; p = 0.021) and presence of diabetes (OR 1.76, 95% CI 1.30–2.38; p <0.001) were independent predictors for reaching this LDL cholesterol treatment goal. After 2 years of follow-up, the proportion of patients with LDL cholesterol <70 mg/dl was 1.3% in the first and 9.5% in the second cohort (p <0.001 for the comparison between the two cohorts; p = 0.001 for the comparison of cohort I at baseline vs after 2 years and p = 0.001 for the comparison of cohort II at baseline vs after 2 years).
CONCLUSION: The proportion of CAD patients meeting current lipid treatment goals is low and has only slightly improved.
Low density lipoprotein (LDL) cholesterol is a paramount risk factor for cardiovascular disease. For every increase in LDL cholesterol by 1 mg/dl, cardiovascular risk increases by about 1% [1]. Therefore, and because of the overwhelming evidence for a reduction of cardiovascular risk through treatment of high LDL cholesterol, current guidelines identify LDL cholesterol as the primary target of lipid lowering therapy [2].
LDL cholesterol-lowering statin treatment has become a cornerstone in the lipid management of high risk patients [3–5]. Indeed, meta-analyses of statin trials show a 15%–20% reduction of cardiovascular risk per mmol decrease in LDL cholesterol through statin treatment [6–9]. The reduction in relative cardiovascular risk strongly depends on the obtained on-treatment LDL cholesterol. With the lowest LDL cholesterol, cardiovascular risk reduction is greatest.
Because a given amount of relative risk reduction translates into the greatest reduction of absolute risk in the patients who are at the highest risk, the targets of LDL lowering therapy set forth in current guidelines depend on the cardiovascular risk status. For high-risk patients (such as patients with markedly elevated single risk factors), an LDL cholesterol of at least <100 mg/dl should be achieved; in very high-risk patients, such as patients with coronary arterial disease (CAD), type 1 diabetes with target organ damage, or patients with type 2 diabetes (T2DM) an LDL cholesterol below 70 mg/dl is recommended [10].
Data on the proportion of patients from current clinical practice who actually meet these LDL cholesterol targets are scarce, especially data comparing two different time periods and also including follow-up information. We therefore aimed at investigating the LDL cholesterol levels achieved as well as the proportion of patients achieving current LDL cholesterol goals in two high-risk cohorts of CAD patients who were recruited 7 years apart. We hypothesised that with the increasing evidence for cardiovascular risk reduction the proportion of patients being treated according to guideline recommendations should have increased from the first to the second patient cohort and from baseline to the 2-year follow-up. Subgroup analyses were planned with regard to sex and diabetes status. Given the paramount role of LDL cholesterol and of statin treatment in current national [11, 12] and international lipid guidelines [10] we focused on LDL cholesterol.
We recruited two cohorts of consecutive Caucasian patients who underwent coronary angiography for the evaluation of established or suspected CAD at the Academic Teaching Hospital Feldkirch, as reported previously [13, 14]. Patients with recent (<3 months) acute coronary syndromes were not included. Cohort I (n = 756) was consecutively enrolled from July 1999 to August 2000, and cohort II (n = 1033) 7 years later, from August 2005 to February 2007.
CAD had previously (>1 month) been diagnosed in 346 patients of the first and in 850 patients of the second cohort, in total in 1,196 patients. In the present retrospective, observational analysis only these patients who had previously established CAD were included, that is, 45.7% of the first and 82.2% of the second patient cohort. Thus, inclusion criteria for the present analysis were a history of CAD and referral for coronary angiography, the sole exclusion criterion was a recent (<3 months) acute coronary syndrome.
Data were collected both from patient records and from standardised interviews, and were cross-checked between these sources. All coworkers involved in data collection were specifically trained by the authors of the present manuscript (CHS, AV). The same methods of data collection were used for both cohorts.
