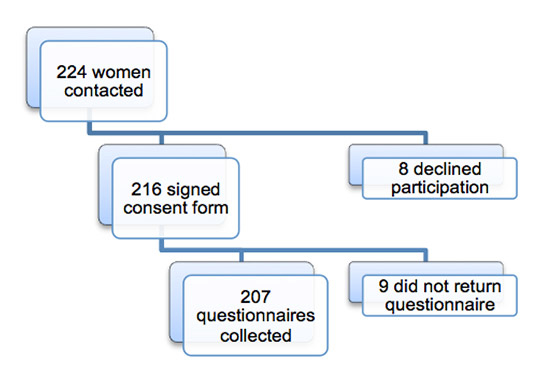
Figure 1
Inclusion of the study patients.
DOI: https://doi.org/10.4414/smw.2013.13795
Foetal exposure to maternal smoking leads to perinatal complications and may also have adverse long-term effects on children’s health [1]. In addition, maternal smoking increases the risk of miscarriage, ectopic pregnancy, premature birth, placenta praevia and premature rupture of membranes [1]. Birth weight is also influenced: a mean decrease of 377 g has been reported for children born to mothers who smoked. Low birth weight is associated with long-term consequences including an increased risk of developing coronary artery disease, arterial hypertension and insulin resistance in adulthood [1]. Independently, pregnant women’s exposure to close relatives’ tobacco smoking also leads to decreased birth weight [2, 3].
Over a hundred years ago, the harmful effects on the foetus of alcohol drinking by pregnant women were already known [4]. In 1968, a syndrome in the neonates born to alcoholic mothers was described in France, and in 1973 Jones et al. observed the same phenomenon and used the term “foetal alcohol syndrome” for the first time [5–7]. Since then, cognitive, behavioural and physical consequences have been proved to be related to foetal exposure to a high quantity of alcohol. These problems have been named “foetal alcohol spectrum disorder” [8]. The consequences of low to moderate maternal alcohol consumption are still debated, as the recent literature shows contradictory results [9]. Because there is no demonstrated threshold under which alcohol consumption is harmless, complete alcohol abstinence during pregnancy is recommended in many countries [10].
The objective of this study was to describe alcohol and tobacco consumption during pregnancy in women delivering in the maternity ward of the Geneva University Hospitals. We also aimed to explore risk factors related to tobacco and alcohol use during pregnancy, in particular the consumption habits of close relatives and their behaviour toward pregnant women.
We conducted a cross-sectional questionnaire survey after delivery using retrospective self-reports of smoking and alcohol drinking during pregnancy. The questionnaire (see appendix http://www.smw.ch/fileadmin/smw/pdf/Appendix/SMW_13795_Appendix.pdf ) was based on the authors’ experience and on a review of the literature. It was pretested in the maternity ward of the Geneva University Hospitals and in a private gynaecology practice to ensure clarity of content and acceptability to women. The study protocol was approved by the ethics committee of the Geneva University Hospitals. In order to obtain a precision of ± 4% to 6% for proportions contained between 10% and 30%, a sample size of 200 participants was required. Every woman giving birth in the maternity ward during a 3-week period (January and February, 2008) was eligible. During the phase of data collection, we went to the maternity ward twice a week and ensured we did not miss any woman by using official registers. About 230 women delivered during the period of data collection. The study was systematically presented to potential participants by one of the investigators, and every woman could decline participation without having to provide a justification. The questionnaire was anonymous, and we emphasised that data would be treated confidentially and not transmitted to the medical staff or to any third party. If a woman agreed to participate, she was asked to sign a consent form and was given the questionnaire and a blank envelope that we collected one hour later. The closed envelopes were mixed and opened later, making any matching with individuals impossible.
Questions covered sociodemographic characteristics, family situation, tobacco and alcohol consumption before and during pregnancy, and the smoking and drinking habits of close relatives. Some questions about alcohol and tobacco consumption before pregnancy were adapted from the 2002 Swiss Health Survey (obtained from the Swiss Federal Statistical Office) and the 2001–2006 Tobacco Monitoring Switzerland questionnaires (obtained from the Department of Psychology of the University of Zurich).
