The impact of brief psychotherapy centred on parenthood on the anxio-depressive symptoms of mothers during the perinatal period
DOI: https://doi.org/10.4414/smw.2013.13769
Amir
Moayedoddin, Dominik A.
Moser, Nathalie
Nanzer
Summary
OBJECTIVES: Depression and anxiety are major causes of distress amongst parents during the perinatal period. Their pervasive effects on the parents’ self-confidence, on the parent-infant relationship and on the child’s development have been well documented. The aims of the present study were to describe the psychological characteristics of mothers consulting during the perinatal period and to assess the effect of brief Psychotherapy Centred on Parenthood (PCP) on the mothers’ depressive and anxiety symptoms. The evolution of the mother-infant relationship is also documented. PCP is a brief mother-infant psychotherapy which focuses on the mother-infant relationship as well as the mother’s mental representations in order to reduce her psychological conflicts.
METHOD: Thirty-four mothers consulting an infant-parent outpatient clinic were assessed with respect to depression, anxiety, global functioning, severity of symptoms and the quality of their adaptation to the infant (T1). They were offered a brief PCP with an average of seven sessions. Outcome measures were collected after the end of the therapy (T2).
RESULTS: Overall, 28 of 34 mothers completed the therapy (83%), and 23 participated in the post-therapy evaluation. Paired samples t-tests showed that completers of PCP displayed significant improvement in post-treatment measures of depression (EPDS: t = 5.13; p <0.001), anxiety (STAI-State: t = 3.06; p = 0.006), clinical impression (CGI: n = 21; t = 4.50; p <0.001), and global functioning (GAF: t = –5.05; p <0.001). The quality of adaptation in the infant-parent relationship showed a tendency to improve (PIRGAS: t = –1.98; p = 0.062).
CONCLUSIONS: These preliminary results suggested that providing PCP to this sample of consulting mothers is feasible and accompanied by high rate of clinical and functional improvement.
Introduction
Perinatal depression (PD) is a major public health issue not only in Switzerland but also all over the world [3]. It affects an average of 20% of women during pregnancy [30] and 13% during the first year postpartum. The detection of this form of depression is not easy for the woman herself and for her circle. Indeed, several symptoms such as fatigue and sleep disturbance may be considered as normal and ignored. During the postpartum period, the woman is concerned with her baby and has a tendency not to focus on her own needs and suffering. Professionals caring for women do not always investigate for depressive symptoms or attribute them to pregnancy or recent delivery, as the women themselves do. Recently, Marcus [29] found that only 18% of women who met criteria for major depressive disorder received treatment during the perinatal period. Therefore, depression is one of the most under-diagnosed and under-treated conditions at this period of life [9].
Antenatal mood disorder is associated with several complications during pregnancy such as excessive weight gain, increased substance use or premature birth [29]. Postpartum depression has negative effects on the mother’s and infant’s functioning as well as on the quality of the mother-baby relationship [50]. Mothers are less sensitive to their child and they tend to be less affectively attuned and possibly less responsive to their infant’s needs. Infants demonstrate fewer vocal, visual and corporal interactions, but more crying, feeding and sleeping disorders [46]. The consequences for infants are serious and include less secure attachments and poorer emotional, behavioural and cognitive development than infants of non-depressed women [31, 34]. Even when the mother’s depression is in remission, infants may be at risk of disturbances such as an insecure attachment, behavioural problems, cognitive and verbal delays, and emotional dysregulation [46]. Furthermore, untreated depression presents a high risk of relapse [5]. On the other hand, a recent systematic review showed that there are associations between successful treatment of parents’ depression and improvement in children’s symptoms and functioning [25]. Anxiety is also a frequent symptom among young mothers and it is not always easy to differentiate it from depressive symptoms [51]. Correia and Linhares [10] found that high levels of maternal anxiety in the prenatal phase were associated with obstetrical problems, emotional damage to foetal development, and behavioral problems in childhood and adolescence. It also has negative impacts on depression and on the mother-infant relationship. It is also considered as a predictor of postnatal depression [4]. Few studies have examined the correlation between anxiety and other perinatal mood disorders and their relationship to the child’s development.
Once the depressive and anxiety symptoms are identified, an effective and acceptable intervention ought to be proposed to the mothers, but few efficient early interventions have been validated for PD [33]. According to the STAR*D research [47], there is no statistical difference between different treatment modalities for depression, that is, pharmacotherapy, psychotherapy or a combination of the two methods. While psychotropic medication is often effective, most women, despite their mental illness, are reluctant to take medication while pregnant [44] or while breastfeeding [27]. Relatively few studies of antidepressive medication for this population have been conducted compared with psychological interventions, and overall most interventions have not been assessed in comparison with control or other active treatment modalities [48]. Studies show that mothers are more likely to choose a psychotherapeutic intervention over medication owing to concerns about its effects on the developing child in utero or through breastfeeding [17, 43]. Most studies show that psychological interventions are effective [26, 41]. In a recent meta-analysis, Cuijpers noted that most psychological interventions during the perinatal period result in a reduction of depressive symptoms [15]. Interpersonal, cognitive-behavioural or psychodynamic psychotherapy and other supportive interventions like telephone-based support, counseling by a health visitor or partner support are more effective than usual care or a waiting-list [19]. Recent findings show that individual psychotherapy is superior to group psychotherapy to treat PD, and interpersonal therapy components were found to have greater effect than interventions including a cognitive-behavioural component [48].
Nevertheless, some studies have suggested that therapies in which only the mother is involved may not be associated with better child outcomes or improvements in the mother-infant relationship in the long term [20, 37, 40]. Treating postpartum depression may not be sufficient for improving cognitive development, attachment and attitude in infants and toddlers [25]; thus interventions for PD should include an approach focused on the parenting role. Mother-infant psychotherapies expressly include the infant; they are focused on the mother-infant interactions and on maternal capacities in order to increase sensitivity and responsiveness [6]. They also address issues that have arisen as a result of becoming a mother or coping with PD [40, 42]. Research on the efficacy of mother-infant treatments has demonstrated improvements in the mother-infant relationship, increased maternal sensitivity and responsiveness, and better child outcomes, both initially and over time [8, 21]. Some studies have also demonstrated an improvement in self-esteem and a reduction in parenting stress and maternal depression [7, 22, 32]. These dyadic approaches are vital to protect the child against the negative consequences of maternal mental health problems in the long-term [40]. There is a need to develop research on interventions focused on parenthood and to study their impact not only on maternal mental health but also on the parent-infant relationship [38].
