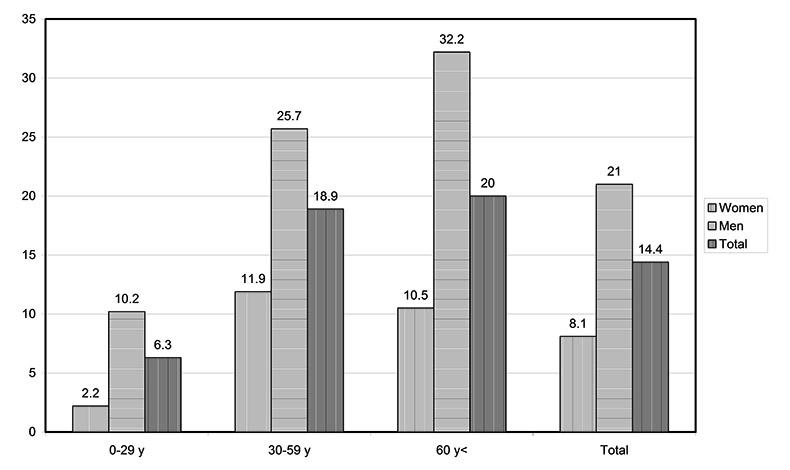
Figure 1
Suicide rate per 100,000 inhabitants and year including assisted suicide by age group and sex (n = 256).
DOI: https://doi.org/10.4414/smw.2013.13779
Several comprehensive studies or meta-analyses claim that more than 90% of suicides are suffering from mental illness [1–4]. This idea has recently been challenged [5], since the method used by most of the researchers, the psychological autopsy, is not sufficiently standardised (time between suicide and interviewing of informants, number of informants, instruments used) to draw a generalised conclusion [6]. It has been suspected that “worrying” [7] or “shame” [8], which are not psychiatric conditions, are in many cases the decisive precursor of suicide. The Swiss experience focuses in particular on another cause of suicide: physical illness. During the last decade there have been some 1,300 suicides per year, a figure that has remained stable. However, the share of assisted suicide has been growing continuously, attaining almost a quarter of all suicides [9]. Even a highly critical article on the practices of one of the Swiss “right to die societies”, at no point challenged the notion that the motivation for assisted suicide is in most cases a serious physical illness or disability and not a mental disorder [10]. The role of serious or lethal somatic illnesses as a motive for suicide, however, has not even been addressed in the comprehensive studies mentioned above. But even if one does not challenge the important role of mental disorder as a precursor of suicide, only a minority of suicide victims were in contact with the mental health system at the time of their suicide [11].
Contrary to van Praag’s assertion [7] that suicide rates have remained stable for decades, the annual rate of suicide in Switzerland reached a maximum in the early eighties and has since then declined continuously to the end of the millennium [12]. This phenomenon has also been observed in the Nordic countries [13]. In the case of Denmark, the improvement in the general quality of life has been suggested as a possible reason for this favourable development [14], Hepp and others consider that further reasons may be restriction of access to lethal materials and improvement in general psychiatric care [12]. None of these hypotheses, however, has been empirically tested for these countries in the period since the 1980s [12, 14]. It is interesting to note that the decline in suicide numbers in the Nordic countries started before the introduction of SSRI’s [13].
Rates and patterns of suicide differ considerably, not only between but also within countries [15]. For instance, suicide rates vary between cantons in Switzerland and even between urban and rural regions within cantons [16]. If one takes the number of practising psychiatrists per head of population as proxy for the quality of psychiatric care in a given region – the rate of available beds in psychiatric hospitals might be a poor indicator [17] – the conditions in some individual cantons must be excellent: 51/100,000 in Zurich and 41/100,000 in the north-western region of Switzerland. This exceeds the average in the EU (10-19/100,000) by a factor of 3 to 4 [17, 18]. Interestingly, cantons with a large number of practising psychiatrists such as Basle (northwestern Switzerland) or Zurich have a higher suicide rate than cantons with a smaller proportion of practising psychiatrists [18]. Two studies of suicides from these cantons have however shown that less than two fifths of suicide victims had ever received an official psychiatric diagnosis [16, 19]. Even assuming that some of these suicides were treated for a time by a practising psychiatrist, it is likely that in the course of their treatment they would have been referred for inpatient treatment once they showed symptoms of suicidality – either voluntarily or involuntarily, in accordance with Art. 397 a of the Swiss Civil Code (from 2013, Art. 426 Swiss Civil Code). Since there is no official register of patients treated by practising psychiatrists, it is impossible to verify how many of the suicides were exclusively treated by a practising psychiatrist. Hence it is still unclear why, in a country with excellent psychiatric facilities, fewer than 40% of all suicides have ever been seen by a public psychiatric service.
Suicides who never had contact to the mental health system might differ from former psychiatric patients with respect to residence (rural, urban), age or suicide method. For instance, in his study on suicides by weapons in Switzerland, Frei [19] found that young men without any psychiatric history and of good professional background are particularly prone to use their army weapons, which, as conscripts, they keep at home, as a means of suicide. We therefore thought it worthwhile to investigate differences between suicides with past contact to psychiatric facilities compared to suicides without such contact, with the intention of characterising the latter group.
