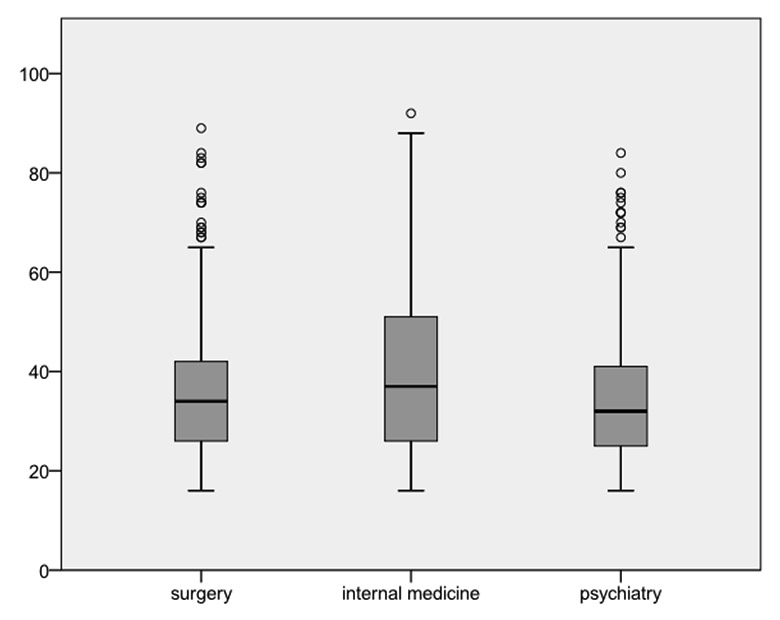
Figure 1
Age distribution and reason for presentation (clinical discipline). The boxes represent medians with 25% and 75% centiles.
DOI: https://doi.org/10.4414/smw.2013.13753
There are more than 10 million prison inmates throughout the world and this number is increasing continuously [1–3]. The trend is upwards in Switzerland too, with a maximum of 103 prison inmates per 100000 people in 2010 [4]. A prison is primarily a component of the penal system and must ensure that the prisoners complete their sentences. This can lead to conflicts with adequate health care in this minority group [3]. According to a UN resolution of 1990, all prisoners have the right to adequate health care [2]. Since the end of the 1990s, there have been a variety of national and international actions to create foundations for the improvement and development of prison medicine [5, 6]. The main goal of these efforts is to achieve equity in healthcare access between prisoners and the general population [5]. Nevertheless, the inadequate state of health in prisons is still cause for international concern [3, 5, 7].
Even though much has been written about the poor healthcare conditions of prisoners, there is little knowledge of their actual disease profile [8]. Most of the prisoners were either non-skilled employees or unemployed prior to prison, which correlates with increased morbidity and mortality [9]. Several studies have shown that between 65% and 81% of all prisoners suffer from one or more health problems [10, 11]. In particular, psychiatric diseases are very common [5, 7, 8, 11, 12]. But it has been shown that only a small percentage of psychiatric diseases are recognised at the start of the sentence [3]. Prisoners are generally young [8], but the number of prisoners older than 60 years is increasing [1, 3, 13]. Older prisoners – like the “normal” older population – are expected to suffer from more health problems. Additionally, studies have shown that up to 20% of prisoners’ health problems are unrecognised or treated too late. Foreign prisoners are increasingly common in prisons in Switzerland [4]. Foreigners are even more vulnerable, as language barriers often make it difficult to achieve adequate medical care in prison, and health problems may be misunderstood for this reason [8, 14]. Prisoners are a particularly vulnerable minority group that has special healthcare needs and makes special demands on healthcare services and providers.