Previous CAD was defined as previous acute coronary syndromes, previous angiographic evidence of coronary atherosclerosis, or previously documented cardiac ischaemia in standard stress tests. A history of angina without confirmatory stress testing or angiography was not considered sufficient for a diagnosis of previous CAD. The same criteria were used for both patient cohorts.
Furthermore, we performed follow-up examinations in these two patient groups after 2 years, in 2002–2004 in cohort I, and in 2009–2011 in cohort II. The mean follow-up time was 2.3 years in cohort I and 2.6 years in cohort II. The patients visited our outpatient research centre for the follow-up evaluations; patient interviews with standardised questionnaires in which also medication was queried were performed. Lost to follow-up rates were 19.3% in cohort I and 13.5% in cohort 2. The same methodology of follow-up was used in both cohorts.
Information on conventional cardiovascular risk factors was obtained by means of a standardised interview with patients and systolic/diastolic blood pressure was measured by the Riva-Rocci method under resting conditions in a sitting position at the day of hospital entry at least 5 hours after hospitalisation. Hypertension was defined according to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [15] and T2DM was diagnosed according to World Health Organisation criteria [16]. Height and weight were recorded, and body mass index (BMI) was calculated as body weight (kg) / height (m)². All patients received routine instructions regarding lifestyle changes (including diet, exercise and smoking cessation where applicable) at baseline as well as at follow-up, as recommended in current guidelines [10]. Statins were prescribed or statin prescription was recommended at discharge for all patients.
Coronary angiography was performed using the Judkins technique. Coronary artery stenoses with lumen narrowing of 50% or more were considered significant, and CAD was diagnosed in the presence of any visible lumen narrowing at angiography, as described previously [17, 18]. The ethics committee of the University of Innsbruck approved the present study, and all participants gave written informed consent.
Venous blood samples at baseline were collected after an overnight fast of 12 hours before angiography was performed. Blood sampling at follow-up was performed during the outpatient visits. The serum levels of triglycerides, total cholesterol, LDL cholesterol, and high density lipoprotein (HDL) cholesterol were determined using enzymatic hydrolysis and precipitation techniques (Triglycerides GPO-PAP, Cholesterol CHOD/PAP, QuantolipLDL, QuantolipHDL; Roche, Switzerland) on a Hitachi-Analyzer 717 or 911. Haemoglobin A1c (HbA1c) was determined by high-performance liquid chromatography on a Menarini-Arkray KDK HA 8140 (Japan), and glucose levels were measured enzymatically from venous fluoride plasma by the hexokinase method (Roche, Switzerland) on a Hitachi 717 or 911.
To test independent between-group differences of continuous variables for statistical significance, two-sided t-tests and analysis of variance were used for normally distributed variables and Mann-Whitney-U-tests for nonparametric variables; for paired within group comparisons, paired t-tests and non-parametric Wilcoxon tests were applied for normally and for non-normally distributed variables, respectively. Discrete parameters were compared by chi-square tests for nonpaired analyses and with McNemar tests for paired analyses. Adjusted odds ratios (ORs) were derived from logistic regression models. We used a fully adjusted logistic regression model, where all investigated covariates were forced into the model. As covariates standard demographic variables (age, gender) and standard cardiovascular risk factors (BMI, diabetic state, hypertension, smoking history) were selected. The same statistical methods as those used for the total study population were applied in subgroup analyses. P-values <0.05 were considered statistically significant. All statistical analyses were performed with SPSS 20.0 for Windows.
