Figure 1
Flow-chart.
DOI: https://doi.org/10.4414/smw.2013.13825
Plantar fasciitis is the most common cause of inferior heel pain, and about 10% of people develop this disease throughout their lifetime. The aetiology of plantar fasciitis is not clearly understood, but several risk factors such as bone spurs, pronated foot type, obesity, limb-length discrepancy and work-related weight-bearing appear to increase the risk of plantar fasciitis [1–3]. Histological findings show that “plantar fasciitis” is a chronic degenerative process rather than an acute inflammatory change [4].
Plantar fasciitis is regarded as a self-limiting disease, and over 90% of patients will be cured within 6 months with nonoperative treatment [5]. Conservative treatment includes: physical treatment such as low dye strapping, therapeutic orthotic insoles, orthotic devices, night splints, Achilles and plantar fascia stretching; pharmacotherapy such as oral inflammatory medication, cortisone injections and botulinum toxin injections [6]. The American College of Foot and Ankle Surgeons (ACFAS) heel pain committee recommend that patients should have chronic symptoms and undergo conservative treatment for at least 6 months prior to considering extracorporeal shock wave therapy (ESWT) or surgical treatment [7].
ESWT is a derivative of lithotripsy. The use of ESWT for the treatment of plantar fasciitis evolved in Europe. ESWT received first FDA-approval for the treatment of plantar fasciitis in 2000. Methods of shockwave generation include electrohydraulic, electromagnetic, piezoelectric or radial. Low-energy ESWT (LESWT) was considered to be flux application <0.2 mJ/mm2 and high-energy ESWT (HESWT) was flux application >0.2 mJ/mm2; high-energy flux application may require local or regional anaesthesia when not well tolerated. Chow compared the effectiveness of a “fixed” energy density and “maximum tolerable” energy density of ESWT in the treatment of RPF, and the results showed that ESWT with a maximum tolerable energy density was more effective in terms of relieving pain and restoring functional activity [8]. It is generally understood that enough energy should be delivered to induce a therapeutic response, and that LESWT needs repeated treatments to achieve a therapeutic dose and is more expensive than HESWT.
We performed this meta-analysis focusing on HESWT in order to produce a firm evidence base for clinical decision-making. Strong evidence is needed to guide clinical decisions and to provide the best therapeutic schedule for the patients.
We reviewed all RCTs comparing ESWT and placebo from PubMed, EMBASE and the Cochrane Central Register of Controlled Trials up to the end of December 2013, as well as the reference lists of the articles, and contacted the original author if necessary. We also searched unpublished RCTs to minimise publication bias. The keywords included “shock waves” or ”ultrasonic therapy” concatenated with ”plantar fasciitis” or ”plantar fasciopathy” or ” heel spur syndrome”. Assessment of eligibility of studies and extraction of data from study reports were preceded by two independent reviews, and any dispute was resolved by the third reviewer. Title and abstract were reviewed first and if they met our inclusion criteria, the full article was obtained.
All research was screened for eligibility into the study using the inclusion and exclusion criteria listed in table 1.
All identified studies were reviewed in full text and abstracted data independently and in parallel by two authors (Li ZY, Jin Tao). The following data were extracted: the author and year of publication, method of randomisation, method of blinding, method of allocation concealment, withdrawals and dropouts inclusion criteria; exclusion criteria, HESWT applied; patients enrolled and loss to follow up, follow up period and also clinical success on VAS. Disagreements were resolved through discussion.
Reviewers Li ZH and Jin Tao evaluated the quality of all included trials in accordance with the Jadad score [9]; allocation concealment was included in this quality score. This widely used scale evaluates the reporting of studies with respect to the method of randomisation, adequacy of blinding and appropriate description of withdrawals. Allocation concealment was assessed as a supplement. Controversy was also resolved by discussion.
Five RCTs were included in this study and thus the sample size was too small for a funnel plot to detect publication bias. Q-statistic was used to investigate the degree of variation between trials, a p-value >0.1 was interpreted as homogeneity. The I2-statistical test was further used as a measure of heterogeneity, I2 <30% was considered as mild heterogeneity, I2 >50% was considered notable heterogeneity, and a value of I2between the two values was considered as moderate heterogeneity. Since in our study I2was equal to 0.31, a fixed-effects model was used to pool estimates.