In Switzerland, there are two medical prison wards, one in Geneva and one in Bern [2]. The High Security Ward (BEWA) of the Inselspital in Bern [15, 16] is part of the Clinic for General Internal Medicine and is the only facility of this sort in German-speaking Switzerland. It was opened in 1971 and provides medical care to about 400 prisoners per year, from all of Switzerland. There are 13 beds. The High Security Ward is built both as a prison and as an acute hospital. The medical staff and guards are specially trained for working with prisoners. Medical care is provided by somatic and psychiatric teams.
The University Emergency Centre is responsible for the primary admission and investigation of all prisoners admitted on an emergency basis to the prison ward of the Inselspital. Apart from the prison doctors, this is the initial point of contact for prisoners and is an important component in the healthcare chain. The aim of this study was to give an overview on the healthcare problems of prisoners leading to emergency department admission, in order to make recommendations to help to optimise treatment for this target group.
Our retrospective data analysis included adult (age ≥16 years) prisoners admitted to our emergency department, in transit to admission to our hospital-associated medical prison ward, between 2nd February 2000 and 30th April 2012. The study was initiated in April 2012 and the analysis of the data started on 1st May 2012. No power analysis was conducted. The following clinical data were extracted from medical records: reason for presentation, history of substance abuse, history of transmissible disease and rehospitalisation rate. No nursing records were consulted. Demographical data such as gender, age and nationality were also recorded. All medical records were reviewed by an internal specialist and a specialist in emergency medicine. Records of patients with psychiatric disorders were discussed with a psychiatrist. The data were categorised into three disciplines (internal medicine, surgery, psychiatry). The reason for presentation was extracted according to diagnosis and medical history; no International Classification of Diseases (ICD) 10 coding was used. Diagnoses were grouped. Each patient was assigned to only one group (e.g., cuts with suicidality - suicidality). If the patient presented for more than one reason, the major cause for presentation was determined by the study team. For all categorisations, all specialists had to agree independently. Patients with incomplete medical records (rudimentary anamnesis; n = 667) and duplicated records (n = 9) were excluded from the analysis. Patients who were excluded were neither unstable nor transferred before completion of medical records, nor did they present out of office hours.
All statistical analyses were performed with the SPSS 20.0 Statistical Analysis program (SPSS Inc; Chicago, IL). Descriptive statistics (i.e, numerical, percentage data, means and standard deviations (SDs)) were used to analyse most of the data. The significance of the data was analysed with the chi-squared test (Pearson, Fisher exact test) for qualitative data and the unpaired t-test and unidirectional analysis of variance (ANOVA; Tamhane-T2) for quantitative data. All p values were two-tailed, with a level of significance of 0.05.
The study was approved by the ethical commission of the Canton of Bern, Switzerland. Individual patient consent was not obtained.
A total of 1703 patients were available for analysis. Of these, 78.2% (n = 1333) were male and 21.8% (n = 370) female. The mean age was 36.6 years (SD 14.6, range 16–92 years). Female patients were significantly older than male patients (p <0.001, 95% confidence interval (CI) 3.1–6.4). Patient characteristics in our study are summarised in table 1. For comparison with prisoners' characteristics in the whole of Switzerland, see table 2 [4]. The annual number of prisoners in our emergency centre increased from 122 prisoners in 2001 to 222 prisoners in 2011.
