Career after successful medical board examination in general practice – a cross-sectional survey
DOI: https://doi.org/10.4414/smw.2013.13839
Ryan
Tandjung, Oliver
Senn, Franz
Marty, Linda
Krauss, Thomas
Rosemann, Nina
Badertscher
Summary
QUESTION UNDER STUDY: Switzerland is facing a shortage of general practitioners (GPs). Knowledge of the factors influencing career choice is crucial for increasing the attractiveness of general practice. The aim of our study was to report the working conditions of recently certified GPs and the effect of vocational training in general practice on GP skills and knowledge, and economic skills. Furthermore, we recorded when GPs chose general practice as a career, as well as potential barriers to and facilitators of their decision.
METHODS: Study design: Cross-sectional survey with an online-based questionnaire. Study group: 1,133 physicians certified in general practice between the years 2000 and 2010.
RESULTS: The response rate was 40.6% (456); 426 (44.1% females) were included in further analysis. A total of 341 (80.0%) were currently working in general practice. Female GPs were significantly more often employed (rather than working independently), working part-time and in group practices. Fifty-two (12.2%) of the participants did not work in general practice although they had intended to earlier. The majority (54.3%) of the participants working as GPs decided to become a GP during their residency. Overall, 60.6% of all participants completed vocational training in a general practice, which significantly improved self-perceived general practice skills compared with their colleagues without such training.
CONCLUSIONS: Residency is a more important time-period than medical school for career decisions to become a GP. Attractive residency programmes must be developed to engage physicians in this vulnerable phase. The workplace settings of female GPs were significantly different from those ofmale GPs. Vocational training in general practice had a positive effect on self-perceived GP skills.
Background
Like most European countries, Switzerland is facing a shortage of physicians, particularly of general practitioners (GPs) [1]. The average age of Swiss GPs is between 55 and 60 years [2], and half of today’s 6,000 GPs and general internists will retire within the next 10 years. The Swiss Society of General Practitioners (SGAM) has been observing practice openings for several years (general internists as well as GPs). The average demand for 250–300 more GPs per year between 2006–2010 contrasts with the fact that, overall, only 379 practices were opened in all these years [3, 4]. Furthermore, there is a substantial and unexplained gap between the numbers of board certifications in general practice and actual practice openings by GPs.
The low attractiveness of general practice has been reported in the international [5–12] and Swiss [13–17] literature. Many factors have been assessed, including financial incentives, workload, work environment, the role of general practice in medical schools and the lack of general practice experience during residency. Studies focusing on the career choices of medical students or residents in Switzerland revealed that the attractiveness of a career in general practice was very variable [14, 17–19]: the interest of medical students in a career in general practice was very low (9.7%) [17], whereas residents of clinics in internal medicine and surgery showed more interest (45%) [18]. All these studies assessed career intentions and not real decisions. In contrast, our study assessed real career decisions retrospectively by assessing GPs’ careers after their board certification.
The aim of our study was to report the working conditions of recently certified GPs. Furthermore, we recorded when GPs chose general practice as a career, and potential barriers to and facilitators of their decision. Residency is usually completed in a hospital, and in the ongoing political debate the importance of vocational training in general practice has been emphasised. We aimed to evaluate the effect of this training on self-perceived skills and knowledge.
Methods
Questionnaire
To create the questionnaire a literature review was undertaken of themes such as career in general practice and factors influencing the choice of medical specialty in an international setting and for Switzerland in particular. A German version with, overall, 28 multiple-choice questions was created. Prior to the start of the study, the German questionnaire was pilot-tested for comprehensibility by nine GPs and adapted accordingly. In addition, a French version of the questionnaire was created. Briefly, the questionnaire assessed the following characteristics: age, sex, medical school, year of graduation, current working conditions such as employment status (self-employment: investments, salary depending on revenues vs employed: fixed salary independent of revenues) and practice form, time of decision for or against a career in general practice, and participation in vocational training in general practice during residency. Self-perceived qualification regarding GP-specific knowledge, clinical and economic skills at the time the participant started working in a practice was assessed with three global questions (one for each dimension) on a Likert scale ranging from 1 (very bad) to 6 (very good).
Study population
In Switzerland, specialisation under 43 certified titles is possible; the number of physicians for a specific speciality is not regulated. Primary healthcare is mainly provided by general practitioners and general internists. In contrast to GPs, a substantial proportion of board-certified general internists primarily pursue a career as a specialist or work in a hospital. We only considered GPs representing the vast majority of physicians working in primary care.
