Comparison of the safety and effectiveness of endoscopic biliary decompression by nasobiliary catheter and plastic stent placement in acute obstructive cholangitis
DOI: https://doi.org/10.4414/smw.2013.13823
Ruling
Zhang, Li
Cheng, Xiaobo
Cai, Hang
Zhao, Feng
Zhu, Xinjian
Wan
Abstract
BACKGROUND: Endoscopic retrograde biliary drainage (ERBD) using a plastic stent is suggested to be as effective as endoscopic nasobiliary drainage (ENBD) with a nasobiliary catheter for temporary biliary drainage in acute obstructive cholangitis. However, there are few studies that have compared the two methods. We therefore compared the safety and effectiveness of endoscopic biliary decompression by nasobiliary catheter versus plastic stent placement in these patients.
METHODS: A total of 94 screened patients with acute obstructive cholangitis were randomised to undergo emergency endoscopic biliary drainage with ENBD (n = 47) or ERBD (n = 47). Clinical outcomes and adverse events were compared.
RESULTS: Patient backgrounds were similar in the two groups. Endoscopic biliary drainage was successfully achieved in all patients. Eleven patients underwent unscheduled endoscopic retrograde cholangiopancreatography (ERCP) to replace the nasobiliary catheter, 10 due to a catheter (1 in the ENBD group) or stent (9 in the ERBD group) blockage and 1 due to catheter migration. Clinical manifestations were similar, however, there was a significantly lower patient discomfort score in the ERBD group (p <0.05). The mean serum gamma-glutamyltransferase and total bilirubin concentrations after ERCP were significantly higher in the ERBD than ENBD group (p <0.001). Complication rates were similar in the ENBD and ERBD groups. However, the incidence rate of blockage in ERBD was statistically higher than ENBD (p = 0.015).
CONCLUSIONS: Endoscopic biliary decompression is an effective treatment for patients with acute obstructive cholangitis. In contrast to other studies, we found an increased rate of blockage in the ERBD group and a greater decrease in liver enzyme levels in the ENBD group.
Introduction
Acute obstructive cholangitis, especially suppurative cholangitis due to bile duct stones or biliary stricture, is an emergency situation that can cause septic shock and even death without prompt and appropriate therapy. Biliary drainage is the cornerstone of the treatment of acute cholangitis, which is achieved by means of endoscopic drainage, percutaneous transhepatic drainage and surgery. Although traditionally most patients with acute obstructive cholangitis undergo emergency surgery for urgent biliary drainage [1], emergency surgery in these patients is associated with significant morbidity and mortality rates owing to patient infirmity. Recent advances in endoscopic retrograde cholangiopancreatography (ERCP) have made the effective treatment of acute obstructive cholangitis in a minimally invasive manner possible [2]. Although stone extraction may not be feasible during an acute episode of obstructive cholangitis, endoscopic biliary decompression is effective and superior to surgical drainage as a temporary measure [3–6], with these patients later requiring a second elective ERCP or surgery for removal of bile duct stones.
Methods of endoscopic biliary drainage include endoscopic nasobiliary drainage (ENBD) and endoscopic retrograde biliary drainage (ERBD), with or without endoscopic sphincterotomy (EST). EST with stone extraction is considered to be the procedure of choice in patients with acute cholangitis. Endoscopic biliary drainage by nasobiliary catheter or biliary stent insertion is a simple and quick method for biliary decompression. ENBD is an external drainage procedure with the advantages of monitoring the bile, doing bile cultures and washing the catheter. However, patients with ENBD treatment will be uncomfortable because of the transnasal tube, and may even pull it out. ERBD is an internal drainage procedure with no discomfort and no loss of electrolytes or fluid. There are risks of occlusion and migration with both catheters and stents. Sphincterotomy may be performed to facilitate biliary drainage and cannulation of the bile duct. There have been a few studies that compared ERBD and ENBD in acute obstructive cholangitis [7–9], which showed that there was no difference in the safety and efficacy of endoscopic biliary drainage by nasobiliary catheter or blliary stent. However, stent occlusion is observed more frequently than nasobiliary catheter occlusion in our clinical experience. We therefore compared the safety and effectiveness of endoscopic biliary decompression by nasobiliary catheter with plastic stent placement in these patients in a randomised control trial.