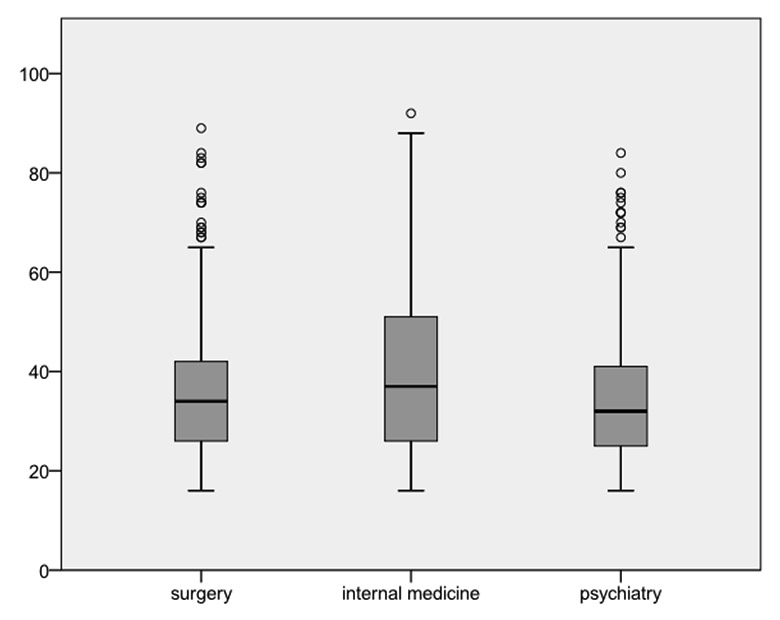
Figure 1
Age distribution and reason for presentation (clinical discipline). The boxes represent medians with 25% and 75% centiles.
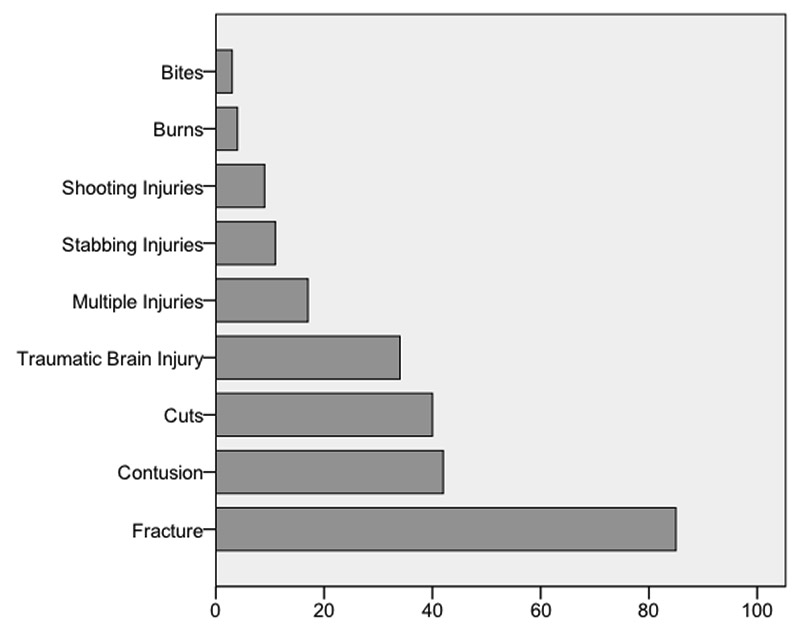
Figure 2
Summary of admissions related to trauma (number of patients per category).
The largest group of prisoners were Swiss, who accounted for 49.7% (n = 847) of all patients, followed by other Europeans (15.4%; n = 263), Africans (16.8%; n = 286) and other nationalities (18.0%; n = 307). The ratio of Swiss to foreign prisoners decreased from 1.22 in 2001 to 0.94 in 2011 (p <0.001). Foreigners were significantly younger than the Swiss (p <0.001, 95% CI 7.3–10.0).
The most frequent reasons for presentation were psychiatric problems (43.4%; n = 739), followed by need for medical treatment (31.6%; n = 539) and for surgical treatment (25.0%; n = 425).
In all, 8.7% (n = 149) of our patients suffered from underlying transmissible diseases: 1.7% (n = 29) from isolated HIV disease, 4.2% (n = 72) from isolated hepatitis C, 0.4% (n = 7) from isolated hepatitis B, 1.6% (n = 27) from tuberculosis and 2.2% (n = 38) from a combination of transmissible diseases. These patients were predominantly younger than the others (p <0.001, 95% CI 2.2–2.6) and predominantly male (p <0.047). Overall, 16.7% (n = 284) of patients suffered from an addiction: 4.1% (n = 70) had a chronic alcohol problem, 9.6% (n = 164) multiple drug addictions and 2.9% (n = 50) were both drug and alcohol abusers. Patients with addiction problems were significantly younger than the patients without addiction (p <0.007, 95% CI 0.8–5.0), but neither predominantly male nor female (p <0.31).