Psychotherapy Centred on Parenthood (PCP) is an intervention that is adapted from the Geneva mother-infant psychotherapeutic model [14] and can be offered throughout pregnancy and the postnatal period, with or without the presence of the child. This therapy, published in a manual [39], has recently been tested on a non-clinical sample of pregnant women and produced a significant decrease of depression scores after four therapeutic sessions with continued of improvement after 6 months postpartum [38]. PCP has not yet been tested on a clinical sample of patients and we found no paper describing the anxio-depressive state of mothers consulting a parent-infant outpatient unit. The aim of this research is to describe the psychological characteristics of mothers consulting a psychiatric infant-parent outpatient clinic during the perinatal period and to assess the effects of PCP on the mothers’ depressive and anxiety symptoms, and on the mother-infant relationship.
Hypotheses:we wanted to test our clinical impression that most mothers consulting a parent-infant outpatient clinic suffered from depression and/or anxiety symptoms during the perinatal period. We hypothesise that patients have significantly less anxiety, less depression and a better relationship with their child after PCP therapy than before.
Furthermore, we were interested in whether highly anxious and depressive subjects at the pretreatment assessment session differed from less anxious and depressive subjects with respect to their clinical improvement after therapy.
Method
Study individuals
The research procedures were approved by the ethical committee of the University Hospital of Geneva (HUG). Between October 2009 and March 2011, the study was proposed to a total of 65 mothers who consulted during their perinatal period (from pregnancy to 1 year postpartum) at an outpatient parent-infant clinic of the Geneva University Hospital (Switzerland) for a problem with their infant (crying, sleeping, feeding problems), with the relationship to the infant or with their own feelings (depression or anxiety). After the mother called the outpatient clinic, a research clinician called her back to propose that she participate in the study, which included a pretreatment assessment session of about 90 minutes and a post-treatment session. They were assured that the treatment would be the same with or without the inclusion in the study.
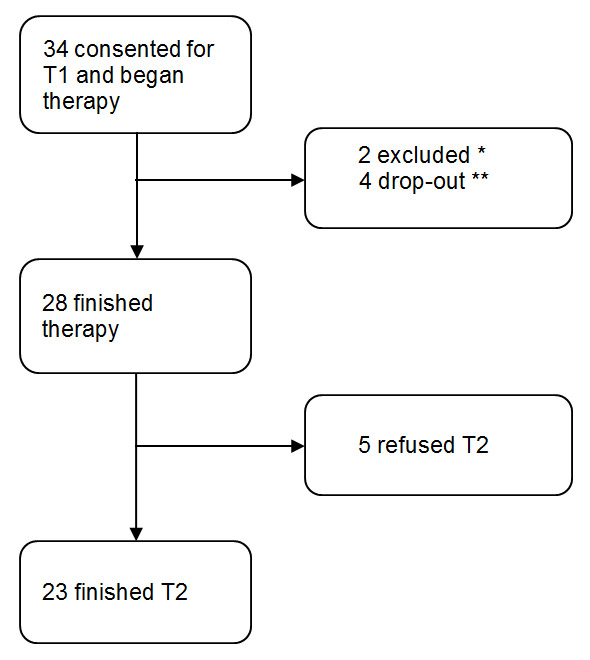
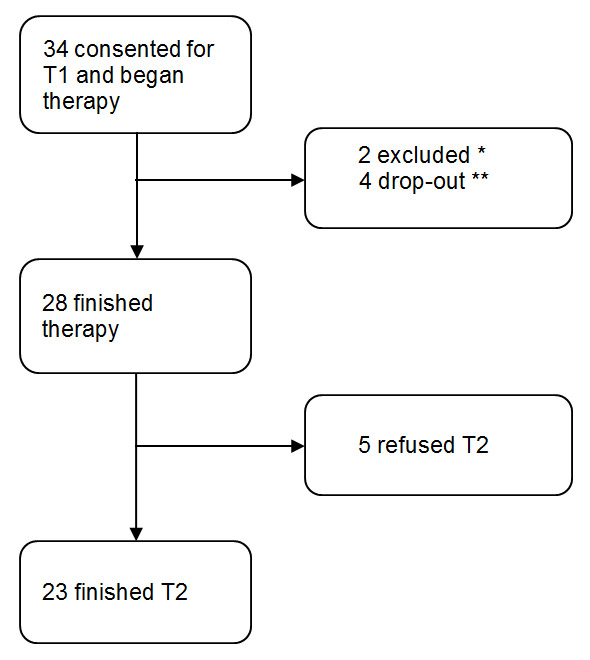
Figure 1
Participant rates at each stage of the trial.
* Procedure bias: One woman consulted for her elder son and not her baby. The other woman had her T1 session after the first therapy session.
** All four stopped after the first session and refused T2. Two stopped because they already had another therapy in parallel, the two others did not give the reason.
Exclusion criteria were a poor level of French, mental retardation and a severe psychiatric condition needing intensive care. All other mothers who agreed to participate to the study were included. Thirty-four mothers accepted and were included in the study and 31 refused to participate. The reasons of refusal were: refusing to talk to a person (a research clinician) other than the therapist, need of urgent care or lack of time. The participant rates at each stage of the trial are shown in figure 1. Of the 33 children born, 17 (52%) were male and 16 (48%) were female. The gender of the last child was not known because the woman stopped the therapy before delivery.
Study design
The mothers who agreed by phone to take part in the study were convened for a pretreatment assessment session (T1) with an experienced child-psychiatric research clinician, who was previously trained and experienced in the use of the different study instruments described below. The mothers filled out an informed written consent form and were interviewed by the research clinician for socio-demographic features, depression and anxiety symptoms, depression diagnosis, global functioning, clinical global assessment and the quality of adaptation of the infant-parent relationship.
