Added value of an intensive multidisciplinary functional rehabilitation programme for chronic low back pain patients
DOI: https://doi.org/10.4414/smw.2013.13763
Anne-Sylvie
Steiner, Marlène
Sartori, Sandra
Leal, Danièle
Kupper, Jean-Paul
Gallice, Denis
Rentsch, Christine
Cedraschi, Stéphane
Genevay
Summary
BACKGROUND: Several treatments exist for chronic low back pain (cLBP) patients although none has shown superiority. Among group treatments, muscle reconditioning programmes (MRPs) are the most commonly used. Multidisciplinary functional rehabilitation programmes (MFRPs) are an alternative.
OBJECTIVE: To compare a MFRP with a MRP as few studies compare these treatments
METHODS: This was a prospective, nonrandomised, controlled study comparing cLBP patients participating in a MRP or MFRP in an outpatient setting. The predetermined primary outcome measure was the daily life activity subscale (DLA) of the Dallas Pain Questionnaire (DPQ) within one year after the end of the treatment.
RESULTS: Twenty-one patients were included in the MRP and 24 in the MFRP. At inclusion, the groups were similar in terms of age (mean 40 years), sex (50%–60% males), sick leave duration (mean 6.0 months, standard deviation (SD) 4.4 months) and follow up (mean 9.0 months, SD 2.0 months). The DLA score decreased from 59.5% (SD 16.9) to 44.8% (SD 25.4), p <0.01, in the MFRP and from 62.3 (SD 20.3) to 58.8 (SD 20.7), p = 0.3, in the MRP. The between-groups difference at follow-up was 13.8, p = 0.05, and the difference in the mean improvement was –11.5 (5.9), p = 0.058. Seventy-eight percent of MFRP patients versus 47 % in the MRP group returned to work (p = 0.08).
DISCUSSION: In a population of highly disabled cLBP patients, MFRP seems more effective in increasing function and return to work. Interpretation is limited by the small population included and by the type of trial.
CONCLUSION: Randomised studies are needed to confirm these results and explore the cost-effectiveness of MFRP.
Introduction
Non-specific low back pain (LBP) is a major public health problem. Overall, 60%‑80% of the population will be affected by this problem at least once in their lifetime [1, 2]. The majority will recover favourably and return to a normal active life within a few weeks without consequences. Seven to ten percent will develop a chronic condition (pain lasting >3 months [3]) associated with numerous incapacities in daily life [4]. For these patients, several therapeutic approaches have been developed. These can be basically classified into two groups. One group includes treatments focusing on muscle reconditioning through exercises. Benefits of these treatments on pain and function have been reported for the short term [5, 6], but the effect on return to work is less clear [5, 7]. The second group includes cognitive behavioural treatments, based on the theory and observations that avoidance behaviour and inappropriate beliefs are major factors in the development of chronicity. Treatments based on these theories have a moderate effect on pain, function and behaviour [8–10]. The addition of a cognitive component to physical approaches has been rather disappointing [11–13]. More complex multidisciplinary treatments integrating physical rehabilitation, psychological evaluation, cognitive behavioural methods and occupational therapy with a socioprofessional component are frequently advocated [14], but there is a lack of studies directly comparing these complex approaches with simpler muscle reconditioning programmes (MRPs).
The development of an outpatient multidisciplinary functional rehabilitation program (MFRP) to replace a more traditional outpatient MRP gave us the opportunity to compare these two approaches.