Of the surgical patients, 82.6% (n = 351) were male and 17.4% (n = 74) female. Their overall mean age was 36.0 years (SD 13.3, range 16–89 years). Patients with surgical presentations were significantly younger than patients with medical problems (p <0.001, 95% CI 2.3–7.1), but not younger than patients with psychiatric problems (p <0.016, 95% CI 0.3–4.0; fig. 1). Of the surgical patients, 57.6% (n = 245) suffered from injuries. An overview of reasons for presentation related to trauma is shown in figure 2. The most frequent nontraumatic surgical presentations (42.4% n = 180) were related to abdominal pain (75.6%, n = 136), followed by musculoskeletal symptoms (15.0%, n = 27) and urolithiasis (9.4%, n = 17).
Of the medical patients, 77.0% (n = 415) were male and 23.0% (n = 124) female. Patients with medical problems were significantly older than patients with psychiatric (p <0.001, 95% CI 2.3–7.1) and surgical presentations (p <0.001, 95% CI 4.7–9.0; fig. 1). Infectious diseases were most frequent (29.1%; n = 157), followed by cardiac diseases (21.7%; n = 117), neurological diseases (16.7%; n = 90), body packers (16.5%; n = 89), gastroenterological diseases (4.1%; n = 22), vascular diseases (3.5%; n = 19), diabetic problems (3.2%; n = 17), respiratory diseases (2.7%; n =15) and other diseases (2.4%; n = 13).
Of the patients with psychiatric problems, 76.7% (n = 567) were male and 23.3% (n = 172) female. Their mean age was 33.9 years (SD 11.3, range 16–84 years). Patients with psychiatric problems were significantly younger than those with medical or surgical problems (p <0.001, 95% CI 4.6–7.5; fig. 1). Figure 3 shows details of the psychiatric admissions. Of the patients presenting with autoaggression, 71.3% (n = 251) were suicidal and 28.7% (n = 101) autoaggressive but not suicidal. Of the patients with substance abuse, 38.4% (n = 53) presented with alcoholic intoxication, 44.9% (n = 62) with intoxication from drugs or medicine and 16.7% (n = 23) with withdrawal symptoms. Of the patients with intoxication, 28.3% (n = 39) were known alcoholics and 31.9% (n = 44) known to have multiple drug dependencies.
Overall, 130 (7.6%) of our patients were rehospitalised within the study period. Of these patients, 86.9% (n = 113) were male, 13.1% (n = 17) were female. Their mean age was 33.9 (SD 11.1, range 17–83). Rehospitalised patients were significantly younger than others (p <0.031, 95% CI 0.3–5.5).
| Table 1: Characteristics of the patients in our study (n = 1703). | |
| Characteristic | |
| Age, mean (SD) | 36.6 (14.6) |
| Gender, n (%) male female | 1333 (78.2%) 370 (21.8%) |
| Nationality, n (%) Swiss non-Swiss Reason for presentation, n (%) surgical medical psychiatric | 847 (49.7%) 856 (50.3%) 425 (25.0%) 539 (31.6%) 739 (43.4%) |
| History of transmissible disease, n (%) History of substance abuse, n (%) Rehospitalisation, n (%) | 149 (8.7%) 284 (16.7%) 130 (7.6%) |
| Table 2: Characteristics of prisoners in Switzerland in 2011 (n = 8546) [4]. | |
| Characteristic | n (%) |
| Age distribution younger than 40 years older than 60 years | 7463 (87.3%) 163 (2.2%) |
| Gender male female | 7860 (91.9%) 656 (8.1%) |
| Nationality Swiss non-Swiss | 3105 (36.3%) 5441 (63.7%) |
The number of prisoners treated in our emergency centre is rising, but is still only a small percentage (0.41%) of all consultations. A literature search in PubMed and the Cochrane Database using appropriate linked terms did not show any results on prisoners and emergency department use. We therefore conclude that prisoners’ healthcare problems that lead to emergency department admission are rarely studied. To the best of our knowledge, this is the first study on the impact of prisoners on emergency medicine.