All data analyses were performed using Revman 5.0.
| Table 1: Inclusion criteria and exclusion criteria. | ||
| Inclusion criteria | Exclusion criteria | |
| Participants | Adults over the age of 18 years; recalcitrant plantar fasciitis(plantar fasciitis over 6 months; unsuccessful conservative treatment including at least one pharmacological therapy and two nonpharmacological therapies; Baseline pain ≥5 points on VAS. | Any other treatment used for the duration of the study. |
| Intervention | ESWT with energy >0.2 mJ/mm2 | ESWT with energy ≤0.2 mJ/mm2 |
| Comparison | Placebo treatment without energy transmit to treatment site | Low dose of ESWT or other conservative treatment |
| Outcome | Clinical success on VAS | Lack of reporting clinical success on VAS score |
| Study | RCT with double blind | No blinding or single blind |
| VAS, visual analog scale. Clinical success on VAS: 50% decrease from baseline and a VAS score ≤4 cm or >60% improvement from baseline on the visual analog scale | ||
| Table 2: Characteristics of included trials. | |||||
| Study | HESWT applied | Patients enrolled (completed), N (n) | Follow- up | Outcome (Clinical success) | Result |
| Ogden et al. [21], 2004 | Single treatments 1,500 shockwaves 0.22 mj/mm2 | 293 (285) | 12 weeks | 50% decrease from baseline and a VAS score ≤4 cm | Significant difference |
| Theodore et al. [16], 2004 | Single treatments 3,800 shockwaves 0.36 mJ/mm2 | 150 (146) | 12 weeks | >60% improvement from baseline on the visual analogue scale | Significant difference |
| Kudo et al. [26], 2006 | Single treatments 3,800 shockwaves 0.36 mJ/mm2 | 114(105) | 12 weeks | >60% improvement from baseline on the visual analogue scale | Significant difference |
| Malay et al. [27], 2006 | Single treatments 3,800 shockwaves High energy“ Level 7” | 172 (152) | 12 weeks | 50% decrease from baseline and a VAS score ≤4 cm | Significant difference |
| Gollwitzer et al. [28], 2007 | 3 treatments 2,000 shockwaves 0.25 mJ/mm2 | 40 (40) | 12 weeks | >60% improvement from baseline on the visual analogue scale | Not significant |
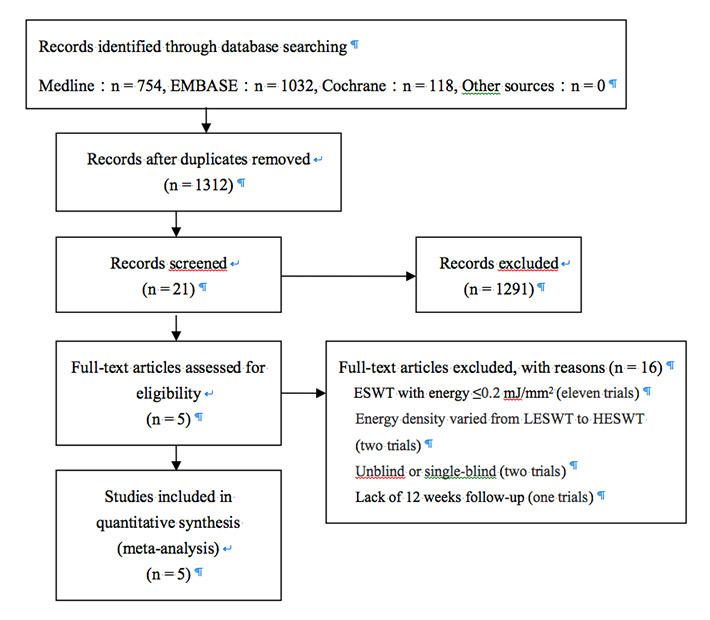
We identified 21 RCTs comparing ESWT with placebo in the treatment of plantar fasciitis from the initial search. After full text review, eleven trials were excluded because the energy of ESWT was <0.2 mJ/mm2; Cosentino [10] employed energy densities varying from 0.03 to 0.4 mJ/mm2 in the active group and was excluded; Buchbinder [11] compared ESWT with energy varying from 0.02 to 0.33 mJ/mm2 with a small dose of ESWT as placebo and was also excluded; Hammer [12] and Chow [8] performed nonblinded and single-blind RCTs, respectively, which were excluded; Wang [13, 14] performed a RCT with a long follow-up, which was excluded. Ultimately, five trials (table 2) met all inclusion criteria and were included in the final meta-analysis (fig. 1).
Figure 1
Flow-chart.
