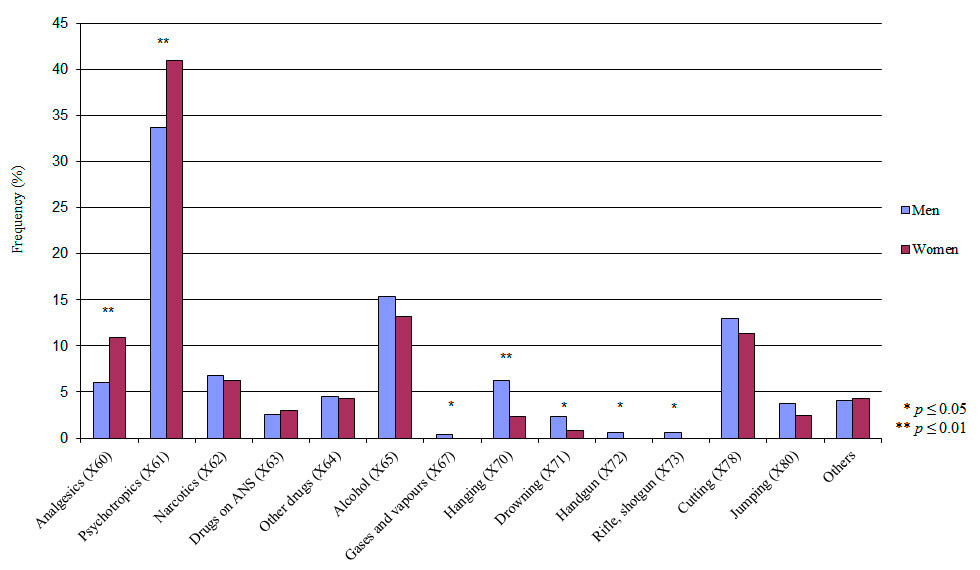
Figure 1
Distribution of the suicide attempt methods according to ICD-10 (multiple nominations). ANS = autonomous nervous system (X63).
DOI: https://doi.org/10.4414/smw.2013.13759
Suicidal behaviour is identified as a major public health problem in many European countries including Switzerland, both because it contributes to preventable mortality and because it is associated with severe emotional suffering for the affected ones and their environment [1–3]. Furthermore, suicidal behaviour represents a considerable burden on both primary and secondary healthcare [4, 5].
Swiss suicide rates are in the upper range compared with other European countries. For example, in Switzerland in the year 2000 the total suicide rate per 100,000 inhabitants was 19.1, whereas in Italy it was lower at 7.1 and in Lithuania it was higher at 44.1 [6]. The Federal Office of Public Health is aware of this finding, as it summarised the most relevant facts in the published public health survey in 2005 [2]. In addition, more people die from suicide than from traffic accidents [2]. Even though the relevance of suicide in Switzerland is known and notable national and regional suicide studies have been published (e.g. on methods used [7–10], inpatient suicides [11], suicidal behaviour in the emergency setting [12, 13] or after hospital discharge [14], treatment studies [15] and assisted suicide [16–21]), there is so far no national suicide prevention strategy. For developing a prevention strategy, Bertolote and Fleischmann reported the importance of not focusing solely on completed suicide, but including suicide attempts, which are known to be one of the strongest risk factors for completed suicide [1, 22–29].
The World Health Organisation (WHO) acknowledged this problem of suicidal behaviour, which is not only found in Switzerland and Europe, but also in many other parts of the world. One of the 12 ‘health-for-all’ targets of the WHO, included in the ‘Global Strategy for Health for All by the Year 2000’, is thereby “the reduction of the current rising trends in suicide and attempted suicide” [22, 30].
Therefore, the WHO/EURO Multicentre Study on Suicidal Behaviour was designed as part of the effort to implement these targets [1, 23–27]. The WHO/EURO Multicentre Study on Suicidal Behaviour allows international comparison of the frequency of suicide attempts and the methods used. It has provided accurate and continuous information about the epidemiology of attempted suicide in several European regions (e.g. northern centres such as Helsinki, Umea, Stockholm; central centres such as Oxford, Cork, Leiden, Rennes, Würzburg; southern centres such as Padua, Guipuzcoa; eastern centres such as Szeged, Kiev, Riga). Furthermore, the study helps understanding the factors involved and develop new and specific prevention projects in well-defined catchment areas. The only valid Swiss data available on suicide attempts are those published by Michel et al. for the conurbation of Bern in 1989 and for the study period up until 1998 [1, 31, 32]. Other reports from Michel’s workgroup include newer data from 2004 to 2010 [33, 34]. In 2003 the opportunity to participate in this valuable European study was offered to the county of Basel-City.
Thus, this study examines the rate of suicide attempts and their methods, as a part of the WHO/EURO Multicentre Study on Suicidal Behaviour, over four years in the catchment area of the county of Basel-City in Switzerland. Beyond gathering epidemiological information about suicide attempts, our interest lies in identifying specific risk groups. We therefore calculated a factor of suicide attempt risk exposure. Among other factors, the analysis of methods and drugs used in our sample and the mental disorders diagnosed should help to develop targeted public health programmes.
The study was conducted as part of the WHO/EURO Multicentre Study on Suicidal Behaviour. It was approved by the local ethics committee and conducted in accordance with the declaration of Helsinki.
In order to avoid errors made in previous studies, to rule out inadequacies from an epidemiological standpoint (e.g. no standardised information about the local catchment area) and to ensure that data collection was identical in all participating institutions, the WHO/EURO project required the use of a common definition of suicidal behaviour. A suicide attempt (previously called parasuicide [35, 36]) was defined as “an act with non-fatal outcome, in which an individual deliberately initiates a non-habitual behaviour that, without intervention from others, will cause self-harm, or deliberately ingests a substance in excess of the prescribed or generally recognised therapeutic dosage, and which is aimed at realising changes which the subject desired via the actual or expected physical consequences” [1, 23]. The definition includes acts that are interrupted before actual self-harm occurs, such as the behaviour of a person who lies across railway tracks with the intention of being run over by a train, but is rescued before the train arrives. Self-harmful acts by people who do not understand the meaning or consequences of their own actions were excluded. Completed suicides were not included in our study and not recorded separately.
The county of Basel-City is a district in the north-western part of Switzerland, located at river Rhine bordering with Germany and France.
Included in the study were subjects presenting at medical institutions with a suicide attempt, aged 15 years and older, and residing in the county of Basel-City. At the time of data collection the county of Basel-City had, according to the mean of the four ‘census years’, 164,960 inhabitants aged 15 years and older [37].
In the present study a standardised protocol sheet was used (appendix http://www.smw.ch/fileadmin/smw/pdf/smw-13759-Appendix.pdf ), which was based on that used in the WHO/EURO Multicentre Study on Suicidal Behaviour [25]. It comprised 24 questions. The items included socio-demographic variables (sex, age, change of address during the past year, current marital status, household composition, religious faith, educational status, educational qualifications, nationality), methods (up to four methods according to ICD-10 X-Code [38] including details on up to three chemical agents per case and their corresponding pharmacological categories) and motive, place and date of the attempt, days between repeated attempts if applicable, details on previous suicide attempts, economic situation at the time of the attempt, arranged treatment procedures, as well as the preliminary diagnosis of mental disorders according to ICD-10 [38].
Data were collected from January 2003 to December 2006. Data for comparison with the general population were retrieved from the Statistics Office Basel-City either as an end of the year census or from the census “Volkszählung 2000” [39]. (Census ‘Volkszählung 2000’ is the source for calculating rates/100,000 for the variables ‘education’ and ‘employment status’.)
In Basel-City, medical emergency care is mostly provided by the University Hospital (USB), which includes a psychiatric outpatient clinic and a crisis-intervention ward. Psychiatric inpatient treatment is provided by the Psychiatric University Hospitals (UPK; about 70% of the cases) and a private psychiatric hospital. According to the insurance system, patients are urged to seek inpatient treatment in their home canton.
The data were retrieved either by a member of the local research team or by the physicians responsible for the patient, via interview and/or analysis of the case record. Patients admitted to more than one medical institution for a suicide event were identified and the data merged to give one event. It must be noted that the data used here relate to cases of suicide attempts, and not attempters. Accordingly the same person can appear several times in the data set, if he or she was involved in more than one suicide attempt during the period of data collection. These attempters are so called ‘repeaters’.
The validity of data was ensured by close cooperation with all medical services in the county of Basel-City. As full coverage of events for the entire study period was not possible, two detailed investigations into the proportion of missed cases were conducted to provide the appropriate factor for estimation of all cases.
Firstly, at the end of the first study-year (2003) full coverage was sought, as we contacted all general practitioners as well as psychiatrists of the county of Basel-City and questioned them as to whether they had treated patients with suicide attempts in the elapsed year.
Secondly, in the entire month of June during the third year of the study (2005), 476 general practitioners, psychiatrists and hospitals in the catchment area as well in the municipalities surrounding the catchment area were contacted again by letter and phone [40].
Our research group agreed to follow the recommendations of the Bern study centre [31–33] for the value of the estimation factor (see results section).
The reliability of data collection was ensured by thorough training of the research staff and continuous supervision by the steering group of the WHO/EURO Multicentre Study.