| Table 1:Baseline characteristics. | |||
| Cohort 1 | Cohort 2 | p-value | |
| Men (%) | 70.8 | 66.5 | 0.177 |
| Age (years) | 63.4 ± 10.0 | 66.5 ± 10.5 | 0.001 |
| HbA1c (%) | 6.2 ± 1.1 | 6.2 ± 1.1 | 0.856 |
| BMI (kg/m²) | 27.8 ± 12.6 | 27.8 ± 4.6 | 0.035 |
| Hypertension (%) | 53.9 | 73.9 | <0.001 |
| Sign. stenoses (%) | 76.2 | 66.2 | 0.001 |
| Smoking (%) | 59.0 | 57.2 | 0.441 |
| Diabetes (%) | 24.9 | 26.9 | 0.480 |
| Triglycerides (mg/dl) | 170 ± 113 | 140 ± 85 | <0.001 |
| Cholesterol (mg/dl) | 207 ± 52 | 190 ± 45 | <0.001 |
| HDL Cholesterol (mg/dl) | 45 ± 13 | 55 ± 15 | <0.001 |
| LDL cholesterol (mg/dl) | 122 ± 40 | 123 ± 40 | 0.499 |
| BMI = body mass index; CAD coronary artery disease; HDL = high density lipoprotein; LDL = low density lipoprotein; To convert values for triglycerides to mmol/l multiply by 0.0113 and to convert total cholesterol, LDL cholesterol, or HDL cholesterol to mmol/l multiply by 0.0259; p-values are given for the all overall difference between study groups. Data are given as mean ± standard deviation; p-values are given for between group differences. | |||
| Table 2:Proportion of patients taking lipid lowering drugs. | ||||||
| Cohort 1 baseline | follow-up | p-value | Cohort 2 baseline | follow-up | p-value | |
| Statins (%) | 43.0 | 52.7 | <0.001 | 47.0 | 39.1 | <0.001 |
| Nicotinic acid (%) | 0.0 | 0.0 | – | 0.5 | 2.3 | <0.001 |
| Fibrates (%) | 3.2 | 2.2 | 0.250 | 1.4 | 0.7 | <0.001 |
| Ezetrol (%) | 0.0 | 0.0 | – | 0.7 | 2.1 | <0.001 |
Overall, both cohort I (n = 346) and cohort II (n = 850) were characteristic of CAD patients undergoing coronary angiography, with a mean age of around 65 years, a preponderance of male gender, and a high prevalence of hypertension, smoking, and diabetes. Coronary angiography revealed significant coronary stenoses in 76.2% of the patients from cohort I, and in 66.2% from cohort II, respectively. Baseline characteristics of the two patient cohorts are summarised in table 1. The proportion of patients taking statins, fibrates, or nicotinic acid at baseline and after follow-up is shown in table 2. No other lipid lowering agents were taken.
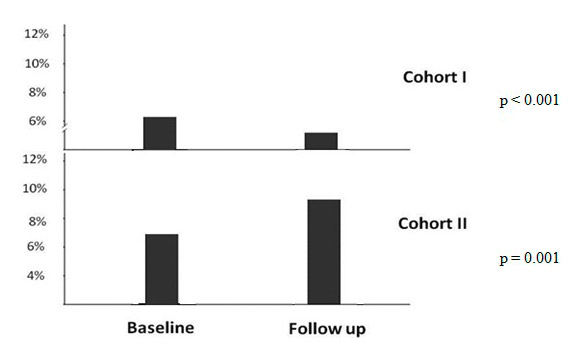
Figure 1
Proportion of patients with LDL cholesterol <70 mg/dl in both cohorts.
Overall, the proportion of patients with baseline LDL cholesterol <100 mg/dl was 26.9% in the first and 31.6% in the second patient cohort (p = 0.066), and the proportion of patients with baseline LDL cholesterol <70 mg/dl, as recommended in the ESC guidelines, was 6.1% in the first and 7.3% in the second cohort (p = 0.236). In cohort I 45% of the patients who did not achieve the LDL cholesterol goal <70 mg/dl and in cohort II 49% of the patients who did not achieve the LDL cholesterol goal <70 mg/dl, were on statin therapy at baseline.
In cohort I, median LDL cholesterol was 123 [interquartile range 44–218; 95% CI of mean 119.2–127.1] at baseline and 134 [interquartile range 52–313; CI of mean 132.2–142.1] at follow-up. The corresponding LDL cholesterol values were 119.0 [interquartile range 26–283; 95% CI of mean 119.4–125.7] and 112 [interquartile range 33–234; CI of mean 103.5–110.8] in cohort II at baseline and at follow-up, respectively.
