Congenital syphilis in Switzerland: gone, forgotten, on the return
DOI: https://doi.org/10.4414/smw.2012.13325
Sauteur
Meyer, J
Trück, PP
Bosshard, M
Tomaske, Cadenas
Morán, S
Lautenschlager, P
Goetschel
Summary
INTRODUCTION:Acquired syphilis has re-emerged in many Western European countries. In contrast to international guidelines, screening for syphilis in pregnancy is not generally recommended in Switzerland. There has been an increase in the incidence of laboratory syphilis notifications in recent years, regardless of gender and age.
METHODS: We conducted a retrospective study, evaluating the total numbers of pregnant women with positive syphilis serology (Treponema pallidum Particle Agglutination assay, TPPA) from 2000 to 2009, and evaluated the clinical management and outcome of their offspring. In addition, we sought to determine cases of infectious syphilis (primary, secondary, and early latent syphilis) reported to the Swiss Federal Office of Public Health in women of childbearing age, which has previously been shown to precede changes in the incidence of congenital syphilis within a population.
RESULTS: Out of 13,833 women who gave birth at our institution, positive syphilis serology was found in 9 pregnant women during the 10 years studied. A total of 6 pregnant women were diagnosed having syphilis infection during pregnancy. Regarding their offspring, 8 of the 9 newborns were tested serologically. One neonate experienced congenital syphilis because the adequately treated mother developed re-infection after treatment. Within the Swiss population, infectious syphilis cases in women of childbearing age increased substantially from 2006 to 2009.
CONCLUSIONS: The epidemiologic data suggest that congenital syphilis could become a medical problem in Switzerland due to the rise of infectious syphilis cases in women of childbearing age that have been shown to be followed by changes in the congenital syphilis incidence. The persistence of congenital syphilis in Switzerland along with this rise of infectious syphilis in women of childbearing age suggests a potential for improvement of prenatal care and syphilis control programmes.
Abbreviations
CDC: US Center for Disease Control and Prevention
CS: Congenital syphilis
EIA: Enzyme immunoassay
FTA-ABS: Fluorescent Treponemal Antibody-Absorption test
IUSTI: International Union against Sexually Transmitted Infections
MSM: Men who have sex with men
SFOPH: Swiss Federal Office of Public Health
SPSU: Swiss Paediatric Surveillance Unit
STI: Sexually transmitted infection/sexually transmitted disease
TPHA: Treponema Pallidum Haemagglutination assay
TPPA: Treponema Pallidum Particle Agglutination assay
VDRL: Veneral Disease Research Laboratory test
WHO: World Health Organization
Introduction
Syphilis is a sexually acquired infection caused by the spirochete Treponema pallidum. Many people with syphilis have unrecognised disease. Thus, transmission may occur from persons who are unaware of their infection [1]. As a separate entity, congenital syphilis (CS) is a serious condition [2]: it is associated with miscarriage, stillbirth, foetal abnormalities, and prematurity. Babies born with syphilis develop either an early symptomatic disease (early CS) or may be asymptomatic at birth developing serious problems later (late CS).
In Western Europe, the incidence of syphilis has been increasing since the late nineties [3]. Switzerland has two distinctive features regarding syphilis surveillance: first, syphilis was removed from the list of notifiable sexually transmissed diseases (STIs) in 1999 due to decreasing incidence rates but was re-included in 2006 due to recognition of rising rates of disease [4–6]. Second, syphilis screening on a regular basis during pregnancy was stopped during the 1990s and has not been routinely performed since that time [7]. This is in contrast to worldwide guidelines and the course of action of almost every nation in the world [8, 9].
We aimed to assess recent trends of syphilis cases in pregnant women and neonates in Switzerland. Therefore, we analysed data between 2000 and 2009 from a large urban hospital to evaluate the total numbers of pregnant women tested seropositive for syphilis, and the clinical management and outcome of the neonates born to these mothers. In addition, we reviewed national surveillance data from recent years captured by the Swiss Federal Office of Public Health (SFOPH) in order to assess infectious syphilis cases in women of childbearing age, as changes in this measurement have been previously shown to precede similar changes in the incidence of CS [10].