Mean raw and extrapolated values (the latter are raw values multiplied by the estimation factor) for the entire study period are presented, and mean rates/100,000 inhabitants were calculated using the mean population census data from 2003 to 2006 in the catchment area. Furthermore, as an indicator of risk, a ratio was calculated for the suicide attempt rate per 100,000 inhabitants according to specific socio-demographic characteristics in proportion to the total suicide attempts per 100,000 inhabitants. Differences were analysed for the epidemiological variables (sex, age, civil status, household composition, religious faith, education, vocational training and employment status) and clinical variables (used methods and drugs, intention, and psychiatric diagnosis). For the present analyses, age groups were documented using five-year intervals. For a more global analysis of methods, ICD-10 [38] suicide codes X60–X69 (e.g. variations of self-poisoning) were merged into a category ‘soft methods’, whereas the remaining codes X70–X82 (e.g. self-harm by sharp object, hanging, firearm discharge, jumping) were considered to be ‘hard methods’ [41, 42]. Psychiatric illnesses were diagnosed according to ICD-10 and documented up to the second decimal place [38]. For the present article, evaluation was carried out for the broad diagnostic categories F0–F6. For the variables ‘methods’ and ‘agents’ multiple nominations were used.
Frequencies were calculated using univariate frequency tables and multivariate cross-tabulations for multiple response items, using SPSS 17.0. Chi-square statistics were used to test for the statistical significance of gender differences. T-tests were used for interval-based variables where appropriate. Statistical significance was defined as p ≤0.05.
As full data coverage was sought, two separate investigations for the estimation factor were made.
First, at the end of the first study-year, all general practitioners and all psychiatrists were asked whether they had treated patients with suicide attempts in the past year (2003). A total of 169 of 356 physicians responded (47.5%), who mentioned an additional nine cases. The latter corresponded to 4% of the total cases recorded in 2003, and thus 96% had been collected. The same number of missed cases had been found in the centre of Bern [31–33].
Secondly, in the month of June in 2005, 476 general practitioners, psychiatrists and hospitals in the catchment area were re-contacted several times by letter and phone, of whom 233 responded (48.9%). In addition to the 18 reported cases from the two main study hospitals (USB, UPK) during that month, five additional cases were found (thus 80% had been collected).
We estimate in summary that the number of cases going unreported was about 10% (mean of the two investigations), so we multiplied all data by the corresponding estimation factor, which was in this study therefore 1.1. Furthermore, we concluded that most suicide attempts were collected from the two main hospitals USB and UPK.
We documented a total of 984 suicide attempts involving 778 persons in the four-year study period. Of the total number of cases, 326 were performed by men and 658 by women, which was a statistically significant difference (χ2 = 112.016, p ≤0.001). Cases correspond to a female–male ratio of 2:1 (or 512 women and 266 men in absolute numbers). Considering all age groups and both sexes, the suicide attempt rate for the total group (event related) was 164.04/100,000 (115.88/100,000 for men and 206.58/100,000 for women). Person-related suicide attempt rates were in total 129.69/100,000, with 94.54/100,000 for men and 160.74/100,000 for women (χ2 = 17.04, p ≤0.001).
Table 1 shows the mean raw and extrapolated values for male and female suicide attempters, the general population numbers and the mean average age- and sex-specific rates per 100,000 inhabitants aged 15 years and older from 2003 to 2006 (based on cases). It also shows their proportion to the corresponding population, which suggests over- and under-representation, respectively.
| Table 1: Suicide attempt rates in the county of Basel-City, 2003–2006, according to sex and age. | |||||||||||||||
| Age (yr) | Men | Women | Total | ||||||||||||
| SA1 | x 1.12 | Popu- lation3 | Rate SA/100,000 | SA risk-exposure4 | SA1 | x 1.12 | Popu- lation3 | Rate SA/100,000 | SA risk-exposure4 | SA1 | x 1.12 | Popu- lation3 | Rate SA/100,000 | SA risk-exposure4 | |
| 15–19 | 3.5 | 3.9 | 4,296 | 89.61 | 0.8 | 10.8 | 11.8 | 4,344 | 272.20 | 1.3 | 14.3 | 15.7 | 8,641 | 181.41 | 1.1 |
| 20–24 | 9.0 | 9.9 | 5,808 | 170.45 | 1.5 | 33.3 | 36.6 | 6,608 | 553.54 | 2.7 | 42.3 | 46.5 | 12,416 | 374.33 | 2.3 |
| 25–29 | 9.5 | 10.5 | 6,879 | 151.92 | 1.3 | 24.5 | 27.0 | 6,947 | 387.94 | 1.9 | 34.0 | 37.4 | 13,826 | 270.51 | 1.6 |
| 30–34 | 11.5 | 12.7 | 6,931 | 182.51 | 1.6 | 18.5 | 20.4 | 6,796 | 299.44 | 1.4 | 30.0 | 33.0 | 13,727 | 240.40 | 1.5 |
| 35–39 | 10.0 | 11.0 | 7,425 | 148.15 | 1.3 | 18.3 | 20.1 | 7,164 | 280.23 | 1.4 | 28.3 | 31.1 | 14,589 | 213.01 | 1.3 |
| 40–44 | 8.3 | 9.1 | 7,641 | 118.77 | 1.0 | 13.5 | 14.9 | 7,339 | 202.36 | 1.0 | 21.8 | 23.9 | 14,980 | 159.72 | 1.0 |
| 45–49 | 7.0 | 7.7 | 6,887 | 111.80 | 1.0 | 13.3 | 14.6 | 6,764 | 215.49 | 1.0 | 20.3 | 22.3 | 13,651 | 163.17 | 1.0 |
| 50–54 | 6.0 | 6.6 | 6,083 | 108.51 | 0.9 | 8.8 | 9.6 | 6,172 | 155.95 | 0.8 | 14.8 | 16.2 | 12,255 | 132.40 | 0.8 |
| 55–59 | 4.0 | 4.4 | 5,751 | 76.52 | 0.7 | 4.8 | 5.2 | 5,934 | 88.06 | 0.4 | 8.8 | 9.6 | 11,684 | 82.38 | 0.5 |
| 60–64 | 2.5 | 2.8 | 5,122 | 53.69 | 0.5 | 5.8 | 6.3 | 5,562 | 113.72 | 0.6 | 8.3 | 9.1 | 10,684 | 84.94 | 0.5 |
| 65–69 | 2.8 | 3.0 | 4,066 | 74.40 | 0.6 | 2.8 | 3.0 | 5,149 | 58.75 | 0.3 | 5.5 | 6.1 | 9,215 | 65.66 | 0.4 |
| 70–74 | 2.3 | 2.5 | 3,643 | 67.93 | 0.6 | 2.3 | 2.5 | 5,147 | 48.09 | 0.2 | 4.5 | 5.0 | 8,790 | 56.31 | 0.3 |
| 75–79 | 3.3 | 3.6 | 3,111 | 114.91 | 1.0 | 2.3 | 2.5 | 5,108 | 48.46 | 0.2 | 5.5 | 6.1 | 8,219 | 73.61 | 0.4 |
| 80–84 | 0.8 | 0.8 | 2,178 | 37.89 | 0.3 | 2.5 | 2.8 | 4,269 | 64.41 | 0.3 | 3.3 | 3.6 | 6,447 | 55.45 | 0.3 |
| 85–89 | 1.3 | 1.4 | 1,042 | 132.02 | 1.1 | 2.0 | 2.2 | 2,488 | 88.43 | 0.4 | 3.3 | 3.6 | 3,529 | 101.30 | 0.6 |
| 90+ | 0.0 | 0.0 | 505 | 0.00 | 0.0 | 1.5 | 1.7 | 1,804 | 91.48 | 0.4 | 1.5 | 1.7 | 2,309 | 71.46 | 0.4 |
| Total | 81.5 | 89.7 | 77,367 | 115.88 | 164.5 | 181.0 | 87,593 | 206.58 | 246 | 270.6 | 164,960 | 164.04 | |||
| The table includes mean distribution of frequencies (mean raw and extrapolated values), rates/100,000 and suicide attempt risk-exposure. 1 SA = suicide attempt (mean raw values, unrounded); 2 x 1.1 = suicide attempt multiplied by the estimation factor 1.1 (mean extrapolated values, unrounded) which is the basis for calculation of the SA rate/100,000; 3 Mean population numbers for persons aged >15 years (based on end of the year census); 4 Values >1.0 and <1.0 indicate over- under-representation, respectively, of the specific group category in relation to the total rate SA/100,000. | |||||||||||||||
Table 2 shows the socio-demographic characteristics of the sample.
The mean age (SD) for men was 41.62 (16.81) years, ranging from age 17 to 89 years, and was 37.43 (16.87) years for women, ranging from age 15 to 103 years. Women were statistically significant younger at the time of the suicide attempt than men (t = 3.674, p ≤0.001).
In both sexes two peaks in the age distribution of suicide attempts could be identified: among the male population, men aged 30 to 34 years were at highest risk, with an age-specific rate of 182.51/100,000, followed by men aged 20 to 24 years, with an age-specific rate of 170.45/100,000. Among the female population, the age group with the highest rate was the group aged 20 to 24 years, with an age-specific rate of 553.54/100,000, followed by the group aged 25 to 29 years (with a rate of 387.94/100,000). A second peak was observed in the elderly (age ≥60) with men aged 85 to 89 years showing 132.02/100,000 suicide attempts and women aged 60 to 64 aged showing 113.72/100,000, respectively.