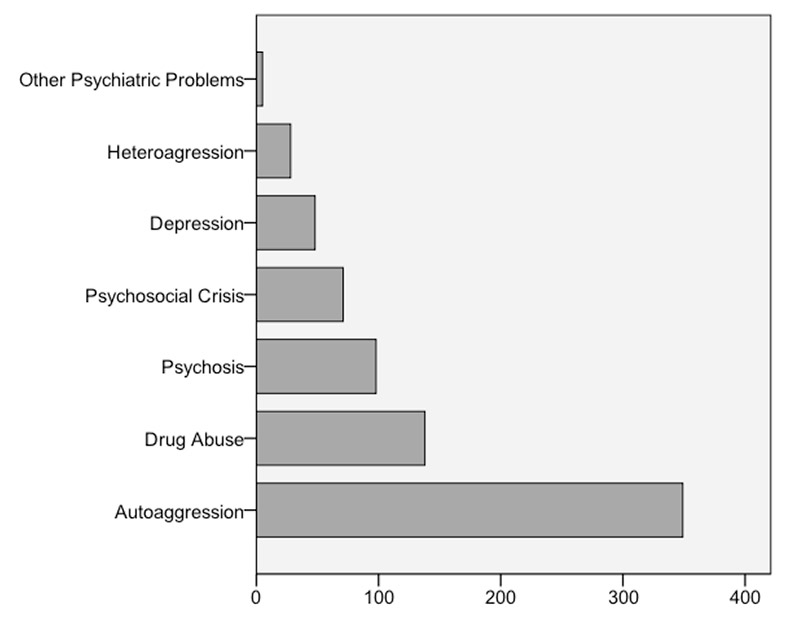
Figure 3
Summary of admissions for psychiatric diseases (number of patients per category).
About a fifth of our study population was female. This figure is notably higher than the proportion of women found in a British study on gender differences, age differences and minorities in prisons, in which the percentage of women was 6% [8]. We had a male to female ratio of 3.35 in 2011, a ratio that is markedly lower than the value of 11.45 found for all of Switzerland [4] (see table 2). It is difficult to say why the number of female prisoners was so high in our study. Several studies have indicated that female prisoners suffer from a higher number and more severe diseases than male prisoners [9, 17]. A further reason for the high rate of admissions of female prisoners may be the proximity of the Inselspital to a female detention facility.
The least frequent reason for presentation to our emergency centre was a need for surgery. There is little published information on this issue. In a study on the self-reported health problems of 914 prisoners, Butler et al. found that 19% of the women and 18% of the men had suffered an injury in the previous 3 months, with a total of 11% head injuries [10]. This is markedly greater than our overall value of 14%. We can only speculate about the reasons. It is nevertheless possible that many of these injuries were not sufficiently severe to lead to presentation at our emergency centre.
The second most frequent reason for presentation to our emergency centre was that the prisoner was suffering from an internal medical emergency. The high number of medical presentations may be due to a variety of factors, some of them social [3, 8, 10]. For example, a study by Plugge et al. on the prevalence of cardiovascular risk factors and the influence of prison showed that many women have a striking profile of cardiovascular risks when they are first admitted to prison [9]. In this study, 85% of women smoked on admission, 87% took no sort of physical exercise and more than 30% were obese [9]. We assume that the high rate of presentation for cardiological and cerebrovascular diseases that we found is due to the high prevalence of cardiovascular risk factors in prisoners. This emphasises how important it is to investigate patients’ cardiovascular risk profiles when they present to an emergency centre. The opportunity must then be taken to perform diagnostic testing and perhaps to start therapy for cardiac risk factors.