Whenever the examining physician is in doubt about a natural cause of death, Swiss criminal procedure considers this as “an extraordinary death” (aussergewöhnlicher Todesfall) and he is obliged to inform the authorities, who then start an investigation [20]. In Canton Lucerne, it is the district attorney who then examines the case, assisted by a public health officer, who may recommend further proceedings such as a postmortem. Suicides and all other causes of death are registered in the Swiss mortality statistics, from which age, sex, method of suicide, somatic and psychiatric diagnosis at time of death, actual place of residence and country of origin can be extracted. Specific clinical information on suicides can only be obtained at the level of the cantons, e.g. by consulting the coroners’ files, which are usually kept in the local institutes of forensic medicine or offices of the district attorneys [19, 21] and – after permission has been given – cross-checking the names of the suicides in the registers of the local public psychiatric institution [19]. The region we have chosen for our investigation, Canton Lucerne, has a mixed rural-urban population. About 5% of the Swiss population live in Canton Lucerne, in which the number of practising psychiatrists is comparatively small (17/100,000) [18].
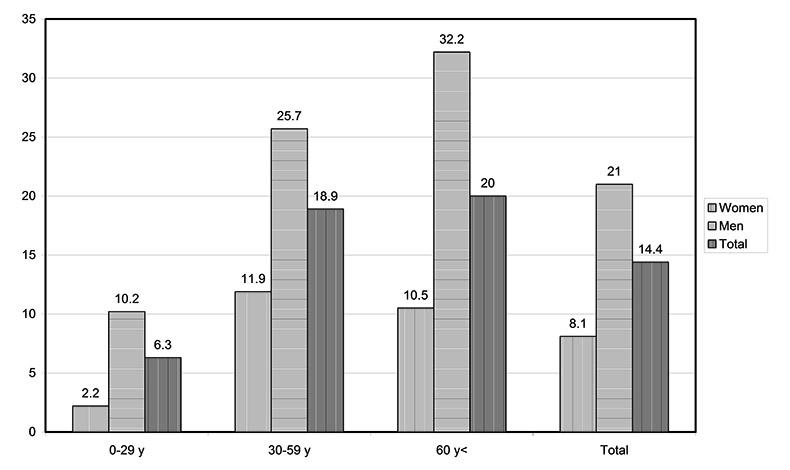
Figure 1
Suicide rate per 100,000 inhabitants and year including assisted suicide by age group and sex (n = 256).
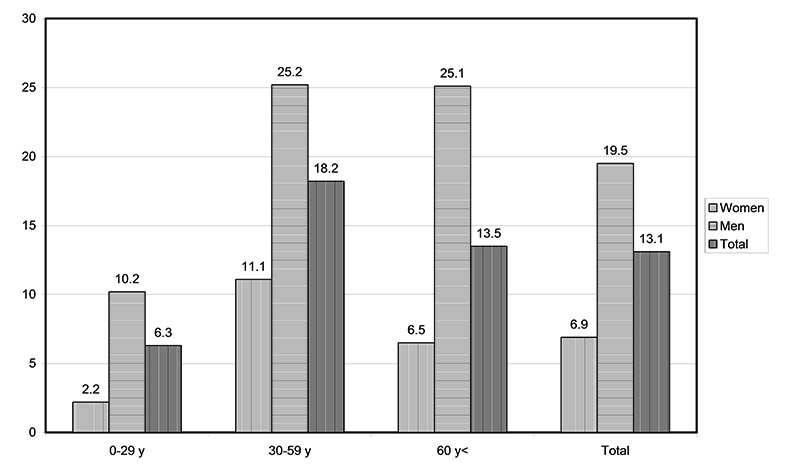
Figure 2
Suicide rate per 100,000 inhabitants and year by age group and sex, excluding assisted suicides (n = 232).
Our study was approved by the the local head district attorney and the Federal Commission for the Protection of Patients’ Rights in Medical Research.
In Lucerne the records of all extraordinary deaths are kept in the offices of the local district attorneys. After obtaining permission from the head district attorney, we selected all records classified as suicide or probable suicide (Chapter X 60 – X 84 according to ICD-10) for the years 2002–2006. Suicide methods which were less frequent than 5% of the total were aggregated as “others”. We cross-checked the data with the records kept in the archives of the cantonal psychiatric institutions. This was done with the permission of the Federal Commission for the Protection of Patients’ Rights in Medical Research. We extracted the following clusters of variables and their categories and subcategories from different disciplines:
Sociodemography: Age group, sex, profession, marital status, religion, country of origin.
Suicidology: Suicide methods, crime scene, suicide announcements, suicide notes, psychiatric history as the time lapse since the last contact with one of the respective psychiatric institutions. We analysed the data to determine whether we could identify any temporally and or locally related suicide clusters in the sense of particular buildings or bridges [22], copycat suicides in the sense of the "Werther effect” [23], homicide-suicide [24] or suicide pacts [25].
Health: Physical illness, official psychiatric diagnosis according to Chapter F 00 – 09 of ICD-10, informal remarks relating to mental health in the coroners’ files, obtained either from relatives or general practitioners (so called “police diagnosis”, i.e. comments like “depression”, “grief”, "frustration” or “addiction” which were coded by us according to Chapter F 00 – 09 of ICD-10).
We compared suicides with an established psychiatric diagnosis and suicides without an established diagnosis. Since patients whose last contact was three or more years prior to the suicide are considered to have the same suicide risk as the general population [26], such suicides were allocated to the group without psychiatric diagnosis. Hospitalised patients who committed suicide within up to 7 days after release were indicated as “acute inpatients”, patients who had been seen within 30 days by a psychiatric out-patients service were indicated as “acute outpatients”
In a second step, we examined only suicides without prior contact to the official psychiatric institutions and, using the same variables compared them with cases with and without “police diagnosis”.