The distribution of the subgroups was expected: suicide attempters who were single showed highest suicide attempt rates with 156.81/100,000 in men and 306.51/100,000 in women. Being divorced was reported in one-tenth with a total rate of 181.90/100,000. Being married (25.8% of the male cases, 24.0% of the female cases) followed next with 85.25/100,000. Only a minority were widowed which showed the lowest attempt rate. All rates (split for gender) of the different civil states can be found in table 3.
| Table 2: Sample characteristicsa in the WHO/EURO Study (n = 778). | ||
| Characteristic | ||
| Age in years (Mean, SD) | 39.81 ± 17.46 | |
| n | % | |
| Gender | ||
| Women | 512 | 65.8 |
| Men | 266 | 34.2 |
| Civil status | ||
| Single | 355 | 45.6 |
| Married | 207 | 26.6 |
| Divorced | 130 | 16.7 |
| Widowed | 37 | 4.8 |
| Household composition | ||
| Single | 249 | 32.0 |
| Single with child | 35 | 4.5 |
| With partner, no child | 160 | 20.6 |
| With partner and child | 99 | 12.7 |
| Adults living with parent(s) | 56 | 7.2 |
| Adults living with relative(s) | 35 | 4.5 |
| In institution | 33 | 4.2 |
| Other | 25 | 3.2 |
| Religious faith | ||
| None | 93 | 12.0 |
| Protestant | 143 | 18.4 |
| Catholic | 148 | 19.0 |
| Muslim | 112 | 14.4 |
| Other | 29 | 3.8 |
| Not known | 253 | 32.6 |
| Education | ||
| Primary/special-needs schools (low) | 301 | 38.7 |
| Secondary school (middle) | 248 | 31.9 |
| University/applied (high) | 25 | 3.2 |
| Employment status | ||
| Economically active employed | 197 | 25.3 |
| Economically active unemployed | 93 | 12.0 |
| Economically inactive | 355 | 45.6 |
| History of migration | ||
| Yes | 234 | 30.1 |
| No | 473 | 60.8 |
| Diagnostic group (ICD-10) | ||
| F1 | 86 | 11.1 |
| F2 | 80 | 10.3 |
| F3 | 300 | 38.6 |
| F4 | 174 | 22.4 |
| F5 | 7 | 0.9 |
| F6 | 85 | 10.9 |
| Method of suicidal actionb | ||
| Hard | 234 | 30.1 |
| Soft | 539 | 69.3 |
| Intentionc | ||
| Lethal | 357 | 45.9 |
| Nonlethal | 314 | 40.3 |
| a Percentages not adding up to 100 are due to missing information. b Soft methods according to ICD-10 X60-X69, including self-poisoning; hard methods ICD-10 X70-X84, including hanging, cutting, running into traffic, jumping, burning or drowning. c Intention of dying as opposed to parasuicidal gestures and pauses, deliberate self-harm or overdoses due to dependency. | ||
| Table 3: Suicide attempt rates in the county of Basel-City, 2003 to 2006, according to gender for a) civil status, b) household composition, c) religious faith, d) education, e) employment status, f) nationality. | |||||||||||||||
| Men | Women | Total | |||||||||||||
| SA1 | x 1.12 | Popu- lation3 | Rate SA/100,000 | SA risk-exposure4 | SA1 | x 1.12 | Popu- lation3 | Rate SA/100,000 | SA risk-exposure4 | SA1 | x 1.12 | Popu- lation3 | Rate SA/100,000 | SA risk-exposure4 | |
| a) Civil status | |||||||||||||||
| Single | 42.0 | 46.2 | 29,462 | 156.81 | 1.5 | 80.3 | 88.3 | 28,800 | 306.51 | 1.7 | 122.3 | 134.5 | 58,262 | 230.81 | 1.6 |
| Married | 21.0 | 23.1 | 39,622 | 58.30 | 0.6 | 39.5 | 43.5 | 38,445 | 113.02 | 0.6 | 60.5 | 66.6 | 78,067 | 85.25 | 0.6 |
| Divorced | 7.0 | 7.7 | 6,024 | 127.82 | 1.3 | 18.5 | 20.4 | 9,397 | 216.56 | 1.2 | 25.5 | 28.1 | 15,421 | 181.90 | 1.3 |
| Widowed | 1.8 | 1.9 | 2,180 | 88.30 | 0.9 | 8.0 | 8.8 | 10,923 | 80.56 | 0.4 | 9.75 | 10.7 | 13,103 | 81.85 | 0.6 |
| Total | 71.8 | 78.9 | 77,288 | 102.12 | 146.3 | 160.9 | 87,565 | 183.72 | 218.0 | 239.8 | 164,853 | 145.46 | |||
| b) Household composition | |||||||||||||||
| Single | 30.5 | 33.6 | 20,212 | 165.99 | 1.6 | 48.3 | 53.1 | 27,630 | 192.09 | 1.0 | 78.5 | 86.4 | 47,842 | 180.49 | 1.2 |
| Single with child | 3.3 | 3.6 | 2,585 | 138.30 | 1.4 | 8.3 | 9.1 | 5,799 | 156.49 | 0.8 | 11.5 | 12.7 | 8,384 | 150.88 | 1.0 |
| With partner, no child | 14.5 | 16.0 | 24,386 | 65.41 | 0.6 | 33.8 | 37.1 | 24,269 | 152.97 | 0.8 | 48.25 | 53.1 | 48,655 | 109.08 | 0.7 |
| With partner and child | 7.5 | 8.3 | 23,236 | 35.51 | 0.3 | 21.5 | 23.7 | 22,240 | 106.34 | 0.6 | 29.0 | 31.9 | 45,476 | 70.15 | 0.5 |
| Adults living with parent(s) | 5.8 | 6.3 | 399 | 1585.21 | 15.5 | 10.3 | 11.3 | 725 | 1555.17 | 8.3 | 16.0 | 17.6 | 1,124 | 1’565.84 | 10.6 |
| Adults living with relative(s) | 2.8 | 3.0 | 392 | 771.68 | 7.6 | 6.8 | 7.4 | 421 | 1763.66 | 9.4 | 9.5 | 10.5 | 813 | 1’285.36 | 8.7 |
| In institution | 4.3 | 4.7 | 1,175 | 397.87 | 3.9 | 11.0 | 12.1 | 2,644 | 457.64 | 2.4 | 15.25 | 16.8 | 3,819 | 439.25 | 3.0 |
| Other | 2.8 | 3.0 | 4,297 | 70.40 | 0.7 | 10.3 | 11.3 | 3,868 | 291.49 | 1.5 | 13.0 | 14.3 | 8,165 | 175.14 | 1.2 |
| Total | 71.3 | 78.4 | 76,682 | 102.21 | 150.0 | 165.0 | 87,596 | 188.36 | 221.0 | 243.1 | 164,278 | 147.98 | |||
| c) Religious faith | |||||||||||||||
| None | 8.5 | 9.4 | 27,228 | 34.34 | 0.3 | 19.0 | 20.9 | 25,575 | 81.72 | 0.4 | 27.5 | 30.3 | 52,803 | 57.29 | 0.5 |
| Protestant | 15.0 | 16.5 | 17,247 | 95.67 | 0.7 | 39.0 | 42.9 | 24,623 | 174.23 | 0.8 | 54.0 | 59.4 | 41,870 | 141.87 | 1.2 |
| Catholic | 17.0 | 18.7 | 18,390 | 101.69 | 0.8 | 32.0 | 35.2 | 23,069 | 152.59 | 0.7 | 49.0 | 53.9 | 41,069 | 131.24 | 1.1 |
| Muslim | 10.0 | 11.0 | 5,107 | 215.39 | 1.6 | 22.3 | 24.5 | 4,145 | 590.47 | 2.5 | 32.3 | 35.5 | 9,252 | 383.43 | 3.1 |
| Other | 5.0 | 5.5 | 5,052 | 108.87 | 0.8 | 6.3 | 6.9 | 6,333 | 108.56 | 0.5 | 9.5 | 10.5 | 11,385 | 91.79 | 0.7 |
| Not known | 26.3 | 28.9 | 3,658 | 789.37 | 6.0 | 46.0 | 50.6 | 3,851 | 1313.94 | 5.6 | 72.3 | 79.5 | 7,509 | 1’058.40 | 8.6 |
| Total | 81.8 | 89.9 | 67,972 | 132.30 | 164.5 | 181.0 | 77,412 | 233.75 | 162.8 | 179.0 | 144,994 | 123.47 | |||
| d) Education | |||||||||||||||
| Primary/special-needs schools (low) | 31.8 | 34.9 | 13,604 | 256.73 | 2.4 | 66.3 | 72.9 | 20,489 | 355.68 | 1.8 | 98 | 107.8 | 34,093 | 316.19 | 2.1 |
| Secondary school (middle) | 26.8 | 29.4 | 32,549 | 90.40 | 0.9 | 54.3 | 59.7 | 38,871 | 153.52 | 0.8 | 81 | 89.1 | 71,420 | 124.75 | 0.8 |
| University/applied (high) | 3.8 | 4.1 | 18,964 | 21.75 | 0.2 | 7.5 | 8.3 | 13,146 | 62.76 | 0.3 | 11.3 | 12.4 | 32,110 | 38.54 | 0.3 |
| Total | 62.3 | 68.5 | 65,117 | 105.0 | 128.0 | 140.8 | 72,506 | 194.19 | 190.3 | 209.3 | 137,623 | 152.06 | |||
| e) Employment status | |||||||||||||||
| Economically active employed | 17.5 | 19.3 | 49,573 | 38.83 | 0.4 | 47.3 | 52.0 | 42,387 | 122.62 | 0.7 | 64.8 | 71.2 | 91,960 | 77.45 | 0.6 |
| Economically active unemployed | 12.8 | 14.0 | 2,773 | 505.77 | 5.3 | 12.5 | 13.8 | 3,033 | 453.35 | 2.5 | 25.3 | 27.8 | 5,806 | 478.38 | 3.4 |
| Economically inactive | 36.0 | 39.6 | 24,336 | 162.72 | 1.7 | 83.0 | 91.3 | 42,176 | 216.47 | 1.2 | 119 | 130.9 | 66,512 | 196.81 | 1.4 |
| Total | 66.3 | 72.9 | 76,682 | 95.0 | 143.0 | 157.0 | 87,596 | 179.0 | 209.0 | 230.0 | 164,278 | 140.0 | |||
| f) Nationality | |||||||||||||||
| Swiss | 50.8 | 55.8 | 51,988 | 107.38 | 0.5 | 24.8 | 27.2 | 65,214 | 41.75 | 0.5 | 159.8 | 175.7 | 117,202 | 149.93 | 3.4 |
| Non-Swiss | 109.0 | 119.9 | 25,308 | 473.76 | 2.0 | 43.0 | 47.3 | 22,362 | 211.52 | 2.5 | 67.8 | 74.5 | 47,670 | 156.34 | 1.4 |
| Total | 159.0 | 175.7 | 77,296 | 227.34 | 67.8 | 74.5 | 87,576 | 85.1 | 227.5 | 250.3 | 164,853 | 151.80 | |||
| The table includes mean distribution of frequencies (mean raw and mean extrapolated values), rates/100,000 and suicide attempt risk-exposure. 1 SA = suicide attempt (mean raw values, unrounded); 2 x 1.1 = suicide attempt multiplied by the estimation factor 1.1 (mean extrapolated values, unrounded) which is the basis for calculation of the SA rate/100,000, 3 Mean population numbers for persons aged >15 years (based on end of the year census), 4 Values >1.0 and <1.0 indicate over- respective under-representation of the specific group category in relation to the total rate SA/100,000. | |||||||||||||||
Almost a third of the suicide attempters were living in single households. This corresponds to the general population distribution. Another third was living with a partner or a partner and child/children. A total of 6% of the attempters were living in an institution (e.g. nursing home, youth or penal institution). Men showed a slightly higher percentage of single households (37%) compared with women (29%). Otherwise, only few gender differences were found.