Vocational training in general practice
Most of the training for future GPs takes place in hospital-based residencies, but in the late 1990s vocational training in general practice was introduced. The aim of this training programme was to teach specific aspects of general practice to future GPs. The teaching GPs are specially accredited by the medical board and have completed a didactic course. A minimum of 6 months of vocational training in general practice is recommended, but not mandatory, to achieve the medical board certification.
All physicians who received a diploma in general practice from Swiss Medical Board (FMH) between the years 2000 and 2010 were invited to participate. The postal addresses were provided by the Swiss Medical Board FMH. The invitations were sent by post with a link to the online survey, and a reminder was sent 5 weeks later. There were no financial incentives to participate in this study.
Statistics
Descriptive statistics are presented as mean (standard deviation [SD]) and frequencies. Sex comparisons have been performed for GPs career characteristics using t-tests and chi-squared statistics as appropriate. To investigate the effect of vocational training on self-perceived practical skills, unpaired t-test comparisons (vocational vs non-vocational training) were applied. A Cuzick’s trend test was used to test whether employment showed an association with years of board certification. A two-sided alpha level of 0.05 was assumed to indicate significance. We performed analyses using Stata® Version 12.1 (Stata Corporation, College Station, TX 77845, USA, http://www.stata.com )
Under Swiss ethics guidelines the study did not require formal ethics approval. Postal address data were linked to a code to coordinate the reminder letter. The codes together with any linked personal data were deleted before analyses to ensure anonymity of the participants.
Results
Data are presented in percentages and absolute numbers with the corresponding total number after the slash. A total of 1,133 physicians were eligible, 11 letters were undeliverable, and 456 physicians responded to the survey (participation rate 40.6%). When responders and nonresponders were compared, no differences were found for sex (p = 0.370), time since certification (p = 0.279) or age (p = 0.346). There was a significant difference (p <0.001) in language (according to the database of Swiss Medical Board FMH) and corresponding region within Switzerland, with a higher number of German- and Italian-speaking participants (German 42,3%, Italian 40.9%) than French-speaking participants (28.2%).

Figure 1
Employment of currently working general practitioners. (p <0.05 between the sexes).
x-axis: year of title received and sex of participants.
y-axis:the height of the bar represents the percentage of the participants that were currently working in general practice.
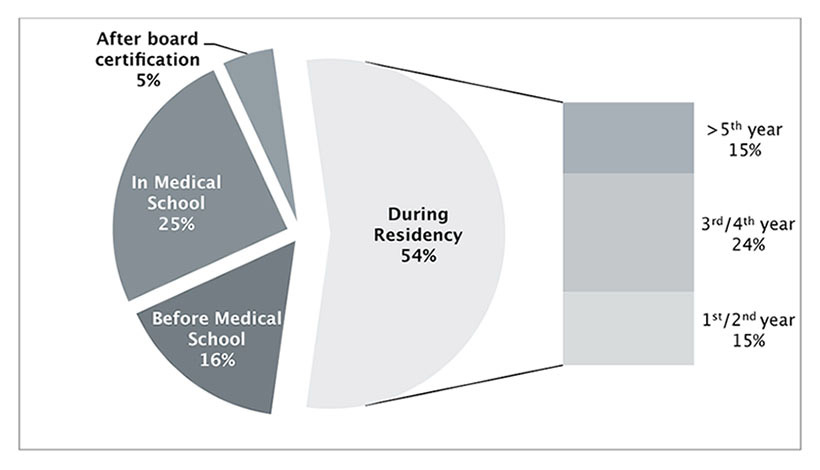
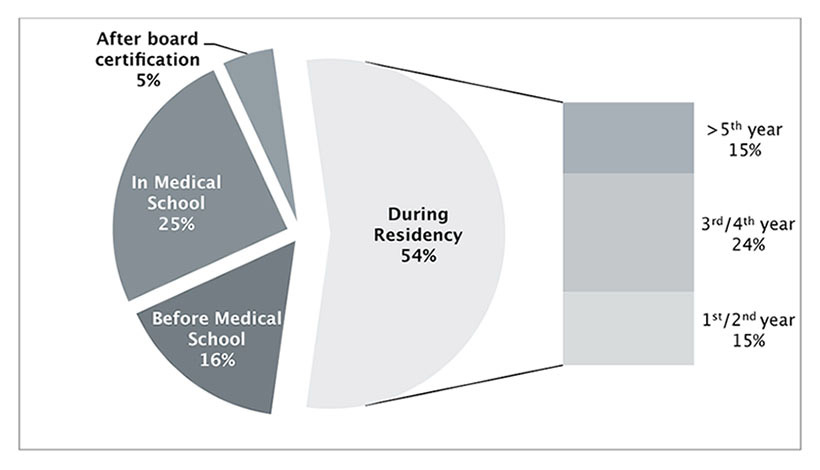
Figure 2
Time of decision to become a general practioner.