According to the new practice of the Federal Statistical Office, which excludes assisted suicides from “ordinary” suicides in the mortality register [9], we excluded assisted suicides from the comparative analysis. On the other hand, since all extraordinary deaths from an overdose of any illicit drug were, despite some ambiguity [27], considered to be suicides by the authorities, they were included in our descriptive analyses.
All categorical variables were compared in bivariate analyses by the chi-square test. Each variable which yielded significant results was included in a stepwise binary logistic regression. The dependent variable was coded for suicides with and without established psychiatric diagnoses. Similarly, we selected all suicides who had no prior contact to the official psychiatric institutions and coded suicides with and without “police diagnosis” as dependent variables. Here we also included all variables with significant differences in bivariate analyses in a stepwise binary logistic regression. The calculations were performed using SPSS Version 18 [SPSS Inc., Statistical Package for Social Sciences].
| Table 1: Group differences between suicides with and without an established psychiatric diagnosis. | |||||||
| Variable | Total sample | Former psychiatric treatment | No psychiatric diagnoses | ||||
| N | % | N | % | N | % | p | |
| Total | 232 | 100 | 81 | 34.9 | 151 | 65.1 | |
| Sociodemographic variables | |||||||
| Sex | |||||||
| Male | 170 | 73.3 | 52 | 64.2 | 118 | 78.1 | 0.029 |
| Female | 62 | 26.7 | 29 | 35.8 | 33 | 21.9 | 0.029 |
| Residence | |||||||
| Urban | 135 | 58.2 | 44 | 54.3 | 91 | 60.3 | n. s. |
| Rural | 97 | 41.8 | 37 | 45.7 | 60 | 39.7 | n. s. |
| Civil state | |||||||
| Spouse (married, common law) | 80 | 34.5 | 21 | 25.9 | 59 | 39.1 | n. s. |
| Single (also widowed) | 152 | 65.5 | 60 | 74.1 | 92 | 60.9 | n. s. |
| Nation | |||||||
| Swiss | 207 | 89.2 | 72 | 88.9 | 135 | 89.4 | n. s. |
| Foreigner from EU | 15 | 6.5 | 5 | 6.2 | 10 | 6.6 | n. s. |
| Foreigner outside the EU | 10 | 4.3 | 4 | 4.9 | 6 | 4.0 | n. s. |
| Religion | |||||||
| Catholic | 132 | 56.9 | 52 | 64.2 | 80 | 53.0 | n. s. |
| Protestant | 24 | 10.3 | 7 | 8.6 | 17 | 11.3 | n. s. |
| Other/no religion | 76 | 32.8 | 22 | 27.2 | 54 | 35.8 | n. s. |
| Age groups | |||||||
| 0–29 | 41 | 17.7 | 16 | 18.5 | 25 | 17.2 | n. s. |
| 30–59 | 139 | 59.9 | 59 | 72.8 | 80 | 53.0 | 0.003 |
| 60< | 52 | 22.4 | 7 | 8.6 | 45 | 29.8 | <0.001 |
| Professions | |||||||
| Disabled | 32 | 13.8 | 20 | 24.7 | 12 | 13.9 | 0.001 |
| Blue-collar | 45 | 19.4 | 19 | 23.5 | 26 | 17.2 | n. s. |
| White collar/Graduate | 71 | 30.6 | 20 | 24.7 | 51 | 33.8 | n. s. |
| Unemployed/Asylum Seeker | 32 | 13.8 | 12 | 14.8 | 20 | 13.2 | n. s. |
| Unskilled/Housewife | 15 | 6.5 | 5 | 6.2 | 10 | 6.6 | n. s. |
| Retired | 37 | 15.9 | 5 | 6.2 | 32 | 21.2 | 0.002 |
| Health | |||||||
| No illness | 162 | 69.8 | 47 | 58.0 | 115 | 76.2 | 0.007 |
| Chronic illness | 54 | 23.3 | 31 | 38.3 | 23 | 15.2 | <0.001 |
| Lethal illness | 16 | 6.9 | 3 | 3.7 | 13 | 8.6 | n. s. |