Using the general population statistics, the following attempt rates were calculated: for pupils at legal age / students living with their parents 1565.84/100,000 or living with their relatives 1285.36/100,000; for single households 180.49/100,000; for single parents 150.88/100,000; for those living with a partner only 109.08/100,000 and for persons living with partner and children 70.15/100,000. Rates split for both sexes can be found in table 3.
There were big differences in the rates of attempted suicide between the various religious groups. Those who had no religious faith represented 10.9% and the rate of attempted suicide was 57.29/100,000, which was the lowest compared with the other religious categories. The 13.1% of Muslims had the highest rate of 383.43/100,000, which was unexpectedly high compared with their representation in the general population (6.4%). Rates for both sexes separately are shown in table 3.
For cross-cultural comparisons, level of schooling was recoded to match international standards. Persons were assigned to three categories (low, middle, high) according to the level of education when leaving school: ‘low’ was defined as primary school / Primarschule and special-needs schools / Sonderschule composing 39.8% of the cases; ‘middle’ consisted of secondary school / Mittelschule including academic-track high school / Gymnasium with 32.9% of the cases, and ‘high’ contained university/Universität and other applied university / Fachhochschule with 4.5% of the cases. Suicide attempt rates were highest for those with low education (316.19/100,000) compared with those with middle education (124.75/100,000) and those with high education (38.54/100,000). For details see table 3.
People who were economically active (e.g. not of school age, nor retired or disabled) showed lower attempt rates compared with unemployed or economically inactive people. Highest rates of attempted suicides were found in the group of the economically active but unemployed persons: 505.77/100,000 in men (7% of the sample) and 453.35/100,000 in women (3% of the sample). The rates per 100,000 for economically active employed were 38.83/100,000 in men (62% of the sample) and 122.62/100,000 in women (48% of the sample). The rates for the economically inactive were 162.72/100,000 in men (31% of the sample) and 216.47/100,000 in women (49% of the sample), respectively. Further results are shown in table 3.
An average of 23% of the male attempters and 18% of the female attempters were of foreign nationality, which is slightly higher than the mean percentage of foreigners in Switzerland (19%). Foreign nationality was defined non-Swiss citizenship as indicated in the passport / identity card. In the county of Basel the mean percentage of foreigners in the four-year study period was 28.91%. The suicide attempt rates were 474.76/100,000 (men) and 211.52/100,000 (women) for foreigners compared with 107.38/100,000 (men) and 41.75/100,000 (women) for the Swiss population. Further details are shown in table 3.
Figure 1 shows the frequency distribution of the employed methods, categorised by sex. ‘Soft methods’ (70% of the cases) were used significantly more frequently than ‘hard methods’ (χ2= 156.48, p ≤0.001). Self-poisoning with drugs (X60-X64) was used most frequently by both men and women (53.6% for men and 65.5% for women). Self-poisoning with alcohol (X65) came second (15.4% in men, 13% in women). Intentional self-harm by sharp objects (X78) ranked third (13.2% in men, 11.4% in women).
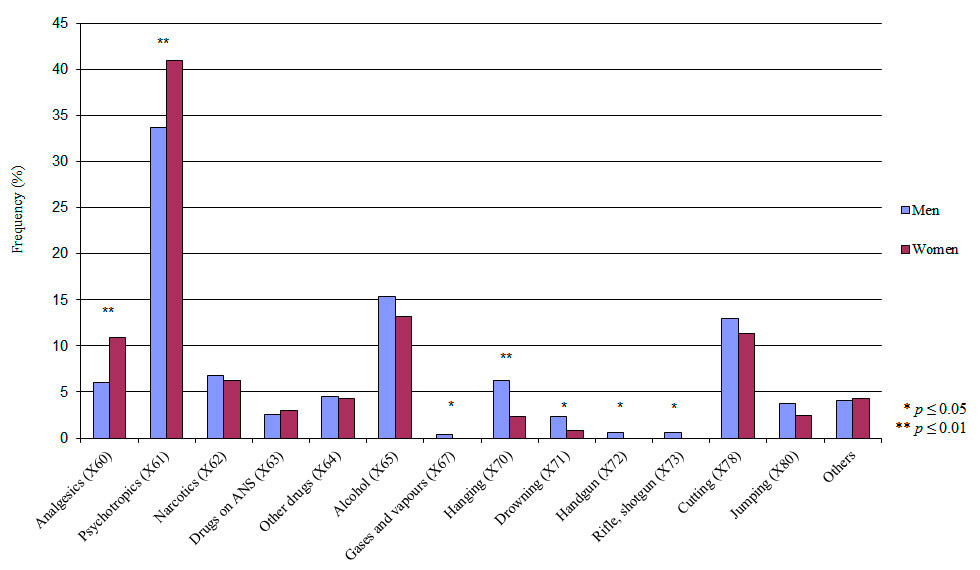
Figure 1
Distribution of the suicide attempt methods according to ICD-10 (multiple nominations). ANS = autonomous nervous system (X63).
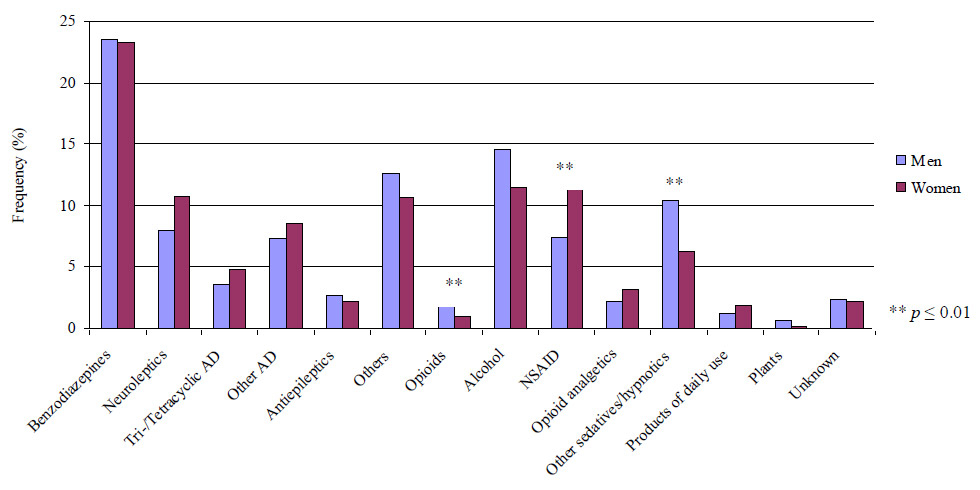
Figure 2
Distribution of used drugs in suicide attempts (multiple nominations). NSAID = nonsteroidal anti-inflammatory drug; AD = antidepressant.
Figure 3
Distribution of primary ICD-10 diagnoses.
Women were more prone to use analgesics, X60, (χ2= 6.05, p ≤0.01) or psychotropics, X61, (χ2= 6.67, p ≤0.01). Men were more likely to use gases and vapours, X67, (χ2= 3.83, p ≤0.05), hanging, X70, (χ2= 7.5, p ≤0.01), drowning, X71, (χ2= 4.64, p ≤0.05) as well as suicide attempts using handguns, X72, (χ2= 4.51, p ≤0.05) and suicide attempts using rifles or shotguns, X73, (χ2= 4.51, p ≤0.05). In all other methods no significant differences were found between men and women.
A total of 33.1% of both sexes used more than one method. The most frequently used supplementary method was the ingestion of alcohol (X65). No significant difference between men (48.2%) and women (43.7%) was found.