In the category “any smoking, even temporary use”, we included women who decreased, did not modify or increased their tobacco consumption during pregnancy, as well as those who quit smoking during pregnancy. In the category “continuing smoking”, we included women who smoked during the entire pregnancy. To determine the factors associated with the continuation of smoking when the woman got pregnant, we analysed the subgroup of participants who had smoked in the year before their pregnancy and used “continuing smoking” during the entire pregnancy as an outcome. The same process was used for alcohol. Binge drinking was defined as drinking four glasses or more on a single occasion, as is usually found in the literature [11].
The statistical analysis was performed using PASW Statistics version 18 (SPSS). We used chi-square tests to examine associations between categorical variables and defined statistical significance as p <0.05. We reported odds ratios (OR) and their 95% confidence intervals (95% CI). For continuous variables, we compared means and evaluated statistical significance using the Student’s t-test.
| Table 1:Baseline characteristics of the participants. Results are reported as n (%) or mean [standard deviation]. If unspecified, N = 207. | ||
| Mean age (years) | 31.20 | [5.068] |
| Swiss origin | 70 | (33.8) |
| French-speaking (most frequently used) | 152 | (73.4) |
| Familial situation (N = 206) | ||
| Lives with a husband/partner | 192 | (93.2) |
| Lives alone | 10 | (4.9) |
| Lives with relatives/others | 4 | (1.9) |
| Subjective estimation of income (N = 198) | ||
| Below average | 33 | (16.7) |
| Average | 153 | (77.3) |
| Above average | 12 | (6.1) |
| Salaried employment before delivery (even part-time) (N = 202) | 157 | (77.7) |
Consent and response rates were 96.4% and 95.8%, respectively (fig. 1). The 207 participants were between 15 and 43 years of age (mean 31.2 years; table 1). One-third of women were of Swiss origin. Almost all participants (93.2%) lived with a husband or partner. Ten percent of women consumed both tobacco and alcohol during pregnancy. Half the women (51.2%) abstained from any consumption of these products during pregnancy.
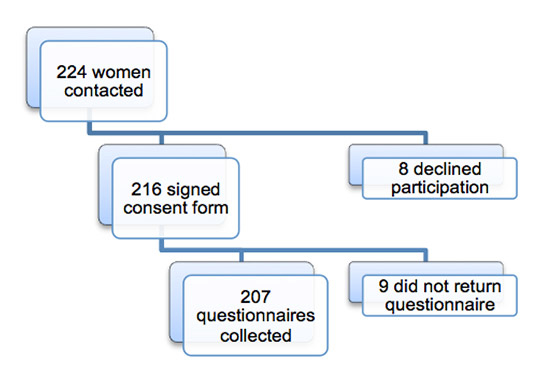
Figure 1
Inclusion of the study patients.
A third of the women (31.2%, 95% CI 24.8%–37.6%) had smoked during the year preceding their pregnancy (table 2). Most of them (91.5%) were encouraged by close relatives to decrease their smoking. The proportion of smokers decreased to 21.7% during pregnancy (95% CI 16.1%–27.3%). Fewer than half of the smokers (19/45, 9.2% of all participants, 95% CI 5.3%–13.1%) smoked continuously until delivery. Most (83.3%) felt guilty about smoking during their pregnancy and two-thirds tried to quit unsuccessfully. A third of women lived with a smoker. In about half the cases, this person made an effort to decrease his consumption or never smoked in the presence of the pregnant woman. The majority (85.1%) of participants had been informed about the risks of smoking during pregnancy. Fewer than half of the women (42.1%) received this information from their general practitioner or gynaecologist.
Employment status before delivery and the country of origin were not associated with smoking during pregnancy (table 3). Tobacco consumption was more frequent among pregnant women living with a smoker (40.0% vs 12.4%; OR 4.71, 95% CI 2.34–9.45), and among participants exposed directly to the smoke of other people (59.5% vs 19.4%; OR 6.11, 95% CI 2.02–18.48). Finally, the proportion of women who smoked during pregnancy was higher among participants who had drunk alcohol during the year before they became pregnant than among those who had not (27.0% vs 13.3%, p = 0.02), but smoking was not associated with drinking during pregnancy.