Patients and methods
Patients
Between 2007 and 2010, a total of 94 patients with acute obstructive cholangitis secondary to choledocholithiasis or a bile duct benign stricture requiring emergency endoscopic biliary drainage were enrolled in the study after screening. It was a single-centre study and the patients were randomised, according to computer-generated numbers in sealed envelopes, to the ENBD group or the ERBD group. In the study, bile duct stones were not all cleared at time of initial ERCP in every patient because of severe inflammation of the bile duct or the poor condition of patients. Acute cholangitis was diagnosed in the presence of Charcot’s triad of abdominal pain, jaundice and fever, and abnormal liver biochemistry suggestive of biliary obstruction. Emergency drainage was indicated for patients with acute obstructive cholangitis secondary to choledocholithiasis or benign stricture of the common bile duct as follows: imaging methods showing evidence of bile duct obstruction and without obvious remission with antibiotic therapy. These patients often presented with progressive jaundice, right upper abdominal pain, unmanageable fever and even haemodynamic instability. Patients were excluded before randomisation with any one of the following: intrahepatic duct stones, a malignant stricture of the bile duct, sclerosing cholangitis, liver abscess, chronic liver disease including cirrhosis or other infectious diseases, and previous intervention at the papilla and bile duct.
All patients or their next of kin provided written informed consent for the procedures and treatment. The study protocol was approved by the ethics committee of our hospital.
ERCP and medicinal treatment
All ERCPs were performed by experienced endoscopists within 24 hours after the onset of acute obstructive cholangitis. Patients received diazemuls and meperidine for conscious sedation, with ERCPs performed using a conventional therapeutic duodenoscope (TJF-260V, Olympus, Japan) and standard procedures. EST was selected to be performed in patients with impacted bile duct stones or difficult cannulation. After cannulation of the common bile duct through the duodenal papilla, low-osmolar nonionic contrast medium was carefully injected to confirm the aetiology of cholangitis, the location of bile duct obstruction and the diameter of the bile duct. Patients randomised to the ERBD group or the ENBD group, respectively, underwent placement of the plastic stent (straight biliary stent, 8.5F, Wilson Cook Medical, Inc., USA) or cannulation with the nasobiliary catheter (pigtail nasal catheter, 7F and 5 side holes, Wilson Cook Medical, Inc., USA) through the obstruction. After the procedure, all patients were treated with intravenous antibiotics. It has been demonstrated that prophylactic treatment with somatostatin significantly reduced post-therapeutic ERCP pancreatitis [10–12]. Therefore, somatostatin was used for 24 hours to prevent post-ERCP pancreatitis in all patients. At the same time, the output from the nasobiliary catheter in the ENBD group was monitored. The nasobiliary catheter was aspirated continuously and not irrigated routinely. If the nasobiliary catheter or the stent became occluded with inadequate or no drainage, it was irrigated with metronidazole, or even replaced with a new catheter.
Outcome measures after ERCP
After the procedure, all patients were strictly observed for 7 days. The primary outcome measure was the serum total bilirubin level. The secondary outcome measures were clinical manifestations such as abdominal pain, fever, jaundice, leucocyte count, liver function tests (serum alanine transaminase [ALT], gamma-glutamyltransferase [GGT]), adverse events related to ERCP, and catheter (or stent) blockage or migration. Pancreatitis after ERCP is a clinical illness with typical pain associated with at least a three-fold increase in serum amylase (or lipase) at 24 hours, with symptoms impressive enough to require admission to hospital for treatment [13]. Procedure-related pancreatitis was resolved with conservative therapy including treatment with somatostatin. The immediate bleeding was not counted as a complication if it could be stopped by endoscopic manipulation during the procedure. Postprocedure bleeding was treated with endoscopic or interventional methods. Flushing or subsequent nasobiliary catheter replacement was utilised to alleviate inadequate drainage when blockage or migration occurred. In addition, the patients’ discomfort after the procedure was evaluated with a 10-cm visual analogue scoring system (0, no discomfort; 10, severe discomfort). The amount and the characteristics of the bile drained during nasobiliary drainage were monitored. After symptom relief, all patients underwent a second elective ERCP or surgery to remove bile duct stones.