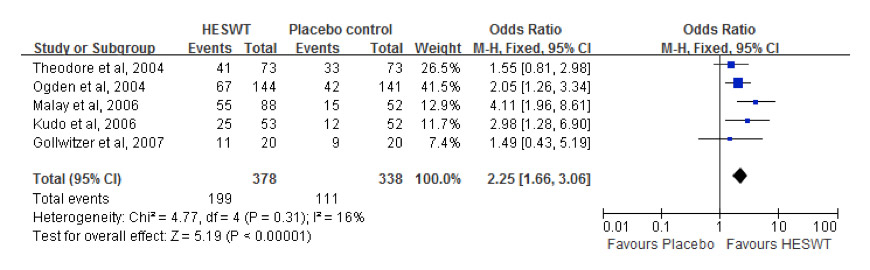
Figure 2
Forest plot of the five studies.
Inclusion criteria and exclusion criteria were generally similar among the five trials. However, three trials applied 3,800 shockwaves with similar energy density in a single treatment while the other two applied different energy densities or different treatment times. All five trials reported 12 weeks of follow-up with assessment of clinical success on a visual analogue scale (VAS). Two criteria for clinical success were used (table 2): in the 10-point VAS, either over 60% improvement from baseline or over 50% improvement and a VAS score ≤4 cm. Four trials showed significant differences in the outcome and one nonsignificant outcome after 12 weeks follow-up.
The results of quality scoring are shown in table 3, and all five trials met the criteria for high quality.
From our pooled analysis of five studies with 716 patients, clinical success varied from 46.5% to 62.5% in the active group and 28.8% to 45.2% in the placebo group. A Forest plot illustrating the ORs of the individual trials and the pooled data are shown in figure 2. The Forest plot revealed obvious overlapping confidence intervals, indicating homogeneity between these trials. Formal testing for heterogeneity confirmed the presence of little heterogeneity (p = 0.31, I2= 16%), and a fixed-effects model was used to pool estimates. Therefore, conclusions from this analysis are crediblebecause of the high quality of the inclusion trials and homogeneity among these trials. Meta-analysis of the five studies indicated a significant curative effect of HESWT in the treatment of recalcitrant plantar fasciitis, the pooled OR from the five trials was estimated at 2.25 (95% CI 1.66–3.06; p <0.00001).
Table 4 shows the results of the sensitivity and subgroup analyses. We performed sensitivity analyses for the fixed-effects model versus a random-effects model by dislodging one study in turn. The fixed effects model and random-effects model had similar results, and the overall risk estimates do not show obvious change by any of the studies, with OR value ranging from 1.98 (95% CI 1.41‒2.78) to 2.5 (95% CI 1.77‒3.55).
| Table 3: Validity assessment. | |||||
| Ogden et al. 2004 | Theodore et al. 2004 | Kudo et al. 2006 | Malay et al. 2006 | Gollwitzer et al. 2007 | |
| Study described as randomised? | Yes | Yes | Yes | Yes | Yes |
| If randomised, is the method described and appropriate? | Yes | Not clear | Yes | Yes | Yes |
| Study described as double blind? | Yes | Yes | Yes | Yes | Yes |
| If double blind, is the method described and appropriate? | Yes | Yes | Yes | Yes | Yes |
| Appropriate description of withdrawals and dropouts? | Yes | Yes | Yes | Yes | Yes |
| Study described as allocation concealment | Yes | Yes | Yes | Yes | Yes |
| If allocation concealment, is the method described and appropriate? | Yes | Not clear | Yes | Yes | Yes |
| Total score | 7 points | 5 points | 7 points | 7 points | 7 points |
| Table 4: Sensitivity and subgroup analysis. | ||||||
| No. of studies | Group; no. | Pheterogeneity | I2(%) | OR [95% CI] | ||
| HESWT | Placebo | |||||
| Analysis model | ||||||
| Fixed effects model | 5 | (119) 378 | (111) 338 | 0.31 | 16 | 2.25 [1.66, 3.06] |
| Random effects model | 5 | (119) 378 | (111) 338 | 0.31 | 16 | 2.26 [1.60, 3.21] |
| HESWT applied times | ||||||
| Single treatments | 4 | (188) 358 | (102) 318 | 0.23 | 31 | 2.31 [1.69, 3.18] |
| Triple treatments | 1 | (11) 20 | (9) 20 | Null | Null | 1.49 [0.43, 5.19] |
| Flux application | ||||||
| >0.3 mJ/mm2 | 2 | (66) 126 | 45 (125) | 0.23 | 30 | 1.99 [1.19, 3.32] |
| <0.3 mJ/mm2 | 2 | (78) 164 | 51 (161) | 0.64 | 1.97 [1.25, 3.10] | |
| Outcome | ||||||
| >50% decrease and VAS score <=4 cm | 2 | (122) 232 | (57) 193 | 0.12 | 58 | 2.54 [1.70, 3.81] |
| >60% decrease from baseline | 3 | (77) 146 | (54) 145 | 0.45 | 1.91 [1.19, 3.06] | |