Among the 63 women who smoked, even occasionally, during the year preceding their pregnancy, some factors were associated with the continuation of smoking during the entire pregnancy. Women who did not succeed in quitting smoking during pregnancy were more likely to live alone (83.3% vs 24.6%; OR 15.36, 95%CI 1.65–142.84) and their close relatives were less likely to change their consumption (quitting or diminishing smoking: 13.0% vs 53.8%; OR 0.13, 95% CI 0.03‒0.66).
Most participants (62.7%, 95% CI 56.0%–69.4%) consumed alcohol (even occasionally) before they became pregnant (table 4). Just over half of these women drank one glass of alcohol or more during their pregnancy (36.3% of all participants, 95% CI 29.7%–42.9%). Among the 73 women who reported drinking alcohol during pregnancy, eight women reported at least one episode of binge drinking (3.9% of all participants). The women who drank alcohol were encouraged by people around them to decrease their consumption in 40.9% of cases. Fewer than a quarter of the women felt guilty about their alcohol consumption. The majority of participants (70.7%) had a husband/partner who drank alcohol. Husbands/partners made an effort to decrease their consumption in about a quarter of cases (26.1%). Nearly half the women were offered alcohol at least once by someone aware of their pregnancy. Most participants (86.1%) had been informed about the risks of drinking during pregnancy. Fewer than half (44.1%) received this information from their general practitioner or gynaecologist.
We did not observe any difference in age, country of origin, language, marital status, household income or tobacco consumption between women who drank alcohol during their pregnancy and those who were abstinent (see table 3). However, alcohol consumption was more frequent among pregnant women whose husband/partner was an alcohol consumer (44.6% vs 19.6%; OR 3.30, 95% CI 1.53–7.15). Participants who were offered alcohol by someone aware of their pregnancy were also more prone to drink alcohol (47.9% vs 25.5%; OR 2.69, 95% CI 1.48–4.90).
In women who had consumed alcohol during the year preceding their pregnancy, we did not find any association between continuation of drinking during pregnancy and the other variables.
| Table 2: Descriptive statistics for tobacco consumption. Results are reported as n (%) or mean [standard deviation]. If unspecified, N = 207. | ||
| Smoking during the year preceding pregnancy (even occasional) (N = 202) | 63 | (31.2) |
| Encouragement to diminish smoking from people around (N = 59) | 54 | (91.5) |
| Smoking during pregnancy, even temporary use (any smoking, even temporary use) | 45 | (21.7) |
| Smoking during the entire pregnancy (continuing smoking) | 19 | (9.2) |
| Daily consumption (N = 18) | 13 | (72.2) |
| Number of cigarettes smoked per day (N = 14) | 7.93 | [4.178] |
| Feeling guilty about smoking during pregnancy (N = 18) | 15 | (83.3) |
| Unsuccessful attempt to quit smoking (N = 18) | 12 | (66.7) |
| Lives with a smoker | 70 | (33.8) |
| This person (N = 70) | ||
| Quitted smoking | 4 | (5.7) |
| Diminished smoking | 35 | (50.0) |
| Did not change his consumption | 31 | (44.3) |
| This person smoked in the presence of the pregnant woman (N = 68) | ||
| Often | 9 | (13.2) |
| Sometimes | 28 | (41.2) |
| Never | 31 | (45.6) |
| Had been informed about the risks of smoking during pregnancy (N = 202) | 172 | (85.1) |
| Through (multiple answers possible) | ||
| Media | 131 | (64.9) |
| General practitioner / gynaecologist | 85 | (42.1) |
| Poster campaign | 83 | (41.1) |
| People around | 68 | (33.7) |
| Other | 19 | (9.4) |
| Table 3:Factors influencing tobacco and alcohol consumption during pregnancy. If unspecified, N = 207. | |||||||||
| Any smoking, even temporary use1 | Continuing smoking2 | Alcohol consumption | |||||||
| n (%) | p value | N | n (%) | pvalue | N | n (%) | pvalue | N | |
| Origin | |||||||||
| Swiss | 20 (28.6) | 0.088 | 8 (11.4) | 0.423 | 27 (39.7) | 0.475 | 201 | ||
| Other | 25 (18.2) | 11 (8.0) | 46 (34.6) | ||||||
| Language (most frequently used) | |||||||||