Regarding baseline triglyceride levels, 54.9% from the first and 68.6% from the second cohort achieved the goal of <150 mg/dl (p <0.001). Current guidelines recommend following non-HDL cholesterol rather than LDL cholesterol targets in patients with serum triglycerides >200 mg/dl. From the 26.1% CAD patients of cohort I and the 16.3% CAD patients of cohort II with baseline triglycerides >200 mg/dl, 6.7% and 18.1%, achieved a non-HDL cholesterol of <130 mg/dl; this difference was statistically significant (p = 0.014). Furthermore, 2.5% in cohort I and 19.1% (p <0.001) in cohort II achieved the non-HDL cholesterol goal of <100 mg/dl.
In cohort I, the mean baseline systolic blood pressure was 137 ± 20 mm Hg and the mean baseline diastolic blood pressure was 78 ± 11 mm Hg. In cohort II, the mean baseline systolic blood pressure was 137 ± 18 mm Hg and the mean diastolic blood pressure 81.84 ± 9 mm Hg.
After 2 years of follow-up, the proportion of patients with LDL cholesterol <100mg/dl was 17.2% in the first and 48.5% in the second cohort (p for the comparison between the cohorts <0.001). There were significant differences between baseline and follow-up in both patient cohorts (p = 0.001 and p <0.001 for cohorts I and II, respectively). Furthermore, the proportion of patients with LDL cholesterol <70mg/dl was 1.3% in the first and 9.5% in the second cohort (p <0.001 for the comparison between the cohorts). Again, there were significant differences between baseline and follow-up in both patient cohorts (p <0.001 and p = 0.001 for cohorts I and II, respectively). In cohort I 55% of the patients who did not achieve the LDL cholesterol goal <70 mg/dl and in cohort II 47% of the patients who did not achieve the LDL cholesterol goal <70 mg/dl, were on statin therapy at follow-up.
Regarding triglycerides, 54.3% in cohort I and 65.5% in cohort II achieved values <150 mg/dl (for the comparison between the cohorts p = 0.003) with a significant difference between baseline and follow-up (p = 0.001 and p = <0.001 for cohort I and cohorts II, respectively). A total of 23.9% of the patients of cohort I and 16.1% of cohort II had triglycerides >200 mg/dl after 2 years of follow-up; p <0.001 for the comparison between the cohorts). From these patients, 7.6% in cohort and 25.4% in cohort II achieved a non-HDL cholesterol of <130 mg/dl (p <0.001); 4.8% in cohort I and 12.8% in cohort II achieved the non-HDL cholesterol goal of <100 mg/dl (p <0.001). There again was a significant difference between baseline and follow-up in non-HDL goal attainment in cohort I and cohort II (p <0.001; fig. 1).
At follow-up systolic and diastolic blood pressure were 139 ± 24 mm Hg and 80 ± 12 mm Hg, respectively in cohort I and 143 ± 28 mm Hg and 83.52 ± 12, respectively, in cohort II. Among smokers, the smoking cessation rate was 12% in cohort I and 18% in cohort II during the follow-up period.
Table 3 summarises lipid parameters of our two populations with respect to gender. Among our male coronary patients, LDL cholesterol at baseline was <70 mg/dl in 6.9% of the first and in 6.8% in the second patient cohort (p = 0.445 for the comparison between the two cohorts). After 2 years of follow-up, the proportion of patients with an LDL cholesterol <70 mg/dl was 2.0% and 6.9% in cohorts I and II, respectively (p <0.001 for both comparisons). There was no significant difference with regard to achieving the <70 mg/dl goal between baseline and follow up in cohort I (p = 0.180) but in cohort II (p = 0.002).