Thirty participants were excluded because they achieved medical board certification in a different medical field or before 2000. Therefore, in our final analysis we included 426 answers. Of the 426 participants, 85.0% (362/426) answered the German version and 15.0% (64/426) the French version of the questionnaire; 54.7% (233/426) were male and 44.1% (188/426) were female (5 missing answers). The mean age was 44 years (range 34–60 yrs, SD 5.5 yrs). The mean year of university degree was 1996 (SD 4.69 yrs) without any difference between the sexes. Details are shown in table 1. Exactly 16.0% (68/426) graduated outside Switzerland, 60 from Germany. Attendance of the Swiss medical schools was distributed thus: 14.1% (60/426) from Basel, 16.9% (72/426) from Berne, 4.9% (21/426) from Geneva, 9.2% (39/426) from Lausanne and 37.1% (158/426) from Zurich; eight participants did not state their medical school.
Overall, 80.0% (341/426) of the physicians were currently working as GPs and 23 planned to take up work as a GP in the near future; 14.6% (62/426) were neither working as a GP nor intended to work as a GP in the future, even though 83.9% (52/62) initially intended to work as a GP.
Workplace characteristics of GPs
Detailed workplace characteristics of the 341 physicians currently working as a GP are presented in table 2. Reported workload was significantly higher for men than women. Women (35.8% [53/148]) were significantly (p <0.001) more likely to work 5 half-days or less a week than men (4.8% [9/188]). Overall, 28.7% (98/341) were working in a single-handed practice, 31.7% (108/341) were working in double-handed practice and 39.3% (134/341) were working in practice with more than two doctors. Women were significantly more likely to work in double-handed and group practices than men (p = 0.001).
Concerning employment: 77.1% (263/341) were working independently in a practice and 22.9% (78/341) were employed, 24.4% (19/78) by physicians, 62.8% (49/78) by a nonphysician organisation and 12.8% (10/78) by a mixed physician and nonphysician organisation. Women were significantly more often employed than men (p <0.001). Furthermore, in women a significant trend was observed towards more employment many years after graduation (p <0.001). No such trend was found in men (fig. 1).
We asked the participants working as GPs when they decided on a career in primary care: 53.7% (183/341) decided during residency; 15.8% (54/341) decided before entering medical school, 24.6% (84/341) during medical school and 4.7% (16/341) after their board certification (fig. 2). No difference was found between medical schools where the GPs graduated or over the observed time period. Four answers were missing. Details are shown in table 3.
Non-GPs
One fifth (20.0%; 85/426) of the participants were not working as GPs. Of these, 27.1% (23/85) stated their intention to work in a practice within 0–6 years (mean 2.85 years), 11.8% (10/85) never had the intention to work as a GP, but obtained the title for different reasons (e.g. working as a company medical officer or in the pharmaceutical industry) and 12.2% (52/426) of the participants stated they had no further intention to work as a GP although they had earlier intended to do so. Of the latter group, 61.5% (32/52) changed their career goal after board certification and 30.8% (16/52) during residency (one during medical school, three missing answers). Several reasons were mentioned, most often a career in another medical field (28 times) and the incompatibility of family and professional life as a GP (17 participants; 10 female, 7 male). Fifteen participants regarded the investment as too high. The temporary practice stop – a federal law restricting the opening of private practices from 2002 to 2011 – was mentioned by 19.3% (10/52) as a reason against following a GP career.
Vocational training in general practice
Overall, 60.6% (258/426) completed vocational training in general practice during their residency. No significant differences in age, sex or medical school were found between the two groups who did or did not complete vocational training in general practice.