Then all the participants were sent to one of the four child psychotherapists for the PCP. These four psychotherapists were well-experienced psychoanalytic psychiatrists or psychologists with more than five years of experience in parent-infant psychotherapy and in PCP. The mothers were seen once a week at the beginning and then the sessions were spaced once every two or three weeks. The number of sessions of therapy was decided by both the therapist and the mother according to the therapeutic need, with a maximum of 10 sessions. The termination criteria were based on the therapist’s clinical evaluation and the mother’s own account of her improvement of mood, quality of relationship with her baby or the improvement of the baby’s symptoms. When additional therapy was indicated by the therapist, mothers were referred to an adult psychiatrist after the PCP.
At the end of the treatment, mother and infant were sent to the post-therapy evaluation session (T2) for assessment of the outcome measures by the same research clinician that they met at T1. The research clinician was unaware of the content and modalities of the therapy.
The PCP
This brief intervention centred on parenthood is based on the Geneva mother-infant psychotherapeutic model [14, 28], focusing on the mother-infant relationship and on maternal mental representations. Several studies have shown that this model of intervention has a positive impact on the mother’s mood and infant symptomatology during the first years of life [13]. We adapted this protocol to the pre- and postpartum period and developed the PCP. A manual of this model has been published [39]. The goal of treatment goal is to identify and modify the nature of the core conflicting themes concerning motherhood that are responsible for the woman’s feelings of guilt and mood disturbances. In our intervention, the therapist is active in creating an alliance and in remaining centred on the identified focus. The identification of the focus allows the mother to recognise and work out the distortions of her mental representations concerning herself and her (future) baby. These unbalanced representations are frequently related to the woman’s past history and to her relationship with her own mother. Fava and collegues have demonstrated that, during pregnancy, the woman's image of herself, her foetus and her own mother evolves in a way that reflects her relational history and associated conflicts and representations [18]. Free associations and dream narratives are encouraged in order to identify the unconscious beliefs in connection with future parenthood: What parent am I going to be? What child am I going to have? What kind of parents did I have? What kind of a child was I? What was my attitude toward siblings? Clinical practice of brief mother-infant psychotherapy shows that the main psychic themes observed during pregnancy and early motherhood are: (1) the fear of not being a good mother, (2) the fear of reproducing the patterns that the mother suffered during her childhood, (3) the existence of a too high maternal ideal. These conflicts are connected to unconscious or unresolved bereavements in the woman’s past, with more or less conscious reproaches addressed to her parents. The conflicts are turned against herself when she becomes a mother. The intervention leads to an improvement of the mother’s mood by relieving the anxiety and guilt, allowing her to engage in an active psychological process, and to be emotionally ready for motherhood. After birth, the presence of the child allows the therapist to work not only on maternal mental representations, but also on the actual interactions between the mother and her infant. At that period, the antenatal internal conflicts are frequently externalised and acted out in the mother-baby relationship. In the postpartum sessions, the therapist examines these interactions and shows to the mother how her internal conflicts are enacted in her relationship with the child. His or her work is centred on helping the mother recognise these aspects.
Study instruments
To evaluate the depressive and anxiety symptoms in women, the following instruments were used:
– The depression part of the Structured Clinical Interview for DSM IV [1], Axis I Disorders (SCID-I) was used to diagnose a major depression.
– The Edinburgh Postnatal Depression Scale (EPDS) is a questionnaire widely used to measure depressive symptoms during the postpartum period [11]. According to Murray and Carothers [36], the EPDS is a reliable method to identify depressive mothers. It has also been validated during pregnancy [37]. We used the French version validated by Guedeney and Fermanian [23].
– The State-Trait Anxiety Inventory (STAI) is a self-report instrument that differentiates between the temporary condition of state anxiety and the longstanding quality of trait anxiety [49]. The STAI consists of two scales containing 20 items each, one addressing state anxiety and the other addressing trait anxiety. Scores range from 20 to 80, with higher scores correlating with greater anxiety.
To evaluate the level of maternal functioning and quality of the mother-infant relationship three instruments were used:
– The Global Assessment Functioning (GAF) is a numeric scale included in the DSM-IV [1], which is generally used by mental health clinicians and physicians to rate the social, occupational, and psychological functioning of adults. This scale rates the person's functioning during a specified period on a continuum from psychiatric illness to health. The scale value ranges from 1 (hypothetically sickest person) to 100 (hypothetically healthiest person).
– The Clinical Global Impression (CGI) Gravity and Improvement are 7-point scales that measure symptom severity, treatment response and efficacy in treatment studies of patients with mental disorders [24].
– The Parent–Infant Relationship Global Assessment Scale (PIR-GAS) is a 90-point scale providing a continuous scale of the quality of the infant–parent relationship adaptation, ranging from “dangerously impaired” to “well-adapted”. The PIR-GAS is a supplement to the DC-03 diagnostic classification [52].
Statistical analysis
We first analysed general demographics descriptively for the sample as a whole. We then compared baseline demographic and clinical characteristics of those who dropped out or were withdrawn from the study with the rest of the sample using independent t-tests for continuous variables and chi-squared analyses for categorical variables.
To evaluate changes in symptoms from baseline to post-treatment for treatment completers, we used paired t-tests (whenever normality could be assumed as tested using the Shapiro-Wilks test) to analyse the change from T1 to T2 and between completers and noncompleters. This was the case for the EPDS, STAI, GAF and PIRGAS scores.
We used repeated measures analysis of variance (ANOVA) to test for group differences in development throughout therapy. All statistical tests used an alpha level of 0.05.
Since the Shapiro-Wilks was positive for the CGI, we used Wilcoxon tests to test for differences in this measure and Spearmans correlations instead of Pearsons.
We also performed additional analysis that had not been previously planned. We did this in order to better understand whether there is a central factor whose outcome is particularly important. We thus correlated the final EPDS and STAI to all measures at T1 in order to see which would predict them best. We were also particularly interested to see whether low final levels of depression affected the course of mother-child relationship and thus split the patients into outcome groups using the EPDS and applied to them a repeated measure ANOVA of the PIRGAS.