Aim of the study
The aim of the study was to compare MRP with MFRP in order to evaluate their respective efficacies and to explore the potential additional value of the more complex intervention.
|
Table 1: Content of the programmes. |
|
|
Multidisciplinary functional rehabilitation programme
|
Muscle reconditioning programme
|
| Number patients per group |
4–6 |
4–6 |
| Hours per day |
5 |
3 |
| Duration, weeks |
4 |
3 |
| Total number of hours |
97* |
46 |
| Group physiotherapy, hours |
46 |
40 |
| Unsupervised exercises, hours |
20** |
|
| Occupational therapy, hours |
7 |
6 |
| Analytic group therapy, hours |
4 |
|
| Patient education session, hours |
12 |
|
| Workplace evaluation |
yes (optional) |
no |
| Individualised treatment goals |
yes |
no |
| Cognitive-behavioural approach |
yes |
no |
| * This figure includes welcoming and closing sessions, individual biopsychosocial evaluation, goal setting and restitution sessions for a total of 8 hours
** Only for patients who cannot go back to work part time during week 3 and 4 of the programme. |
Method
This was a prospective nonrandomised controlled study comparing patients with chronic low back pain (cLBP) participating in a group programme based on intensive physical exercises (MRP) with similar patients participating in a multidisciplinary rehabilitation programme (MFRP). Patients with recurrent episodes of low back pain for more than four weeks within the same year were considered chronic and could also be included. This study was conducted on the occasion of a change in treatment strategy in our institution, with MFRP replacing MRP. The data were collected from mid-2006 to mid-2007 for MRP and from the end of 2007 to 2008 for MFRP. All patients were recruited at the tertiary rheumatology and rehabilitation centre of Geneva University Hospitals with strictly identical eligibility criteria. To be included, patients had to be 18 to 65 years old, suffering from non-specific low back pain (with or without radiating leg pain) despite standard care from their general practitioner, including pain medication and individual physiotherapy. Patients working outside the home had to be on sick leave. A good understanding of spoken and written French was also required. Exclusion criteria were specific low back pain due to infection, tumour, spondylarthropathy, radicular leg pain due to disc herniation and neurogenic claudication related to spinal stenosis. Patients suffering from medical comorbidities that could interfere or prohibit their participation (e.g. cardiac or pulmonary failure, severe mood disorder, disabling knee osteoarthritis) or with a diffuse chronic pain syndrome were also excluded. Patients on sick leave for more than two years or receiving a disability pension were likewise excluded. All eligible patients who consulted at the rheumatology and rehabilitation centre were included unless the programme was full. In this case, the patient was included in the next programme session. Whilst in the study, pain medication was adapted as needed but physiotherapy outside the programme was interrupted.
Interventions
The MRP was designed to increase musculoskeletal strength and endurance and to teach basic knowledge of ergonomics. It was held for groups of four to six participants, five half-days/week over three weeks, providing a total of 45 hours of physical therapy with muscle reinforcement and stabilisation exercises, relaxation, proprioception sessions and water gymnastics. Six hours of occupational therapy focusing on prespecified activities (sitting, lifting, handling and driving) were provided. No individualisation of therapy during the sessions was offered (table 1).
The MFRP was designed to restore the individual’s musculoskeletal function and included significant cognitive behavioural components and work-related goals and outcomes [15, 16]. It was designed by an extensive multidisciplinary team (rheumatologist, rehabilitation physician, pain specialist, psychiatrist, physical therapists, occupational therapists and a psychologist) for groups of four to six patients, and was held over four weeks for a total of 100 hours (table 1). A complete description of the methods used to devise the programme has been published [17, 18]. All treatments were delivered in groups, but the type and intensity of the physical treatment were tailored to each patient, based on an initial evaluation of his/her physical capacities, psychosocial impairments, expectations and priorities. Most importantly, personalised, realistic and measurable objectives were defined individually at the beginning of the programme and reassessed in the end. Treatments sessions included: (1.) cardiorespiratory fitness, muscular strength, muscular flexibility, stabilisation exercises, relaxation, proprioception and water gymnastics; (2.) occupational therapy with emphasis on individual professional and daily life situations; (3.) patient education sessions based on a noninjury model [19, 20] and the biopsychosocial model; and (4.) one hour per week of support group discussion led by a psychiatrist (table 1). The programme was designed to increase muscle activities progressively and to help the patients overcome their fear of movement whenever fear avoidance beliefs were detected during initial evaluation. Alongside the programme, patients developed their own booklet of illustrated and annotated exercises and techniques that they found appropriate for their condition. Return to work during the mornings of the third or the fourth week was encouraged when possible. If not working, patients had to come each morning to the site to perform two hours of unsupervised exercises, as taught during the first weeks.