Three hundred and sixty-four participants were either already working as GPs (n = 341) or planned to work as GPs (n = 23). Fifty-two abandoned their earlier career goal to become a GP. We compared those two groups. In both groups a high percentage (55.8% non-GPs vs 62.3% GPs) completed vocational training in general practice (p = 0.369 between groups).
Overall self-perception of general practice knowledge (mean score 4.45, SD 0.90) and general practice skills (mean score 4.32, SD 0.97) was high, whereas perception of the economic skills needed to manage a private practice (mean 2.61, SD 1.25) were low. We compared participants who completed vocational training in general practice with those without such training. Regarding clinical general practice skills, the group with vocational training in general practice scored significantly (p = 0.003) higher with a mean of 4.47 (SD 0.93) compared with a mean of 4.07 (SD 0.97) in the group without specific training in general practice. We did not find a significant difference between the two groups for general practice knowledge (p = 0.235) or economic skills needed to manage a private practice (p = 0.063)
|
Table 1:Participants. |
|
|
Male (n = 233)
|
Female (n = 188)
|
p-value difference
|
| Age (years) |
44.2 (5.23) |
43.2(5.82) |
0.080 |
| Years since graduation |
15.6 (4.71) |
15.5 (4.68) |
0.553 |
| Years since medical board certification |
7.1 (3.07) |
6.5 (83.3) |
0.154 |
| Figures represent mean (standard deviation) |
|
Table 2:Workplace settings of participants currently working as general practitioners. |
|
|
Male (n = 188)
|
Female (n = 148)
|
p-value difference
|
| Age |
43.9 (5.23) |
42.8 (5.66) |
0.077 |
| Average workload in half-days |
8.81 (1.6) |
6.29 (2.03) |
<0.001 |
| Group practice |
59 (31.6%) |
75 (50.7%) |
<0.001 |
| Employed |
23 (12.2%) |
55 (37.2%) |
<0.001 |
| Figures for age and workload represent mean (standard deviation); figures for practice size and employment represent absolute numbers and percentages |
|
Table 3: Decision time to become a GP according to medical school where the participants graduated. |
| |
Basel
n = 49
|
Berne
n = 64
|
Geneva
n = 18
|
Lausanne
n = 29
|
Zurich
n = 122
|
Other
n = 50
|
Total
n = 332
|
| Before medical school |
12.2% |
15.6% |
16.7% |
17.2% |
18.0% |
12.0% |
15.6% |
| During medical school |
16.3% |
26.6% |
33.3% |
20.7% |
30.3% |
18.0% |
25.0% |
| During residency |
65.3% |
50.0% |
44.4% |
62.0% |
47.5% |
66.0% |
54.5% |
| After title obtained |
6.1% |
7.8% |
5.6% |
0.0% |
4.1% |
4.0% |
4.8% |
| No differences were observed between medical schools |
Discussion
Decision for a career in primary care
The most important and interesting finding of our retrospective survey among board-certified GPs was that residency was much more important when choosing a medical specialty than medical school. This confirms prior findings showing that the interest in general practice as a medical specialty is higher among residents than among medical students.
The greater significance of residency than medical school in the choice of a career has been shown in a Swiss cohort of physicians in the German speaking part of Switzerland [13]. The low interest of Swiss medical students in becoming GPs [17] and higher number of residents in surgery and medicine (45% of participants) considering a career in general practice [18] might reflect a similar finding. Traditionally, the role of general practice in medical school has been very small. But newer teaching concepts have recently been introduced in medical schools, for example in Basel 1997, with a one-on-one tutorial in general practice [20]. Other medical schools followed later: Zurich introduced tutorials in general practice in 2007. In our study, the comparison over time or between medical schools showed no significant difference: there was no measurable direct influence on the time of decision.