| Suicidological variables | |||||||
| Suicide methods | |||||||
| Others | 48 | 20.7 | 18 | 22.2 | 30 | 19.9 | n. s. |
| Total Fire weapons | 55 | 23.7 | 6 | 7.4 | 49 | 32.5 | <0.001 |
| Army weapon | 32 | 13.8 | 5 | 6.2 | 27 | 17.9 | 0.016 |
| Private gun | 23 | 9.9 | 1 | 1.2 | 22 | 14.6 | 0.001 |
| Hanging | 58 | 25.0 | 19 | 23.5 | 39 | 25.8 | n. s. |
| Leaping | 19 | 8.2 | 7 | 8.6 | 12 | 7.9 | n. s. |
| Intoxication | 52 | 22.4 | 31 | 38.3 | 21 | 13.9 | <0.001 |
| Legal drugs | 30 | 12.9 | 16 | 19.8 | 14 | 9.3 | 0.038 |
| Illegal drugs | 22 | 9.5 | 15 | 18.5 | 7 | 4.6 | 0.002 |
| Suicide note | s. | ||||||
| Yes | 85 | 36.6 | 25 | 30.9 | 60 | 39.7 | n. s. |
| No | 147 | 63.4 | 56 | 69.1 | 91 | 60.3 | n. s. |
| Suicide announcement | |||||||
| Yes | 138 | 59.5 | 71 | 87.7 | 67 | 44.4 | <0.001 |
| No | 94 | 40.5 | 10 | 12.3 | 84 | 55.6 | <0.001 |
| Crime scene | |||||||
| Home | 137 | 59.1 | 46 | 56.8 | 91 | 60.3 | n. s. |
| Public | 85 | 36.6 | 34 | 35.8 | 51 | 37.1 | n. s. |
| Institution | 10 | 4.3 | 6 | 7.4 | 4 | 2.6 | n. s. |
| n. s. = not significant | |||||||
| Table 2: Predictors of suicides with and without psychiatric diagnosis. | |||||
| Explanatory variables | Regression coefficient | Odds-Ratio | 95% confidence interval | p | |
| Sociodemographic variables | |||||
| Sex | |||||
| Female | 1 (reference category) | ||||
| Male | –.393 | .675 | .299 | 1.523 | .344 |
| Profession | |||||
| White collar/Graduate | 1 (reference category) | ||||
| Disabled | .021 | 1.021 | .320 | 3.260 | .972 |
| Retired | –1.974 | .139 | .044 | .439 | .001 |
| Blue-collar | .590 | 1.804 | .688 | 4.729 | .230 |
| Unemployed/Asylum Seeker | .121 | 1.129 | .387 | 3.295 | .825 |
| Unskilled/Housewife | –.452 | .636 | .146 | 2.765 | .546 |
| Suicidological variables | |||||
| Suicide methods | |||||
| Others | 1 (reference category) | ||||
| Army weapon | –.527 | .591 | .166 | 2.100 | .416 |
| Private gun | –1.847 | .158 | .018 | 1.403 | .098 |
| Hanging | –.158 | .854 | .360 | 2.026 | .721 |
| Leaping | .523 | 1.686 | .441 | 6.451 | .445 |
| Legal drugs | 1.519 | 4.567 | 1.153 | 18.085 | .031 |
| Illegal drugs | 1.436 | 4.204 | 1.302 | 13.577 | .016 |
| Suicide announcement | |||||
| No | 1 (reference category) | ||||
| Yes | 2.402 | 11.042 | 4.751 | 25.666 | <0.001 |
| Health | |||||
| No illness | 1 (reference category) | ||||
| Chronic illness | 1.158 | 3.185 | 1.310 | 7.741 | 0.011 |
| Lethal illness | –.858 | 424 | .125 | 1.435 | 0.168 |
Between 2002 and 2006, there were 256 suicides in the canton of Lucerne, 24 or 9.4% of these being assisted suicides. The mean suicide rate over these five years of all suicides was 14.4/100,000 and 13.1/100,000 after excluding assisted suicides. The exclusion of assisted suicides had an important impact on the suicide rate related to age.
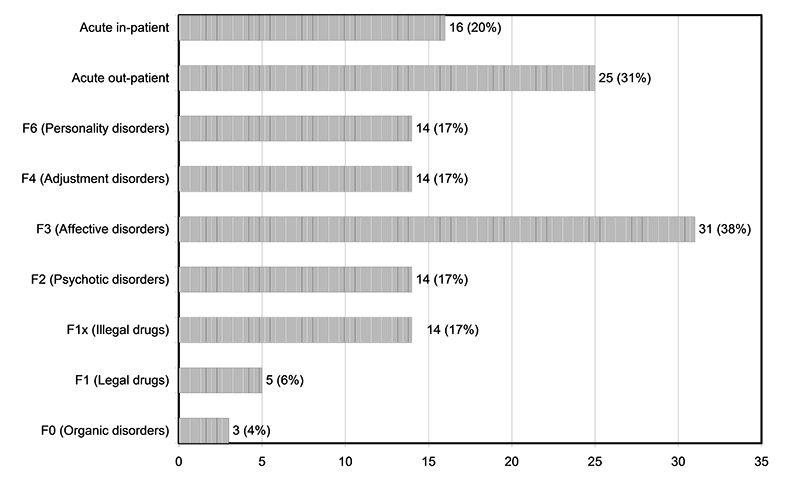
Figure 3
Psychiatric diagnoses and relevant information on suicides with psychiatric files (n = 81).
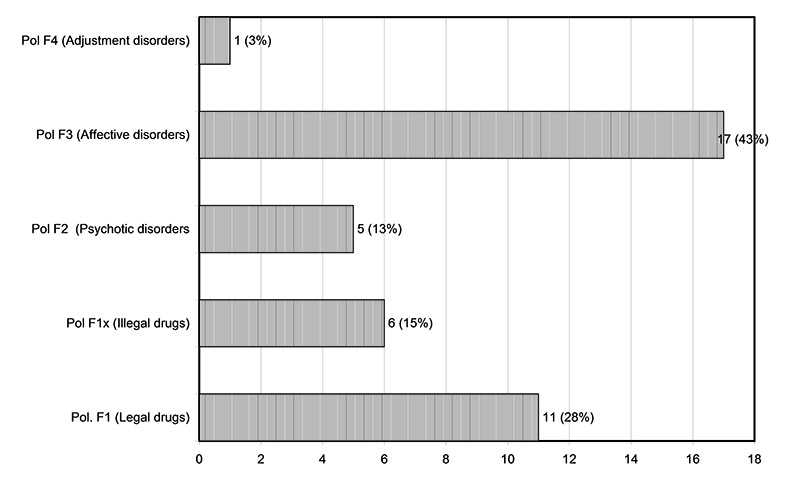
Figure 4
Psychiatric diagnoses from police files (“police diagnosis”, n = 40).