| French | 40 (26.3) | 0.008 | 18 (11.8) | 0.027 | 58 (38.9) | 0.193 | 201 | ||
| Other | 5 (9.1) | 1 (1.8) | 15 (28.8) | ||||||
| Lives with a husband/partner | |||||||||
| Yes | 38 (19.8) | 0.008 | 206 | 14 (7.3) | <0.001 | 206 | 67 (35.8) | 0.598 | 201 |
| No | 7 (50.0) | 5 (35.7) | 6 (42.9) | ||||||
| Reported estimation of income | |||||||||
| Below average | 9 (27.3) | 0.445 | 198 | 6 (18.2) | 0.067 | 198 | 11 (33.3) | 0.750 | 193 |
| Average / above average | 35 (21.2) | 13 (7.9) | 58 (36.3) | ||||||
| Salaried employment before delivery (even part-time) | |||||||||
| Yes | 38 (24.2) | 0.219 | 202 | 15 (9.6) | 0.893 | 202 | 62 (40.5) | 0.038 | 196 |
| No | 7 (15.6) | 4 (8.9) | 10 (23.3) | ||||||
| Lives with a smoker | |||||||||
| Yes | 28 (40.0) | <0.001 | 10 (14.3) | 0.069 | |||||
| No | 17 (12.4) | 9 (6.6) | |||||||
| This person quitted or diminished smoking | |||||||||
| Yes | 17 (43.6) | 0.492 | 70 | 3 (7.7) | 0.077 | 70 | |||
| No | 11 (35.5) | 7 (22.6) | |||||||
| This person smoked in the presence of the pregnant woman | |||||||||
| Yes | 22 (59.5) | 0.001 | 68 | 10 (27.0) | 0.002 | 68 | |||
| No | 6 (19.4) | 0 (0.0) | |||||||
| Alcohol consumption during pregnancy (a glass or more) | |||||||||
| Yes | 20 (27.4) | 0.198 | 201 | 10 (13.7) | 0.120 | 201 | |||
| No | 25 (19.5) | 9 (7.0) | |||||||
| Husband/partner consumes alcohol | |||||||||
| Yes | 58 (44.6) | 0.002 | 181 | ||||||
| No | 10 (19.6) | ||||||||
| Husband/partner stopped or diminished alcohol consumption | |||||||||
| Yes | 15 (44.1) | 0.946 | 130 | ||||||
| No | 43 (44.8) | ||||||||
| Alcohol offered by someone aware of the pregnancy (once or more) | |||||||||
| Yes | 46 (47.9) | 0.001 | 198 | ||||||
| No | 26 (25.5) | ||||||||
| Smoking during pregnancy, even temporary use | |||||||||
| Yes | 20 (44.4) | 0.198 | 201 | ||||||
| No | 53 (34.0) | ||||||||
| 1 This group includes women who decreased, did not modify or increased their tobacco consumption as they were pregnant, as well as those who quit smoking during pregnancy 2 This group includes women who smoked during the entirety of pregnancy. | |||||||||
| Table 4:Descriptive statistics for alcohol consumption. Results are reported as n (%). | ||
| Alcohol consumption during the year preceding pregnancy (even occasional) (N = 201) | 126 | (62.7) |
| Alcohol consumption during pregnancy (even a single glass) (N = 201) | 73 | (36.3) |
| Consumption frequency (N = 71) | ||
| Once a week or more often | 5 | (7.0) |
| Once to 3 times a month | 16 | (22.5) |
| Less than once a month | 50 | (70.4) |
| Mean consumed amount (per occasion) (N = 63) | ||
| ≤1 glass | 52 | (82.5) |
| >1 glass | 11 | (17.5) |
| Consumption of 4 glasses or more (at least once) (N = 72) | 8 | (11.1) |
| Encouragement to diminish consumption from people around (N = 66) | 27 | (40.9) |
| Feeling guilty about alcohol drinking during pregnancy (N = 71) | 16 | (22.5) |
| Alcohol-consuming husband/partner (N = 184) | 130 | (70.7) |
| This person (N = 130) | ||
| Stopped drinking during the pregnancy | 2 | (1.5) |
| Diminished his consumption | 32 | (24.6) |
| Did not modify his consumption | 95 | (73.1) |
| Increased his consumption | 1 | (0.8) |
| Alcohol offering by someone aware of the pregnancy (N = 201) | ||
| Never | 105 | (52.2) |
| Once | 30 | (14.9) |
| Several times | 66 | (32.8) |
| Had been informed about the risks of alcohol drinking during pregnancy (N = 202) | 174 | (86.1) |
| Through (multiple answers possible) | ||
| Media | 130 | (64.4) |
| General practitioner / gynaecologist | 89 | (44.1) |
| Poster campaign | 75 | (37.1) |
| People around | 54 | (26.7) |
| Other | 21 | (10.4) |
In this public hospital, one in five women smoked and almost two-thirds drank alcohol during pregnancy. The consumption and behaviour of close relatives were associated with tobacco and alcohol use during pregnancy. Pregnant women were more aware of the risks of smoking than of the risks of drinking during pregnancy. Surprisingly, only half of participants remembered having received information about these risks from their doctors.