In our study sample, 12.2% of the participants did not work as GPs after they obtained the title although they had intended to earlier. The most frequent reason for leaving the career path of a GP was a more interesting, different medical field. Often the more structured programme, the security of employment while pursuing residency and financially brighter prospects are more attractive than a self-structured programme with certain financial and planning uncertainties. Both the general shortage of physicians and the fact that with the new specialty title in general internal medicine [21] more physicians are qualified to pursue an internal medicine subspecialty such as cardiology; therefore, these issues might contribute to fewer GPs. Additionally, attractive workplace settings for GPs, and attractive structured and financed residency programmes for future GPs, should be implemented. Attractive GP programmes offer a broad clinical content tailored for general practice, coordinated in successive rotations. Short-term residencies (e.g. 6 months) are often not feasible for the hiring clinics and, therefore, difficult to obtain, and several short-term residencies are difficult to coordinate. For the residents this implies either a narrower medical spectrum, a prolonged residency or other organisational challenges (e.g. not directly consecutive residencies or residencies in different geographical regions). Financial incentives for the hiring clinics, with copayments that enable short-term residencies in different medical specialties (e.g. dermatology or otorhinolaryngology) at one hospital might be a viable solution to these problems [22].
The new GPs
The workplace conditions of female and male GPs were significantly different: female GPs were more likely to work part-time, be employed and work in group-practices. It is not surprising that the proportion of female GPs working part-time was much higher than that of men. Nevertheless, this finding has substantial implications for the future of general practice in Switzerland. Although in our study sample the majority were male, the proportion will most likely change in the future: the majority of current medical students are female. Female students and residents are, for many reasons, more likely to choose general practice as their specialty [11, 13, 23]. Furthermore, the combination of self-employment in a single-handed practice and part-time work is hardly feasible. New practice models, such as group-practices, that allow future GPs to be employed and work part-time might help to recruit future (female) GPs, thus counteracting the impending shortage of GPs.
Vocational training in general practice
In Switzerland, there is not much known about the impact of vocational training in general practice. Compared with other European countries [24, 25], specific vocational training in an outpatient setting has a minor role in Switzerland. Nevertheless, a substantial number of our participants have completed vocational training in general practice. We could demonstrate a significant and positive effect of the training on the self-perceived GP skills. Interestingly, the training had no significant influence on the final workplace of the participants. This contrasts with the assumption that vocational training in general practice helps to recruit future GPs. The role of vocational training in general practice might be more to optimise the quality of care by future GPs. We assumed that vocational training in general practice would also increase the economic skills needed to manage a private practice. Interestingly, this assumption has not been confirmed, since no difference could be observed between GPs with and without participation in such vocational training. Taking into account the increasing economic burden on general practices because of decreasing financial resources in the healthcare system, this finding emphasises the importance of special qualification offers for residents interested in general practice. It could also be hypothesised that the increasing economic challenges of general practice, in combination with a self-perceived lack of specific knowledge, forces young GPs to become employed.
Strength and Limitations
In this study we showed where physicians after board certification in general medicine were actually working, rather than displaying future intentions. The response rate of 40.6% – given that there were no incentives and considering the high workload of general practitioners – was higher than can be expected [26]. As far as a comparison between nonresponders and responders was possible, no significant differences were found in age, year of board certification and sex. Our response rate was higher in the German-speaking part than in the French-speaking part of Switzerland, possibly because the study centre is in the German-speaking part. We compared the two subgroups of German and French responders and did not find any differences in working conditions (specifically more part-time working by females), time of career decision, age and sex distribution, and assume that generalisability is not limited by the lower response rate in the French part of Switzerland. A significant difference was found in employment (p <0.001), with a lower proportion in the French-speaking responders being employed compared with the German responders. Differences in forms of practice organisation might be an explanation for this result. Group practices (insurance companies, trust companies, networks) are much less common in the French part than in the German-speaking part. The study sample only included GPs representing the vast majority of physicians working in general practice. We are aware that general internists form a relevant part of the workforce in primary care. However, in contrast to GPs, a substantial proportion of board-certified general internists primarily pursue a career as specialists or do not work in ambulatory care; thus, pooling the two medical specialities would have resulted in a very heterogeneous group. A further survey focusing on the careers and workplace settings of board-certified general internists is planned at the current author’s institution.
Conclusions
Residency is a much more important time-period for choice of a certain medical speciality than medical school. Attractive structured residency programmes have to be developed to engage physicians in this vulnerable phase. The workplace settings of female GPs are significantly different from those of male GPs; female GPs were more often employed and were more likely to work part-time and in a group practice. Vocational training in general practice influenced on self-perceived GP skills, but not on whether the board certified GP finally really worked in general practice.
References
1 OECD. OECD Reviews of Health Systems Switzerland accessed online [http://www.oecd.org/switzerland/oecdreviewsofhealthsystems-switzerland.htm]. 2011.