81/232 (34.9%) of the suicide victims had been registered once or several times over the last three years as patients in one of the public psychiatric institutions, while 151/232 suicides (65.1%) had not been registered. A small majority of those with an established psychiatric diagnosis, i.e. 41/81 (51%), were in contact with the psychiatric services at the time of suicide. This corresponds to 17.7% of the 232 unregistered suicides. The most frequently established diagnosis, in 31/81 patients (38%), was “affective disorder” (F3 according to ICD 10).
40/151 (26.5%) of suicides without a diagnosis established by the public psychiatric service had references relating to mental problems in their files, making it possible to establish a psychiatric diagnosis. Affective disorder (“depression”) was again the most frequent diagnosis, viz. 17/40 (43%)
Among the suicides with neither an established nor a “police” diagnosis, there was only one case of “homicide-suicide” – with four additional victims. This corresponds to a rate of 0.05 cases/100,000/y. Apart from that, we could not identify any suicide “hot-spot” and found no evidence of a copy-cat suicide.
Table 1 shows all variables and the cross-tabulations of the variables related to the two groups for established psychiatric diagnosis – “yes” or “no”. The most frequent suicide methods – shooting, hanging and poisoning – showed almost identical frequency, but shooting was significantly more frequent among the suicides with no psychiatric diagnosis, poisoning among those with a psychiatric diagnosis and hanging was evenly distributed among the two groups. It is noteworthy that hanging was used in only three cases (5%) as a suicide method in an institution (prison, clinic)
According to the logistic regression model (table 2), suicide victims with an established psychiatric diagnosis were more likely to have died from legal and illegal drugs (legal drugs: regression coefficient 1.519 , OR = 4.567, confidence interval 1.153–18.085, p = 0.31; illegal drugs: regression coefficient 1.436, OR = 4.204, confidence interval 1.302–13.577, p = 0.16), to have suffered from a chronic somatic illness (regression coefficient 1.158, OR=3.185, confidence interval 1.310–7.741, p = 0.011) and to have announced their suicide (regression coefficient 1.158, OR = 11.042, confidence interval 4.751–25.666, p <0.001); on the other hand, retired suicide victims were seven times more likely never to have contacted a public psychiatric service (regression coefficient –1.974, OR = 0.134, confidence interval 0.044–0.439).
Table 3 shows the cross-tabulations of the variables related to the two groups “police diagnosis“ “yes“ or “no”. There was only one foreigner with a “police diagnosis”. “Hard” or “impulsive” suicide methods like shooting or hanging were not considered by the coroner to indicate a psychiatric disorder – in contrast to intoxication with legal drugs.
According to the logistic regression model (table 4), suicide victims without a police diagnosis were about 2.6 times more likely to be male (regression coefficient –.975, OR = 0.377, confidence interval 0.145–0.979, p = 0.045) and also 2.6 times more likely to have left a suicide note (regression coefficient –.969, OR = 0.380, confidence interval 0.155–0.929, p = 0.34).
| Table 3: Group differences of suicides without established psychiatric diagnosis split into with and without “police diagnosis”. | |||||||
| Variable | Total Sample | Police diagnosis | No police diagnoses | ||||
| N | % | N | % | N | % | p | |
| Total | 151 | 100 | 40 | 26.5 | 111 | 73.5 | |
| Sociodemographic variables | |||||||
| Sex | |||||||
| Male | 118 | 70.3 | 24 | 60.0 | 94 | 84.7 | <0.003 |
| Female | 33 | 26.7 | 16 | 40.0 | 17 | 15.3 | 0.003 |
| Religion | |||||||
| Catholic | 80 | 53.0 | 22 | 55.0 | 58 | 52.3 | n. s. |
| Protestant | 17 | 11.3 | 7 | 17.5 | 10 | 9.0 | n. s. |
| Other/no religion | 54 | 32.7 | 11 | 27.5 | 43 | 38.7 | n. s. |
| Professions | |||||||
| Disabled | 12 | 7.9 | 7 | 17.5 | 5 | 4.5 | 0.016 |
| Blue-collar | 26 | 17.2 | 3 | 7.5 | 23 | 20.7 | n. s.* |
| White collar/Graduate | 51 | 33.8 | 13 | 32.5 | 38 | 34.2 | n. s. |
| Unemployed/Asylum Seeker | 20 | 13.5 | 2 | 5.0 | 18 | 16.2 | n. s. |
| Unskilled/Housewife | 10 | 6.6 | 7 | 17.5 | 3 | 2.7 | 0.004 |
| Retired | 32 | 21.2 | 8 | 20.0 | 24 | 21.6 | n. s. |
| Suicidological variables | |||||||
| Suicide means | |||||||
| Others | 30 | 19.9 | 5 | 12.5 | 25 | 16.1 | n. s. |
| Total fire weapons | 49 | 32.5 | 10 | 25.0 | 39 | 35.1 | n. s. |
| Army weapon | 27 | 17.9 | 4 | 10.0 | 23 | 20.7 | n. s. |
| Private gun | 22 | 14.6 | 6 | 15.0 | 16 | 14.4 | n. s. |
| Hanging | 39 | 25.8 | 10 | 25.0 | 29 | 26.1 | n. s. |
| Leaping | 12 | 7.9 | 4 | 10.0 | 8 | 7.9 | n. s. |
| Intoxication | 21 | 13.9 | 11 | 27.5 | 10 | 9.0 | 0.007 |
| Legal drugs | 14 | 7.2 | 6 | 15.0 | 8 | 9.3 | 0.009 |
| Illegal drugs | 7 | 4.6 | 5 | 12.5 | 2 | 1.8 | n. s. |
| Suicide note | |||||||
| Yes | 60 | 39.7 | 9 | 22.5 | 51 | 45.9 | 0.014 |
| No | 91 | 60.3 | 31 | 77.5 | 60 | 54.1 | 0.014 |
| Suicide announcement | |||||||
| Yes | 67 | 44.4 | 22 | 55.0 | 45 | 40.5 | n. s. |
| No | 84 | 55.6 | 18 | 45.0 | 66 | 59.5 | n. s. |
| n. s. = not significant | |||||||
| Table 4: Predictors of suicides without established psychiatric diagnosis. | |||||
| Explanatory variables | Regression coefficient | Odds-Ratio | 95% Confidence interval | p | |
| Sociodemographic variables | |||||
| Sex | |||||