Results
Sample characteristics
Tables 1 and 2 summarise the socio-demographic and psychological characteristics of the total group, the completers and the noncompleters. Twenty of the total sample of 34 were of Swiss nationality (59%), 18 (53%) had a high level of education and 25 (73%) had a good level of family income. The average age was 34 (19–46) years. Twenty-seven (79%) of the participants were employed. Thirty-three were living with their husband or partner (97%). The infants’ median age was 3 (1–12) months at the first evaluation interview. Nine of the 23 infants of the completers had health problems at birth (39%). The most frequent health problems were icterus (67%), and nutritional (22%) and gastrointestinal problems (33%).

Figure 2
Change in PIRGAS scores between T1 and T2 for the group that showed heightened depressive symptoms at T2 (EPDS >9) vs the less depressed group (EPDS ≤9).
Error bars depict standard deviation.
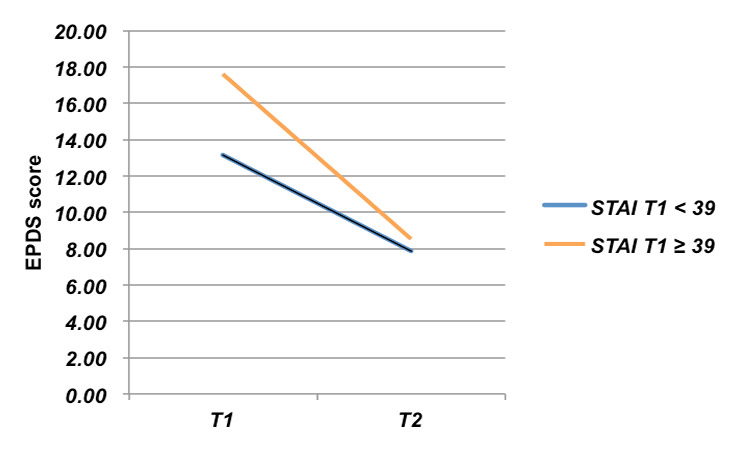
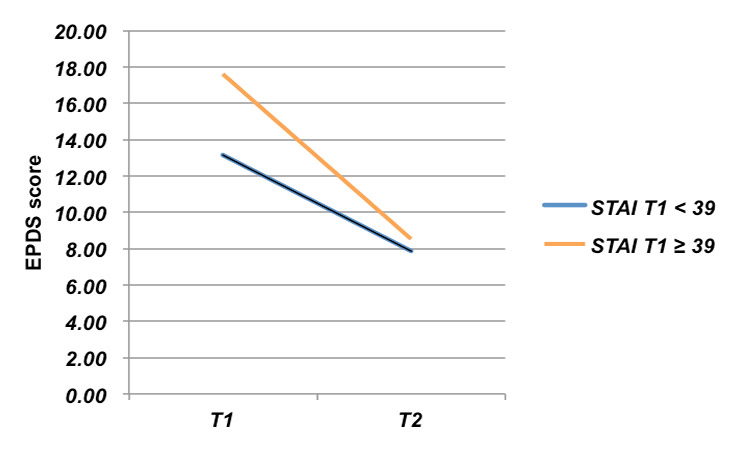
Figure 3
Change in depression depending on initial anxiety levels.
Nineteen women (56%) suffered from major depression (SCID) with 25 (73%) suffering from depressive symptoms (EPDS ≥12). The total mean EPDS score was 15 (1–27; standard deviation (SD) = 7). Twenty-four (70%) of the mothers suffered from anxiety symptoms (STAI state >39), with a mean state STAI score of 43.2 (21–69; SD = 12). Twenty-five (73%) of the mothers had a moderate to low global functioning (GAF <70), with a mean GAF score of 60 (45–85; SD = 11) and 10 (29%) showed a significant perturbation of the relationship with their child (PIRGAS <70) (mean PIRGAS = 75; 45–91; SD = 12).
The most frequent risk factors for depression were: hyperemesis during pregnancy (n = 23; 68%), stressful life events during the past 12 months (n = 21; 62%), family psychiatric history (n = 20; 59%), known past depression (n = 16; 47%) and marital conflict (n = 15; 44%).
Noncompleters did not differ from completers in any demographic and clinical category, with the exception of a lower number of children (df = 32; t = 2.38; p = 0.025) and a lower employment grade (df = 32; t = 2.39; p = 0.023).
|
Table 1:Socio-demographic characteristics for participants enrolled in the study. |
|
Variable
|
Total n = 34
|
Completers n = 23
|
Noncompletersn = 11
– dropouts n = 6
– refused T2 n = 5
|
| Mother’s age: mean (SD) |
34 (5.3) |
33.5 (4.4) |
35 (7.7) |
| Father’s age: mean (SD) |
35.8 (6.7) |
35.5 (6.5) |
36 (7.7) |
| Infant’s age in months: mean (SD) |
4 (3.16) |
4.62 (3.3) |
2.7 (2.6) |
| Pregnant at T1: n (%) |
3 (9%) |
2 (9%) |
1 (9%) |
| Infant’s sex (male): n (%) |
17 (52%) |
11 (50%) |
5 (45%) |
| Swiss nationality: n (%) |
20 (59%) |
12 (52%) |
8 (73%) |
| University-level education: n (%) |
18 (53%) |
14 (61%) |
4 (36%) |
| Employed: n (%) |
27 (79%) |
16 (70%) |
4 (36%) |
| Other children at home: n (%) |
10 (29%) |
9 (39%) |
1 (9%) |
| Income: n (%)
– less than 15’000 CHF
– 15’000 to 60’000 CHF
– 60’000 to 110’000 CHF
– more than 110’000 CHF |
0
3 (8%)
6 (16%)
25 (76%) |
0
1 (4%)
3 (13%)
19 (83%) |
0
2 (18%)
3 (27%)
7 (55%) |
| Living with partner: n (%) |
33 (97%) |
22 (96%) |
11(100%) |
| Marital conflicts: n (%) |
15 (44%) |
8 (35%) |
7 (64%) |
| Lack of support from partner: n (%) |
9 (26%) |
6 (26%) |
3 (27%) |
| Lack of support from family: n (%) |
13 (38%) |
9 (39%) |
4 (36%) |
| Poor relationship with own mother: N (%) |
18 (62%) |
10 (53%) |
8 (80%) |
| Previous miscarriage: n (%) |
8 (22%) |
3 (13%) |
5 (45%) |
| Unplanned pregnancy: n (%) |
11 (32%) |
6 (26%) |
5 (45%) |
| Hyperemesis during pregnancy: n (%) |
23 (68%) |
16 (73%) |
2.70 (1%) |
| Birth weight (g): mean (SD) |
3302 (595.0) |
3295 (595.1) |
3317 (628.8) |
| Infant’s health problem at birth: n (%) |
10 (31%) |
7 (32%) |
3 (27%) |
| Stressful life events during last 12 months: n (%) |
21 (62%) |
13 (56%) |
8 (73%) |
| Family psychiatric problems (depression and bipolar): n (%) |
20 (59%) |
15 (65%) |
5 (45%) |
| Past depression known: n (%) |
16 (47%) |
12 (52%) |
4 (4%) |
| Past psychiatric problem known: n (%) |
12 (35%) |
7 (30%) |
5 (45%) |
Post-treatment outcomes for the sample as a whole
The average number of therapy sessions was 6.91 (1‒10; SD = 3.10). Paired sample t-tests showed that the 23 subjects who completed the therapy and the T2 interview experienced a significant improvement at almost all the scales. They differ significantly between T1 and T2 in STAI state (mean difference: 9.4, SD = 14.7, n = 23 t = 3.06; p = 0.006), EPDS (mean difference: 7.9, SD = 7.4, n = 23 t = 5.13; p <0.001), CGI (mean difference: 1.5, SD = 1.5, n = 21 Z = –3.27; p = 0.001) and GAF (mean difference: –16.5, SD = 15.1, n = 21 t = –5.05; p <0.001), and have a tendency to differ in the PIRGAS (mean difference: –8.8, SD = 19.8, n = 20 t = –1.98; p = 0.062) (table 3).