Outcome measures
The main outcome measure was the French validated version of the Dallas Pain Questionnaire (DPQ), as it is the only self-administered questionnaire developed according to the biopsychosocial model of cLBP [21]. It explores four different dimensions (daily life activities, work-leisure, anxiety-depression and sociability) in 16 questions, each dimension having between three and seven questions. The answer to each question is recorded on a Likert scale and computed so that each dimension has a final score ranging from 0% to 100%, where 0% is best. Pain was evaluated on a visual analogue scale (VAS) from 0–10. Work ability at follow up was defined as being at work or having the ability to be at the workplace (e.g. an unemployed patient without sickness leave). For both types of treatment, data were collected prior to the programme and a questionnaire was mailed six to eight months after its conclusion. In addition to pain and the DPQ, return to work was also assessed. The data were collected from mid-2006 to mid-2007 for the MRP and from the end of 2007 to 2008 for the MFRP, at the tertiary rheumatology and rehabilitation centre of Geneva University Hospital.
Statistical analysis
Distribution of the variables was checked for normality using normality plots and by determining skewness and kurtosis. Within-groups comparisons were made with paired Student t-tests, between-groups comparisons were made with unpaired Student t-tests for normally distributed variables and a non-parametric test (Mann-Whitney U test) was used when this assumption was not satisfied. Analysis was performed using STATA version 11 for Windows (StataCorp).
|
Table 2: Baseline characteristics of the study population. |
|
|
Multidisciplinary functional rehabilitation programme
(n = 24)
|
Muscle reconditioning programme
(n = 21)
|
p
|
| Age (years), mean (SD) |
39.9 (11.7) |
41.1 (10.9) |
NS |
| Sex (male), n (%) |
14 (58.3) |
10 (47.6) |
NS |
| Length of follow up (months), mean (SD) |
8.7 (2.9) |
8.8 (1.2) |
NS |
| Length of sick leave (months), mean (SD) |
6.0 (4.4) |
5.1 (4.7) |
NS |
| Type of work, n (%)
sedentary
physical
mixed
not employed |
3 (13)
13 (54)
8 (33)
0 |
5 (24)
8 (38)
6 (28)
2 (10) |
NS |
| Length of the present episode (months), n (%)
<3
3–6
>6 |
3 (13)
2 (8)
19 (79) |
5 (24)
4 (19)
12 (57) |
NS |
| Pain (VAS 0‑100), mean (SD) |
59.3 (16.3) |
59.0 (20.4) |
NS |
| Dallas Pain Questionnaire (0–100), mean (SD)
daily life activity
work-leisure
depression-anxiety
social interest |
59.5 (16.9)
61.0 (24.3)
51.8 (28.8)
38.3 (24.3) |
62.3 (20.3)
65.5 (23.1)
45.2 (26.9)
39.5 (24.3) |
NS
NS
NS
NS |
| SD = standard deviation; NS = not significant |
Results
Twenty-one patients were included in the MRP group and 24 in the MFRP group. The MRP patients had a subsequent evaluation after 8.8 (standard deviation (SD) 1.2) months, the MFRP group after 8.7 (SD 2.9) months. The main sociodemographic and clinical data are presented in table 2.