| Female | 1 (reference category) | ||||
| Male | –.975 | .377 | .145 | .979 | .045 |
| Profession | |||||
| White collar/Graduate | 1 (reference category) | ||||
| Disabled | 1.151 | 3.162 | .805 | 12.417 | .099 |
| Retired | –.180 | .835 | .286 | 2.436 | .741 |
| Blue-collar | –.972 | .378 | .094 | 1.519 | .170 |
| Unemployed/Asylum Seeker | –1.274 | .280 | .054 | 1.454 | .130 |
| Unskilled/housewife | 1.295 | 3.651 | .721 | 18.498 | .118 |
| Suicidological variables | |||||
| Suicide note | |||||
| No | 1 (reference category) | ||||
| Yes | –.969 | .380 | .155 | .929 | .034 |
In this study the number of suicides who had never been seen by a public psychiatric service was notably high, even slightly higher than in other studies from Switzerland [16, 19] or from Denmark [14]. Our practice of counting suicides without contact to public psychiatric mental services during the preceding three years as suicides without an established psychiatric diagnosis may explain this difference. Since our figure of suicides without an established psychiatric diagnosis is similar to that found in the region of Basle or in Canton Zurich with their much greater concentrations of practising psychiatrists, we do not think this is mainly a problem of scarce psychiatric facilities. The fact that the 41 of 80 cases (51%) with an established psychiatric diagnosis committed suicide within a very short time of the last contact to a psychiatric service (seven days for inpatients, 30 days for outpatients) is a well known phenomenon [18, 29], but is not the subject of this paper.
Our study showed similar results for the frequency of suicide methods to those found in the above-mentioned studies from other parts of Switzerland, namely the high frequency of suicide with guns [16, 19], even though our study sample was smaller. The exclusion of assisted suicide had an important impact on the distribution of suicide rates in the different age categories, since the age group with the highest suicide rate is no longer the oldest, but the intermediate age group [2, 30].
Hanging, shooting and intoxication were the most frequent suicide methods. Contrary to our expectations [15], neither shooting, which might be used impulsively in critical situations, or jumping from heights, which the severely mentally ill might be expected to use [31, 32], differentiated between the two groups after checking for sociodemographic factors or health.
The fact that suicides with a psychiatric diagnosis were more closely associated with the use of illicit or legal drugs was no surprise. This may be because users of illicit drugs have a better chance of having been registered as psychiatric patients, or because legal drugs were prescribed by doctors.
In our sample suicides with former contact to the psychiatric health system were three times more likely to have suffered from a chronic somatic disorder than those without former contact. Since it is a well-known fact that people suffering from a mental disorder are likely to die prematurely – not only by suicide, but from somatic illnesses [33] – this might suggest that the process which eventually led to the suicide was probably more acute than for suicides without former contact to the mental health system.
Our finding that retired persons were seven times more likely to be in the group without a registered mental health problem is somehow inconsistent with de Leos’ notion of the “paradox of suicide in old age”: De Leo wondered why old people who have overcome many crises in their lives should commit suicide at all when the natural end of life is close anyway [34]; according to our results, however, some still do.
The clearest difference was in suicide announcement, which might be explained by the fact that “suicidality” as such was a motive for referral to psychiatric care or treatment; it is, however, noteworthy that a large group of those without a psychiatric diagnosis also announced their suicide.
Even though almost two thirds of all suicides had no established diagnosis, there were 40 cases where a putative mental disorder was noted, allowing us to hypothesise about a diagnosis. These diagnoses, however, relied on the impressions of lay people and were therefore less differentiated than diagnoses established in psychiatric institutions. The diagnosis “personality disorder”, for example, was absent and alcohol related problems were more frequent. This observation is in accordance with the meta-analysis of studies on psychiatric disorders and suicide by Bertolote [35], who found that the diagnosis of suicides who had been treated in psychiatric institutions differed considerably from the diagnoses of other suicides; he actually challenged the latter’s accuracy. However, we do not agree with Hoffmann-Richter’s notion that the information taken from police reports of suicides is rather meaningless [36].
We have no explanation for the finding that female suicides were more likely to be given a “police diagnosis”.
Suicides without any hint of a psychiatric problem were more likely to have left a suicide note than those with a remark in the files; almost half of them had an urge to communicate with posterity or to explain themselves somehow. Our finding is contrary to the general notion in the literature that there is no difference between suicides who have left a suicide note and those who have not [37, 38]. The rate of suicide notes in the whole sample was comparatively high [39, 40].
