Figure 1:
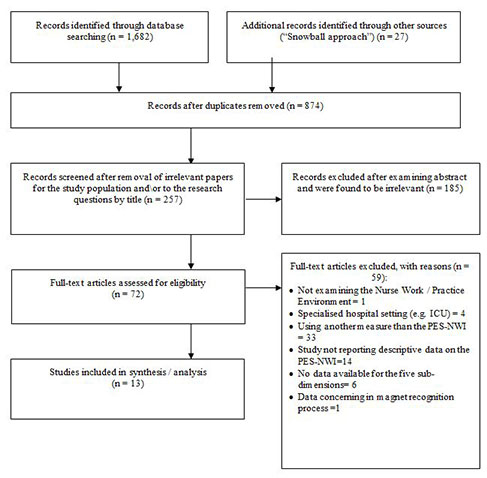
Flow diagram of study selection process.
DOI: https://doi.org/10.4414/smw.2012.13733
Excellence in nursing practice is recognised as a quintessential feature of high performing healthcare systems [1]. In order to achieve this, nurses need a work environment that permits and sustains the full expression of their skills and knowledge. The Magnet Recognition Program®, developed by the American Nurses Credentialing Centre (ANCC), is a well-known best practice model which includes guidelines for the development of supportive nurse work environments.
In the early 1980’s, as a result of a national study conducted by the American Academy of Nursing (AAN), 41 hospitals were awarded the “Magnet hospital” designation. Within the context of a severe nursing shortage, the aims of the AAN initiative were to identify hospitals that were successful in attracting and retaining nurses and to determine the organisational features those hospitals had in common that might account for their success [2]. The term ”Magnet” was used to illustrate the capacity to attract, retain and motivate professional nurses. In 1990, the AAN board of directors approved the “Magnet recognition program for excellence in nursing services®”. Since its inception, this accreditation programme has evolved, expanded to different types of care facilities, changed its name into the “ANCC Magnet Recognition Program®” and become a standard for excellence in nursing care and the nurse work environment. In 2007, the original 14 forces of Magnetism were refined into five Magnet Model Components: (1.) Transformational leadership, (2.) Structural empowerment, (3.) Exemplary professional practice, (4.) New knowledge, innovations and improvements, and (5.) Empirical quality outcomes. As a whole, these components cover structure, process and outcome features prerequisite to creating high quality nurse work environments that sustain excellence in nursing practice (for additional information on the Magnet Recognition Program®please visit the official ANCC’s homepage http://www.nursecredentialing.org/magnet.aspx).
Research on Magnet hospitals has shown that these hospitals have a higher quality of nurse work environment compared to Non-Magnet hospitals [3, 4]. A growing body of literature demonstrates that a more favourable nurse work environment is associated with better nurse outcomes (i.e., lower levels of burnout and lower overall stress), lower job dissatisfaction and lower intention to leave [5–8]. Also, in view of patient outcomes, studies have revealed the importance of the quality of the nurse work environment regarding patient safety: better nurse work environments are associated with lower mortality, fewer failures to rescue and lower nurse-sensitive adverse events such as medication errors, pressure ulcers, nosocomial infections or patient falls [9–16].
As a mechanism behind improved nurse and patient outcomes in Magnet hospitals, it has been suggested that a higher nurse work environment quality provides nurses with the organisational framework for practice development and a learning culture [17], leading to the development of evidence based practice, improved clinical decision-making and, finally, to an increased sense of professionalism [18–20]. Previous studies also confirmed the mediating role of the work environment on organisational trust and sustainability of work efficiency, both of which are associated with substantial economies for the organisation, including reduced lengths of stay and lower costs linked to turnover and adverse events [21, 22]. Consequently, Magnet hospitals have a positive image as high-quality healthcare organisations.
One key principle of the Magnet recognition process is that Magnet facilities continuously monitor and assess the quality of their nurse work environments. To measure and compare nurse work environment quality, the Practice Environment Scale of the Nursing Work Index (PES-NWI) is the most widely used and reported measure [23]. Developed by Lake in 2002 [24] from the Nursing Work Index (NWI), the PES-NWI is based on three research efforts: the American Academy of Nursing study on original “Magnet hospitals” in the early 1980s, the NWI development, and the use of revised NWI version to measure hospitals' organisational attributes [25]. In the US, leading organisations, including the ANCC, the Joint Commission or the National Quality Forum have all endorsed the PES-NWI as a valuable indicator. Cross-cultural use of the PES-NWI to monitor and assess the quality of the nurse work environment in international healthcare settings is growing [26–28].