Methods
In Zurich, the Triemli Hospital Zurich is an urban hospital with approximately the seventh largest maternity unit in Switzerland providing increasing numbers of live births (from 1,246 in 2000 to 1,654 in 2009). In all pregnant women who gave birth in Triemli Hospital Zurich, those with conducted syphilis serology were further analysed and only cases with a positive serology were included in the study. Women were defined as seropositive if the T. pallidum Particle Agglutination assay (TPPA) was positive at any time during pregnancy. In most cases in which TPPA was positive, the Veneral Disease Research Laboratory test (VDRL), the Fluorescent Treponemal Antibody-Absorption test (FTA-ABS), and an IgM enzyme immunoassay (EIA) test (Pathozyme Syphilis M Capture) were performed. We evaluated the clinical management and analysed the outcome of the neonates born to these mothers by review of the patient's medical records. The study was approved by the ethics committee of Zurich (Study No. 2009-0050/0).
In Switzerland, since 2006, all syphilis cases have to be reported to the SFOPH by laboratories and attending clinicians. Each case is classified by the SFOPH according to the supporting clinical information, which means that cases cannot be classified if this information is missing or incomplete. Out of this database, we were especially interested in the numbers of confirmed infectious syphilis cases among women in the childbearing age group (20–44 years) for the years 2006 to 2009.
Results
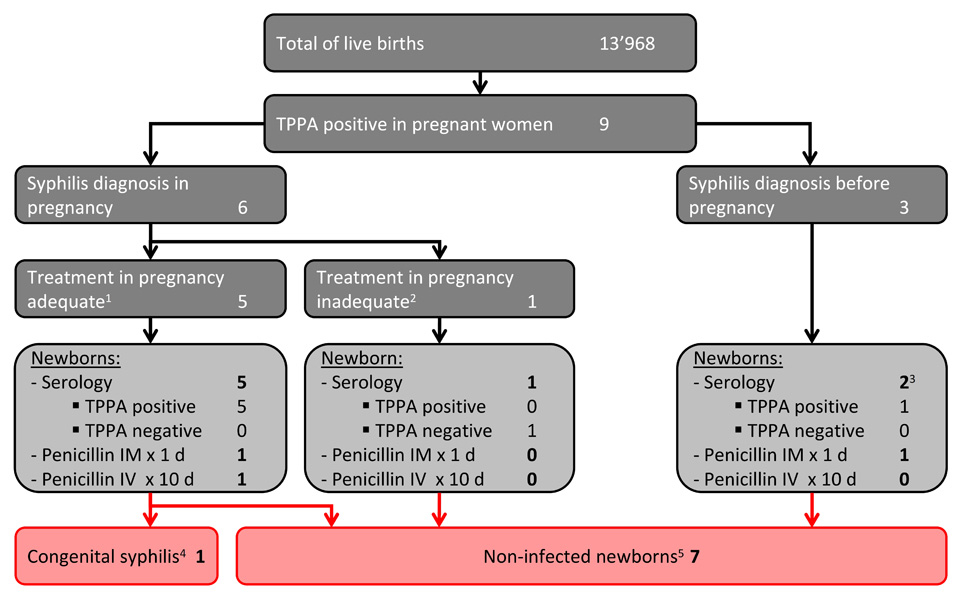
During the study period, 13,833 women delivered 13,968 infants (135 twins). A positive syphilis serology was found in 9 pregnant women giving birth to 9 children (fig. 1) with the following distribution: 2000: 1 (case), 2001: 1, 2002: 2, 2005: 1, 2006: 1, 2009: 3 (data not shown). Out of these 9 women, 6 were newly diagnosed in pregnancy: 5 were found to have active or latent syphilis (re-)infection and received antibiotic treatment, and 1 residual antibody titre of a past infection (Appendix 1). A total of 8 of the 9 women were immigrants.
Regarding their offspring, 8 of the 9 newborns were tested serologically after birth (fig. 1). The results showed a total of 5 children with positive TPPA at birth, negative IgM antibodies, and no signs of CS, and 1 case of symptomatic CS together with a high positive IgM antibody concentration (Appendix 2). In 2 of the newborns of adequately treated mothers, a single dose of penicillin IM was administered directly after birth.