The establishment of telemedicine in prisons has been proven to increase appropriate access to care [18, 19]. According to a review by Meystre et al. telemonitoring is promising for patients with chronic illnesses such as cardiopulmonary diseases and asthma [20], diseases from which many of the patients in our study suffered. It has been shown that telemedicine reduces delays in the transfer of patients with potential exacerbations of chronic medical conditions [18, 19], and decreases transfer rates from prisons to emergency departments by 38% [19]. A study by Fox et al. on timeliness and access to healthcare services via telemedicine for adolescents in prisons even showed a reduction of 7% in emergency department admissions [18].
Our study confirms reports that many prisoners suffer from transmissible infectious diseases [1, 3]. The review of Watson et al. [3] estimated that the prevalence of transmissible diseases may be up to 20% greater in prison than in the general population. It is of the greatest importance that the emergency team should be aware of the high prevalence of transmissible diseases in the prison population. On one hand, they must attempt to detect these diseases. On the other hand, they should use appropriate protective measures (isolation, mask, gloves) before starting treatment.
Psychiatric problems were the most frequent reason for presentation to our emergency centre. The high numbers of prisoners with psychiatric diseases has been repeatedly reported [1–3, 6, 21]. There is evidence that psychiatric diseases in prison can be much more easily detected if standardised assessments are used [22]. Because of the high prevalence of psychiatric diseases in prisons, it would be sensible to screen every prisoner presenting to the emergency centre. Staff must be trained and a psychiatrist consulted if there is any doubt. Furthermore, evidence has shown that psychiatric disorders also may often may be treated via telemedicine [23]. According to the findings by Davies et al. in their study on telemedicine and psychiatric disorders, telemedicine promises to initiate treatment early, to improve the quality of care, and to reduce the length of hospital stay [23]. Additionally, they showed that the implementation of a hospital-driven telepsychiatry network reduces healthcare costs [23].Therefore, telemedical consultation between the emergency department staff and prison staff should be established to avoid unnecessary emergency department admissions and healthcare costs.
There are several limitations to the study. Because of the retrospective study design, misinterpretations cannot be excluded. We therefore also assume that our figures on multiple drug dependence, alcohol consumption and transmissible diseases underestimate the actual prevalence in this population. The exclusion of 667 patients because of a lack of clinical data may also bias our results. Moreover, our data collection was not standardised. It should also be noted that this study does not represent a cross-section of the state of health of the whole prison population, as prisoners who present to our emergency centre suffer from potentially serious diseases.
The prisoners in our study suffered from many psychiatric and infectious diseases, together with an increased risk of cardiovascular diseases. They are a vulnerable minority group within our society with limited access to medical care. Our emergency centre is a primary site of treatment for prisoners and is a fundamental component of the provision of basic medical care for this population. If an emergency centre works with prisoners, there are personnel and structural requirements that clearly differ from those for the “normal” population.
It is of great importance to smooth the transfer of information between the emergency department and prison staff, for example with a telemedical service. Furthermore, it is important that further, more wide-ranging research on the healthcare problems of prisoners is performed, so that conclusions and recommendations can be made for the general population of prisoners in Switzerland who need access to health care.
Acknowledgement:The authors wish to thank Beat von Baeriswyl from the Federal Office for Statistics for providing data for the whole of Switzerland on persons serving prison sentences and Mr Rodney Yeates for language editing.