Statistical analysis
All statistical analyses were performed with statistical software (SPSS 11.0). A two-sample t-test was used to test the hypothesis of equality of means. Categorical data were analysed with the Fisher's exact test. A p value <0.05 was considered statistically significant.
|
Table 1: Baseline demographic and clinical characteristics of the patients undergoing emergency ERCP. |
|
Characteristics
|
ENBD Group (n = 47)
|
ERBD Group (n = 47)
|
| Sex (M/F) |
28/19 |
31/16 |
| Age (y) (mean ± SD) |
56.8 ± 19.2 |
55.3 ± 17.1 |
| Clinical characteristics (n [%]) |
|
|
| Right upper quadrant pain |
45/47 (95.7) |
42/47 (89.4) |
| Fever |
38/47 (80.9) |
40/47 (85.1) |
| Jaundice |
21/47 (44.7) |
19/47 (40.4) |
| Confusion |
4/47 (8.5) |
6/47 (12.8) |
| Hypotension |
7/47 (14.9) |
8/47 (17) |
| Duration of symptoms (d) (mean ± SD) |
1.3 ± 0.7 |
1.5 ± 0.6 |
| Interval between admission and ERCP (h) (mean ± SD) |
4.8 ± 2.1 |
5.2 ± 1.8 |
| Body temperature before ERCP (°C) (mean ± SD) |
38.6 ± 1.7 |
38.2 ± 1.9 |
| Laboratory parameters (mean ± SD) |
|
|
| Total leucocyte count (109/l) |
15.8 ± 6.9 |
17.4 ± 5.8 |
| ALT (IU/l) |
121.4 ± 52.8 |
113.5 ± 48.2 |
| AST (IU/l) |
157.1 ± 62.3 |
166.9 ± 70.4 |
| GGT (IU/l) |
204.3 ± 71.1 |
213.8 ± 89.2 |
| Total bilirubin (µmol/l) |
58.1 ± 27.5 |
62.7 ± 32.9 |
| ALT = alanine aminotransferase; AST = aspartate aminotransferase; ENBD = endoscopic nasobiliary drainage; ERBD = endoscopic retrobiliary drainage; ERCP = endoscopic retrograde cholangiopancreatography; GGT = gamma-glutamyltransferase |
|
Table 2: Endoscopic findings in the ENBD and ERBD groups. |
|
Endoscopic findings
|
ENBD Group (n = 47)
|
ERBD Group (n = 47)
|
| Procedure time (min) (mean ± SD) |
22.5 ± 7.4 |
19.5 ± 8.1 |
| Endoscopic presentations (n [%]) |
|
|
| Impacted bile duct stones |
9/47 (19.1) |
7/47 (14.9) |
| Bile duct single stone |
31/47 (66.0) |
29/47 (61.7) |
| Bile duct multiple stones |
12/47 (25.5) |
15/47 (31.9) |
| Bile duct benign stricture |
4/47 (8.5) |
3/47 (6.4) |
| Purulent bile (n [%]) |
16/47 (34) |
14/47 (29.8) |
| EST (n [%]) |
10/47 (21.3) |
9/47 (19.1) |
| ENBD = endoscopic nasobiliary drainage; ERBD = endoscopic retrobiliary drainage; EST = endoscopic sphincterotomy |
Results
Characteristics of the enrolled patients
The demographic and clinical characteristics of the 94 patients with acute obstructive cholangitis are presented in table 1. The patients were randomised to two groups, the ERBD Group (n = 47) and the ENBD Group (n = 47). There were no significant differences between the groups for any parameter at baseline, with mean ± SD ages of the ENBD and ERBD groups of 56.8 ± 19.2 years and 55.3 ± 17.1 years, respectively. Most patients in the ENBD and ERBD groups presented with right upper quadrant pain (95.7% vs 89.4%) and fever (80.9% vs 85.1%), with 44.7% and 40.4%, respectively, presenting with jaundice. Approximately 10% and 15% of patients in both groups had mental confusion and hypotension. The mean ± SD duration of symptoms was 1.3 ± 0.7 days in the ENBD group and 1.5 ± 0.6 days in the ERBD group, with mean ± SD intervals between admission and ERCP of 4.8 ± 2.1 hours and 5.2 ± 1.8 hours, respectively. There was no between-group difference in total leucocyte count and liver function abnormalities.