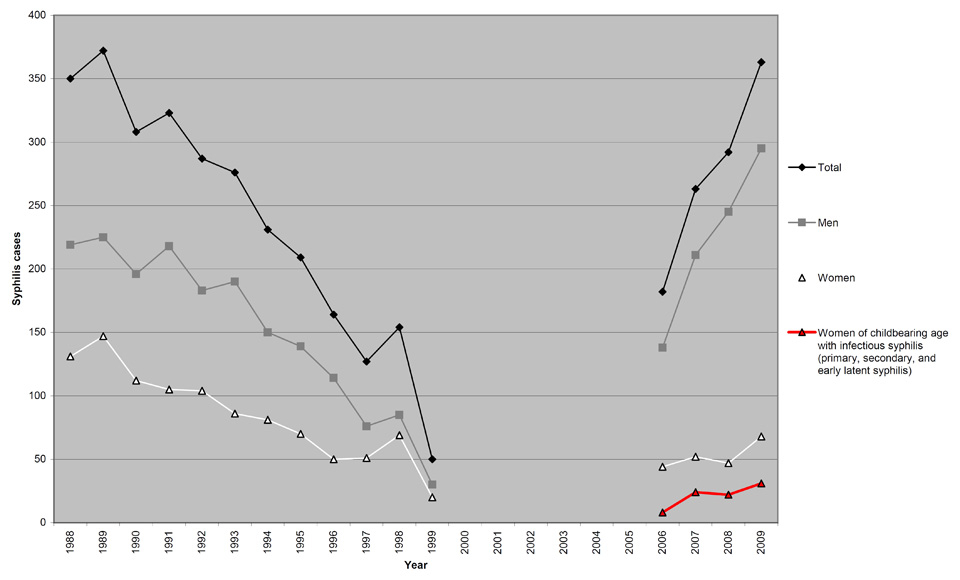
Within the SFOPH database, nearly 75% of confirmed cases in females were found in 20–44 year old women, which is the age group accounting for almost 99% of all births in Switzerland. Including only cases classified as being infectious (primary, secondary, and early latent syphilis), numbers in this age group increased from 8 cases in 2006 to 31 cases in 2009 (fig. 2).
Discussion
Recent data show an increasing syphilis incidence in other developed and newly industrialised countries [10, 11]. Since 2006, syphilis is clearly re-emerging also in Switzerland [4–6]. The reported cases are amongst the highest in Western Europe [12] with a parallel increase of other STIs [4–6, 13], also as a consequence of a better notification compliance. Along with the rise of reported syphilis cases, infectious syphilis in women of childbearing age increased substantially from 2006 to 2009 (fig. 2), which implies that a substantial proportion of syphilis testing is performed as part of the prenatal screening. The increasing numbers of infected women is worrisome and suggests either novel sexual networks, a change in sexual behaviour or an increased "heterosexual bridging" from contacts with men who have sex with men (MSM) [14]. Although true incidences cannot be calculated through the current notification approach, both the numbers themselves as well as the trend of reported cases suggest an increase in syphilis cases in all ages and both sexes in Switzerland [6]. As changes in the population incidence have been shown to be followed by similar changes in the CS incidence [10, 11, 15], the epidemiologic data suggest increasing numbers of CS cases in Switzerland. Although CS numbers were low throughout the whole study period, we found 1 case of symptomatic CS together with a peak of 3 syphilis seropositive pregnant women in 2009.