At the end of treatment, the number of major clinical depressions (SCID) declined from 13 to 3, which is significant (Wilcoxon signed ranks test; n = 19; Z = 2.83; p = 0.005). In terms of response to treatment (defined a priori as ≥50% reduction in symptoms), 13 (56%) of completers experienced at least a 50% reduction in their EPDS depression scores, and the percentage in the “depressed” range of functioning (EPDS ≥12) had decreased from 73% to 26%. On the STAI, 13 (56%) of completers reported at least a 50% reduction in anxiety scores and 19 (83%) had scores in the “not anxious” range at T2, increased from 7 (30%) at T1. The number of women presenting a good level of global functioning (GAF ≥70) increased from 6 (26%) at T1, to 19 (81%) at T2.
At T1, the STAI trait is correlated with the EPDS (n = 23; r = 0.44; p = 0.037), while the STAI state only shows a tendency to correlate with the EPDS. At T2, both STAI correlate with the EPDS (STAI state: n = 23; r = 0.58; p = 0.004 STAI trait: n = 23; r = 0.76; p <0.001).
The effect of treatment and initial anxiety and depression levels
We performed repeated measures ANOVAs using the STAI state at T1 (STAI ≥39) as a between-subject factor to differentiate the anxious subjects from the nonanxious subjects, and the EPDS, PIRGAS and GAF at T1 and T2 as within-subject factors (see table 4 for numerical values). The EPDS (df = 21; F = 18.51; p <0.001; fig. 3) and GAF (df = 19; F = 17.588; p <0.001) showed the main changes with time (T1 to T2), but no measure showed a significant interaction. No significant effect of group could be found.
The less anxious (STAI state <39) subjects (n = 7) changed significantly from T1 to T2 in GAF (mean difference = –13.3, SD = 8.9, n = 5; t = 3.673; p = 0.014), but no significant difference between T1 and T2 could be found for the EPDS and PIRGAS. The more anxious group (STAI state ≥39; n = 16) also showed a significant change on the GAF over time (mean difference = –17.7, SD = 17.0, n = 15; t = 4.02; p = 0.001). They also changed significantly in the EPDS (mean difference = 9.1, SD = 6.9, t = 5.34; p <0.001), and had a tendency to change in the PIRGAS (mean difference = –10.3, SD = 21.0, n = 14; t = 1.83; p = 0.090).
We also performed repeated measures ANOVAs using the EPDS at T1 (EPDS ≥12) as a between-subject factor to differentiate the depressive subjects from the nondepressive subjects, and the EPDS, PIRGAS, and GAF at T1 and T2 as within-subject factors (see table 4 for numerical values). The STAI (df = 21; F = 6.92; p = 0.016), GAF (df = 19; F = 17.02, p = 0.001), showed the main changes with time (T1 to T2), but no measure showed significant interactions.
|
Table 2: Psychological characteristics for participants enrolled in the study (T1). |
|
Variable
|
Totaln = 34
|
Completersn = 23
|
Noncompleters n = 11
‒ dropouts n = 6
– refused T2 n = 5
|
| EPDS: mean (SD) |
15 (7.2) |
16.26 (6.94) |
15.09 (7.89) |
| STAISTATE:mean (SD) |
43.2 (12.6) |
44.39 (11.90) |
40.64 (14.18) |
| STAI TRAIT: mean (SD) |
49.8 (12.5) |
47.35 (11.06) |
54.82 (14.32) |
| GAF: mean (SD) |
60 (11.0) |
62.33 (10.29) |
58.36 (9.60) |
| PIRGAS: mean (SD) |
75 (11.9) |
71.00 (12.20) |
75.10 (11.93) |
| CGI: mean (SD) |
4 (1.2) |
3.78 (1.20) |
4 (1.15) |
Additional analysis
Predictive correlations of EPDS and STAI
EPDS at T2 was predicted by EPDS (r = 0.446; p = 0.033), STAI trait (r = 0.642; p = 0.001, see fig. 3) and GAF (r = –0.415, p = 0.049) at T1, but not by STAI state and PIRGAS. STAI state at T2 is predicted by STAI state (r = 0.436; p = 0.038), STAI trait (r = 0.574; p = 0.004), at T1, but not by any other measure.
Prediction of PIRGAS at T2
PIRGAS at T2 was not predicted by PIRGAS at T1 or any other clinical measure assessed at T1. PIRGAS score at T2 is highly correlated with EPDS at T2 (n = 21; r = –0.80; p <0.001) and CGI (n = 21; spearman r = 0.76; p <0.001) and GAF (n = 21; r = 0.76; p <0.001).