Given the successes of Magnet hospitals in attracting and retaining nurses as well as providing high quality care, there is an increasing interest in Europe to understand Magnet hospital attributes [29, 30]. Over the last ten years many research efforts were made in translating and utilising cross-cultural measures to assess the quality of the nurse work environment in European hospitals. Although there is no evidence on the transferability and meaning of the Magnet concept as a whole to cross-cultural settings, several studies have confirmed the importance of the quality of nurses’ work environment for patient and nurse outcomes in European hospitals [31–34]. In Switzerland, no systematic study of the quality of nurses’ work environment in acute care hospitals has yet been conducted, and no national benchmarking of Swiss hospitals has been carried out on the topic. Little reliable information is available, then, on how nurses in acute care hospitals appraise the quality of their work environments, or the extent to which the quality of the nurse work environments in Swiss hospitals is comparable to the “best in class” (i.e. Magnet hospitals). Therefore, this study aimed (1) to describe the quality of the nurse work environment in a national sample of Swiss acute care hospitals, and (2) to benchmark findings on Swiss nurse work environments against published results from international Magnet hospital research.
In this multi-method study we combined two approaches to achieve the study aims. First, a structured literature review was conducted to obtain relevant international data on nurse work environments from Magnet hospital research. Second, we used nurse survey data from the Swiss arm of the international, multi-centre cross-sectional RN4Cast (Nurse Forecasting: Human Resources Planning in Nursing) study to describe the quality of the nurse work environment in 35 acute care hospitals.
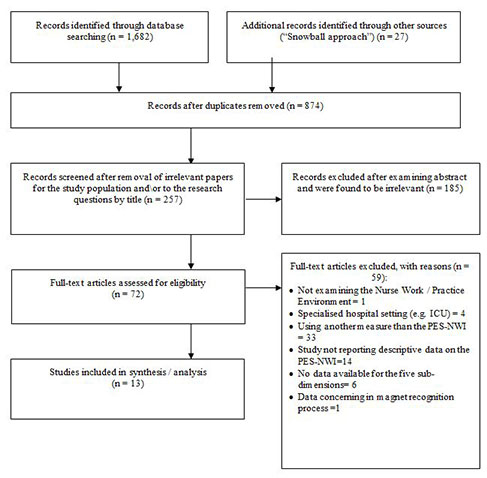
Figure 1:
Flow diagram of study selection process.
To compare Swiss findings on the nurse work environment with international data, we carried out a structured literature search of the electronic databases Medline (PubMed), Embase and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCOhost). The literature searches were completed in November 2011 (PubMed, CINAHL) and August 2012 (Embase) and were limited to primary studies. In the absence of adequate corresponding Medical Subject Heading (MeSH) Terms for the PubMed search, we combined the search terms “nurse work environment” as follows: “nurse work environment AND nurse work index”, “nurse work environment AND practice environment scale”, “nurse work environment AND Magnet hospitals”, “nurse work environment AND Non-Magnet hospitals”, and “nurse work environment AND Magnet recognition”. The same searches were also performed using the search terms “nurse practice environment” and “healthy work environment” instead of “nurse work environment”. In EBSCOhost we followed the same search strategy as in PubMed, combining the CINAHL subject heading MH “work environment” with all the search terms mentioned above. In addition we used the “snowball approach” by looking for relevant titles in the reference list of two recently published systematic reviews from 2010 and 2011, respectively [5, 26] to identify relevant papers.
