Competency in interpretation of the 12-lead electrocardiogram among Swiss doctors
DOI: https://doi.org/10.4414/smw.2013.13806
Jean Jacques
Goy, Jürg
Schlaepfer, Jean-Christophe
Stauffer
Physicians of all specialties and levels of training frequently make errors in interpreting 12-lead electrocardiograms (ECGs). Some studies have shown that noncardiologist physicians make more ECG interpretation errors than do cardiologists [1]. There have been many proposals to optimise training, testing and competency in interpretation of ECGs. However, despite several earlier consensus-based recommendations regarding ECG interpretation, substantive evidence on the training needed to obtain and maintain ECG interpretation skills is not available. Previous recommendations proposed to improve ECG knowledge are not derived from clinical practice or clinical trials [2]. Recently, computerised interpretation and computerised ECG databases have been tested and shown to decrease the number of false ECG interpretations by up to 29% [3, 4]. However, these have shown less accuracy than physician interpreters and must be relied upon only as an adjunct interpretation tool for trained providers. Interpretation of ECGs varies greatly even among expert electrocardiographers. Noncardiologists seem to be more influenced by patient history when interpreting ECGs. Cardiologists appear to perform better than other specialists in standardised ECG examinations when minimal patient history is provided.
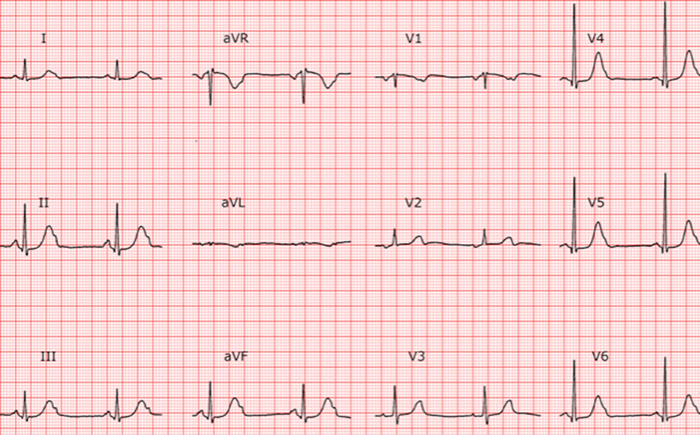
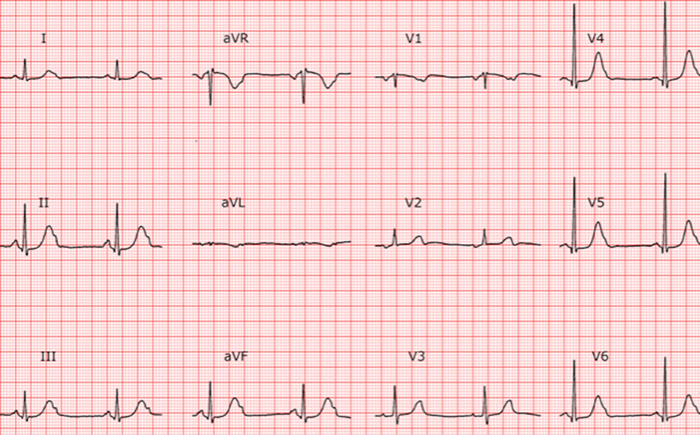
Figure
One ECG from the survey. Description and MCQ are provided before voting. Diagnosis and comments are given after the vote.
Description:
Basic rhythm: sinus rhythm, regular at 50 bpm.
P waves: normal, but every second wave is blocked.
PR interval: normal.
QRS: normal duration, increased amplitude from V4 to V6, normal axis.
ST segment: isoelectric.
T waves: normal.
QT interval: prolonged (510 ms).
MCQ:
1. Normal sinus rhythm
2. Second degree AV block
3. Long QT syndrome and second degree AV block
4. Long QT syndrome
5. U wave and normal sinus rhythm
Diagnosis:Congenital long QT syndrome with functional 2:1 AV block. (Number 3)
Comments: The long QT syndrome prolongs the refractory phase of the AV conduction pathways, which explains why a portion of the P waves (which are clearly visible on the descending portion of the T wave) is blocked. In the time it takes for the next excitation to occur, the conduction pathways have completed the refractory phase and the atrioventricular sequence returns to normal. The P waves are not completely regular, since the PP interval with a QRS complex is slightly shorter than the PP interval without a QRS complex. This is owing to an ill-explained phenomenon called “ventriculophasic variation”.
We tried to understand better the level of knowledge of ECG interpretation of Swiss doctors through the use of an Internet survey. Every 2 weeks a 12-lead ECG was submitted to physicians via an Internet platform exclusively reserved for physicians. A team of three cardiologists chose test ECGs representing daily practice (exceptional or very difficult ECGs were excluded). A short medical history and a description of the ECG were provided. Physicians had to choose independently the correct answer in a multiple-choice question (MCQ) system (fig.). During a 26-month period, 63 traces were submitted. Because the answer had to be given using an MCQ, the expected correct answer score was estimated at approximately 66% (two-thirds of the number of participants). Internists and general practitioners represented 60% of the participants, intensivists 18%, anaesthetists 16% and various other specialists 6%. The mean number of participants was 161 (range 60 to 240). Overall (all groups of specialists and ECG categories combined), the mean number of correct answers was only 31% (range 8 to 76%). Even if we accept the limitations of an internet survey analysis, the percentage of correct answers is dramatically low and worrisome. ECG, the simplest and oldest medical paraclinical test, is still poorly interpreted, at least by physicians practicing in Switzerland, with possible impact on patient outcomes. This test represents a picture of the situation in Swiss hospitals.
We suggest that medical schools, hospitals and medical societies become aware of this problem and spend more time on ECG training, rather than teaching other esoteric specialties. Pending more definitive research, residency training in internal medicine should be improved, at least in Switzerland, to ensure proficiency in the bedside interpretation of 12-lead ECGs in routine and emergency situations. The value of an internet platform as a teaching tool has not been extensively tested or compared with conventional ways of learning ECG interpretation. Our goal was not to teach ECG interpretation, but rather to give the participants the opportunity to check their level of knowledge (continuous formation).
References
1 Competency in interpretation of 12-lead electrocardiograms: a summary and appraisal of published evidence. Salerno SM, Alguire PC, Waxman HS. Ann Intern Med. 2003;138(9):751–60.
2 Recommandations for the standardization and interpretation of the electrocardiogram. Mason JW, Hancock EW, Gettes LS. Circulation. 2007;115:1325–32.
3 Automated serial ECG comparison improves computerized interpretation of 12-lead ECG. Gregg RE, Deluca DC, Chien CH, Helfenbein ED, Ariet M. J Electrocardiol. 2012;45:561–5.
4 The Moli-Sani project: computerized ECG database in a population-based cohort study. J Electrocardiol. 2012;45:684–9.