In our sample firearms were the second most frequent suicide method. In contrast to the study of Frei [19], army weapons were more frequent than private weapons, even among former psychiatric patients. A people's initiative requesting that army weapons be no longer left to Swiss conscripts to keep at home was recently rejected by the majority of voters. Nevertheless, the authorities no longer deny the danger of misuse of army weapons, and ammunition is no longer given to conscripts to keep at home [41]. The use of private (or illegal) guns is more difficult to handle; the proposal to establish a national register was also rejected recently [41]: The only homicide-suicide in our study was committed by a farmer without a criminal record whose three weapons had been confiscated by the police four months before the event, after he had threatened his estranged wife; he committed the act with a gun obtained from an unknown source.
However, the most frequent method, hanging, was also equally distributed betweensuicides with and without an established psychiatric diagnosis. This is of concern in that this method is easy to use and besides the prevention of its use in institutions – which was rare in our study – there exist no specific strategies for prevention [42].
In this retrospective study we chiefly used established data such as sex, age, suicide methods or the psychiatric diagnosis from medical files. We are aware that in our retrospective study the label “established psychiatric diagnosis” does not necessarily signify that a psychiatric disorder was causal or that suicides without an established diagnosis did not suffer from a mental disorder all the same. Some suicides with a mental disorder might have been treated only by a practising psychiatrist without our knowledge. As there are comparatively few practising psychiatrists in Canton Lucerne [18], it can be presumed that the number of such suicides in our study is small. We presume that some of the mentally ill who had been treated only by a practising psychiatrist or general practitioners were registered as “police diagnosis”. It should also be mentioned that in his study of 100 suicides “outside the mental health care system” Owens was unable to establish a psychiatric diagnosis in 28 cases [11].
Even though our sample is small, we still consider that it is representative of the whole of Switzerland since we investigated a mixed rural/urban population. The small sample size might be of particular relevance for rare events such as homicide-suicides; the rate in our study of 0.05/100,000/y was five times smaller than that found in the Basel region [19].
This study deals with cases that occurred six to eleven years ago, so that the accuracy of its data might be open to challenge. Contrary to countries like Greece, however, Switzerland has scarcely been affected in recent years by an economic crisis, a factor which is known to contribute to a rise in suicide rates [43]. We feel that the growing acceptance of assisted suicide in the whole of Switzerland might lead to a rise in its rate; the ongoing national debate surrounding suicide by gun could have had a favourable influence on the general suicide rate in Lucerne too.
Nevertheless, we cannot suggest any factor which might have had an influence on the distribution between suicides with and without established psychiatric diagnosis.
The majority of suicides in the canton of Lucerne had never been in contact with an official psychiatric service and had fewer somatic health problems than those who had. About a fourth of this group, however, showed some special features which seemed noteworthy to the coroner. Suicides without any hint of a mental problem in their files were more likely to have left a suicide note than suicides with a diagnosis. Leenaars [44] asserted that suicide notes were usually written minutes before the act and were an “ultrapersonal” document, allowing an unbiased view of the suicide’s feelings. Since many suicides never looked for professional help and never attracted their environment’s attention, but still left a suicide note, we believe it worthwhile to analyse the contents of suicide notes and compare them, to achieve a better understanding of what motivated them.
1 Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1996;205–28.
2 Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: A worldwide perspective. World Psychiatry. 2002;1:181–5.
3 Arsenault-Lapierre G, Kim C, Turecki K. Psychiatric diagnoses in 3275 Suicides: a meta-analysis. BMC Psychiatry. 2004:37/4.
4 Cavanagh JTO, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychological Medicine. 33; 395–405.
5 Hjelmeland H, Dieserud G, Dyregrov K, Knizek BL, Leenaars AA. Psychological autopsy studies as diagnostic tools: Are they methodologically flawed? Death Studies. 2012;36:605–26.
6 Pouliot L, de Leo D. Critical issues in psychological autopsy studies. Suicide and Life-Threatening Behaviour. 2006;36:491–510.
7 Van Praag HM. A stubborn behaviour: the failure of antidepressants to reduce suicide rates. World Biol Psychiatry. 2003;4:181–91.
8 De Leo D. Suicide prevention is far more than a psychiatric business. World Psychiatry. 2004;3(3):155–6.
9 Junker Ch. Assisted suicide and suicide in Switzerland. Federal Statistical Office 2012.
10 Frei A, Schenker TA, Finzen A, Kräuchi, K, Dittmann V, Hoffmann-Richter U. Assisted suicide as conducted by a ‘Right-to-Die’-society in Switzerland: A descriptive analysis of 43 consecutive cases. Swiss Med Wkly. 2001;131:375–80.
11 Owens C, Booth N, Briscoe M, Lawrecne, C, Lloyd K. Suicide Outside the Care of Mental Health Services. A Case-Controlled Psychological Autopsy Study. Crisis. 2003;24/3:113–21.
12 Hepp U, Ring M, Frei A, Rössler W, Schnyder U, Ajdacic-Gross V. Suicide trends diverge by method: Swiss suicide rates 1969–2005. European Psychiatry. 2010;25:129–35.
13 Zahl PH, De Leo D, I Ekeberg Ø, Hjelmeland H, Dieserud G. The relationship between sales of SSRI, TCA and suicide rates in the Nordic countries- Available from: http://www.biomedcentral.com/1471-244X/10/62
14 Qin Ping, Nordentoft M, Høyer H, Agerbo E, Laursen TM, Mortensen PB. Trends in suicide risk associated with hospitalized psychiatric illness: A case-control study based on Danish longitudinal register. J Clin Psychiatry. 2006;67(12):1936–41.