Two researchers (MD and DA) carried out the literature search independently, filtering and sorting relevant articles according to title and abstract. Figure 1 is a flow diagram of the study selection process. The full papers of relevant articles were evaluated for eligibility according to our inclusion criteria: (a) published as peer reviewed article in English, German, French and Italian, (b) international studies in general acute-care hospital settings (e.g., medical / surgical units), (c) reporting on the nurse work / practice environment, measured with the “Practice Environment Scale of the Nurse Work Index” (Lake, 2002) and (d) descriptive data report on the nurse work / practice environment including data available for all sub-dimensions. To compare our Swiss data on the nurse practice environment with international data in a methodologically correct way, we included only studies that used the same measure: the Practice Environment Scale of the Nurse Work Index (PES-NWI) developed by Lake (2002) [24]. Studies that did not fulfil all inclusion criteria were excluded from further review. In case of differing selections of relevant articles, the two researchers discussed their selections based on the inclusion criteria list and made decisions jointly on inclusion or exclusion. In accordance with our research aim, we categorised studies using the PES-NWI, along with the resulting data, into nurse work environments in either “Magnet hospitals” (i.e., hospitals with Magnet accreditation) or “Non-Magnet hospitals” (i.e., those neither having nor undergoing Magnet accreditation).
Since there is no valid and reliable tool to assess the quality of observational studies [35], we applied the checklist from the STROBE guidelines for reporting observational epidemiological studies [36] to assess potential biases in eligible studies. As we were only interested in descriptive results (mean values) from the PES-NWI, we thus focused our quality assessment on the following domains to minimise the risk of bias in our results: (a) setting and participants, (b) measurement of the study variable (nurse work environment) and (c) appropriate use of descriptive statistics. Based on this quality control all eligible studies could be included in our review.
Switzerland was part of the international, multi-centre cross-sectional RN4cast study funded by the EU 7th Framework (EU Project number: 223468). The Swiss part of the RN4Cast study was conducted by the authors of this paper. The overall research aims and methodology of the international RN4Cast study have been described elsewhere [37, 38]. Between 2009 and 2011 all of the 12 participating European countries conducted the study within their countries according to a national study protocol [37, 38]. All European countries prospectively collected and transferred the survey data to the coordinating study centre at the University of Leuven (Belgium). Cross-national data analyses were carried out by the study centre in Leuven, Belgium in collaboration with the University of Pennsylvania (USA) and international results have already been reported [37, 38]. Each of the countries has full rights over its own data for analyses and dissemination of results. In this study we report on the Swiss data only with the subsequent sections describing Swiss-specific elements of the RN4Cast study.
For the Swiss arm of the RN4Cast study a quota sample of 35 Swiss acute-care hospitals was selected based on geographic location and hospital size. Hospitals were included if they had more than 60 acute care beds, employed more than 50 registered nurses (RNs) and both hospital directors and the chief nursing officers had provided written consent for study participation. In each hospital, we selected a random sample of general medical and surgical units or mixed medical-surgical wards. Within selected units, all RNs – except those on sick leave, maternity leave or vacation – were invited to complete the questionnaires.
All participating countries used standardised survey instruments to enable comparability of data across countries [37, 38]. According to the aims of this study paper we used the following variables from our survey data: the quality of the nurse work environment and characteristics of the participating RNs and hospitals.
Socio-demographic characteristics of the participating nurses, including gender, age, nurse education, employment and professional experience, and intention to leave were measured through single item questions from the nurse survey questionnaire. Characteristics of the participating hospitals included each institution's language region, hospital type, hospital size, hospital group and ownership, all of which were described based on information obtained from the Swiss Federal Office of Public Health prior to the hospital sampling procedure, and through an organisational variable questionnaire filled out by the chief nursing officers.
The quality of the nurse work environment was measured with the revised version of the PES-NWI [24], including 5 dimensions and a total of 32 items: (i) Nurse Participation in Hospital Affairs (8 Items, e.g., “Registered nurses are involved in the internal governance of the hospital (e.g., practice and policy committees”)); (ii) Nursing
Foundations for Quality of Care (9 Items, e.g., “A clear philosophy of nursing that pervades the patient care environment”); (iii) Nurse Manager Ability, Leadership, and Support of Nurses (4 Items, e.g., “A nurse manager who backs up the nursing staff in decision making, even if the conflict is with a physician”); (iv) Staffing and Resource Adequacy (4 Items, e.g., “Enough registered nurses on staff to provide quality patient care”) and (v) Collegial Nurse-Physician Relations (7 Items, e.g., “Physicians respect nurses as professionals”). Using a 4-point Likert scale (ranging from “strongly disagree (1)” to “strongly agree (4)”), nurses were asked how they perceived specific elements of their workplace. Validity (e.g., construct validity) and reliability have been established for the original PES-NWI [23, 24] and several cross-cultural versions [39–41].