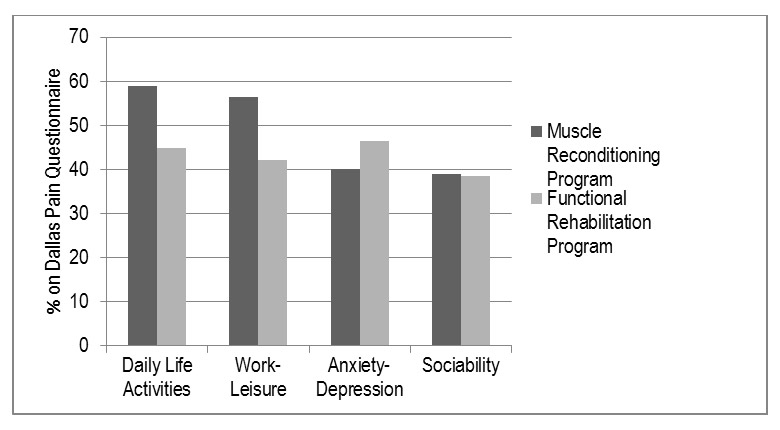
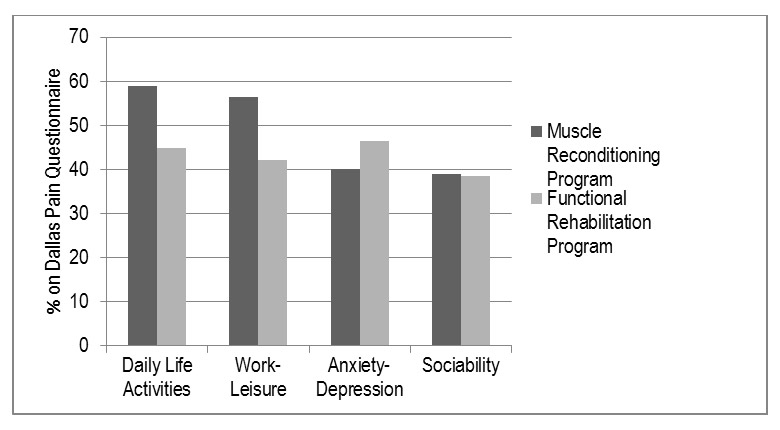
Figure 1
Results at follow-up for the two programmes for each of the Dallas Pain Questionnaire subscales. A difference was observed favouring the multidisciplinary functional rehabilitation programme in terms of “daily life activities” and “work-leisure” with a trend toward statistical significance.
Muscle reconditioning program (MRP)
Mean (SD) values were decreased in three out of the four subscales of the DPQ: ‘daily life activity’ (62.3 (20.3) vs 58.8 (20.7)), ‘work-leisure’ (65.5 (23.1) vs 56.4 (24.4) and ‘anxiety-depression’ (45.2 (26.9) vs 40.0 (24.89)). None of these differences was statistically significant, although a trend was observed for ‘work-leisure’ (-9.1 (22.0), 95% confidence interval (CI) –19.4–1.2, p = 0.08). There was no effect on the social interest subscale (39.5 (24.3) vs 39.0 (26.5)). Pain score on the VAS decreased from 5.9 (2.0) to 5.1 (2.7), (–0.8 (2.7), 95% CI –2.1–0.4, p = 0.19). Out of the 21 patients, work ability outside the home at follow up could be assessed in 17 (three housewives and one early retirement). All were on sick leave at inclusion and eight (47%) were working at follow up.
Multidisciplinary functional restoration program (MFRP)
Mean (SD) values were statistically improved for the ‘daily life activity’ (59.5 (16.9) vs 44.8 (25.4), p = 0.002) and ‘work-leisure’ (61.0 (24.3) vs 42.2 (29.4), p = 0.001) subscales of the DPQ. There was no significant difference for the ‘anxiety-depression’ (51.8 (28.8) vs 46.6 (30.7), p = 0.5) and ‘sociability’ (38.3 (24.3) vs 38.5 (24.9)) subscales. The pain score on the VAS decreased significantly from 5.9 (1.6) to 4.5 (2.4), p = 0.01. Out of the 24 patients, work ability at follow up could be assessed in 23 (the other was a housewife). All were on sick leave at inclusion and 18 (78%) were working at follow up.