15 De Leo D. Struggling Against Suicide. The need for an integrative approach. Crisis. 2002;23(1):23–31.
16 Klein SD, Bischoff Ch, Schweitzer W. Suicides in the canton of Zurich(Switzerland). Swiss Med Wkly. 2010;140:w13102
17 European Communities 2004. The State of Mental Health in the European Union. Available from: http://ec.europa.eu/health/archive/ph_projects/2001/monitoring/fp_monitoring_2001 frep_06
18 Camenzind P, Schuler D, Sturny I, Roth M. Psychiatrische und psychotherapeutische Versorgung in ambulanten Praxen in der Schweiz. Baseline 2006“ Schweizerisches Gesundheitsobservatorium, Obsan: 10.11.2008.
19 Frei A, Han A, Weiss MG, Dittmann V, Ajdacic-Gross V. Use of army weapons and private firearms for suicide and homicide in the Region of Basle. Crisis. 2006;27:140–6.
20 Mund T, Bär W: Rechtmedizinische Aspekte beim plötzlichen Todesfall. Schweiz Med Forum. 2005;5:129–35.
21 Haenel T, Elsässer PN: Double suicide and homicide-suicide in Switzerland. Crisis. 2000;21:122–5.
22 Reisch T, Schuster U, Michel K. Suicide by jumping and Accessibility of Bridges: Results from a National Survey in Switzerland. Suicide Life Threat Behav. 2007;37(6):681–7.
23 Phillips DP. The influence of suggestion on suicide: substantive and theroretical implications of the Werther effect. Am Sociol Rev. 1974;39/3:340–54.
24 Marzuk PM, Tardiff K, Hirsch CS. The epidemiology of murder-suicide. JAMA. 1992;267:3179–83.
25 Fishbain D, Aldrich T. Suicide Pacts: International Comparisons. J Clin Psychiatry. 1985;46:154–7.
26 Steer RA, Brown GK, Beck At. When does the daily hazard rate for committing suicide stabilize in Psychiatric outpatients? Psychological Reports. 2006;99:462–4.
27 Laberke PJ, Bartsch Ch. Trends in methadone-related deaths in Zurich. Int J Legal Med. 2010;124:381–5.
28 Meehan J, Kapur, Hunt IM, Turnbull B, Robinson J, Bickley H et al. Suicide in mental health in-patients and within 3 months of discharge. Br J Psychiatry. 2006;188:129–34.
29 Hoffmann-Richter U, Känzig S, Frei A, Finzen A. Suizid nach der Entlassung aus der psychiatrischen Klinik. Psychiatr Prax; 29/1:22-4.
30 Leenaars AA. Can a theory of suicide predict all “suicides” in the elderly? Crisis. 2003;24(1):7–16.
31 Cantor CH, Hill MA, McLachlan EK. Suicide and related behaviour from river bridges. A clinical perspective. Br J Psychiatry. 1989;155:829–35.
32 Reisch T, Schuster U, Michel K. Suicide by jumping from bridges and other heights: Social and diagnostic factors. Psychiatric Res. 2008;161:97–104.
33 Colton CW, Manderscheid RW. Congruencies in Increased Mortality Rates, Years of Potential Life Lost, and Causes of Death Among Public Mental Health Clients in Eight States. Prev Chronic Dis. 2006;3(2):A42. Available from: http://www.ncbi. nlm.nih.gov/pmc/articles/pmc 1563985 http://www.ncbi. nlm.nih.gov/pmc/articles/pmc 1563985
34 De Leo D. Reasons for living and the paradox of suicide in old age. Crisis. 1998;19(4): 147–51.
35 Bertolote JM, Fleischmann A, de Leo D, Wassermann D. Psychiatric Diagnosis and Suicide: Revisiting the Evidence. Crisis. 2006;25(4):147–55.
36 Hoffman-Richter U, Frei A, Finzen A. Suizidmotive aus der Sicht der Ermittlungsbehörde eines Schweizer Kantons. Suizidprophylaxe. 1997;4:170–2.
37 O’Connor RC, Sheehy NP, O’Connor DB. A thematic analysis of suicide notes. Crisis. 1999;20(3):106–14.
38 Foster T. Suicide note themes and suicide prevention. Int J Psychiatry Med. 2003;33(4):323–31.
39 Shneidmann ES. The psychological autopsy. Suicide Life Threat Behav. 1981;11(4):325–40.
40 Eisenwort B, Berzlanovich A, Heinrich M, Schuster A, Chocholous P, Lindorfer S, Eisenwort G. Suizidologie: Abschiedsbriefe und ihre Themen. Nervenarzt. 2007;78(6):672. 674–8.
41 Michel K. Suizid und die Waffengesetzgebung in der Schweiz. Oder: Die aufrechten Söhne Tells. Suizidprophylaxe. 2011;38/2:76–8.
42 Gunnell D, Bennewith O, Hawton K, Simkin S, Kapur N. The epidemiology of suicide by hanging: a systematic review. Int J Epidemiology. 2005;34:433–42.
43 Kentikelenis A, Karanikolos M, Papanicolas, Basu Sanjay, McKee M, Stuckler D. Health effects of financial crisis: omens of a Greek tragedy. Lancet. 2011;378:1456–7.
44 Leenaars AA. Suicide: A multidimensional malaise. Suicide Life Threat Behav. 1996;26(3):221–36.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.