Switzerland has three national language regions and the original English measures, including the PES-NWI were translated into German, French and Italian using a systematic translation process including forward-backward translation and expert panel review with content validity indexing [42, 43].
In Switzerland, the nurse survey was conducted between October 2009 and June 2010. For each participating hospital a contact person (chief nursing officer or nursing expert) facilitated the planning and processing of the data collection. The questionnaires were distributed via the contact person, along with pre-stamped, pre-addressed envelopes, allowing nurses to return completed questionnaires directly to the research team. If response rates were below 70% after 2 weeks of data collection, reminders were sent. Completed questionnaires were scanned and data were subjected to quality control procedures, including verification and control for data entry errors in a random sample of 10% of the entered questionnaires.
Directors and chief nursing officers of the 35 Swiss hospitals provided written consent for participation in the study, anonymous benchmarking and dissemination of the results. Positive approval for the RN4CAST study was acquired from all 13 responsible ethical committees of the respective Cantons. Nurse participation was voluntary. To guarantee anonymity of individuals and confidentiality of data, questionnaires were coded. This allowed the research team to identify units and hospitals, but not individual respondents.
To describe the quality of the nurse work environment in Swiss acute care hospitals and to benchmark Swiss hospitals with Magnet and Non-Magnet hospitals we used descriptive statistics, including means, standard deviations, medians, inter-quartile ranges, frequencies, cross-tabulations and graphs (e.g., box plots) as appropriate. We computed one-way analysis of variance (ANOVA) to explore whether differences between the 35 Swiss hospitals (independent variable) of the five dimensions and the composite score of the PES-NWI (dependent variables) were statistically significant. All analyses on our Swiss data were computed by one author of this article (DA), independently from the international study centre.
First, we calculated mean scores for each PES-NWI subscale by aggregating nurse responses to the single items according to their affiliation to the five dimensions. The composite score of the PES-NWI was calculated as the mean of the subscale scores. To describe the quality of the work environment in Swiss hospitals and to benchmark its findings with results of international Magnet hospital research, we then aggregated nurse responses on PES-NWI subscales and composite scores at the hospital level. For each of the subscales, the potential mean scores ranged from 1 to 4, with the value of 2.5 considered a neutral midpoint (i.e., neither agreement nor disagreement). Values above 2.5 indicate agreement that the PES-NWI domains are present in the current job setting; values below 2.5 indicate disagreement [27]. In addition, we considered the three-level categorisation developed by Lake and Friese [4] to describe the quality of Swiss hospitals’ nurse work environments. Supported by criterion validity and latent class analysis, the quality of each hospital's nurse work environment can be classified as “unfavourable” (mean scores above 2.5 on no subscales or one subscale), “mixed” (mean scores above 2.5 on 2–3 subscales) or “favourable” (mean scores above 2.5 on 4–5 subscales). As this classification system is easier to interpret than the composite mean score, we computed the number of Swiss hospitals with unfavourable, mixed or favourable work environments.
Second, to compare the quality of the nurse work environment of Swiss hospitals with the international data from our literature review, we calculated weighted means for Magnet (i.e., hospitals with Magnet accreditation) and non-Magnet hospitals (i.e., hospitals neither having nor undergoing Magnet designation). For each PES-NWI subscale and the composite scores, means for Magnet and non-Magnet hospitals were weighted based on the nurse sample size of each study. The following formula was used:
Analyses were performed using IBM SPSS Statistics (version 19.0.1; IBM Inc., Armonk, NY, USA) and figures were plotted using Microsoft Office Excel 2008(R).
Our literature search identified 874 articles of potential interest. After checking for eligibility criteria and research aims we retained 72. Based on our inclusion criteria, we excluded 59 articles that covered ineligible hospital settings (e.g., ICU), did not report descriptive data, or failed to report data for each of the five studied sub-dimensions (fig. 1). Authors (MD, DA) decided to exclude one study reporting on the nurse work environment of a hospital in the Magnet recognition process (see fig. 1), based on our definition of Magnet-hospitals and Non-Magnet hospitals, since this data could not be clearly assigned to one of the two groups without the risk of bias. Finally, we retained 13 studies, the relevant information and data from which are summarised in table 1. Our literature research revealed frequent use (n = 33) of measures other than the PES-NWI to gauge the quality of the nurse work environment, including the revised version of the Nurse Work Index, the Collaborative Practice Scale, the Conditions of Work Effectiveness Questionnaire II and the Perceived Nurse Work Environment Instrument. Unfortunately, nine studies on the nurse work environment in European hospitals had to be excluded, as they used other measures than the PES-NWI (e.g., revised version of the Nurse Work Index/NWI-R), consisting of different numbers and content of subscales. The majority of the included studies were conducted in the United States (n = 9), 2 studies were from Canada and 2 from Australia. Of the 13 studies selected for analysis, 3 reported data from Magnet hospitals, and all reported on Non-Magnet hospitals. Sample sizes of nurses surveyed varied from very small (N = 46) to massive (N = 72,889) (table 1). Calculated weighted mean values for the subscales and composite scores regarding the nurse work environments in Magnet and Non-Magnet hospitals are summarised in table 2.