Between group comparison
There was no significant difference at inclusion on the DPQ subscales or in pain. Mean scores on the ‘daily life activity’ subscale of the DPQ at follow up were better in the MFRP group than in the MRP group (44.8 (25.4) vs 58.6 (20.2), respectively), with a mean difference of 13.8 (6.9), p = 0.05. The difference in the mean improvement was –11.5 (5.9), 95% CI –23.5–0.4, p = 0.058. A similar result was observed for the ‘work-leisure’ subscale: 42.3 (29.4) vs 56.6 (23.8), difference in the mean improvement –11.1 (6.9), 95%CI–25.1–2.9, p = 0.11. The other two subscales and the pain scores showed no between-group differences (fig. 1). Rate of return to work among patients with work ability was higher in the MFRP group, without reaching statistical significance (78% vs 47%, p = 0.08).
Discussion
The main goal of the study was to compare the effect of an intensive multidisciplinary rehabilitation programme with that of a muscle reconditioning programme on biopsychosocial consequences of chronic low back pain as measured by the DPQ. With the MFRP significant improvement was observed in the daily life activity and leisure-work subscales of the DPQ, as well as in pain on the VAS. The difference for the primary endpoint (DPQ daily life activity) reached the threshold of a 30% improvement, which is recommended as a clinically relevant improvement [22]. No such improvement was observed with the MRP. When comparing both programmes, a notable difference in absolute values was observed for these dimensions, however there was a statistical difference only in favour of MFRP. The same effect was observed for return to work, with a 40% increase in the work ability rate in the MFRP group as compared with the MRP group, but statistically a difference in favour only of the more complex programme. No impact was measured on the other DPQ subscales.
Although MRP is recommended for the treatment of cLBP [14], the group of patients receiving this treatment showed only a nonsignificant modest effect. This observation could have resulted from the high degree of functional impairment in this population, which was reflected by the high scores in all DPQ subscales as compared with the usual reports from similar studies [23, 24]. In fact, these scores were at levels comparable to those reported in surgical studies [25–27]. Hence, in this population of highly disabled patients, we hypothesise that straightforward MRP is less effective and that the implementation of a complex multidimensional programme is needed in order to observe a significant effect on function and a substantial increase in the rate of return to work.
This study directly compared, in a similar outpatient setting, two kinds of group therapy based on exercises, and found evidence of greater effectiveness with MFRP as compared with MRP. According to recent reviews, there is no randomised controlled trial that directly compared these two interventions [28, 29]. The superiority of intensive MFPR in an outpatient setting has been mainly compared with usual care [30], passive physiotherapy [31] or a less intensive multidisciplinary programme [30]; when compared to active individual therapy the difference was either modest [24, 32] or nonsignificant [23]. In a different approach, other authors have looked at the effect of adding cognitive behavioural treatment (CBT) to a physical programme and failed to demonstrate an additional effect [10–12].
There are several important differences that could explain the positive results we observed in this study. Firstly, this programme was not designed as a CBT treatment. Principles of CBT were taught to the entire team and the team was encouraged to emphasise the use of personalised objectives within the group sessions in order to adapt the rhythm of progression and to increase motivation and satisfaction, factors known to positively influence pain and function [33–35]. A similar approach has recently been shown to be successful in a large randomised controlled trial performed in a setting of individual physiotherapy [36]. Secondly, interventions were based on a noninjury theory model [19, 37] and this model was introduced to the patients in specific sessions using therapeutic education principles. Classically cLBP is considered to be the consequence of repetitive microinjury of the spine and subsequent muscle deconditioning. This hypothesis has been recently challenged [38] and the alternative noninjury model has been proposed [19]. The implementation of this model in different settings has been shown to have a favourable impact on cLBP [20, 37]. Finally, workplace assessment was also included. Structured intervention at the workplace has shown positive impact on return to work or reduction of sick leave days [39, 40]. In our country, this kind of intervention is extremely difficult to set up and not well accepted by the employers, even when it is integrated into an institutional intervention such as for this programme. Although a thoughtful assessment of the work situation was included for all participants, we could conduct interventions at the workplace for only a fraction of them. Hence the real impact of this part of our intervention on the overall results remains to be proven.