We did an additional repeated measure ANOVA that used the EPDS outcome groups at T2 as a between-subject factor and the PIRGAS as a within-subject variable over time (see fig. 2). The ANOVA showed the main effects of EPDS outcome group (df = 1.18; F= 20.3; p <0.001) but not of time. The time*group interaction was significant (df = 1.18; F = 8.83; p = 0.008). Although subjects with low outcome depression did not differ from those with high outcome depression in the PIRGAS at T1, subjects that ended therapy low on depression had marked improvements in the PIRGAS, and subjects that had high depression scores had actually decreased their PIRGAS performance.
|
Table 3: Comparison of baseline and post-treatment scores for completers (n = 23). |
|
Variable
|
T1mean score (SD)
|
T2mean score (SD)
|
t
|
p
|
| EPDS |
16.26 (6.94) |
8.30 (7.19) |
5.13 |
<0.001 |
| STAISTATE |
44.39 (11.90) |
35.00 (15.28) |
3.06 |
0.006 |
| GAF |
62.33 (10.33) |
78.81 (13.97) |
-5.00 |
<0.001 |
| PIRGAS |
71.00 (12.20) |
79.80 (16.11) |
–1.98 |
0.062 |
| CGI |
3.76 (1.22) |
2.29 (1.45) |
4.50 |
<0.001 |
|
Table 4:Values of the most important measures depending on initial anxiety and depression. |
|
|
|
EPDS not at-risk (<12)
|
EPDS at-risk (≥12)
|
STAI not at-risk (<39)
|
STAI at-risk (≥39)
|
|
|
|
Mean
|
SD
|
Mean
|
SD
|
Mean
|
SD
|
Mean
|
SD
|
|
|
|
n = 7
|
n = 16
|
n = 7
|
n = 16
|
| T1 |
EPDS |
8.00 |
2.51 |
19.88 |
4.73 |
13.14 |
7.90 |
17.63 |
6.26 |
| STAI State |
37.43 |
11.08 |
47.44 |
11.23 |
30.71 |
4.23 |
50.38 |
8.67 |
| STAI trait |
41.86 |
9.924 |
49.75 |
10.95 |
41.43 |
8.97 |
49.94 |
11.12 |
| GAS |
74.43 |
6.876 |
57.38 |
9.05 |
68.71 |
12.31 |
59.88 |
10.45 |
| PIRGAF |
74.00 |
15.57 |
70.00 |
10.95 |
70.00 |
12.24 |
71.33 |
12.16 |
| CGI |
2.43 |
0.976 |
4.38 |
0.719 |
3.14 |
1.069 |
4.06 |
1.18 |
| T2 |
EPDS |
1.00 |
0.000 |
1.25 |
0.447 |
1.00 |
0.000 |
1.25 |
0.447 |
| STAI State |
29.57 |
5.06 |
37.38 |
17.682 |
27.43 |
5.192 |
38.31 |
17.13 |
| STAI trait |
36.29 |
7.58 |
45.88 |
16.276 |
39.86 |
14.96 |
44.31 |
14.89 |
| GAS |
84.67 |
9.416 |
76.47 |
15.047 |
79.33 |
13.58 |
78.60 |
14.57 |
| PIRGAF |
85.00 |
15.49 |
78.73 |
16.434 |
75.33 |
19.66 |
82.60 |
14.61 |
| CGI |
1.67 |
0.816 |
2.53 |
1.598 |
2.33 |
1.966 |
2.27 |
1.28 |
Discussion
In the scientific literature, very little data exist on mothers seeking help in a parent-infant outpatient psychiatric clinic. In our study population, a majority of the mothers presented with a high level of depressive (73%) and/or anxiety (70%) symptoms. Consequences on the mother-child relationship and the child’s development are well known. These data should encourage professionals to screen better for adult psychopathologies even when the patient is the child.
As we hypothesised, patients receiving the brief PCP displayed a significant improvement at the post-treatment assessment on almost all measures (depression, anxiety, clinical global impression and global functioning) and a tendency to improve on the measure of parent-infant relationships. The effect sizes observed from pretherapy to post-therapy were medium to large (depression d = 1.06; anxiety d = 0.63; CGI d = 0.99) yielding significant results even with this small sample size. In a meta-analysis of treatments for perinatal depression [48], Sockol found a similar significant improvement in depressive symptoms from pretreatment to post-treatment, with an overall effect size (g = 0.65) comparable to that found in a meta-analysis of the efficiency of psychological treatments for adult depression (g = 0.67) [16].
Altogether, 56% of the completer subjects reduced their depression symptoms by ≥50%, and 56% of them reduced their anxiety symptoms by ≥50%. At the end of the treatment, the number of people with major clinical depression declined drastically from 13 to 3. This represents an important improvement which is particularly marked if one takes into account the short duration of the PCP. It confirms the findings of another study using this same intervention, in which all the initially depressed women had an EPDS score <12 after a four-session PCP [37]. It is also of importance to note that at the end of the treatment, 81% of women had a good level of functioning, as compared with only 26% before the treatment.
However, results of this study do not confirm a significant improvement in the mother-infant relationship, although the p value (0.062) is very close to the significant value of 0.05. We hypothesise that this is owing to the small sample size, and that a larger sample could potentially show significance. These results should thus be confirmed in further studies using more precise and objective relational scales.
Whether patients had a low or high initial depression level did not have a significant impact on the outcome of the most important measures (depression, anxiety, mother-child relationship, global functioning). On the other hand, we can see that women with lower depression scores after therapy also have lower scores for anxiety, better functioning and have a better relationship with their child, as compared with those who have high depression scores at T2. Patient groups that had similar levels on the PIRGAS at T1 were successfully differentiated by their depression outcome. Mothers who ended their therapy with a lower level of depression improved their relationship with their child, whereas mothers who still suffered from a high level of depression after therapy actually had a worse relationship with their child after therapy than before. This shows the particular importance that the treatment of maternal depression has for the improvement of the mother-infant relationship. This study stresses the importance of depression outcome upon the successful development of the mother-infant relationship.