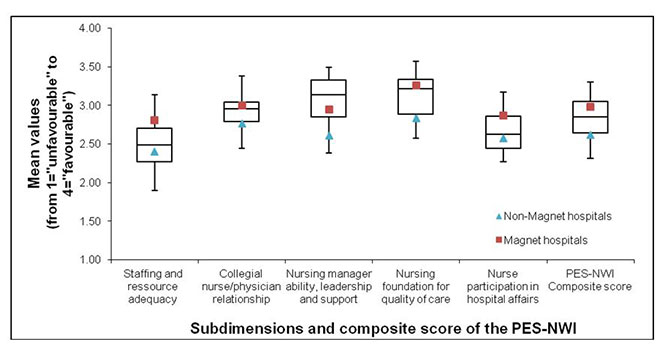
Figure 2
The quality of the nurse work environment in our sample (box plots), compared to work environments in Magnet and Non-Magnet hospitals
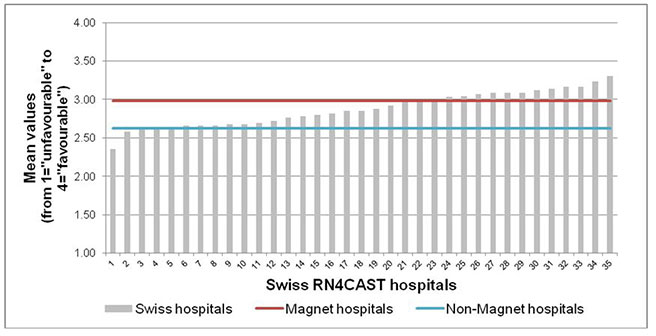
Figure 3
Variability in the quality of the nurse work environment (PES-NWI composite score) in our sample, compared to international data from Magnet and Non-Magnet hospitals
The Swiss arm of the RN4cast study included 35 hospitals, slightly more than half of which (n = 19, 54%) were part of hospital groups and had fewer than 200 acute care beds. Nearly all (n = 34, 97%) were state subsidised. Four (11%) university hospitals, 15 (43%) cantonal and 16 (46%) regional hospitals participated. A majority (57%) came from the German speaking part of Switzerland; the French- and Italian-speaking regions accounted for 31.5% and 11.5% respectively.
The response rate for RNs was 73% (n = 1,633; table 3). Furthermore, 44.8% of eligible respondents (n = 731) worked on 59 surgical wards, 48.4% (n = 789) on 61 medical wards, with the remaining 6.8% (n = 110) working on 12 mixed units. German-speaking nurses were predominant (65.9%). A total of 1,278 respondents were trained in Switzerland, corresponding to 78% of the total sample. The number of university-trained nurses (bachelor’s degree or higher) was 9.7%. Employment status showed equilibrium between full-time and part-time workers (n = 788, 48.5%). The mean age for our sample was 35.2; the mean length of experience was 11.09 years.
Overall, Swiss RNs appraise their work environment positively (see fig. 2). However, we observed statistical significant between-hospital variability for the composite mean score and the 5 dimensions (see table 2). The composite nurse work environment score (Mean 2.85 ± 0.23; Range 2.31–3.30) indicated RNs’ general agreement that subscale items are present in the current job setting. Considering the PES-NWI subscales, the “Nursing foundations for quality of care” subscale (Mean 3.12 ± 0.27; Range 2.57–3.57) had the highest mean score, followed by “Nursing Manager ability, leadership and support of nurses” (Mean 3.06 ± 0.31; Range 2.38–3.49), “Collegial nurse –physician relationships” (Mean 2.92 ± 0.20; Range 2.38–3.49), and “Nurse participation in hospital affairs “(Mean 2.65 ± 0.24; Range 2.27–3.17). The subscale “Nursing staffing and resources adequacy” (Mean 2.50 ± 0.32; Range 1.90–3.14) was rated lowest.