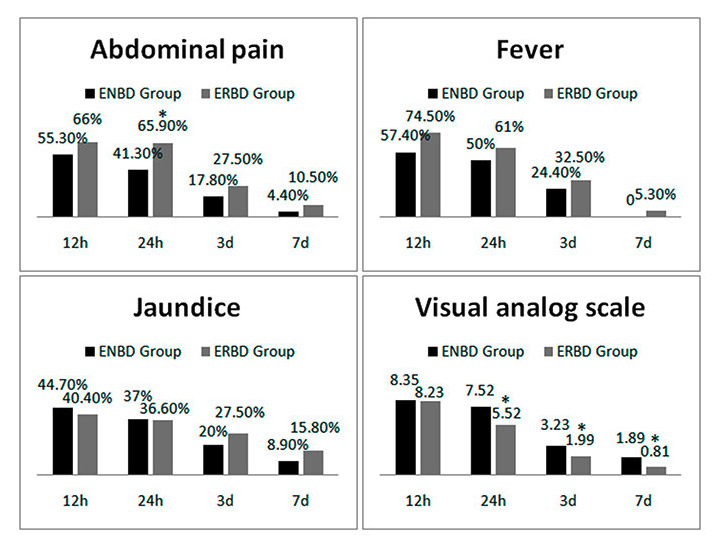
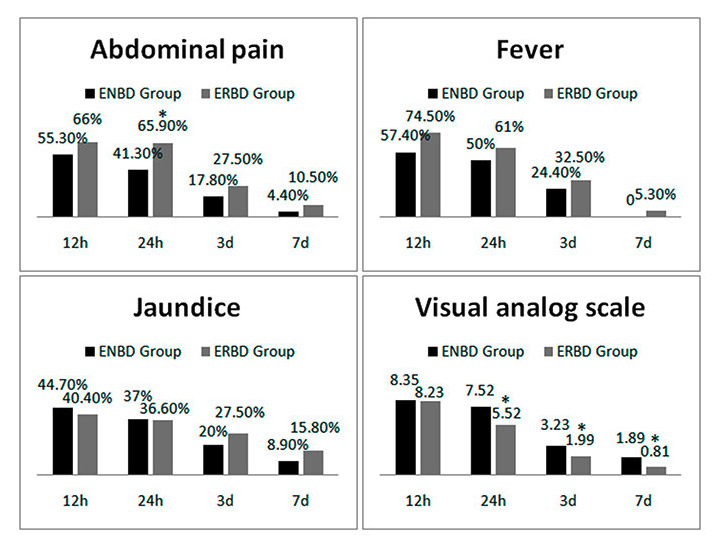
Figure 1
Rates of abdominal pain, fever and jaundice 12 hours, 24 hours, 3 days and 7 days after endoscopic retrograde cholangiopancreatography in the endoscopic nasobiliary drainage (ENBD) and endoscopic retrobiliary drainage (ERBD) groups.
* p <0.05 vs ENBD group.
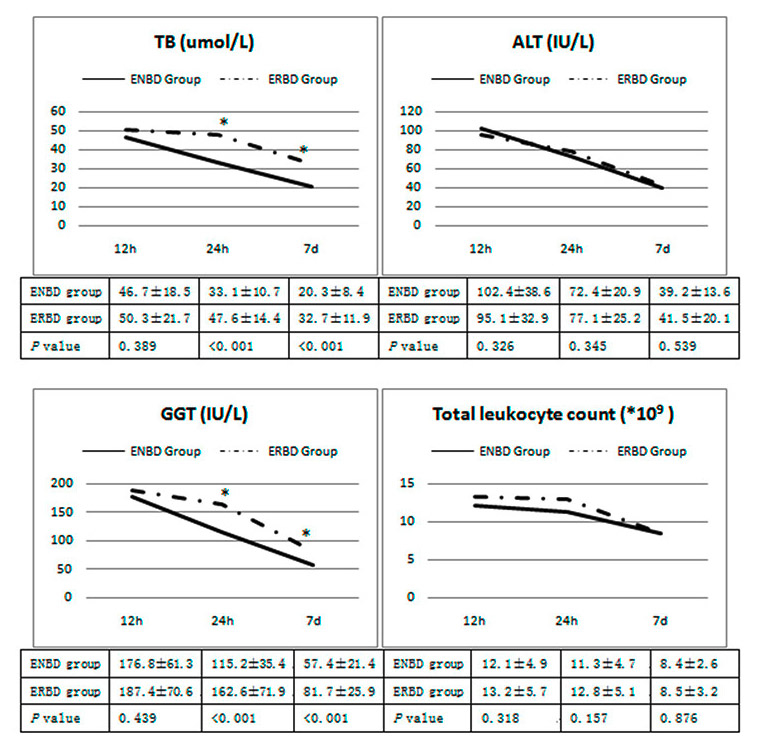
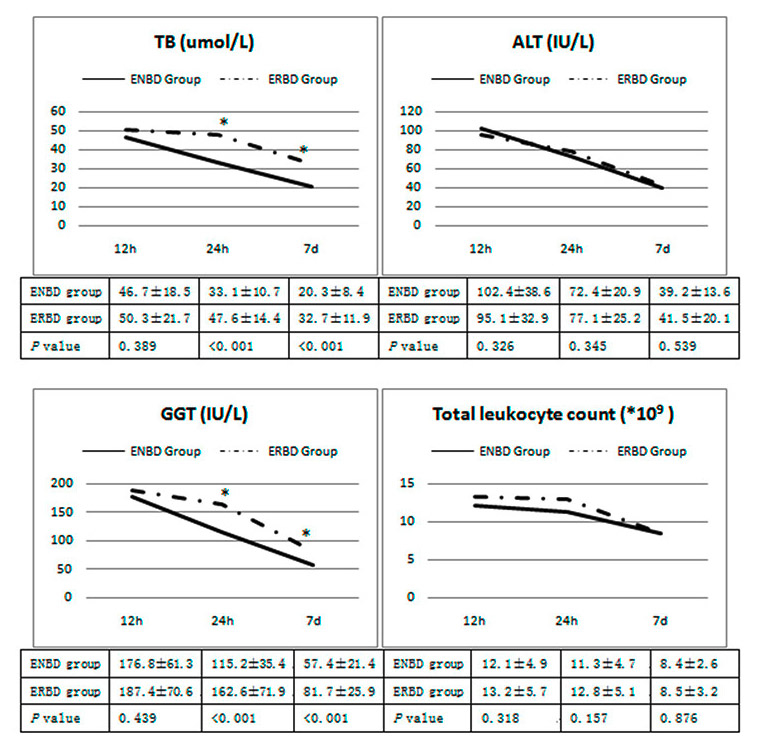
Figure 2
Total bilirubin (TB), alanine aminotransferase (ALT) and gamma-glutamyl transferase (GGT) concentrations and total leucocyte count 12 hours, 24 hours and 7 days after endoscopic retrograde cholangiopancreatography in the endoscopic nasobiliary drainage (ENBD) and endoscopic retrobiliary drainage (ERBD) groups.
* p <0.05 vs ENBD group.
Endoscopic findings
Endoscopic biliary decompression using a nasobiliary catheter or a plastic stent was successful in all 94 patients (100%). The mean ± SD procedure times were similar in the ENBD (22.5 ± 7.4 min) and ERBD (19.5 ± 8.1 min) groups. EST was performed in 19 patients, 10 patients in the ENBD group and 9 in the ERBD group. The most common cause of acute obstructive cholangitis was bile duct stones, with 66.0% in the ENBD and 61.7% in the ERBD group having a single stone in the bile duct, and 19.1% and 14.9%, respectively, of the ENBD group and ERBD groups having impacted stones. During ERCP, purulent bile drainage occurred in 34% and 29.8% of these patients, respectively. Overall, there was no significant difference in the endoscopic findings in the two groups (table 2).