Up to 90% of patients with PF will be cured within 6 months with conservative treatment. For the remaining 10%, with what was regarded as recalcitrant plantar fasciitis (RPF), the dispute is as to whether one should take HESWT or progress to surgery. The results of this meta-analysis provide strong evidence that HESWT is effective in the treatment of recalcitrant plantar fasciitis compared with placebo. According to our meta-analysis, 46.5% to 62.5% RPF patients achieved clinical success with HESWT after 12 weeks follow-up. Ogden [15] performed retreatment for the failure patients, and found that at 3 months, 22 of the 42 patients who received a second active treatment attained success. Actually, the effect of shockwave therapy seemed cumulative and time-dependent. Theodore [16] reported 94% success at 12 months follow-up while Wang reported 82.7% excellent or good pain and function scores at 60 to 72 months.
Subjective reports of pain as the primary outcome usually exhibit a large placebo effect and it seems typical in our included studies that success rates vary from 28.8% to 45.2% in the placebo group. However, in the nonblinded or single-blinded RCTs, the placebo group reported minimal improvement in pain scores, as compared with blinded studies [17, 18]. This large placebo effect demonstrates the effectiveness of the blinding technique, so nonblinded or single-blinded RCTs were excluded from our meta-analysis. There are two possible explanations for the relatively high success rates of placebo group: the self-limiting character of this disease or the placebo curative effect [19]. Partial PF patients take a turn for the better without any kind of special treatment; however, RPF patients do not experience any improvement when no intervention is applied [20]. For the placebo group, the recurrence rate was 38.1%–55% versus 3%–11% for the shockwave group [14, 21]. All of these suggest that the placebo treatment effect may play the main role in the high success rates in the placebo group. The unalloyed treatment effect and the associated placebo effect are not distinguishable and mingle to produce the clinical effect [22].
Compared with traditional treatment, HESWT is no more effective but more expensive [23, 24], but in contrast to surgery, HESWT is noninvasive, well-tolerated and a relatively inexpensive treatment. Patients return to daily life and most jobs within a short time. The main adverse events with HESWT for RPF included erythema, swelling of the local region and pain during treatment. The patients recover in several days after the treatment [16, 21].
However, many orthopaedists recommend surgery as a remedial measure after the failure of conservative treatment. The main reason is the conflicting results reported by different kinds of randomised controlled trials (RCTs) and the lack of homogeneity between these RCTs, which makes it unfeasible to combine these results in a meta-analysis and very difficult to make the final decision.
Meta-analysis of all the studies with ESWT compared with placebo is not feasible because significant heterogeneity between the studies precluded pooled analyses [25]. Heterogeneity between these studies is related to differences in study design, the method of shockwave generation (electrohydraulic, electromagnetic, piezoelectric or radial), the amount of shockwave energy delivered, the use of anaesthesia and sedation and the outcome measure. We included only high quality studies and focused on the HESWT in order to reduce the heterogeneity. As we mention above, satisfactory homogeneity between these trials make the conclusion of this meta-analysis stable and credible.
From all of our analysis above, we can conclude that HESWT is an effective treatment for RPF. We recommend HESWT as a remedial measure after failure of traditional conservative treatment and before of surgical intervention. RCTs will still be needed to compare the curative effect of HESWT with surgery in the treatment of recalcitrant plantar fasciitis.
1 Irving DB, Cook JL, Young MA, Menz HB. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskelet Disord. 2007;8:41.
2 Mahmood S, Huffman LK, Harris JG. Limb-length discrepancy as a cause of plantar fasciitis. J Am Podiatr Med Assoc. 2010;100(6):452–5.
3 Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for Plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003;85-A(5):872–7.
4 Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234–7.
5 Davis PF, Severud E, and Baxter DE. Painful heel syndrome: results of nonoperative treatment. Foot Ankle Int. 1994;15(10):531–5.