Furthermore, up to three drug-categories per case were documented and coded in detail regarding employed methods (multiple nominations analysis). We found that benzodiazepines were the most frequently ingested drug for both sexes (23% each), as shown in figure 2. A total of 14.6% of the men and only 1.0% of the women used opioids. This difference was statistically significant (χ2= 5.15, p ≤0.01). Men also used sedatives/hypnotics significantly more often than women (10.4% vs. 6.3%; χ2= 4.98, p ≤0.01). A total of 7.5% of the male and 13.7% of the female suicide attempters used nonsteroidal anti-inflammatory drugs. Hence, the use of nonsteroidal anti-inflammatory drugs in suicide attempts was significantly higher in women compared to men (χ2 = 6.56, p ≤0.01). In most cases, the drugs were prescribed by a physician.
A total of 31.1% of the male cases (corresponding to 42 men) and 32.1% of the female cases (corresponding to 65 women) were so called ‘repeaters’ in the entire study period. As many as 85% of the repeaters re-attempted within one year (men in 77.6%, women in 89.8%). About one-third re-attempted within one month after the initial attempt (men in 29.03%, women in 39.0%), typically with unchanged suicide methods.
The number of days it took until 50% of the repeaters re-attempted suicide was 125 days (or about four months) in men, and 59 days (or two months) in women.
Patients were also asked to recall their past suicide attempt history: 33.1% (men) and 29.0% (women) of all attempters were first-ever attempters. A total of 19.6% of the men and 29.0% of the women said that they had made at least one attempt within the previous 12 months. The analysis of all cases of the total sample revealed a repetition rate of 15.3% among male first-ever attempters and a repetition rate of 20.5% among female first-ever attempters within a 12-month period.
Apart from the details on the suicide attempt, the intention of the act was requested. The five response options, which were based on Bronisch [43], were as follows: (a) deliberate self-harm (DSH), (b) ‘parasuicidal pause’, an act with a motive of caesura, (c) ‘parasuicidal gesture’, an action motivated by an appeal, (d) overdose in an addiction disorder and (e) suicide attempt in the narrow sense with the intention to decease. The vast majority of the patients had ‘serious’ intentions to die at the moment of the attempt: for 45.5% of men and 42.4% of women, the definition in the narrow sense was applied. ‘Parasuicidal gesture’ and ‘parasuicidal pause’ ranked in second and third place. Statistically significant differences between male and female attempters were found for ‘parasuicidal pause’ (χ2 = 7.54, p ≤0.01) and for suicide attempt in the narrow sense (χ2 = 7.48, p ≤0.05): women presented ‘parasuicidal gestures’ more frequently whereas men presented more suicidal attempts in the narrow sense.
Because of the advantages of our liaison system, with a psychiatrist on duty seeing every suicide attempter brought to the hospitals in the catchment area, the primary clinical diagnosis at the time of the suicide attempt could be recorded. Suicide attempters suffered most frequently (38%) from a mood disorder (F3). Overall, 19.1% had a neurotic, stress-related and somatoform disorder (F4), whereas 15.3% had a disorder of adult personality and behaviour (F6). About 10% of the suicide attempters suffered from a mental and behavioural disorder due to psychoactive substance use (F1), and 10% each from schizophrenia, schizotypal or a delusional disorder (F2) .
Men were significantly more often affected by a substance abuse disorder or a psychosis (χ2 = 10.42, p ≤0.001 and χ2 = 11.08, p ≤0.001), whereas in women adjustment disorders and personality disorders were diagnosed significantly more frequently (χ2 = 4.56, p ≤0.05 and χ2 = 20.24, p ≤0.001). In only 1.5% of men and in 1.2% of women no psychopathology was found. The frequency distribution (in %) of the primary diagnosis is shown in figure 3.
Suicide attempters were most often treated in inpatient psychiatric care (68.1% in men and 65.3% in women), whereas psychiatric outpatient care ranked second with 14.2% for men and 16.9% for women. General inpatient hospital care was arranged for men in 5.2% and for women in 4.6% of cases, mainly because of somatic problems. General outpatient care was only rarely carried out, for 2.8% of the male attempters and for 1.8% of the female attempters, for example. In 5.2% (men) and 4.9% (women) of cases, patients were discharged without any aftercare, at least to our knowledge. In 85.7% the patients accepted treatment on a voluntary base. A total of 90.8% accepted psychiatric care (in- or out-patient-treatment) voluntarily.
Our study provides representative epidemiological data on suicide attempts in the county of Basel for the first time. Identifying risk groups helps to develop local prevention strategies and contributes to the international efforts to reduce mortality and morbidity related to suicidal behaviour.
The total suicide attempt rate in Basel was 164/100,000 inhabitants and was within the European average [44]. The lowest rate has been found in Turkey with 35/100,000 and the highest in Finland with 327/100,000 [44]. It must be noted that European numbers are highly heterogeneous: they range, for example, in French départements from 30/100,000 in rural areas to 590/100,000 in the towns as these areas have specific medical and socio-cultural characteristics [45, 46]. Regarding Switzerland, our mean rate was with 164/100,000, 1.5-fold higher than the rate found in the centre of Bern with 111/100,000 in the same time period [34].
As with 15 of the 19 countries involved in the WHO/EURO Multicentre Study, we found higher suicide attempt rates among women [25, 45] and confirm this risk-factor known from the literature. The Basel suicide attempt rates among men (115/100,000) and women (206/100,000) are lower than the published European suicide attempt average in 2004 (170/100,000 in male attempters and 209/100,000 in female attempters).
In our study the female/male ratio was almost 2:1 and tended to be higher than in other study centres but still lies in the range found elsewhere of 2.3:1 (Turkey and Sweden: [45]) to 0.7:1 (Estonia: [45]). In Bern, suicide was attempted nearly equally frequently by men and women [33].
In Basel, as in the majority of the centres, the highest suicide attempt rates were found in the younger ages groups [25]. The highest age-specific rates were found in the 20–29 years age group for female attempters and in the 20–34 years age group for male attempters. This confirms that suicide attempts occur more commonly in teenagers and young adults [47]. The rates among attempters aged 55 years and over were generally the lowest, which is a constant finding within the WHO/EURO Multicentre Study [25]. An expected finding was a second peak in the age distribution with raising suicide attempt rates which reach a climax in 85–89 year old men and in 60–64 year old women. The study of Murphy et al. found older adults, especially men aged 75 years and above, to be at risk for suicide after deliberate self-harm [46]. Furthermore, in our study, women were significantly younger than men, a finding which finds no support from other centres and could be interpreted as a specific characteristic of our sample.
In line with the findings of other centres from the WHO/EURO Study the highest attempt rates were that of single persons [49]. Nock [50] and Weissman [51] concluded that being unmarried (i.e. single, divorced) is a consistent cross-national risk factor for suicide attempts. On the other hand, lowest rates were found in all study centres and in Basel in widowers [49].
A recent study on suicide attempts in immigrants of the WHO/EURO Multicentre Study showed higher rates in immigrants than in natives [52]. Previous findings from our study group [53–55] and from Germany [56, 57] also showed immigrants to be at high risk. Our findings support the current data.
We found persons living without a partner (with or without a child) to have higher rates than those living with a partner. This was true for various centres in the study [31, 49] and is a well-known finding from the literature: perceptions of social and family support and connectedness have been shown to be significantly associated with lower rates of suicidal behaviour [58]. Other findings suggest that feelings of loneliness are associated with an increased risk of suicide attempt [59, 60], and that family and social support are protective factors [61]. In his study on the impact of parental status on the risk of completed suicide Qin [62] concluded that having children, especially young children, is protective against suicide. The high rates found in our study for adults living with their parents and living with relatives should not be overvalued as absolute numbers of cases are rather small.
It appears that religious/spiritual persons have lower rates of suicide attempts (e.g. 62–67), although two studies showed that religiosity was not associated with suicide attempts [68, 69]. Protestant and Catholic attempters manifested similar characteristics in their suicidal behaviour [70] and religiosity [71]. Studies on the association of Christian faith and completed suicide showed lower rates in Catholics than in Protestants (e.g. [72]). Studies regarding Muslim faith found high rates of suicide and attempted suicide in Middle Eastern countries [73]. Our study found highest rates for Muslims and lowest for those who indicated no religious persuasion. Moreover, suicide attempt rates in Catholics were slightly lower than in Protestants. Potential reasons for this relationship have previously been discussed, for instance moral objection to suicide [74] and social support [75], which also seem to protect against suicide attempts. These were not investigated in the present study.
Earlier studies have suggested that poor educational level is related to an increased risk of suicide attempt [76, 77]. We also found highest suicide attempt rates for those with low education (primary/special-needs school) and lowest for university graduates in the current study.
Regarding employment status, we found, as expected, highest rates for economically active but unemployed persons and therefore replicated risk-factors from other studies: for example, Nock [61] wrote in his review that lack of education and unemployment, which are associated with social disadvantage, may represent increased risk for suicidal behaviours, although the mechanisms through which these factors may lead to suicidal behaviour are not yet understood. Schmidtke [25] concluded from the WHO/EURO Study that “compared with the general population, suicide attempters more often belong to the social categories associated with social destabilisation and poverty”.
The methods used in the current study were primarily ‘soft’ (poisoning with drugs or alcohol) and the third frequent method used was ‘cutting’. Our results are consistent with findings from other centres within the WHO/EURO Multicentre Study [49, 78]. We found significant gender differences, which are in line with the literature [49, 79]: women were more prone to use analgesics and psychotropics, whereas men were more likely to use gases and vapours, hanging, and drowning, as well as handguns or rifles/shotguns. Gender differences in suicide and suicide attempt methods are cited frequently as it is known that men choose more lethal methods [80]. Furthermore, it is important to indicate that the same methods might be used with different intentions [80].