There were more foreign women in our sample (66.2%) than among women aged between 20 and 39 years in the general population in Geneva in 2008 (49.9%) [12], probably because foreign women are less affluent and less likely to have an insurance that covers care in private clinics, and are, therefore, more likely to give birth in public hospitals.
Smoking before pregnancy was more frequent in our sample (31%) than in a another survey conducted in 2005 in Switzerland (20.3%) [13]. Regarding the proportion of women who smoked continuously during pregnancy, our results were closer to the findings of the same study (10.9%) [13]. Our results are in agreement with the prevalence of smoking among women aged 15 to 34 years in Geneva reported in 2007 in the Swiss Health Survey (34.3%) [14].
The smoking habits of close relatives seem to influence tobacco use by pregnant women. Several surveys, including one conducted in Switzerland, show that close relatives or husband/partner smoking are a major risk factor for smoking by pregnant women [15–18]. As well as the smoking status of husbands/partners or family members, the fact that these people smoked in the presence of the pregnant woman was associated with her consumption. Among pregnant smokers, we found a higher proportion of women reporting exposure to passive smoking than among nonsmokers. An American survey showed that women who succeed in quitting smoking during pregnancy were significantly less exposed to passive smoking from their family members [19]. Our results showed that women who smoked also tended to drink alcohol. Not drinking alcohol is a known predictive factor for quitting smoking in pregnant women [19].
In participants who smoked before pregnancy, living alone was associated with continued smoking during the entire pregnancy. Consistent with our results, a French survey showed that pregnant women living alone struggle more to quit smoking [20]. When the husband/partner is seen as supportive (especially if he quits smoking), pregnant women succeed more often in quitting smoking at the beginning of pregnancy [21].
The prevalence of alcohol drinking (36.3%) was similar to the results of a survey conducted in pregnant women in Lausanne, Switzerland, in 2006 (39.3%) [22]. A French survey showed that fewer than half the women who drank alcohol before pregnancy stopped drinking during pregnancy, which is in agreement with our results [23]. A minority of participants reported a binge drinking episode during pregnancy, which is consistent with a previous study (2.2%) [24]. We noted that pregnant women who drank alcohol during pregnancy felt less guilty than the ones who smoked (22.5% vs 83.3%). They were also less frequently encouraged by close relatives to reduce alcohol consumption when compared with tobacco smoking (40.9% vs 91.5%). These observations and the high proportion of participants who were offered alcohol during pregnancy suggest that there is an important difference in risk perception between these two behaviours in the general population. Fewer than 40% of women reported receiving information about the risks of smoking and drinking from their general practitioner or gynaecologist. These results contrast greatly with the observations of a Swiss survey conducted in 2007–2008, which reported that 77% of gynaecologists asserted that they gave systematic information on the risks related to alcohol drinking during pregnancy and 87% on the risks related to tobacco smoking [25]. The difference may be due to the source of information, as the previous study was questioning physicians, rather than the women themselves. The true figure probably lies in between.
Various factors associated with alcohol drinking during pregnancy are described in the literature, including low education, tobacco consumption, high income, not being married, and being more than 30 years old [22, 26–32]. We did not find any significant difference related to these factors between women who drank alcohol during pregnancy and women who did not. This could be due to the limited size of our sample. The importance of close relatives in influencing pregnant women’s consumption was also reported in previous studies [13]. An invitation to drink alcohol was strongly associated with women’s consumption during pregnancy in our study.