6 Healey K, and Chen K. Plantar fasciitis: current diagnostic modalities and treatments. Clin Podiatr Med Surg. 2010;27(3):369–80.
7 Thomas JL, Christensen JC, Kravitz SR, Mendicino RW, Schuberth JM, Vanore JV, et al. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010;49(3 Suppl):S1–19.
8 Chow IH, and Cheing GL. Comparison of different energy densities of extracorporeal shock wave therapy (ESWT) for the management of chronic heel pain. Clin Rehabil. 2007;21(2):131–41.
9 Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
10 Cosentino R, Falsetti P, Manca S, De Stefano R, Frati E, Frediani B, et al. Efficacy of extracorporeal shock wave treatment in calcaneal enthesophytosis. Ann Rheum Dis. 2001;60(11):1064–7.
11 Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. JAMA. 2002;288(11):1364–72.
12 Hammer DS, Adam F, Kreutz A, Kohn D, Seil R. Extracorporeal shock wave therapy (ESWT) in patients with chronic proximal plantar fasciitis: a 2-year follow-up. Foot Ankle Int. 2003;24(11):823–8.
13 Wang CJ, Chen HS, and Huang TW. Shockwave therapy for patients with plantar fasciitis: a one-year follow-up study. Foot Ankle Int. 2002;23(3):204–7.
14 Wang CJ, Wang FS, Yang KD, Weng LH, Ko JY. Long-term results of extracorporeal shockwave treatment for plantar fasciitis. Am J Sports Med. 2006;34(4):592–6.
15 Ogden JA, Alvarez RG, Levitt RL, Johnson JE, Marlow ME. Electrohydraulic high-energy shock-wave treatment for chronic plantar fasciitis. J Bone Joint Surg Am. 2004;86-A(10):2216–28.
16 Theodore GH, Buch M, Amendola A, Bachmann C, Fleming LL, Zingas C. Extracorporeal shockWave therapy for the treatment of plantar fasciitis. Foot Ankle Int, 2004, p. 290–297.
17 Cosentino R, Falsetti P, Manca S, De Stefano R, Frati E, Frediani B, et al. Efficacy of extracorporeal shock wave treatment in calcaneal enthesophytosis. Ann Rheum Dis. 2001;60(11):1064–7.
18 Mehra A, Zaman T, Jenkin AI. The use of a mobile lithotripter in the treatment of tennis elbow and plantar fasciitis. Surgeon. 2003;1(5):290–2.
19 Gerdesmeyer L, Frey C, Vester J, Maier M, Weil L Jr, Weil L Sr, et al. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med. 2008;36(11):2100–9.
20 Rompe JD, Hopf C, Nafe B, Burger R. Low-energy extracorporeal shock wave therapy for painful heel: a prospective controlled single-blind study. Arch Orthop Trauma Surg. 1996;115(2):75–9.
21 Ogden JA, Alvarez RG, Levitt RL, Johnson JE, Marlow ME. Electrohydraulic high-energy shock-wave treatment for chronic plantar fasciitis. J Bone Joint Surg Am. 2004;86-A(10):2216–28.
22 Nilsson G. Placebo effect is valuable. Add placebo effect to medical treatment outcome! Lakartidningen. 2011;108(44):2209–10.
23 Hammer DS, Adam F, Kreutz A, Kohn D, Seil R. Extracorporeal shock wave therapy (ESWT) in patients with chronic proximal plantar fasciitis: a 2-year follow-up. Foot Ankle Int. 2003;24(11):823–8.
24 Yucel I, Ozturan KE, Demiraran Y, Degirmenci E, Kaynak G. Comparison of high-dose extracorporeal shockwave therapy and intralesional corticosteroid injection in the treatment of plantar fasciitis. J Am Podiatr Med Assoc. 2010;100(2):105–10.
25 Rompe JD, Furia J, Weil L, Maffulli N. Shock wave therapy for chronic plantar fasciopathy. Br Med Bull. 2007;81-82:183–208.
26 Kudo P, Dainty K, Clarfield M, Coughlin L, Lavoie P, Lebrun C. Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. J Orthop Res. 2006;24(2):115–23.
27 Malay DS, Pressman MM, Assili A, Kline JT, York S, Buren B, et al. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg. 2006;45(4):196–210.
28 Gollwitzer H, Diehl P, von Korff A, Rahlfs VW, Gerdesmeyer L. Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg. 2007;46(5):348–57.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.