This study gives evidence that it is important to take the level of anxiety into account before beginning therapy. Anxiety prior to therapy is significantly correlated to depression and the woman’s functioning at that time, and is highly predictive of the depression level after the therapy. These results emphasise the impact of initial anxiety on the evolution of the mother’s symptoms and on her relationship with the baby. Furthermore, if symptoms of anxiety and depression persist after the therapy, the quality of the mother-baby relationship and the mother’s functioning do not improve.
Many authors have pointed out the high attrition rate of intervention during the perinatal period. Our data demonstrate that a majority (76%) of the 34 mothers enrolled completed the short PCP, which was well accepted by most of them. This low attrition rate could be explained by the short duration of the intervention, its focus on motherhood and the participation of the infant in the postnatal sessions. All these aspects are particularly important for the mothers at this period of time.
Parenthood is a major life transition. The prevalence of depression and anxiety during the perinatal period emphasises that many women experience significant mental health, adjustment and parenting difficulties. Most of these women will never seek help [29] or will only consult a child psychotherapist once the infant manifests some psychological distress (nervous or inconsolable infants, sleep or feeding problems, developmental delays …). Particular features of the PCP are dealing with the child’s symptoms and taking into account the mother’s psychological conflicts.
By focusing on the particular moment of becoming a parent and on interactions with the infant, PCP has the advantage of helping mothers recover from anxiety and depressive troubles and also of avoiding or treating relational problems with their child. The intervention is well adapted to the perinatal period because it is centred on parenthood and on the difficulties of changing identity when becoming a mother. By questioning and changing distorted maternal mental representations, PCP reduces maternal feelings of guilt and the associated anxiety and depressive symptoms. It focuses on mental representations linked to motherhood, which are of particular concern to future mothers. This means that they are more disposed to investigate their inner world and representations during this particular period.
This study had several methodological limitations derived in part from its clinical setting. The principal limitation was the lack of a control group not undergoing the intervention. For ethical reasons, and because the study was done with clinical patients consulting a specialised centre, PCP was offered to all mothers in order to minimise the effects of depression on the developing child and to avoid future disturbances in the mother-infant relationship. The small sample size was also a limitation, indicating that future studies with larger samples are required to confirm these results. Most of the mothers included in the study had a middle-high socio-economic situation and this limits the findings to this range of population. Indeed, women with a low socio-economic situation tend to have more difficulty accessing care when they are in need of it. The language barrier of some migrants is another obstacle to their care, in addition to all the social problems making the therapeutic alliance more difficult. Further studies should offer easier access to care for this population in order to include them in the study. This study is still ongoing with a follow up planned one year after the end of the therapy. This will give us the opportunity to look for medium term outcome measures and to assess more extensively the children’s symptoms and development more deeply than we have so far reported.
Conclusions
Mothers consulting an outpatient parent-infant clinic during the perinatal period and who participated in this study reported a high degree of depressive and anxiety symptoms. The PCP is a brief therapy focused on parenthood which is accessible to women during pregnancy and after delivery, and which includes the presence of the infant when possible. This study indicated that, for women consulting an infant-mother outpatient unit, this form of therapy had a significant positive impact on womens’ anxiety, depression and global functioning and had a positive impact on the mother-baby relationship. It also suggested that the trait of anxiety before therapy is directly related to depressive symptoms and the quality of the mother-infant relationship after the treatment. The level of depression after therapy is related to the level of anxiety, functioning and the quality of the mother-baby relationship, whereas the level of depression before therapy is not predictive of these measures. Further larger studies are required to confirm these findings.
Acknowledgment:We would like to thank Dr. E. Henzen-Ifkovits, Dr. L. Stauffacher, Dr. G. Vaudan-Vutskits and Mrs. A. Spira for therapy leading; Mrs. M. Pellet, Mrs. M. Gex-Fabry Pun, Mrs. I. Ruata and Mrs. A. Sancho-Rossignol for technical assistance; Dr. B. Stoll, Mr. E. Jeannot and Dr. I. Lampis-Ducommun for article revision.
References
1 American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington DC: Author. 2000.
2 Austin MP, Frilingos M, Lumley J, Hadzi-Pavlovic D, Roncolato W, Acland S, et al. Brief antenatal cognitive behaviour therapy group intervention for the prevention of postnatal depression and anxiety: a randomised controlled trial. J Affect Disord. 2008;105(1–3):35–44.
3 Austin MP, Priest SR, Sullivan EA. Antenatal psychosocial assessment for reducing perinatal mental health morbidity. Cochrane Database Syst Rev. 2008;4:CD005124.
4 Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50(5):275–85.
5 Beck CT. Postpartum depression predictors inventory-revised. Adv Neonatal Care. 2003;3(1):47–8.
6 Cicchetti D, Rogosch FA, Toth SL. The efficacy of toddler-parent psychotherapy for fostering cognitive development in offspring of depressed mothers. J Abnorm Child Psychol. 2000;28(2):135–48.
7 Clark R, Tluczek A, Wenzel A. Psychotherapy for postpartum depression: a preliminary report. Am J Orthopsychiatry. 2003;73(4):441–54.
8 Cohen NJ, Lojkasek M, Muir E, Muir R, Parker C. Six month follow-up of two mother-infant psychotherapies: Convergence of therapeutic outcomes. Infant Mental Health Journal. 2002;23:361–80.
9 Condon J. Women’s mental health: a “wish-list” for the DSM V. Arch Womens Ment Health. 2010;13(1):5–10.
10 Correia LL, Linhares MB. Maternal anxiety in the pre- and postnatal period: a literature review. Rev Lat Am Enfermagem. 2007;15(4):677–83.
11 Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J of Psychiatry. 1987;150:782–6.
12 Cramer B. Are Postpartum depressions a mother-infant relationship disorder? Infant Mental Health Journal. 1993; 14(4): 283-297.
13 Cramer B, Robert-Tissot C, Stern D, Rusconi Serpa S, De Muralt M, Besson G,et al. Outcome evaluation in brief mother-infant psychotherapy: a preliminary report. Infant Mental Health Journal. 1996;11(3):278–300.
14 Cramer B. Mother-infant psychotherapies: a widening scope in technique. Infant Mental Health Journal. 1998;19(2):151–67.