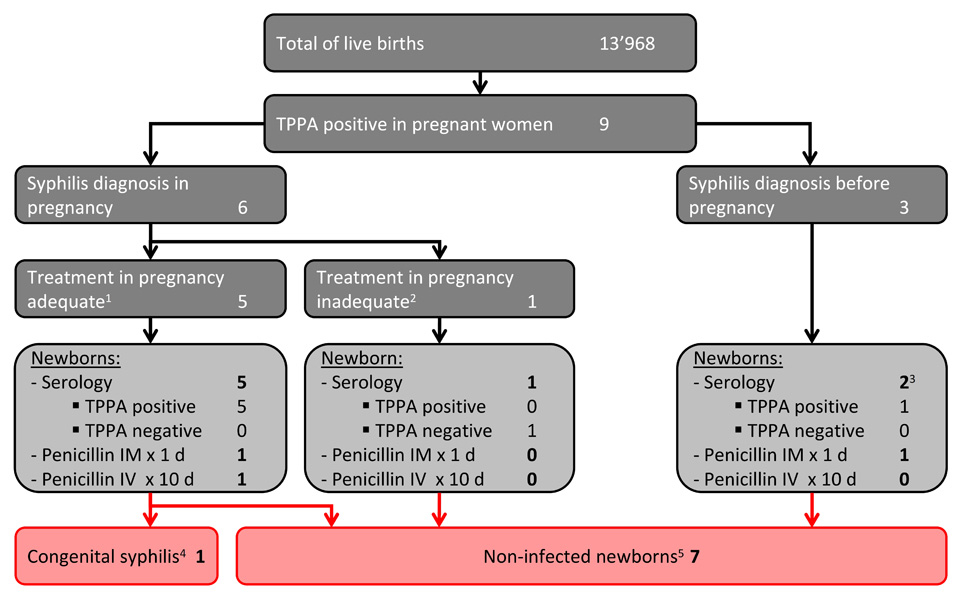
Figure 1
Antenatal syphilis serology, Triemli Hospital Zurich, 2000–2009.
1 Adequate treatment: documented treatment with a penicillin regimen according to current guidelines, and completed ≥4 weeks prior to delivery, and no evidence of treatment failure (as might be suggested, e.g., by unchanged or increasing VDRL titers), and no evidence of syphilis re-infection or relapse.
2 Inadequate treatment: no treatment, no documentation of treatment, treated with a non-penicillin regimen, evidence for treatment failure or treatment completed <4 weeks prior to delivery.
3 One newborn tested only with IgM EIA and without TPPA.
4 Symptomatic disease with IgM EIA test positive and abnormal placental exam (Appendix 2).
5 All parts of the infant's evaluation normal and in 7 of 8 newborns negative syphilis serology (IgM test negative, VDRL <4-fold than maternal VDRL, and placental exam negative (if performed)) (Appendix 1).
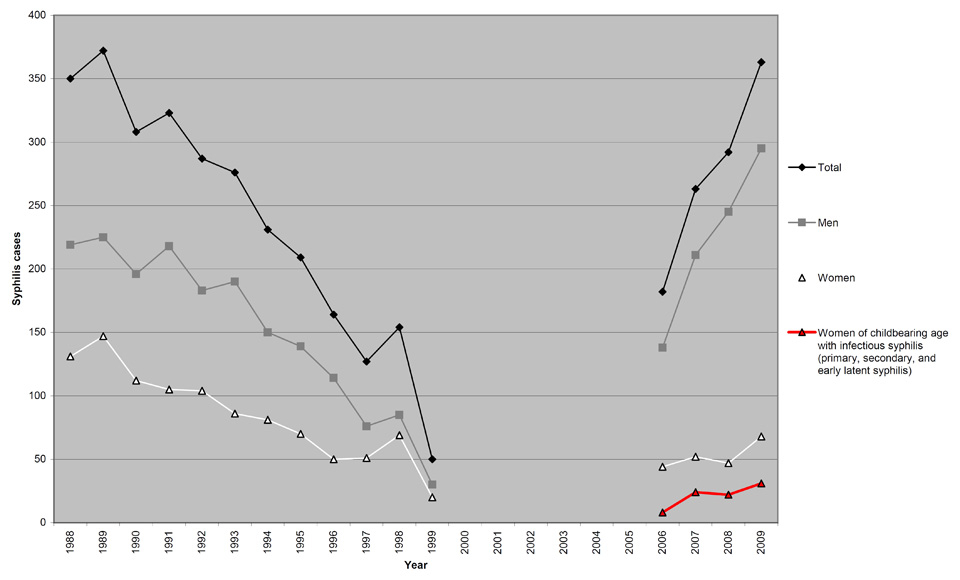
Figure 2
Confirmed infectious syphilis cases among women aged 20–44 years (childbearing age group), 2006–2009 (in red), together with total numbers of laboratory syphilis notification in Switzerland, 1988–2009 (adapted from [5, 6]).
1988–1999: laboratory notifications (Swiss Sentinel Network on STIs);
2000–2005: data not reported for syphilis;
Since 2006: laboratory and clinical notifications (SFOPH and attending physicians).