In female coronary patients, LDL cholesterol was <70 mg/dl in 2.1% of cohort I and in 6.2% of cohort II (p = 0.011). After 2 years of follow up, the proportion of patients with an LDL cholesterol <70 mg/dl was 1.5% and 9.0% in cohorts I and II, respectively (p <0.001 for both comparisons). There was no significant difference with regard to achieving the <70 mg/dl goal between baseline and follow up in cohort I (p = 0.180) nor in cohort II (p = 0.131).
Table 4 summarises lipid parameters of our two populations with respect to the diabetic state Among our diabetic coronary patients, LDL cholesterol was <70 mg/dl in 2.9% of the first and in 8.3% of the second patient cohort (p = 0.001 for the comparison between the two cohorts). After follow-up, the proportion of patients with an LDL cholesterol <70 mg/dl was 1.2% and 11.7% between cohort I and cohort II (p <0.001). There was a significant difference with regard to achieving the <70 mg/dl goal between baseline and follow up in cohort II (p = 0.001) but not in cohort I (p = 0.061).
Among patients who did not have diabetes, LDL cholesterol was <70 mg/dl in 2.6% of cohort I patients and in 1.3% of the cohort II patients (p = 0.008 for the comparison between the two cohorts). After follow-up, the proportion of patients with an LDL cholesterol <70 mg/dl was 1.3% and 5.8% between cohort I and cohort II (p <0.001). There was no significant difference with regard to achieving the <70 mg/dl goal between baseline and follow-up in cohort I (p = 0.086) and in cohort II (p = 0.080).
In logistic regression analysis, male gender (OR 1.33 CI 1.11–2.96; p = 0.021) and the presence of diabetes (OR 1.76 CI 1.30–2.38; p <0.001) proved to be independent predictors of reaching the LDL cholesterol treatment goal after adjustment for age, BMI, hypertension and smoking history (table 5).
| Table 3: Lipid parameters with respect to gender. | ||||||||
| Cohort 1 baseline | follow-up | p-value1 | Cohort 2 baseline | follow-up | p-value1 | p-value 2 | ||
| LDL cholesterol (mg/dl) | male female | 129.9 ± 34 133.3 ± 38 | 139.9 ± 40 149.1 ± 43 | <0.001 <0.001 | 124.5 ± 40 132.4 ± 42 | 109.5 ± 35 117.8 ± 39 | <0.001 <0.001 | <0.001 <0.001 |
| HDL cholesterol (mg/dl) | male female | 44.5 ± 12 56.7 ± 14 | 51.1 ± 13 63.5 ± 17 | <0.001 <0.001 | 52.5 ± 14 63.5 ± 18 | 51.3 ± 16 59.4 ± 19 | <0.001 <0.001 | 0.809 0.007 |
| Triglycerides (mg/dl) | male female | 175.7 ± 114 140.8 ± 78 | 171.2 ±110 142.9 ± 93 | 0.664 0.560 | 142.9 ± 92 131.7 ± 80 | 143.9 ± 91 136.6 ± 83 | 0.482 0.058 | <0.001 0.633 |
| Cholesterol (mg/dl) | male female | 214.2 ± 42 225.3 ±45 | 214.3 ± 44 233.1 ±50 | 0.732 0.016 | 189.1 ± 45 206.1 ± 47 | 181.2 ± 40 196.6 ± 43 | <0.001 0.016 | <0.001 <0.001 |
| LDL-C <100 mg/dl (%) | male female | 19.7 20.2 | 15.3 8.3 | 0.092 0.001 | 29.1 37.1 | 42.7 36.8 | <0.001 0.001 | <0.001 0.298 |
| LDL-C <70 mg/dl (%) | male female | 2.9 2.1 | 1.7 1.5 | 0.180 0.180 | 6.1 6.2 | 9.8 9.0 | 0.002 0.131 | 0.007 0.011 |
| TG <200 mg/dl (%) | male female | 71.7 85.2 | 71.0 84.5 | 0.654 0.212 | 80.9 88.2 | 83.9 87.1 | 0.065 0.486 | <0.001 0.170 |
| Non HDL cholesterol <100 mg/dl (%) | male female | 2.3 2.9 | 4.9 4.7 | 0.041 0.616 | 20.4 16.7 | 22.3 18.4 | 0.069 0.881 | <0.001 <0.001 |