1 Fazel S, Baillargeon J. The health of prisoners. Lancet. 2011;377(9769):956–65.
2 Vetter C, Robert-Tissot L, Cottagnoud P, Stucki A. Working under pressure. Praxis. 2008;97(8):437–42.
3 Watson R, Stimpson A, Hostick T. Prison health care: a review of the literature. Int J Nurs Stud. 2004;41(2):119–28.
4 Statistiken zum Strafvollzug [http://www.bfs.admin.ch/bfs/portal/de/index/themen/19/03/05/key/vollzug_von_sanktionen/strafvollzug.html.] 27.09.2012
5 Plugge E, Douglas N, Fitzpatrick R. Patients, prisoners, or people? Women prisoners’ experiences of primary care in prison: a qualitative study. The British journal of general practice: the journal of the Royal College of General Practitioners 2008;58(554):630–6.
6 Fraser A, Gatherer A, Hayton P. Mental health in prisons: great difficulties but are there opportunities? Public health. 2009;123(6):410–4.
7 Ford PM, Wobeser WL. Health care problems in prisons. CMAJ: Canadian Medical Association journal = journal de l’Association medicale canadienne 2000;162(5):664–5.
8 Harris F, Hek G, Condon L. Health needs of prisoners in England and Wales: the implications for prison healthcare of gender, age and ethnicity. Health & social care in the community. 2007;15(1):56–66.
9 Plugge EH, Foster CE, Yudkin PL, Douglas N. Cardiovascular disease risk factors and women prisoners in the UK: the impact of imprisonment. Health promotion international. 2009;24(4):334–43.
10 Butler T, Kariminia A, Levy M, Murphy M. The self-reported health status of prisoners in New South Wales. Aust N Z J Public Health. 2004;28(4):344–50.
11 Rosen DL, Hammond WP, Wohl DA, Golin CE. Disease prevalence and use of health care among a national sample of black and white male state prisoners. J Health Care Poor Underserved. 2012;23(1):254–72.
12 Fazel S, Benning R. Natural deaths in male prisoners: a 20-year mortality study. Eur J Public Health. 2006;16(4):441–4.
13 Fazel S, Hope T, O’Donnell I, Piper M, Jacoby R. Health of elderly male prisoners: worse than the general population, worse than younger prisoners. Age Ageing. 2001;30(5):403–7.
14 Pfortmueller CA, Graf F, Tabarra M, Lindner G, Zimmermann H, Exadaktylos AK. Acute health problems in African refugees: Ten years’ experience in a Swiss emergency department. Wiener klinische Wochenschrift 2012.
15 Bewachungsstation Inselspital ['Http://www.Pom.Be.Ch/Pom/De/Index/Freiheitsentzug-Betreuung/Gefaengnisse/Bewachungsstationaminselspital/Medizin.Html'.] Last access: 03.09.2012
16 Universitätsklinik für Allgemeine Innere Medizin, Jahresbericht 2010. In., vol. 2010. Bern: Inselspital Bern; 2010.
17 Singleton N MH, Gatward R. Psychiatric Morbidity among Prisoners in England and Wales. London: Office for National Statistics; 1998.
18 Fox KC, Somes GW, Waters TM. Timeliness and access to healthcare services via telemedicine for adolescents in state correctional facilities. The Journal of adolescent health: official publication of the Society for Adolescent Medicine 2007;41(2):161–7.
19 Ellis DG, Mayrose J, Phelan M. Consultation times in emergency telemedicine using realtime videoconferencing. J Telemed Telecare. 2006;12(6):303–5.
20 Meystre S. The current state of telemonitoring: a comment on the literature. Telemedicine journal and e-health: the official journal of the American Telemedicine Association 2005;11(1):63–9.
21 Rabe K. Prison structure, inmate mortality and suicide risk in Europe. Int J Law Psychiatry. 2012;35(3):222–30.
22 Metzner J.L. MRD, Kleinsasser D. Mental health screening and evaluation within prisons. Bulletin of the Academy of Psychiatry and Law. 1994;22:451–7.
23 Davies SF. A hospital driven telepsychiatry initiative to improve patient care and reduce costs. North Carolina medical journal. 2012;73(3):228–30.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.