Clinical outcomes after ERCP
Abdominal pain, fever, jaundice and laboratory parameters were improved within 7 days after ERCP treatment in both groups. All patients with mental confusion and hypotension in both groups became normal within 24 hours after drainage. Clinical and laboratory findings are compared in figures 1 and 2. Clinical manifestations were similar in the two groups, however, there was a significantly lower patient discomfort score in the ERBD group at 24 hours, 3 days and 7 days after the procedure (p <0.001, p = 0.004, p <0.001, respectively). The mean serum GGT and total bilirubin concentrations were significantly higher in the ERBD than in the ENBD group at 24 hours after ERCP (p <0.001) and at 7 days after ERCP (p <0.001), but no other outcomes differed significantly (fig. 2).
The nasobiliary catheter and the plastic stents became occluded by thick biliary sludge in seven patients, one in the ENBD and six in the ERBD group, all of whom had persistent fever 24 hours after the procedure with inadequate or no drainage. Three patients in the ERBD group developed a recurrent fever and abdominal pain at 3, 4 and 7 days, respectively, which was also due to stent occlusion. One patient in the ENBD group developed a recurrent fever 3 days after the first ERCP because of nasobiliary catheter migration. All these patients underwent an unscheduled ERCP to replace their nasobiliary catheters and plastic stents with new nasobiliary catheters.