| BMI = body mass index; CAD coronary artery disease; HDL = high density lipoprotein; LDL = low density lipoprotein; To convert values for triglycerides to mmol/l multiply by 0.0113 and to convert total cholesterol, LDL cholesterol, or HDL cholesterol to mmol/l multiply by 0.0259; p-values are given for the all overall difference between study groups. Data are given as mean ± standard deviation; 1p-value for the comparison between baseline and follow-up; 2p-value for the comparison between groups 1 and 2. | ||||||||
| Table 4: Lipid parameters with respect to diabetic state. | ||||||||
| Cohort 1 baseline | follow-up | p-value1 | Cohort 2 baseline | follow-up | p-value1 | p-value 2 | ||
| LDL cholesterol (mg/dl) | DM No DM | 121.9 ± 38 133.6 ± 35 | 134.8 ± 38 145.1 ± 41 | <0001 0.001 | 115.5 ± 39 131.6 ± 41 | 98.1 ± 32 117.4 ± 37 | <0.001 <0.001 | 0.062 0.178 |
| HDL cholesterol (mg/dl) | DM No DM | 43.8 ± 14 49.8 ± 14 | 50.3 ± 15 56.4 ± 16 | <0.001 <0.001 | 51.0 ± 14 58.3 ± 17 | 50.5 ± 16 55.3 ± 18 | 0.040 0.081 | <0.001 <0.001 |
| Triglycerides (mg/dl) | DM No DM | 203.2 ±137 153.3 ± 91 | 199.6 ±127 151.7 ± 96 | 0.548 0.473 | 156.7 ± 91 132.8 ± 87 | 149.7 ± 87 138.2 ± 88 | 0.002 0.063 | <0.001 <0.001 |
| Cholesterol (mg/dl) | DM No DM | 210.3 ± 48 220.0 ± 41 | 214.1 ± 47 222.1 ± 47 | 0.364 0.129 | 181.1 ± 44 200.2 ± 47 | 170.0 ± 38 192.2 ± 42 | <0.001 <0.001 | <0.001 <0.001 |
| LDL-C <100 mg/dl (%) | DM No DM | 31.2 16.6 | 64.1 12.2 | <0.001 0.006 | 37.6 22.6 | 30.8 35.8 | 0.018 0.030 | 0.102 0.004 |
| LDL-C <70 mg/dl (%) | DM No DM | 2.9 2.6 | 1.2 1.3 | 0.061 0.086 | 8.3 5.3 | 11.7 5.8 | 0.001 0.080 | 0.017 0.008 |
| TG <200 mg/dl (%) | DM No DM | 62.4 80.0 | 50.3 77.8 | <0.001 0.001 | 77.1 85.8 | 46.6 86.2 | <0.001 0.450 | 0.001 0.003 |
| Non HDL cholesterol <100 mg/dl (%) | DM No DM | 4.1 2.0 | 4.3 3.8 | 0.379 0.089 | 26.3 16.4 | 18.0 17.1 | <0.001 0.346 | <0.001 0.001 |
| BMI = body mass index; CAD coronary artery disease; DM = diabetes mellitus; HDL = high density lipoprotein; LDL = low density lipoprotein; To convert values for triglycerides to mmol/l multiply by 0.0113 and to convert total cholesterol, LDL cholesterol, or HDL cholesterol to mmol/l multiply by 0.0259; p-values are given for the all overall difference between study groups. DM denotes diabetes mellitus type 2. Data are given as mean ± standard deviation; 1p-value for the comparison between baseline and follow-up; 2p-value for the comparison between groups 1 and 2. | ||||||||
| Table 5:Logistic regression model. | |||
| Odds ratio | 95% confidence interval | p-value | |
| Presence of diabetes | 1.76 | 1.30–2.38 | <0.001 |
| Male gender | 1.33 | 1.11–2.96 | 0.021 |
| Body mass index | 1.08 | 0.58–2.00 | 0.200 |
| Hypertension | 1.13 | 0.62–2.05 | 0.681 |
| Age | 0.99 | 0.96–1.02 | 0.745 |
| Smoking history | 1.06 | 0.58–1.93 | 0.840 |
From these Central European data we conclude that a huge proportion of patients with established CAD are still not receiving lipid lowering therapy, and that an even greater proportion of CAD patients do not achieve the current cholesterol targets, despite the overwhelming evidence from randomised clinical trials showing that lowering LDL cholesterol with statins significantly reduces cardiovascular events in high-risk patients [19, 20]. The results of the comparison of these two cohorts suggest that there is a disparity between guidelines and clinical reality with regard to statin use and LDL cholesterol goal attainment in our region.