In Basel, the use of drugs, especially benzodiazepines and nonsteroidal anti-inflammatory drugs, for suicide attempts were used. This finding was also reported by other centres, for example in Bern [79] or Hungarian Pecs [81]. We conclude that the high use of benzodiazepine rather than antidepressants could indicate, as suggested by Fekete et al. [81], that many attempters only get symptomatic therapy for anxiety and sleeping disorders, whereas the depressive disorders remain concealed. Michel [82] reported that in Swiss suicides benzodiazepines have been used most often. Furthermore, significant gender differences were found: women used nonsteroidal anti-inflammatory drugs more often, whereas men attempted self-poisoning with opioids and other sedatives/hypnotics more frequently. Unfortunately the reasons for these differences were not investigated.
Studies have shown that there is a high risk of further suicidal behaviours among those who have attempted suicide previously [25, 35, 49, 83–85]. Our results found a third of the attempters to be repeaters. In a systematic review, Owens et al. [85] found that non-fatal repetition was on average 15%–16% at 1 year with a slow rise to 20%–25% over the following few years. Similarly, Schmidtke et al. [49] reported repetition during the first 12 months after the index event to be 16% in men and 17% in women. In our study, repetition during the first year was in line with these findings. Our results highlight that half of the male repeaters re-attempted within four months, while the critical time window was two months for female repeaters. This highlights the importance of additional sensitivity with regard to gender in matters of length of professional aftercare, which includes evidence-based treatment for the underlying/concomitant mental disorder.
In our study we found the investigated sample to have most often indicated the category suicide attempt in the narrow sense as intention (often so called ‘serious’ intentions). We found significant gender differences: men showed more ‘serious attempts’, whereas women made ‘parasuicidal gestures’ more frequently. This finding was consistently reported from the Würzburg centre where Schmidtke [87] reported that “more seriously rated suicide attempts are found in the older age groups and among men, while ‘demonstrative’ suicide attempts are prevalent in younger age groups and among women”. Reasons for this cluster have not been given.
The presence of a mental disorder is among the most consistently reported risk factor for suicidal behaviour [87, 88]. In our study 98.3% of the suicide attempters were diagnosed with a mental disorder. An even higher percentage of 100% was found in the Hungarian centre of Pecs [49]. Our high number is therefore in line with previous findings. The most common clinical diagnoses among medically treated suicide attempters of both genders were affective disorders, adjustment disorders and personality disorders. This corresponds to findings from the German Würzburg centre [86]. In our study there were significant differences in mental disorders between men and women. Adjustment and personality disorders were twice as frequent in women, whereas addiction and psychotic disorders were higher in men. Underlying causes of gender differences remain unclear, although this pattern is known from other studies (e.g. [86]).
More than two-thirds of the attempters had been treated afterwards in in-patient psychiatric care. These results are comparable to the findings from the Bern centre [33]. Regarding medical aftercare, Gibb [84] concluded that those making suicide attempts requiring hospital admission are at high risk of further hospitalisation for suicide attempt and of death from suicide. His and our current and previous findings suggest a need for ongoing support and monitoring, and for enhanced treatment and management for all those making suicide attempts [89]. Our findings regarding risk times for repetition highlight the need for implementation of a gender specific strategy.
Finally, and most importantly, the public health implications, have to be considered. The results should find their way into specific prevention programmes. How can we provide better suicide and suicide attempt prevention following the WHO initiative? Do we have to intensify our efforts to reduce the availability of means for suicide attempts or do we have to focus more on reducing mental disorders, that is, to make access to psychiatric care easier, to provide more comprehensive psychiatric care (primary prevention) and to deliver more intensive and longer aftercare (secondary prevention) [90]?
The relatively stable rates of suicide and suicidal behaviour over time known from the literature highlight the need for greater attention to prevention and intervention. A recent systematic review of suicide prevention programmes [61] revealed that restricting access to lethal means and training physicians to recognise and treat depression and suicidal behaviour shows impressive effects in reducing suicide rates [91]. Means-restriction programmes can decrease suicide rates by 1.5%–23% [92–99], while primary-care physician education and training programmes show reductions of 22%–73% [100–104]. Means-restriction could be made for dangerous medications, such as tri- and tetracyclic antidepressants or nonsteroidal anti-inflammatories (reduction of package sizes, empty house-pharmacy [53, 55, 89]). Although effective global prevention programmes exist, the fact that many people engaging in suicidal behaviour do not receive treatment of any kind [105–107] underlines the need for greater dissemination of information and further development of prevention efforts [107–109]. From our data we conclude that specific efforts should focus on persons at risk who were characterised as being younger, foreign, living alone and being unemployed. This suggestion could be implemented in local programmes as the alliance against depression.
To strengthen the impact of our data we need to critically discuss their validity and question whether they are representative. In contrast to former studies, we were able to use a well-defined catchment area (here a whole canton) that allows for statistical comparison with the population. A further plus was the use of a standardised definition of suicide attempts. Thirdly, we were able to monitor a remarkably high percentage of suicide attempts: 90% [34] compared with 58% in Berne [33]. As two separate investigations on the estimation factor were conducted, we believe it to be realistic [40].
The catchment area of the county of Basel includes mainly an urban population and represents the typical distribution of an urban population into three economic sectors (e.g. low percentage of farming, high industrial output and many service activities). The distribution of sex and labour force participation are similar to Switzerland as a whole. However, there were differences in the age distribution and the proportion of foreigners, which were both slightly higher in Basel. Still, it appears that Basel and its conurbation can be considered fairly representative for Switzerland regarding the main socio-demographic variables [110].
Data collection and processing could be improved as the registered order of methods employed and drug classes do not indicate their impact on the severity of the suicide attempt.
Further analysis of our data is necessary – and currently being implemented – to better understand the increased risk in certain subgroups and to characterise these groups more comprehensively. We will also link the collected quantitative data base with qualitative interviews to allow for a more comprehensive understanding of the socio-cultural phenomenon of suicide attempts and underlying problems and triggers of deliberate self-harm.
Appendix 1: WHO-Studie http://www.smw.ch/fileadmin/smw/pdf/smw-13759-Appendix.pdf
1 Platt S, Bille-Brahe U, Kerkhof A, Schmidtke A, Bjerke T, Crepet P, et al. Parasuicide in Europe: The WHO/EURO Multicentre Study on Parasuicide. I. Introduction and preliminary analysis for 1989. Acta Psychiatr Scand. 1992;85:97–104.
2 Federal Office of Public Health. Suicide and suicide prevention in Switzerland – Report in fulfillment of the postulate Widmer (02.3251). [Bundesamt für Gesundheit. Suizid und Suizidprävention in der Schweiz – Bericht in Erfüllung des Postulates Widmer (02.3251). Bern. Redaktionsteam: Salome von Greyerz, Elvira Keller-Guglielmetti; Wissenschaftliche Mitarbeit: Vladeta Ajdacic-Gross (Psychiatrische Universitätsklinik PUK Zürich), Martin Eichhorn (Psychiatrische Universitätsklinik PUK Basel), Konrad Michel (Universitäre psychiatrische Dienste UPD Bern), Regula Ricka (Bundesamt für Gesundheit)] 15. April 2005 [cited: 20.07.2010]. Available from: http://www.bag.admin.ch/themen/medizin/00683/01915/.
3 Shneidman ES. Suicide as psychache. J Nerv Ment Dis. 1993;181(3):145–7.
4 WHO European Ministerial Conference on Mental Health. Facing the Challenges, Building Solutions. Facing the Suicide Prevention. Helsinki. 12–15 January 2005 (29.10.2004) [cited: 14.03.2010]. Available from: http://www.euro.who.int/document/MNH/ebrief07.pdf.
5 Clayton D, Barcel A. The cost of suicide mortality in New Brunswick, 1996. Chronic Dis Can. 1999;20(2):89–95.
6 World Health Organisation [cited: 30.11.2011]. Available from: http://www.who.int/mental_health/prevention/suicide/country_reports/en/index.html
7 Frei A, Han A, Weiss MG, Dittmann V, Ajdacic-Gross V. Use of army weapons and private firearms for suicide and homicide in the region of Basel, Switzerland. Crisis. 2006;27(3):140–6.
8 Ajdacic-Gross V, Killias M, Hepp U, Haymoz S, Bopp M, Gutzwiller F, et al. Firearm suicides and availability of firearms: the Swiss experience. Eur Psychiatry. 2010;25(7):432–4.
9 Hepp U, Ring M, Frei A, Rössler W, Schnyder U, Ajdacic-Gross V. Suicide trends diverge by method: Swiss suicide rates 1969–2005. Eur Psychiatry. 2010;25(3):129–35.
10 Hepp U, Stulz N, Unger-Köppel J, Ajdacic-Gross V. Methods of suicide used by children and adolescents. Eur Child Adolesc Psychiatry. 2012;21(2):67–73.
11 Ajdacic-Gross V, Lauber C, Baumgartner M, Malti T, Rössler W. In-patient suicide – a 13-year assessment. Acta Psychiatr Scand. 2009;120(1):71–5.
12 Schnyder U, Valach L. Suicide attempters in a psychiatric emergency room population. Gen Hosp Psychiatry. 1997;19(2):119–29.
13 Hepp U, Moergeli H, Trier SN, Milos G, Schnyder U. Attempted suicide: factors leading to hospitalization. Can J Psychiatry. 2004;49(11):736–42.
14 Hoffmann-Richter U, Känzig S, Frei A, Finzen A. Suicide after discharge from psychiatric hospital. Psychiatr Prax. 2002;29(1):22–4.
15 Hepp U, Wittmann L, Schnyder U, Michel K. Psychological and psychosocial interventions after attempted suicide: an overview of treatment studies. Crisis. 2004;25(3):108–17.