The absence of change on the “anxiety-depression” and the “sociability” subscales of the DPQ was not anticipated. These complex problems might be difficult to modify even with a four-week multidisciplinary rehabilitation programme. The absence of effect has been reported by others [10, 31, 41–43]. Other studies did show an effect [24], but their populations had a 10% lower score on the DPQ scales at inclusion compared with our patients, and were referred for individual psychological evaluation and treatment when needed. This illustrates the difficulty of addressing these complex issues in a group programme, and identifies a possible obstacle to better results with extensive and costly multidisciplinary programs for cLB patients.
The main limitations of the present results are due to the nonrandomised design. Despite the abundant literature on back pain, to the best of our knowledge no higher quality evidence has been published on this specific topic. Running two demanding programmes at the same time within the same institution was impossible in terms of logistics. In order to have comparable populations, great care was taken not to modify eligibility criteria. This is reflected by the similarity of the two populations at inclusion (table 2). However we acknowledge that by doing so we were not able to completely rule out confounders such as differences in treatments during the follow-up time. The interpretation of the results is also limited by the small sample size which explains the fact that although MFRP showed a much greater effect in absolute values, the difference between MFRP and MRP was just at the threshold of significance. Post hoc analysis revealed that in the present setting we had only a 50% chance of reaching a statistically significant result. If anything, the efficacy of the MFRP was rather underestimated as the team had to acquire new competencies in the field of CBT and it took several months to be at ease with these concepts. The main reason for the superiority of MFPR over MRP could be attributed to the increasing amount of hours of treatment delivered by the therapists in the MFPR. However, as shown in table 1, most of the increased time in the MFPR, as compared with MRP, was actually dedicated to unsupervised exercises. As increasing the duration of MRP has not been associated with improved effectiveness [3], we postulate that the observed difference relates more to intrinsic advantages of MFRP, such as those described in the previous paragraph. In the present setting, MFRP had a higher direct cost than MRP as there were an increased number of therapeutic interventions administrated over a longer period of time. However, at the societal level, it may be possible that the balance is in favour of MFRP as the rate of return to work was also higher with this programme. Unfortunately a cost analysis was not performed. The clinical characteristics of the sample of patients included in this study make it likely that the results can be transferred to other clinical settings addressing tertiary care of low back pain patients possibly eligible for intensive multidisciplinary functional rehabilitation programmes, but not to other types of settings as such. Additional studies should be performed to discover if the results (in particular the rate of return to work) are maintained over the years.
Conclusion
In conclusion, despite the limitations and in the absence of higher quality evidence on this specific point, we feel that these results provide important information for practitioners and providers alike. MFRP in cLBP patients with severe disability in daily life activities seems to be more effective than a rehabilitation programme based predominantly on muscle reconditioning. Although more demanding for the team, more difficult to set up and with higher direct costs, there are elements (specifically concerning return to work rate) suggesting that these complex interventions could well be cost-effective and thus call for additional studies.
Acknowledgement:We thank all the therapists who participated in these programmes for their dedicated work. We thank Mike Tomcik for his help with the preparation of the manuscript.
References
1 Nachemson R. Epidemiologyand the Economics of Low Back Pain. In: Herkowitz HN, Dvorak J, Bell G, Nordin M, Grob D, editors. The Lumar Spine. 3nd ed. Philadelphia: Lippincott Williams & Wilkins; 2004. p. 3–10.