2 FMH SÄ. Ärztestatistik Schweiz – online Abfrage am 05. August 2011 auf http://aerztestatistik.myfmh2.fmh.ch/. 2011.
3 Marty F. Praxisbarometer 2010. Primary Care. 2011;11:135–6.
4 Marty F, Zemp N. Titelverleihungen Fachärztin/Facharzt FMH für Allgemeinmedizin 2009. Primary Care. 2010;10:149–50.
5 Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med. 2010;85:S81–8.
6 Maiorova T, Stevens F, van der Zee J, Boode B, Scherpbier A. Shortage in general practice despite the feminisation of the medical workforce: a seeming paradox? A cohort study. Bmc Health Serv Res. 2008;8:262.
7 Morra DJ, Regehr G, Ginsburg S. Medical students, money, and career selection: students’ perception of financial factors and remuneration in family medicine. Fam Med. 2009;41:105–10.
8 Newton DA, Grayson MS. Trends in career choice by US medical school graduates. JAMA. 2003;290:1179–82.
9 Scott I, Gowans M, Wright B, Brenneis F, Banner S, Boone J. Determinants of choosing a career in family medicine. CMAJ. 2011;183:E1–8.
10 Senf JH, Campos-Outcalt D, Kutob R. Factors related to the choice of family medicine: a reassessment and literature review. J Am Board Fam Pract. 2003;16:502–12.
11 Shadbolt N, Bunker J. Choosing general practice – a review of career choice determinants. Aust Fam Physician. 2009;38:53–5.
12 Sinclair HK, Ritchie LD, Lee AJ. A future career in general practice? A longitudinal study of medical students and pre-registration house officers. Eur J Gen Pract. 2006;12:120–7.
13 Buddeberg-Fischer B, Klaghofer R, Abel T, Buddeberg C. Swiss residents’ speciality choices – impact of gender, personality traits, career motivation and life goals. Bmc Health Serv Res. 2006;6.
14 Buddeberg-Fischer B, Klaghofer R, Stamm M, et al. Primary care in Switzerland no longer attractive for young physicians? (vol 136, pg 416, 2006). Swiss Med Wkly. 2006;136:520–.
15 Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. The new generation of family physicians – career motivation, life goals and work-life balance. Swiss Med Wkly. 2008;138:305–12.
16 Gnadinger M. The new generation of family physicians – career motivation, life goals and work-life balance. Swiss Med Wkly. 2008;138:618; author reply
17 Halter U, Tschudi P, Bally K, Isler R. Berufsziel von Medizinstudierenden. Primary Care. 2005;5:468–72.
18 Badertscher N, Schoni M, Berger L, Zoller M, Rosemann T. Vocational training of future GPs in Swiss hospitals: the view of assistant physicians. Praxis. (Bern 1994) 2011;100:349–55.
19 Badertscher N, Schoni M, Zoller M, Rosemann T. Vocational training of future GPs in Swiss hospitals: the view of chief physicians. Praxis. (Bern 1994) 2011;100:781–5.
20 Isler R, Romerio S, Halter U, et al. One-on-one long-term tutorials in general practitioners’ practices – a successful new teaching concept in primary care medicine. Swiss Med Wkly. 2009;139:161–5.
21 Bauer W, Hänggeli C. Eine neue Epoche: das Weiterbildungsprogramm Allgemeine Innere Medizin. Schweizerische Ärztezeitung. 2010;91:1929–32.
22 Rosemann T, Bandi-Ott E, Tandjung R. Das Curriculum für Hausarztmedizin am USZ – eine Erfolgsgeschichte. Schweizerische Ärztezeitung. 2012;93:1432–3.
23 Gedrose B, Wonneberger C, Junger J, et al. Do female medical graduates have different views on professional work and workload compared to their male colleagues? Results of a multicenter postal survey in Germany. Deut Med Wochenschr. 2012;137:1242–7.
24 EURACT EAoTiGPFM. Survey on Specialist Training in General Practice / Family Medicine, dynamic interactive database [http://www.euract.eu/resources/specialist-training], accessed online Nov 23rd 2012. 2009.
25 RCGP RCoGP. GP curriculum, accessed online Nov 23rd 2012 on [http://www.rcgp.org.uk/gp-training-and-exams/gp-curriculum-overview.aspx]. 2012.
26 McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732–3; discussion 3–4.