Our data expand existing knowledge in several ways: First, there are only very limited data on the proportion of patients meeting lipid treatment goals in Central Europe. Second, most studies did not evaluate the achievement of lipid treatment goals at different time points and in a longitudinal approach.
The results of our study are consistent with multiple other studies observing that there is a gap between guidelines and actual clinical practice. Coon and Zulkowski [21] investigated the achievement of American Diabetic Association (ADA) lipid goals among diabetic patients. These authors found that only 25% of the investigated 399 patients had serum LDL cholesterol levels below 100 mg/dl. The Lipid Treatment Assessment Project (L-TAP), multicentre study enrolled 4,888 diabetic patients and found that only 18% of these patients achieved LDL-cholesterol levels <100 mg/dl. Furthermore, in a study of 603 patients with CAD, who were recruited in 45 various practices in the United States, only 14% had LDL-cholesterol levels <100 mg/dl, and 33% were taking lipid lowering drugs [20]. In another study electronic medical records of 10,040 patients with CAD from a large cardiology subspecialty practice were reviewed, 79% achieved the recommended goal <100 mg/dl and only few achieved the more aggressive goal of <70 mg/dl [22]. The results of the hospital screening project (HSP) an observational study, which was performed in 20 Austrian departments also were in line with these studies: 48% of the patients did not achieve the LDL goals [23]. A further investigation from Kitgunvgan et al. [24] showed an improving trend in high and very high risk patients but the data were also in line with our study.
In our investigation there was a significant improvement in achieving lipid goals in the second cohort between the baseline investigation and the 2-year follow-up, but the majority of the investigated high-risk patients did still not achieve the recommended goals.
Further, our data show that male gender and diabetes mellitus state are associated with achievement of LDL cholesterol goals. Of note, a recent publication by Martin et al. showed no impact of gender in the achievement of LDL cholesterol [25]. However, this investigation showed results from patients after an acute myocardial infarction and not in stable CAD patients as we did.
The proportion of patients on statins somewhat surprisingly decreased during follow up in cohort II. From our data no unambiguous explanation for this finding can be derived. Whatsoever, we feel that it is important to draw attention to the fact that despite the evolving large body of evidence in favour of statin therapy in CAD patients, it still not infrequently occurs that previously prescribed statins are dismissed in these high-risk individuals. Physicians should be very restrictive regarding the termination of this effective treatment in this population.
Important strengths of our study are the collection of data from two cohorts of coronary patients recruited 7 years apart and after 2 years of follow-up and the additional investigation of these patients during a follow-up period. Our data were collected at the largest medical centre in the province of Vorarlberg, are representative for the region, and our results are in line with the data reported in the literature. This study also has limitations. First, this was a single centre study from a single geographical region, our population therefore does not represent all patients with CAD. Second, data regarding the exact type of statin molecule, dosages of statins, and potential contraindications to statin treatment were not recorded. Further, the LDL cholesterol goals were less strict 10 years before than today (100 mg/dl instead of 70 mg/dl in high-risk patients). Also, we did not achieve a 100% follow-up rate and we do not have quantitative data regarding other factors apart from lipid lowering medication that may influence LDL cholesterol levels such as diet, smoking, exercise, and lifestyle modifications.