2 Hoy D, Brooks P, Blyth F, Buchbinder R. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–81.
3 Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber Moffett J, Kovacs F, et al. COST B13 Working Group on Guidelines for Chronic Low Back Pain. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192–300.
4 Spitzer WO, Leblanc FE, Dupuis M. Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for physicians. Report of the Quebec Task Force on spinal disorders. Spine. 1987;12(7S):S1–S59.
5 Oesch P, Kool J, Hagen KB, Bachmann S. Effectiveness of exercise on work disability in patients with non-acute non-specific low back pain: Systematic review and meta-analysis of randomised controlled trials. J Rehabil Med. 2010;42(3):193–205.
6 van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006;15(Suppl 1):S64–81.
7 Schaafsma F, Schonstein E, Ojajärvi A, Verbeek J. Physical conditioning programs for improving work outcomes among workers with back pain. Scand J Work Environ Health. 2011;37(1):1–5.
8 Buhrman M, Faltenhag S, Strom L, Andersson G. Controlled trial of Internet-based treatment with telephone support for chronic back pain. Pain. 2004;111(3):368–77.
9 Turner JA, Jensen MP. Efficacy of cognitive therapy for chronic low back pain. Pain. 1993;52(2):169–77.
10 van Tulder MW, Ostelo RW, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioural treatment for chronic low back pain. Cochrane Database Syst Rev. 2005;(1):CD002014.
11 Nicholas MK, Wilson PH, Goyen J. Operant-behavioural and cognitive-behavioural treatment for chronic low back pain. Behav Res Ther. 1991;29(3):225–38.
12 Smeets RJ, Vlaeyen JW, Hidding A, Kester AD, van der Heijden GJ, Knottnerus JA. Chronic low back pain: physical training, graded activity with problem solving training, or both? The one-year post-treatment results of a randomized controlled trial. Pain. 2008;134(3):263–76.
13 Turner JA, Clancy S, McQuade KJ, Cardenas DD. Effectiveness of behavioral therapy for chronic low back pain: a component analysis. J Consult Clin Psychol. 1990;58(5):573–9.
14 Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075–94.
15 Waddell G. The Back Pain Revolution. Second ed. Edinburgh: Churchill Livingstone; 2004.
16 Waddell G, Burton AK. Concepts of rehabilitation for the management of low back pain. Best Pract Res Clin Rheumatol. 2005;19(4):655–70.
17 Gallice J-P, Kupper D, Rentsch D, Barthassat V, Cedraschi C, Genevay S. Multidisciplinary programs and chronic low back pain: concepts and practical aspects. 2: clinical aspects. Kinesither Rev. 2010;102:40–4.
18 Kupper D, Gallice J-P, Rentsch D, Barthassat V, Cedraschi C, Genevay S. Multidisciplinary programs and chronic low back pain: concepts and practical aspects.1: Concepts and Development. Kinesither Rev. 2010;102:35–9.
19 Indahl A. Low back pain: diagnosis, treatment, and prognosis. Scandinavian journal of rheumatology. 2004;33(4):199–209.
20 Sorensen PHP, Bendix TT, Manniche CC, Korsholm LL, Lemvigh DD, Indahl AA. An educational approach based on a non-injury model compared with individual symptom-based physical training in chronic LBP. A pragmatic, randomised trial with a one-year follow-up. BMC musculoskeletal disorders. 2010;11:212–.
21 Marty M, Blotman F, Avouac B, Rosenberg S, Valat JP. Validation of the French version of the Dallas pain questionnaire in chronic low back pain patients. Rev Rhum Engl Ed. 1998:65(5):126–34.
22 Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33(1):90–4.
23 Jousset N, Fanello S, Bontoux L, Dubus V, Billabert C, Vielle B, et al. Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study. Spine (Phila Pa 1976). 2004;29(5):487–93; discussion 94.