CS is a preventable disease and syphilis pregnancy screening is an effective measure, both for prevention of the disease as well as for treating pregnant women and their partners [14, 16–18]. The most important risk factor for CS is inadequate prenatal care with an associated lack of syphilis screening [11]. Therefore, the WHO recommends that all pregnant women should be screened for syphilis in pregnancy mainly because of the asymptomatic latent stage of the disease [8]. In Europe, TPPA and TPHA are established as a screening test, with EIA as an alternative [19, 20]. The screening should be done at the first antenatal visit and potentially repeated in the third trimester of pregnancy, and every not yet screened woman must be screened immediately at or after birth [8, 14, 21, 22]. Diagnosis and management of maternal syphilis is complex, leading to uncertainties and time-consuming discussions amongst clinicians. Usually, at least 3 to 4 clinical disciplines are involved (obstetricians, paediatricians, infectious disease specialists, and dermatologists). This complexity is reflected by the fact that we found a great disparity in the management of mothers with a positive syphilis serology and their offspring in our study cohort.
As most of the syphilis screening serologies are performed in private practice in Switzerland and are not documented in the hospital notes, we were not able to retrieve the total number of serologies obtained during the study period, which would have enabled us to calculate sero-prevalences. It is conceivable that in our study some CS cases remained undetected and untreated, simply because (1) pregnancy screening was done externally but women gave birth in the study hospital, (2) due to false-negative screening serologies performed in an early stage of disease, or (3) because there was no serology performed at all. Even symptomatic cases of CS might have been undetected because this disease often presents with unspecific clinical signs. Therefore, the number of seropositive mothers detected in our hospital during the study period is a very conservative estimate and might be underestimated.
Conclusion
Although our study shows only one case of (true) CS, the epidemiologic data suggest more cases due to the rise of infectious syphilis cases in women of childbearing age that have been shown to be followed by changes in the CS incidence within a population. The findings presented in our study should guide public health professionals in planning surveillance and target preventive campaigns, for example by a prospective screening study in several large maternity units in Switzerland and an introduction of a surveillance system for CS by the Swiss Paediatric Surveillance Unit (SPSU). The persistence of CS in Switzerland suggests a potential for improvement of prenatal care and syphilis control programmes.
Appendix 1
Characteristics of syphilis seropositive mothers and their infants in pregnancy and at follow-up examination, Triemli Hospital Zurich, 2000–2009.
Appendix 2
At 33 weeks of gestation, a 25-year-old woman (gravida 5, parity 3) was found to have positive syphilis serology, indicating a syphilis re-infection, as she had reported a syphilis infection 3 years before. She was diagnosed as having early latent syphilis, and received penicillin G benzathine three times at 1-week intervals (7.2 million units IM total). At delivery (1 month after treatment), a two-fold increase in VDRL and TPPA titers as well as a persisting elevated IgM antibody concentration was found. This serology was interpreted as a re-re-infection after adequate treatment in pregnancy. The male sexual partner(s) couldn’t be identified and treated.
The foetus showed intrauterine growth retardation without any other ultrasonographic abnormalities and was born through normal vaginal birth at 39 weeks of gestational age. Foetal adaptation at birth was normal with APGAR scores of 8, 9 and 10 at 1, 5 and 10 minutes, and an umbilical arterial pH of 7.34. The boy’s birth weight was 2560 g, height was 45 cm, and head circumference was 32.2 cm (all measurements below the 3rd percentile for gestational age). Wrinkled skin with a generalised papulosquamous rash was noted at delivery particularly with scaly plaques on the palms and soles. The remainder of the physical examination was unremarkable; in particular no hepatosplenomegaly or lymphadenopathy could be identified. Histologically, the placenta showed funiculitis, delayed maturation of villi together with villous arrest and endangiitis obliterans. Admission to the neonatal intermediate care unit followed for further assessment and treatment.
The infant’s syphilis serology showed positive TPPA and VDRL test results (similar titers compared to the titers of the mother at the same time point), and a high positive IgM antibody concentration. On grounds of the clinical findings and the serology results, this child was found to have congenital syphilis. A CSF sample obtained during the first day of life showed normal cell count and chemistry results. Long-bone radiographs showed metaphyseal destruction (Wimberger’s lines) and osteochondritis.