The high consent and response rates make our sample representative of women giving birth in the maternity ward of the Geneva University Hospitals, where two-thirds of all deliveries in the canton are cared for [33]. No recent investigation had been conducted on this subject locally. An original aspect of our work lies in the distinction made between women who smoked even temporarily and those who kept smoking during the entire pregnancy, two subgroups with different characteristics. The latter could also constitute a weakness by introducing a risk of misclassification, which would reduce the strength of the statistical associations.
Most of the women who give birth in the public hospital represent a population with lower incomes, which, together with the high proportion of foreigners specific to the region of Geneva, could limit the generalisability of our observations. The questionnaire comprehension may have been suboptimal among women who do not speak French as their mother tongue. We had to explain and translate the questionnaire to some of them, and this could have influenced the way these women answered the questions. The data were obtained five years ago, which can constitute a limitation, even if no major prevention campaign has been conducted in Geneva since then. It is important to emphasise that our survey design, using self-reports about habits during pregnancy submitted postpartum, may underestimate actual tobacco and alcohol consumption. This bias has been clearly demonstrated in the literature, and is difficult to avoid when evaluating well-known unfavourable exposures [34, 35].
An important proportion of women reported that they smoked and drank alcohol during pregnancy. Pregnant women were better informed about the risks associated with tobacco than of the risks of alcohol consumption. Health care providers must improve the information on the risks associated with these habits. The involvement of the husband/partner and other close relatives in health promotion interventions should be considered, for example by encouraging tobacco and alcohol avoidance in the presence of the pregnant woman. This counselling could take place during pregnancy follow-up visits.
1 Hofhuis W, de Jongste JC, Merkus PJFM. Adverse health effects of prenatal and postnatal tobacco smoke exposure on children. Arch Dis Child. 2003;88(12):1086–90.
2 Leonardi-Bee J, Smyth A, Britton J, Coleman T. Environmental tobacco smoke and fetal health: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2008;93(5):F351–61.
3 Salmasi G, Grady R, Jones J, McDonald SD. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89(4):423–41.
4 Sullivan W. A note on the influence of maternal inebriety on the offspring. J Mental Sci. 1899;45:489–503; reprinted Int J Epidemiol. 2011;40(2):278–82.
5 Lemoine P, Harousseau H, Borteyru JP, Menuet JC. Les enfants de parents alcooliques. Anomalies observées à propos de 127 cas. Ouest Med. 1968;8:476–82. French.
6 Jones KL, Smith DW, Ulleland CN, Streissguth P. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1(7815):1267–71.
7 Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;302(7836):999–1001.
8 Koren G, Nulman I, Chudley AE, Loocke C. Fetal alcohol spectrum disorder. CMAJ. 2003;169(11):1181–5.
9 Todorow M, Moore TE, Koren G. Investigating the effects of low to moderate levels of prenatal alcohol exposure on child behaviour: a critical review. J Popul Ther Clin Pharmacol. 2010;17(2):e323–330.
10 Grace Chang. Alcohol intake and pregnancy. UpToDate. [cited 2011 Mar 6]. Available from: http://www.uptodate.com/contents/alcohol-intake-and-pregnancy
11 Sayal K, Heron J, Golding J, Alati R, Smith GD, Gray R, et al. Binge pattern of alcohol consumption during pregnancy and childhood mental health outcomes: longitudinal population-based study. Pediatrics. 2009;123(2):e289–96.
12 Office cantonal de la statistique (République et canton de Genève). Population – Mouvement naturel. T_01_02_3_4_05.xls. [cited 2011 Mar 19]. Available from: http://www.ge.ch/statistique. French
13 Grob A, Lemola S. Substanzkonsum junger Eltern in der Schweiz. Final report. Bern: Federal Office of Public Health, 2005. German
14 Office cantonal de la statistique (République et canton de Genève). Santé – Mode de vie. T_14_03_1_5_01.xls. [cited 2011 Mar 20]. Available from: http://www.ge.ch/statistique. French.
15 Penn G, Owen L. Factors associated with continued smoking during pregnancy: analysis of socio-demographic, pregnancy and smoking-related factors. Drug Alcohol Rev. 2002;21(1):17–25.