Across all hospitals, all subscales had mean values above the “favourable” threshold of 2.5, suggesting that the requisite features were present in the current work environment. Based on the three nurse work environment quality categorisations described above [4], 25 of the 35 sampled hospitals (71.4%) could be classified as favourable, 9 (25.7%) as mixed and only 1 (2.9%) as unfavourable. Nevertheless, for “Nurse participation in hospital affairs” and “Nursing staffing and resources adequacy”, a remarkable number of hospitals (14 (40%) and 18 (51.4%), respectively) scored below the “favourable” threshold of 2.5.
The mean scores for the PES-NWI subscales and the composite score for the Swiss Hospitals, compared to international data on the quality of the nurse work environment from Magnet and Non-Magnet hospitals, are shown in figure 2 and figure 3. On average, the Swiss mean scores for all subscales were superior to those reported in Non-Magnet hospitals. The composite score, as well as 4 of the 5 subscale scores – which place approximately 50% of the Swiss Hospitals between the 25th and 75th percentiles overall – fall between those of Magnet and Non-Magnet hospitals. At the upper end of the distribution, 25% of our sampled hospitals received average scores equal to or higher than those of Magnet hospitals (see fig. 2). The mean Swiss score for the subscale “Nursing manager ability” even exceeds the highest reported Magnet hospital score, suggesting that in almost 75% of our sample “Nursing manager ability” is perceived as higher than in Magnet hospitals. However, the Swiss scores for “Nurse participation in hospital affairs” and “Nursing staffing and resources adequacy” were clearly inferior, approaching the mean values of Non-Magnet hospitals. For the composite score we found that 14 out of 35 Swiss hospitals (40%) had higher quality of the nurse work environment than Magnet hospitals, and 5 Swiss hospitals (14%) scored equal or lower than Non-Magnet hospitals (see fig. 3).
| Table 1: Descriptive statistics on the quality of the nurse work environment on studies examining in Magnet and non-Magnet hospitals. | |||||||||||
| Author/s | Country | Hospital setting | Magnet status | Sample size | Subscale mean scores and standard deviations | ||||||
| Nurse participation in organisation affairs - | Nursing Foundation for Quality Care | Nurse manager ability, leadership and support | Staffing and resource adequacy | Collegial nurse / physician relations | Composite score | ||||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| 1 | Armstrong et al. (2009) | CA | Acute-care hospitals (medical-surgical units) | Non-Magnet | 153 nurses hospitals = N.S. | 2.36 (0.51) | 2.77 (0.4) | 2.48 (0.70) | 2.40 (0.57) | 2.93 (0.57) | 2.59 (0.42) |
| 2 | Eaton-Spiva et al. (2010) | USA | Not-for-profit, community-based hospital | Non-Magnet | 46 nurses 1 hospital | 2.76 (0.55) | 2.97 (0.50) | 3.21 (0.56) | 2.56 (0.65) | 2.54 (0.66) | 2.81 (0.50) |
| 3 | Friese (2005) | USA | Non-ANCC hospitals (surgical, nononcology) | Non-Magnet | 896 nurses hospitals = N.S. | 2.72 (N.S.) | 3.09 (N.S.) | 2.74 (N.S.) | 2.35 (N.S.) | 2.90 (N.S.) | 2.76 (N.S.) |