15 Cuijpers P, Geraedts AS, van Oppen P, Andersson G, Markowitz JC, van Straten A. Interpersonal psychotherapy for depression: a meta-analysis. Am J Psychiatry. 2011;168(6):581–92.
16 Cuijpers P, Smit F, Bohlmeijer E, Hollon SD, Andersson G. Efficacy of cognitive-behavioural therapy and other psychological treatments for adult depression: meta-analytic study of publication bias. Br J Psychiatry. 2010;196(3):173–8.
17 Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323–31.
18 Fava Vizziello G, Antonioli ME, Cocci V, Invernizzi R. From pregnancy to motherhood: the structure of representative and narrative change. Infant Mental Health Journal. 1993;14:4–16.
19 Fitelson E, Kim S, Baker AS, Leight K. Treatment of postpartum depression: clinical, psychological and pharmacological options. Int J Womens Health. 2010;3:1–14.
20 Forman DR, O’Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology. 2007;19(2):585–602.
21 First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute. 2002.
22 Gelfand D, Teti DM, Seiner SA, Jameson PB. Helping Mothers Fight Depression: Evaluation of a Home-Based Intervention Program for Depressed Mothers and their Infants. Journal of Clinical Child Psychology. 1996;25:406–22.
23 Guedeney A, Fermanian J. Validation of a study of the french version of the Edinburgh Post Natal Depression Scale (EPDS): new results about use and psychometric properties. Eur. Psychiatry. 1998;13:83–9.
24 Guy W. Clinical Global Impressions (CGI) Scale. Modified From: Rush J, et al. Psychiatric Measures, APA, Washington DC. 2000.
25 Gunlicks ML, Weissman MM. Change in child psychopathology with improvement in parental depression: a systematic review. J Am Acad Child Adolesc Psychiatry. 2008;47(4):379–89.
26 Horowitz JA, Goodman JH. A longitudinal study of maternal postpartum depression symptoms. Res Theory Nurs Pract. 2004;18(2-3):149–63.
27 Horowitz JA, Goodman JH. Identifying and treating postpartum depression. J Obstet Gynecol Neonatal Nurs. 200;34(2):264–73.
28 Manzano J, Palacio Espasa F, Zilkha N. The narcissistic scenarios of parenthood. Int J Psychoanal. 1999;80 (3):465–76.
29 Marcus SM. Depression during pregnancy: rates, risks and consequences – Motherisk Update 2008. Can J Clin Pharmacol. 2009;16(1):e15-22.
30 Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health (Larchmt). 2003;12(4):373–80.
31 Milgrom J, Gemmill A, Westley D. The mediating role of maternal responsiveness in some longer‑term effects of postnatal depression on infant development. Infant Behavior and Development. 2004;27(4):443–54.
32 Milgrom J, Ericksen J, McCarthy R, Gemmill AW. Stressful impact of depression on early mother-infant relations. Stress and Health. 2006;22:107–12.
33 Milgrom, J, Schembri C, Ericksen J, Ross J, Gemmill AW. Towards parenthood: an antenatal intervention to reduce depression, anxiety and parenting difficulties. J Affect Disord. 2011;130(3):385–94.
34 Murray L, Cooper PJ. Postpartum depression and child development. Psychol Med. 1997;27(2):253–60.
35 Murray L, Cox JL. Sceening for depression during pregnancy with the EPDS. Journal of Reproductive and Infant Psychology. 1990;8:99–109.
36 Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. BR J Psychiatry. 1990;157:288–90.
37 Murray L, Cooper PJ, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 2. Impact on the mother-child relationship and child outcome. Br J Psychiatry. 2003;182:420–7.
38 Nanzer N, Sancho Rossignol A, Righetti-Veltema M, Knauer D, Manzano J, Palacio-Espasa F. Effects of a brief psychoanalytic intervention for perinatal depression. Arch Wom Mental Health, 2012;15:259–68.
39 Nanzer N, Knauer D, Palacio Espasa F, Qayoom-Boulvain Z, Hentsch F, Clinton P, et al. Manuel de psychothérapie centrée sur la parentalité. Fil Rouge, PUF. Paris 2012.
40 Nylen KJ, Moran TE, Franklin CL, O’Hara MW. Maternal depression: A review of relevant treatment approaches for mothers and infants. Infant Mental Health Journal. 2006;27(4):327–43.
41 O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry. 2000;57(11):1039–45.
42 Paris R, Sielman E, Bolton R. Mother-infant psychotherapy: examining the therapeutic process of change. Infant Mental Health Journal. 2009;30(3):301–19.
43 Pearlstein TB, Zlotnick C, Battle CL, Stuart S, O’Hara MW, Price AB, et al. Patient choice of treatment for postpartum depression: a pilot study. Arch Womens Ment Health. 2006;9(6):303–8.
44 Raudzus J, Misri S. Managing unipolar depression in pregnancy. Curr Opin Psychiatry. 2009;22(1):13–8.
45 Righetti-Veltema M, Conne-Perréard E, Bousquet A, Manzano J. Risk factors and predictive signs of postpartum depression. J Affect Disord. 1998;49(3):167–80.
46 Righetti-Veltema M, Conne-Perréard E, Bousquet A, Manzano J. Postpartum depression and mother-infant relationship at 3 months old. J Affect Disord. 2002;70(3):291–306.
47 Sinyor M, Schaffer A, Levitt A. The sequenced treatment alternatives to relieve depression (STAR*D) trial: a review. Can J Psychiatry. 2010;55(3):126–35.
48 Sockol LE, Epperson CN, Barber JP. A meta-analysis of treatments for perinatal depression. Clin Psychol Rev. 2011;31(5):839–49.
49 Spielberger CD, Gorssuch RL, Lushene, P.R., Vagg, P.R., & Jacobs, G.A. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press, Inc. 1983.
50 Stuart S, Clark E. The treatment of postpartum depression with interpersonal psychotherapy and interpersonal counseling. Sante Ment Que. 2008;33(2):87–104.
51 Tuohy A, McVey C. Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. Br J Clin Psychol. 2008;47(Pt 2):153–69.
52 Zero to three, Diagnostic classification, 0–3 R: diagnostic classification of mental health and developmental disorders of infancy and early childhood. Zero to three, National Center for Clinical Infant Programs, Arlington, 2005.