The patient was treated with aqueous crystalline penicillin G for 10 days (50,000 units/kg per dose IV every 12 hours for 7 days, followed 8-hourly for 3 days). At the time of hospital discharge after 12 days, the dermal involvement had markedly improved. A follow-up serology 8 months after treatment showed a non-reactive VDRL test and a decrease in the IgM antibody concentration. We weren’t able to perform a further syphilis serology as planned at one year of age as the family was lost to follow-up.
Acknowledgement: We thank David Nadal, Director of the Pediatric Research Center and Head of the Division of Infectious Diseases and Hospital Epidemiology, University Children's Hospital of Zurich, for crucial feedback on the manuscript.
References
1 Doroshenko A, Sherrard J, Pollard AJ. Syphilis in pregnancy and the neonatal period. Int J STD AIDS. 2006;17(4):221–7; quiz 228.
2 Chakraborty R, Luck S. Syphilis is on the increase: the implications for child health. Arch Dis Child. 2008;93(2):105–9.
3 Fenton KA, Lowndes CM. Recent trends in the epidemiology of sexually transmitted infections in the European Union. Sex Transm Infect. 2004;80(4):255–63.
4 Lautenschlager S. Sexually transmitted infections in Switzerland: return of the classics. Dermatology. 2005;210(2):134–42.
5 Sexually transmitted infections (STI) in Switzerland, 1988–2006. Bull Swiss Federal Office of Public Health. 2008;8:140–9.
6 Sexually transmitted infections (STI) in Switzerland, until 2010. Bull Swiss Federal Office of Public Health. 2011;12:253–61.
7 Frischknecht F, Sell W, Trummer I, et al. Serological testing for infectious diseases in pregnant women: are the guidelines followed? Swiss Med Wkly. 2011;140:w13138.
8 WHO. The Global elimination of congenital syphilis: rationale and strategy for action. http://whqlibdoc.who.int/publications/2007/9789241595858_eng.pdf (accessed 24th October 2011).
9 Hossain M, Broutet N, Hawkes S. The elimination of congenital syphilis: a comparison of the proposed World Health Organization action plan for the elimination of congenital syphilis with existing national maternal and congenital syphilis policies. Sex Transm Dis. 2007;34(7 Suppl):S22–30.
10 Congenital syphilis – United States, 2003–2008. MMWR Morb Mortal Wkly Rep. 2010;59(14):413–7.
11 Tucker JD, Chen XS, Peeling RW. Syphilis and social upheaval in China. N Engl J Med. 2010;362(18):1658–61.
12 Robert-Koch-Institut. Syphilis in germany in the year 2008. Epid Bull. 2009;49:503–12.
13 Abraham S, Toutous-Trellu L, Pechere M, et al. Increased incidence of sexually transmitted infections in Geneva, Switzerland. Dermatology. 2006;212(1):41–6.
14 Cheng JQ, Zhou H, Hong FC, et al. Syphilis screening and intervention in 500,000 pregnant women in Shenzhen, the People's Republic of China. Sex Transm Infect. 2007;83(5):347–50.
15 Simms I, Broutet N. Congenital syphilis re-emerging. J Dtsch Dermatol Ges. 2008;6(4):269–72.
16 Blencowe H, Cousens S, Kamb M, et al. Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health. 2011;11(Suppl 3):S9.
17 Liu JB, Hong FC, Pan P, et al. A risk model for congenital syphilis in infants born to mothers with syphilis treated in gestation: a prospective cohort study. Sex Transm Infect. 2010;86(4):292–6.
18 Zhu L, Qin M, Du L, et al. Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. Int J Infect Dis. 2010;14(Suppl 3):e45–8.
19 French P, Gomberg M, Janier M, et al. IUSTI: 2008 European Guidelines on the Management of Syphilis. Int J STD AIDS. 2009;20(5):300–9.
20 Lautenschlager S. Diagnosis of syphilis: clinical and laboratory problems. J Dtsch Dermatol Ges. 2006;4(12):1058–75.
21 Lumbiganon P, Piaggio G, Villar J, et al. The epidemiology of syphilis in pregnancy. Int J STD AIDS. 2002;13(7):486–94.
22 Enders M, Knaub I, Gohl M, et al. Congenital syphilis despite prenatal screening? An evaluation of 14 cases. Z Geburtshilfe Neonatol. 2006;210(4):141–6.