16 Frei A, Schenker TA, Finzen A, Kräuchi K, Dittmann V, Hoffmann-Richter U. Assisted suicide as conducted by a “Right-to-Die”-society in Switzerland: a descriptive analysis of 43 consecutive cases. Swiss Med Wkly. 2001;131(25-26):375–80.
17 Bosshard G, Fischer S, Bär W. Open regulation and practice in assisted dying. Swiss Med Wkly. 2002;132(37-38):527–34.
18 Bosshard G, Ulrich E, Bär W. 748 cases of suicide assisted by a Swiss right-to-die organisation. Swiss Med Wkly. 2003;133(21-22):310–7.
19 Fischer S, Bosshard G, Faisst K, Tschopp A, Fischer J, Bär W et al. Swiss doctors’ attitudes towards end-of-life decisions and their determinants: a comparison of three language regions. Swiss Med Wkly. 2006;136(23-24):370–6.
20 Wasserfallen JB, Chioléro R, Stiefel F. Assisted suicide in an acute care hospital: 18 months’ experience. Swiss Med Wkly. 2008;138(15-16):239–42.
21 Fischer S, Huber CA, Furter M, Imhof L, Mahrer Imhof R, Schwarzenegger C, et al. Reasons why people in Switzerland seek assisted suicide: the view of patients and physicians. Swiss Med Wkly. 2009;139(23-24):333–8.
22 WHO-World Health Organisation. Health-for-all targets. The health policy for Europe. Summary of the updated edition. Copenhagen. September 1991. World Health Organisation. EUR ICP HSC 013; 1992.
23 Bille-Brahe U, Schmidtke A, Kerkhof A, De Leo D, Lönnqvist J, Platt S, et al. Background and introduction to the WHO/Euro Multicentre Study on Parasuicide. Crisis 1995;16(2):72–84.
24 Kerkhof A, Schmidtke A, Bille-Brahe U, De Leo D, Lönnqvist J. Attempted suicide in Europe. Leiden: DSWO Press; 1994. p. 3–14.
25 Schmidtke A, Bille-Brahe U, De Leo D, Kerkhof A, Bjerke T, Crepet P, et al. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989–1992. Results of the WHO/Euro Multicentre Study on Parasuicide. Acta Psychiatr Scand. 1996;93:327–38.
26 Bille-Brahe U, Andersen K, Wasserman D, Schmidtke A, Bjerke T, Crepet P, et al. The WHO/Euro Multicentre Study: risk of parasuicide and the comparability of the areas under study. Crisis. 1996;17(1):32–42.
27 Bille-Brahe U. WHO/EURO Multicentre Study on Parasuicide. Facts and figures. 2nd ed. Copenhagen: World Health Organization; 1999.
28 Neeleman J. A continuum of premature death: meta-analysis of competing mortality in the psychosocially vulnerable. Int J Epidemiol. 2001;30(1):154–62.
29 Bertolote JM, Fleischmann A. Suicidal behavior prevention: WHO perspectives on research. Am J Med Genet C Semin Med Genet. 2005;133C(1):8–12.
30 World Health Organisation. Suicide Prevention in Europe: The WHO European monitoring survey on national suicide prevention programmes and strategies. 2002 [cited: 14.03.2010]. Available from: http://www.euro.who.int/document/E77922.pdf.
31 Schmidtke A, Weinacker B, Löhr C, Waeber V, Michel K. Chapter 17 Suicidal Behaviour in Switzerland. In: Schmidtke A, Bille-Brahe U, Kerkhof A, De Leo D, editors. Suicidal Behaviour in Europe: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour; 1st ed. Göttingen: Hogrefe & Huber; 2004. p. 157–163.
32 Michel K, Knecht C, Kohler I, Sturzenegger M. Suizidversuche in der Agglomeration Bern. Schweiz Med Wschr. 1991;121:1133–9.
33 Reisch T, Maillart A, Michel K. Monitoring of suicidal behaviour in the agglomeration of Bern in the framework of the WHO/EURO Multicenter study on Suicidal Behaviour and the Bern alliance against depression. [Monitoring des suizidalen Verhaltens in der Agglomeration Bern im Rahmen der WHO/EURO Multicenter Study on Suicidal Behaviour und des Berner Bündnisses gegen Depressionen.] April 2007. Report: Available from: http://www.bag.admin.ch/themen/medizin/00683/03923/index.html.
34 Steffen T, Maillart A, Michel K, Reisch T. Monitoring of suicidal behaviour in the agglomeration of Bern from 2004 to 2010 in the framework of the WHO/Monsue Multicenter study on Suicidal Behaviour and the Bern alliance against depression. [Monitoring des suizidalen Verhaltens in der Agglomeration Bern der Jahre 2004 bis 2010 im Rahmen der WHO/Monsue Multicenter Study on Suicidal Behaviour und des Berner Bündnisses gegen Depressionen.] May 2011. Report: Available from http://www.bag.admin.ch/themen/medizin/00683/03923/index.html.
35 Kõlves K, Vecchiato T, Pivetti M, Barbero G, Cimitan A, Tosato F, et al. Non-fatal suicidal behaviour in Padua, Italy, in two different periods: 1992–1996 and 2002–2006. Soc Psychiatry Psychiatr Epidemiol. 2011;46(9):805–11.
36 Bronisch T, Wolfersdorf M. Definition von Suizidalität – Wie grenzen wir suizidales von nicht-suizidalem Verhalten ab? Suizidprophylaxe. 2012;39(2):41–50.
37 Statistical Office Basel-City. Binningerstrasse 6, Postfach, CH-4001 Basel, Switzerland. [cited: 14.03.2010]. Available from http://www.statistik-bs.ch/ on personal request (unpublished).
38 ICD-10 Classification of Mental and Behavioural Disorders with Glossary and Diagnostic Criteria for Research ICD-10: DCR-10. WHO Geneva: Churchill Livingstone; 1991.
39 Swiss Federal Statistical Office, health section, statistics on cause of death, Espace de l’Europe 10, CH-2010 Neuchâtel, Switzerland. [cited: 14.03.2010]. Available from: http://www.statistik.admin.ch on personal request (unpublished).
40 Baer C. Incidence of suicide attempts in the canton of Basel-City: analysis of the completeness of patient data within the WHO/EURO-NF study. [Häufigkeit von Suizidversuchen im Kanton Basel-Stadt: Analyse der Vollständigkeit der Patientenerfassung im Rahmen der WHO/EURO-NF-Studie]. Unpublished Master-Thesis in Public Health. University of Basel. 2006.
41 Lehfeld H, Althaus DA, Hegerl U, Ziervogel A, Niklewski G. Suicide attempts: results and experiences from the German Competency Network on Depression. Adv Psychosom Med. 2004; 26:137–43.
42 Hultén A, Jiang G-X, Wasserman D, Hawton K, Hjelmeland H, De Leo D, et al. Repetition of attempted suicide among teenagers in Europe: frequency, timing and risk factors. Eur Child Adolesc Psychiatry. 2001;10(3):161-9.
43 Bronisch T. Der Suizid: Ursachen – Warnsignale – Prävention. München: C.H. Beck; 2007.
44 Bille-Brahe U, Kerkhof A, DeLeo D, Schmidtke A. Chapter 3 Definitions and Terminology Used in the WHO/EURO Multicentre Study. In: Schmidtke A, Bille-Brahe U, Kerkhof A, De Leo D, editors. Suicidal Behaviour in Europe: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour; 1st ed. Göttingen: Hogrefe & Huber; 2004. P. 11–4.
45 Schmidtke A, Weinacker B, Löhr C, Bille-Brahe U, DeLeo D, Kerkhof A, et al. Chapter 4 Suicide and Suicide Attempts in Europe: An Overview. In: Schmidtke A, Bille-Brahe U, Kerkhof A, De Leo D, editors. Suicidal Behaviour in Europe: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour; 1st ed. Göttingen: Hogrefe & Huber; 2004. p. 15–28.
46 Batt A, Eudier F, Philippe A, Pommereau X. Chapter 14 Suicidal Behaviour in France. In: Schmidtke A, Bille-Brahe U, Kerkhof A, De Leo D, editors. Suicidal Behaviour in Europe: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour; 1st ed. Göttingen: Hogrefe & Huber; 2004. p. 133–140.
47 Hawton K, Arensman E, Wasserman D, Hultén A, Bille-Brahe U, Bjerke T, et al. Relation between attempted suicide and suicide rates among young people in Europe. J Epidemiol Community Health. 1998;52(3):191–4.
48 Murphy E, Kapur N, Webb R, Purandare N, Hawton K, Bergen H, et al. Risk factors for repetition and suicide following self-harm in older adults: multicentre cohort study. Br J Psychiatry. 2011;200(5):399–404.
49 Schmidtke A, Bille-Brahe U, DeLeo D, Kerkhof A, Weinacker B, Löhr C, et al. Chapter 5 Sociodemographic Characteristics of Suicide Attempters in Europe. In: Schmidtke A, Bille-Brahe U, Kerkhof A, De Leo D, editors. Suicidal Behaviour in Europe: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour; 1st ed. Göttingen: Hogrefe & Huber; 2004. p 29–43.
50 Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans, and attempts in the WHO World Mental Health Surveys. Br J Psychiatry. 2008;192:98–105.
51 Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Joyce PR, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med. 1999;29:9–17.
52 Bursztein Lipsicas C, Mäkinen IH, Apter A, De Leo D, Kerkhof A, Lönnqvist J, et al. Attempted suicide among immigrants in European countries: an international perspective. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):241–51.
53 Brückner B, Muheim F, Berger, P, Riecher-Rössler A. Characteristics of suicide attempts among Turkish immigrants living in Basel City – results from the WHO/ EURO-Multicentre study. Nervenheilkunde. 2011;30: 517–22.