Adverse events related to ERCP treatment
Although ERCP-related adverse events occurred in both groups, including bleeding and pancreatitis, their occurrence rates did not differ significantly (table 3). Five patients, three in the ENBD group and two in the ERBD group, experienced immediate bleeding during the procedure. Immediate bleeding was controlled in two patients by local injection of epinephrine and by thermocoagulation, and it stopped spontaneously in the other three patients. Within 7 days, two patients in the ENBD group developed delayed bleeding which was controlled, respectively, by endoscopic treatment with haemostatic clips and angiographic embolisation. There was no delayed bleeding complication in the ERBD group. Two patients in the ENBD and seven in the ERBD group developed pancreatitis, which resolved after conservative treatment. Blockage resulting from nasobiliary catheter or stent occlusion by thick biliary sludge occurred in one patient in the ENBD and nine in the ERBD group, and catheter migration occurred in one patient in the ENBD group. The incidence rate of blockage in ERBD (19.1%) was obviously higher than ENBD (2.1%) (p = 0.015). None of the 94 patients evaluated experienced a perforation complication and none died during the evaluation period.
|
Table 3: ERCP-related adverse events in the ENBD and ERBD groups. |
|
Comparisons
|
ENBD Group(n = 47)
|
ERBD Group (n = 47)
|
p-value
|
| Total occurrence rate (n [%]) |
9/47 (19.1) |
15/47 (31.9) |
0.237 |
| Immediate bleeding (n [%]) |
3/47 (6.4) |
2/47 (4.3) |
0.677 |
| Delayed bleeding (n [%]) |
2/47 (4.3) |
0/47 (0) |
0.495 |
| Pancreatitis (n [%]) |
2/47 (4.3) |
7/47 (14.9) |
0.158 |
| Blockage (n [%]) |
1/47 (2.1) |
9/47 (19.1) |
0.015 |
| Migration (n [%]) |
1/47 (2.1) |
0/47 (0) |
1.0 |
| ENBD = endoscopic nasobiliary drainage; ERBD = endoscopic retrobiliary drainage; ERCP = endoscopic retrograde cholangiopancreatography; |
Discussion
Acute cholangitis due to bile duct stones presents with a wide spectrum of severity, ranging from relatively mild cases to severe cases associated with hypotension and disturbed consciousness. Emergency drainage, as soon as possible, is essential for patients with moderate and mild disease if their condition has not improved with conservative treatment. Endoscopic drainage, ENBD or ERBD, is advocated whenever it is applicable because of the low morbidity rate and shorter duration of hospitalisation. Previous studies comparing ENBD and ERBD showed no significant difference in success rate, effectiveness, or morbidity [14]. However, one study revealed that the indwelling stent was associated with less post-procedure discomfort and avoided the potential problem of inadvertent removal of the nasobiliary catheter [7]. Another study showed that, with an EST, hyperamylasaemia was more frequent in the ERBD group than in the ENBD group [8].
We have compared the safety and effectiveness of endoscopic biliary decompression by nasobiliary catheter and plastic stent placement in patients with acute obstructive cholangitis. In agreement with previous findings, we found that ENBD or ERBD was effective for this condition. Clinical signs and symptoms, and laboratory parameters were improved within 7 days after ERCP treatment in both groups. However, we found that the mean serum concentrations of GGT and TB were significantly higher in the ERBD than in the ENBD group 24 hours and 7 days after endoscopic drainage, which showed that ENBD was more effective in regard to improvement of liver function. The exact mechanism causing the difference was unclear, but the improvement in biliary drainage by nasobiliary catheter aspiration and washing in the ENBD group was thought to be responsible. In addition, there was a significantly higher patient discomfort score in the ENBD group.