16 Murin S, Rafii R, Bilello K. Smoking and Smoking Cessation in Pregnancy. Clinics in Chest Medicine. 2011;32(1):75–91.
17 Nafstad P, Botten G, Hagen J. Partners smoking: a major determinant for changes in women’s smoking behaviour during and after pregnancy. Public Health. 1996;110(6):379–85.
18 Lemola S, Grob A. Smoking cessation during pregnancy and relapse after childbirth: the impact of the grandmother’s smoking status. Matern Child Health J. 2008;12(4):525–33.
19 Severson HH, Andrews JA, Lichtenstein E, Wall M, Zoref L. Predictors of smoking during and after pregnancy: a survey of mothers of newborns. Prev Med. 1995;24(1):23–8.
20 Grangé G, Vayssiere C, Borgne A, Ouazana A, L’Huillier J-P, Valensi P, et al. Description of tobacco addiction in pregnant women. Eur J Obstet Gynecol Reprod Biol. 2005;120(2):146–51.
21 McBride CM, Curry SJ, Grothaus LC, Nelson JC, Lando H, Pirie PL. Partner smoking status and pregnant smoker’s perceptions of support for and likelihood of smoking cessation. Health Psychol. 1998;17(1):63–9.
22 Meyer-Leu Y, Lemola S, Daeppen J-B, Deriaz O, Gerber S. Association of moderate alcohol use and binge drinking during pregnancy with neonatal health. Alcohol Clin Exp Res. 2011;35(9):1669–77.
23 Houet T, Vabret F, Herlicoviez M, Dreyfus M. Comparison of women’s alcohol consumption before and during pregnancy. A prospective series of 150 women. J Gynecol Obstet Biol Reprod (Paris). 2005;34(7 Pt 1):687–93.
24 Lemola S, Grob A. Drinking and smoking in pregnancy: what questions do Swiss physicians ask? Swiss Med Wkly. 2007;137(3-4):66–9.
25 Grob A, Lemola S. Substanzkonsumscreening in der Schwangerschaftsvorsorge. Final report. Bern: Federal Office of Public Health, 2008. German.
26 Ethen MK, Ramadhani TA, Scheuerle AE, Canfield MA, Wyszynski DF, Druschel CM, et al. Alcohol consumption by women before and during pregnancy. Matern Child Health J. 2009;13(2):274–85.
27 Alvik A, Haldorsen T, Groholt B, Lindemann R. Alcohol consumption before and during pregnancy comparing concurrent and retrospective reports. Alcohol Clin Exp Res. 2006;30(3):510–5.
28 Haynes G, Dunnagan T, Christopher S. Determinants of alcohol use in pregnant women at risk for alcohol consumption. Neurotoxicol Teratol. 2003;25(6):659–66.
29 Leonardson GR, Loudenburg R. Risk factors for alcohol use during pregnancy in a multistate area. Neurotoxicol Teratol. 2003;25(6):651–8.
30 Flynn HA, Marcus SM, Barry KL, Blow FC. Rates and correlates of alcohol use among pregnant women in obstetrics clinics. Alcohol Clin Exp Res. 2003;27(1):81–7.
31 Alcohol use among women of childbearing age – United States, 1991–1999. MMWR Morb Mortal Wkly Rep. 2002;51(13):273–6.
32 Ebrahim SH, Luman ET, Floyd RL, Murphy CC, Bennett EM, Boyle CA. Alcohol consumption by pregnant women in the United States during 1988–1995. Obstet Gynecol. 1998;92(2):187–92.
33 Office cantonal de la statistique (République et canton de Genève). Santé – Accouchements et nouveau-nés. T_14_03_2_2_01.xls. [cited 2011 Mar 22]. Available from: http://www.ge.ch/statistique. French.
34 Sayal K. Alcohol consumption in pregnancy as a risk factor for later mental health problems. Evid Based Ment Health. 2007;10(4):98–100.
35 Shipton D, Tappin DM, Vadiveloo T, Crossley JA, Aitken DA, Chalmers J. Reliability of self reported smoking status by pregnant women for estimating smoking prevalence: a retrospective, cross sectional study. BMJ. 2009;339:b4347.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.
Authors’ contribution: JD and VG contributed equally to this work.