We conclude that targeted programmes to improve the lipid management of CAD patients in current clinical practice are necessary. Also, we need further and wide ranging prospective clinical research in this very important area of medicine.
1 Kannel WB. Lipids, diabetes, and coronary heart disease: insights from the Framingham Study. Am Heart J. 1985;110:1100–07.
2 Stone NJ, Bilek S, Rosenbaum S. Recent National Cholesterol Education Program Adult Treatment Panel III update: adjustments and options. Am J Cardiol. 2005;96:53E–9E.
3 Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14(Suppl 2):S1–113.
4 Jeger R, Dieterle T. Statins: have we found the Holy Grail? Swiss Med Wkly. 2012;142:w13515.
5 Braunersreuther V, Mach F, Montecucco F. Statins and stent thrombosis. Swiss Med Wkly. 2012;142:w13525.
6 Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
7 Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78.
8 Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–90.
9 Kearney PM, Blackwell L, Collins R, Keech A, Simes J, Peto R. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371:117–25.
10 Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32:1769–818.
11 AAS Guidelines. 2013; http://www.aas.at.
12 AGLA guidelines. 2013; http://www.agla.ch.
13 Vonbank A, Saely CH, Rein P, Beer S, Breuss J, Boehnel C. Insulin resistance is associated with the metabolic syndrome and is not directly linked to coronary artery disease. Clin Chim Acta. 2011;412:1003–7.
14 Saely CH, Rein P, Vonbank A, Huber K, Drexel H. Type 2 diabetes and the progression of visualized atherosclerosis to clinical cardiovascular events. Int J Cardiol. 2012.
15 Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
16 Zimmet P, Alberti G, de Court. New classification and criteria for diabetes: moving the goalposts closer. Med J Aust. 1998;168:593–4.
17 Drexel H, Amann FW, Rentsch K, Neuenschwander C, Luethy A, Khan SI. Relation of the level of high-density lipoprotein subfractions to the presence and extent of coronary artery disease. Am J Cardiol. 1992;70:436–40.
18 Drexel H, Amann FW, Beran J, Rentsch K, Candinas R, Muntwyler J. Plasma triglycerides and three lipoprotein cholesterol fractions are independent predictors of the extent of coronary atherosclerosis. Circulation. 1994;90:2230–5.
19 Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421.
20 Qayyum R, Chattha AA, Bhullar N, Katsetos M, Schulman P. Achievement of national cholesterol education program goals by patients with dyslipidemia in rural ambulatory care settings. Prev Cardiol. 2006;9:192–7.
21 Coon P, Zulkowski K. Adherence to American Diabetes Association standards of care by rural health care providers. Diabetes Care. 2002;25:2224–9.
22 Karalis DG, Subramanya RD, Hessen SE, Liu L, Victor MF. Achieving Optimal Lipid Goals in Patients With Coronary Artery Disease. Am J Cardiol. 2011.
23 Roden M, Huber K. Lipid profiles and therapy status in the secondary prevention of high risk patients with cardiovascular disease and/or diabetes mellitus: the Austrian Hospital Screening Project (HSP). Wien Klin Wochenschr. 2008;120:558–65.
24 Kitkungvan D, Lynn Fillipon NM, Dani SS, Downey BC. Low-density lipoprotein cholesterol target achievement in patients at high risk for coronary heart disease. J Clin Lipidol. 2010;4:293–7.
25 Martin SS, Gosch K, Kulkarni KR, Spertus JA, Mathews R, Ho PM. Modifiable factors associated with failure to attain low-density lipoprotein cholesterol goal at 6 months after acute myocardial infarction. Am Heart J. 2013;165:26–33.