The overall complication rate in patients undergoing ERCP has been reported to be 4% [15], with complications depending on patient- and procedure-related factors. There was no significant difference in ERCP-related bleeding or pancreatitis between the two groups. The rate of post-ERCP pancreatitis was a little higher in the ERBD group, which seemed to be correlated with traumatic injury to the pancreatic duct and papilla. We found that the most important adverse events related to ERBD or ENBD were migration and blockage, because they reduced the effectiveness of the endoscopic biliary drainage and required an unexpected second ERCP. We observed that blockage resulting from nasobiliary catheter or stent occlusion by thick biliary sludge occurred in 2.1% of patients in the ENBD and 19.1% in the ERBD group, and catheter migration occurred in one patient in the ENBD group. Theoretically, a large 10F stent provides better drainage and a lower rate of stent occlusion for the thick infected bile than an 8.5F stent. However that fact does not seem to be so according to our clinical experience and previous studies. The previous studies showed no significant higher rate of stent occlusion both for a 10F stent and a 6F-7F stent [7–9]. The other reasons considered in selecting an 8.5F stent were as follows: the comparability to the nasobiliary catheter, easy operation and less trauma to the bile duct, especially in the stage of acute infection. The incidence rate of blockage in ERBD was obviously higher than ENBD, which were likely to be associated with vacuum aspiration and washing of the nasobiliary catheter. Therefore, if there is too much purulent bile, an ENBD is preferred to an ERBD, because the nasobiliary catheter can be flushed easily to prevent clogging and may be used for repeat cholangiography.
In conclusion, we have shown here that endoscopic nasobiliary drainage, ENBD or ERBD are effective for the treatment of patients with acute obstructive cholangitis. Absence of discomfort and no loss of electrolytes or fluid are advantages of ERBD. However, patients with ERBD are at significant risk for blockage, suggesting that this method should be used cautiously, especially in patients with too much purulent bile. Further research may be focused on the biliary stent optimisation to avoid the blockage.
Contributors: WXJ proposed the study. WXJ, ZF, ZH performed research. ZRL, CL and CXB analysed the data and wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts. WXJ was the guarantor.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.
References
1 Boey JH, Way LW. Acute cholangitis. Ann Surg. 1980;191:264–70.
2 Lai EC, Mok FP, Tan ES, et al. Endoscopic biliary drainage for severe acute cholangitis. N Engl J Med. 1992;326:1582–6.
3 Christoforidis E, Mantzoros I, Goulimaris I, et al. Endoscopic management strategies in relation to the severity of acute cholangitis. Surg Laparosc Endosc Percutan Tech. 2006;16:325–9.
4 Leung JW, Chung SC, Sung JJ, et al. Urgent endoscopic drainage for acute suppurative cholangitis. Lancet. 1989;1:1307–9.
5 Tsuyuguchi T, Takada T, Kawarada Y, et al. Techniques of biliary drainage for acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:35–45.
6 Nagino M, Takada T, Kawarada Y, et al. Methods and timing of biliary drainage for acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:68–77.
7 Lee DW, Chan AC, Lam YH, et al. Biliary decompression by nasobiliary catheter or biliary stent in acute suppurative cholangitis: a prospective randomized trial. Gastrointest Endosc. 2002;56:361–5.
8 Seon-Young Park, Chang-Hwan Park, Sung-Bum Cho, et al. The safety and effectiveness of endoscopic biliary decompression by plastic stent placement in acute suppurative cholangitis compared with nasobiliary drainage. Gastrointest Endosc. 2008;68:1076–80.
9 Sharma BC, Kumar R, Agarwal N, et al. Endoscopic biliary drainage by nasobiliary drain or by stent placement in patients with acute cholangitis. Endoscopy. 2005;37:439–43.
10 Rudin D, Kiss A, Wetz RV, et al. Somatostatin and gabexate for post-endoscopic retrograde cholangiopancreatography pancreatitis prevention: meta-analysis of randomized placebo-controlled trials. J Gastroenterol Hepatol. 2007;22:977–83.
11 Lee KT, Lee DH, Yoo BM. The prophylactic effect of somatostatin on post-therapeutic endoscopic retrograde cholangiopancreatography pancreatitis: a randomized, multicenter controlled trial. Pancreas. 2008;37:445–8.
12 Omata F, Deshpande G, Tokuda Y, Takahashi O, et al. Meta-analysis: somatostatin or its long-acting analogue, octreotide, for prophylaxis against post-ERCP pancreatitis. J Gastroenterol. 2010;45:885–95.
13 Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–93.
14 Kumar R, Sharma BC, Singh J, et al. Endoscopic biliary drainage for severe acute cholangitis in biliary obstruction as a result of malignant and benign diseases. J Gastroenterol Hepatol. 2004;19:994–7.
15 Cotton PB, Garrow DA, Gallagher J, et al. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80–8.