24 Roche GG, Ponthieux AA, Parot-Shinkel EE, Jousset NN, Bontoux LL, Dubus VV, et al. Comparison of a functional restoration program with active individual physical therapy for patients with chronic low back pain: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88(10):1229–35.
25 Andersen T, Christensen FB, Hansen ES, Bunger C. Pain 5 years after instrumented and non-instrumented posterolateral lumbar spinal fusion. Eur Spine J. 2003;12(4):393–9.
26 Soegaard R, Christensen FB, Christiansen T, Bunger C. Costs and effects in lumbar spinal fusion. A follow-up study in 136 consecutive patients with chronic low back pain. Eur Spine J. 2007;16(5):657–68.
27 Videbaek TS, Christensen FB, Soegaard R, Hansen ES, Hoy K, Helmig P, et al. Circumferential fusion improves outcome in comparison with instrumented posterolateral fusion: long-term results of a randomized clinical trial. Spine (Phila Pa 1976). 2006;31(25):2875–80.
28 Gatchel RJ, Mayer TG. Evidence-informed management of chronic low back pain with functional restoration. Spine J. 2008;8(1):65–9.
29 Schaafsma F, Schonstein E, Whelan KM, Ulvestad E, Kenny DT, Verbeek JH. Physical conditioning programs for improving work outcomes in workers with back pain. Cochrane Database Syst Rev. 2010(1):CD001822.
30 Bendix AF, Bendix T, Labriola M, Boekgaard P. Functional restoration for chronic low back pain. Two-year follow-up of two randomized clinical trials. Spine (Phila Pa 1976). 1998;23(6):717–25.
31 Alaranta H, Rytokoski U, Rissanen A, Talo S, Ronnemaa T, Puukka P, et al. Intensive physical and psychosocial training program for patients with chronic low back pain. A controlled clinical trial. Spine (Phila Pa 1976). 1994;19(12):1339–49.
32 Kaapa EH, Frantsi K, Sarna S, Malmivaara A. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: a randomized trial. Spine (Phila Pa 1976). 2006;31(4):371–6.
33 Cedraschi C, Robert J, Perrin E, Fischer W, Goerg D, Vischer TL. The role of congruence between patient and therapist in chronic low back pain patients. J Manipulative Physiol Ther. 1996;19(4):244–9.
34 Schmitz U, Saile H, Nilges P. Coping with chronic pain: flexible goal adjustment as an interactive buffer against pain-related distress. Pain. 1996;67(1):41–51.
35 Verbeek J, Sengers MJ, Riemens L, Haafkens J. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine (Phila Pa 1976). 2004;29(20):2309–18.
36 Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378(9802):1560–71.
37 Indahl A, Haldorsen EH, Holm S, Reikeras O, Ursin H. Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine (Phila Pa 1976). 1998;23(23):2625–30.
38 Hancock MJ, Battie MC, Videman T, Gibbons L. The role of back injury or trauma in lumbar disc degeneration: an exposure-discordant twin study. Spine (Phila Pa 1976). 2010;35(21):1925–9
39 Lindstrom KJ. Work organization interventions in small and medium-sized enterprises in Scandinavia. Soz Praventivmed. 2004;49(2):95–6.
40 Loisel P, Abenhaim L, Durand P, Esdaile JM, Suissa S, Gosselin L, et al. A population-based, randomized clinical trial on back pain management. Spine (Phila Pa 1976). 1997;22(24):2911–8.
41 Nicholas MK, Wilson PH, Goyen J. Comparison of cognitive-behavioural group treatment and an alternative non-psychological treatment for chronic low back pain. Pain. 1992;48(3):339–47.
42 Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2002;(1):CD000963.
43 Smeets RJ, Vlaeyen JW, Hidding A, Kester AD, van der Heijden GJ, van Geel AC, et al. Active rehabilitation for chronic low back pain: cognitive-behavioural, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229]. BMC Musculoskelet Disord. 2006;7:5.