54 Yilmaz TA, Riecher-Rössler A. Suicid attempts among first and second generation immigrants. Neuropsychiatr. 2008;22(4):261–7.
55 Yilmaz T, Riecher-Rössler A. Attempted suicide in immigrants from Turkey. A comparison with Swiss suicide attempters. Psychopathology. In Press.
56 Löhr C, Schmidtke A, Wohner J, Sell, R. Epidemiologie suizidalen Verhaltens von Migranten in Deuschland. Suizidprophylaxe. 2006;33(4), 171–6.
57 Grube M. Suizidversuche von Migranten in der Akutpsychiatrie. Nervenarzt. 2004;75: 681–7.
58 O’Donnell L, O’Donnell C, Wardlaw DM, Stueve A. Risk and resiliency factors influencing suicidality among urban African American and Latino youth. Am J Community Psychol. 2004;33:37–49.
59 Hjelmeland H, Groholt B. A comparative study of young and adult deliberate self-harm patients. Crisis. 2005;26(2):64–72.
60 Stravynski A, Boyer R. Loneliness in relation to suicide ideation and parasuicide: a population-wide study. Suicide Life Threat Behav. 2001;31(1):32–40.
61 Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–54.
62 Qin P, Mortensen PB. The impact of parental status on the risk of completed suicide. Arch Gen Psychiatry. 2003;60:797–802.
63 Garfinkel BD, Froese A, Hood, J. Suicide attempts in children and adolescents. Am J Psychiatry. 1982;139(10):1257–61.
64 Kaslow NJ, Webb Price A, Wyckoff S, Bender Grall M, Sherry A, Young S, et al. Person factors associated with suicidal behavior among African American women and men. Cultur Divers Ethnic Minor Psychol. 2004;10(1):5–22.
65 Garroutte EM, Goldberg J, Beals J, Herrell R, Manson SM; AI-SUPERPFP Team. Spirituality and attempted suicide among American Indians. Soc Sci Med. 2003;56:1571–9.
66 Dervic K, Oquendo MA, Grunebaum MF, Ellis S, Burke AK, Mann JJ. Religious affiliation and suicide attempt. Am J Psychiatry. 2004;161:2303–8.
67 Blum RW, Halcon L, Beuhring T, Pate E, Campell-Forrester S, Venema A. Adolescent health in the Caribbean: risk and protective factors. Am J Public Health. 2003;93:456–60.
68 Kranitz L, Abrahams J, Spiegel D, Keith-Spiegel P. Religious beliefs of suicidal patients. Psychol Rep. 1968;22(3):936.
69 Loewenthal KM, MacLeod AK, Cook S, Lee M, Goldblatt V. The suicide beliefs of Jews and Protestants in the UK: How do they differ? Isr J Psychiatry Relat Sci. 2003;40(3):174–81.
70 Lester D, Beck AT. Attempted suicide and religion. Psychology: A Journal of Human Behavior. 1974;11(3):32–4.
71 Morphew JA. Religion and attempted suicide. Int J Soc Psychiatry. 1968;14(3):188–92.
72 Spoerri A, Zwahlen M, Bopp M, Gutzwiller F, Egger M. Religion and assisted and non-assisted suicide in Switzerland: National Cohort Study. Int J Epidemiol. 2010;39(6):1486–94.
73 Rezaeian M. Suicide among young Middle Eastern Muslim females. Crisis. 2010;31(1):36–42.
74 Oquendo MA, Dragatsi D, Harkavy-Friedman J, Dervic K, Currier D, Burke AK, et al. Protective factors against suicidal behaviour in Latinos. J Nerv Ment Dis. 2005;193:438–43.
75 Meadows LA, Kaslow NJ, Thompson MP, Jurkovic GJ. Protective factors against suicide attempt risk among African American women experiencing intimate partner violence. Am J Community Psychol. 2005;36:109–21.
76 Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. 2003;160(6):1093–9.
77 Taylor R, Page A, Morrell S, Carter G, Harrison J. Socio-economic differentials in mental disorders and suicide attempts in Australia. Br J Psychiatry. 2004;185:486–93.
78 Bogdanovica I, Jiang GX, Löhr C, Schmidtke A, Mittendorfer-Rutz E. Changes in rates, methods and characteristics of suicide attempters over a 15-year period: comparison between Stockholm, Sweden, and Würzburg, Germany. Soc Psychiatry Psychiatr Epidemiol. 2011;46(11):1103–14.
79 Michel K, Ballinari P, Bille-Brahe U, Bjerke T, Crepet P, De Leo D, et al. Methods used for parasuicide: results of the WHO/EURO Multicentre Study on Parasuicide. Soc Psychiatry Psychiatr Epidemiol. 2000;35(4):156–63.
80 Canetto SS, Sakinofsky I. The gender paradox in suicide. Suicide Life Threat Behav. 1998;28(1):1–23.
81 Fekete S, Voros V, Osvath P. Gender differences in suicide attempters in Hungary: retrospective epidemiological study. Croat Med J. 2005;46(2):288–93.
82 Michel K, Arestegui G, Spuhler T. Suicide with psychotropic drugs in Switzerland. Pharmacopsychiatry. 1994;27(3):114-8.
83 Bille-Brahe U, Kerkhof A, De Leo D, Schmidtke A, Crepet P, Lonnqvist J, et al. A repetition-prediction study of European parasuicide populations: a summary of the first report from part II of the WHO/EURO Multicentre Study on Parasuicide in co-operation with the EC concerted action on attempted suicide. Acta Psychiatr Scand. 1997;95(2):81–6.
84 Gibb SJ, Beautrais AL, Fergusson DM. Mortality and further suicidal behaviour after an index suicide attempt: a 10-year study. Aust NZ J Psychiatry. 2005;39:95–100.
85 Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002; 181:193–9.
86 Schmidtke A, Weinacker B, Löhr C. Chapter 16 Suicidal Behaviour in Germany. In: Schmidtke A, Bille-Brahe U, Kerkhof A, De Leo D, editors. Suicidal Behaviour in Europe: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour; 1st ed. Göttingen: Hogrefe & Huber; 2004. p. 147–56.
87 Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–26.
88 Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–9.
89 Maier R, Stieglitz RDS, Marsch SC, Riecher-Rössler A. Patients in intensive care after a suicide attempts with legal drugs – risk profile and course. Fortschr Neurol Psychiat. 2011;79(5):283–9.
90 Eichhorn M. Suizidforschung – was nützen Zahlen in der Praxis? Psychiatrie (4). 2005:14–18.
91 Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–74.
92 Kreitman N. The coal gas story. United Kingdom suicide rates, 1960–71. Br J Prev Soc Med. 1976;30:86–93.
93 Carrington PJ. Gender, gun control, suicide and homicide in Canada. Arch Suicide Res. 1999;5:71–5.
94 Bridges FS. Gun control law (Bill C-17), suicide, and homicide in Canada. Psychol Rep. 2004;94:819–26.
95 Oliver RG, Hetzel BS. Rise and fall of suicide rates in Australia: relation to sedative availability. Med J Aust. 1972;2:919–23.
96 Lester D. The effect of the detoxification of domestic gas in Switzerland on the suicide rate. Acta Psychiatr Scand. 1990;82:383–4.
97 Reisch, T, Schuster U, Michel K. Suicide by jumping and accessibility of bridges: results from a national survey in Switzerland. Suicide Life Threat Behav. 2007;37(6):681–7.
98 Reisch T, Schuster U, Michel K. Suicide by jumping from bridges and other heights: social and diagnostic factors. Psychiatric Res. 2008;161(1):97–104.
99 Corcoran P, Reulbach U, Keeley HS, Perry IJ, Hawton K, Arensman E. Use of analgesics in intentional drug overdose presentations to hospital before and after the withdrawal of distalgesic from the Irish market. BMC Clin Pharmacol. 2010;10–6.
100 Rutz W, von Knorring L, Walinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand. 1989;80:151–4.
101 Rihmer Z, Belso N, Kalmar S. Antidepressants and suicide prevention in Hungary. Acta Psychiatr Scand. 2001;103:238–9.
102 Szanto K, Kalmar S, Hendin H. Rihmer Z, Mann JJ. A suicide prevention program in a region with a very high suicide rate. Arch Gen Psychiatry. 2007;64:914–20.
103 Hegerl U, Althaus D, Schmidtke A, Niklewski G. The alliance against depression: 2-year evaluation of a community-based intervention to reduce suicidality. Psychol Med. 2006;36(9):1225–33.
104 Neuner T, Hegerl U, Hajak G, Spiessl H. Reducing suicides through an alliance against depression? Gen Hosp Psychiatry. 2010;32(5):514–8.
105 Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293:2487–95.
106 Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine J.P, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–90.
107 Jenkins R. Addressing suicide as a public health problem. Lancet. 2002;359:813–4.
108 United Nations. Prevention of suicide guidelines for the formulation and implementation of national strategies. New York, NY: United Nations; 1996.
109 Jenkins, R., Singh, B. General population strategies of suicide prevention. In: Hawton, K.; van Heeringen, K., editors. International handbook of suicide and attempted suicide. 1st. Chichester, United Kingdom: John Wiley & Sons; 2000. p. 631–44.
110 Swiss Federal Statistical Office, Espace de l’Europe 10, CH-2010 Neuchâtel, Switzerland. Comparator tool. [cited: 14.03.2010]. Available from: http://www.bfs.admin.ch/bfs/portal/en/index/regionen/regionalportraets/comparator.html.
Funding / potential competing interests: Supported by the Federal Office of Public Health and the Otto David Bruderer Foundation. No other potential conflict of interest relevant to this article was reported.