| USA | ANCC hospitals (surgical, nononcology) | Magnet | 755 nurses hospitals = N.S. | 2.98 (N.S.) | 3.35 (N.S.) | 2.93 (N.S.) | 2.77 (N.S.) | 2.99 (N.S.) | 3.00 (N.S.) | ||
| 4 | Friese et al. (2008) | USA | Acute-care hospitals (surgical units) | Non-Magnet | 25,957 nurses 164 hospitals | 2.33 (0.25) | 2.84 (0.20) | 2.38 (0.27) | 2.20 (0.29) | 2.75 (0.17) | 2.5 (N.S.) |
| 5 | Gajewski et al. (2010) | USA | Acute-care hospitals | Non-Magnet | 72,889 nurses 4783 units | 2.76 (N.S.) | 3.01 (N.S.) | 2.88 (N.S.) | 2.65 (N.S.) | 2.95 (N.S.) | 2.85 (N.S.) |
| 6 | Kim et al. (2009) | USA | Acute-care hospitals (geriatric units) | Non-Magnet | 192 nurses 3 hospitals | 2.03 (N.S.) | 2.04 (N.S.) | 1.96 (N.S.) | 2.63 (N.S.) | 2.07 (N.S.) | 2.15 (N.S.) |
| 7 | Lake (2002) | USA | ANCC hospitals | Magnet | 1610 nurses 16 hospitals | 2.76 (0.47) | 3.09 (0.39) | 3 (0.59) | 2.88 (0.62) | 2.99 (0.52) | 2.95 (0.40) |
| USA | Non-ANCC hospitals | Non-Magnet | 689 nurses 8 hospitals | 2.44 (0.44) | 2.83 (0.36) | 2.68 (0.60) | 2.49 (0.62) | 2.82 (0.55) | 2.65 (0.35) | ||
| 8 | Lake & Friese (2006) | USA | Non-ANCC hospitals (medical-surgical, adult intensive care, obstetrics-gynaecology) | Non-Magnet | 10,926 nurses 156 hospitals | 2.30 (0.23) | 2.81 (0.20) | 2.36 (0.24) | 2.18 (0.26) | 2.75 (0.16) | 2.48 (0.18) |
| USA | ANCC hospitals (medical-surgical units) | Magnet | 1,054 nurses 7 hospitals | 2.96 (0.18) | 3.32 (0.15) | 2.91 (0.14) | 2.77 (0.24) | 3.02 (0.12) | 2.99 (0.12) | ||
| 9 | Lucero et al. (2009) | USA | Acute-care hospitals | Non-Magnet | 10,184 nurses 168 hospitals | 2.30 (0.20) | 2.80 (0.20) | 2.40 (0.30) | 2.20 (0.10) | 2.80 (0.20) | 2.50 (N.S.) |
| 10 | Middleton et al. (2008) | AUS | General medical-surgical | Non-Magnet | 67 nurses 1 hospital | 2.71 (0.31) | 2.95 (0.32) | 2.94 (0.47) | 2.07 (0.56) | 2.81 (0.44) | 2.69 (0.36) |
| 11 | Parker et al. (2010) | AUS | Public sector | Non-Magnet | 330 nurses hospitals = N.S. | 2.48 (0.59) | 2.85 (0.50) | 2.61 (0.69) | 2.46 (0.69) | 2.86 (0.63) | 2.67 (0.48) |
| 12 | Patrician et al. (2010) | USA | Army hospitals | Non-Magnet | 955 nurses 23 hospitals | 2.52 (0.62) | 2.85 (0.54) | 2.57 (0.88) | 2.61 (0.74) | 2.99 (0.70) | 2.71 (0.56) |
| 13 | Spence Laschinger et al. (2006) | CA | Medical-surgical units | Non-Magnet | 8,597 nurses 292 hospitals | 2.38 (0.54) | 2.71 (0.49) | 2.46 (078) | 2.32 (0.69) | 2.82 (0.65) | 2.54 (N.S.) |
| N.S. = not stated; PES-NWI mean values: ranging from 1 = “unfavourable” to 4 = “favourable” | |||||||||||
| Table 2:Statistics on the PES-NWI subscale and composite scores from Swiss, Magnet and non Magnet hospitals. | |||||||
| Subscales | 35 Swiss hospitals (RNs = 1,633) | Magnet hospitals (3 studies) (RNs = 755–1,610) | Non Magnet hospitals (13 studies) (RNs = 46–72,889) | ||||
| Mean (SD) | Min‒max | F-statistics° | Mean (SD) | Min‒max | Mean (SD) | Min-Max | |
| Nurse participation in hospital affaires | 2.65 (0.26) | 2.27–3.17 | F(34,1593) = 10.99* | 2.87 (0.12) | 2.76–2.98 | 2.57 (0.22) | 2.03–2.76 |
| Nursing Foundation for Quality | 3.12 (0.27) | 2.57–3.57 | F(34,1594) = 19.96* | 3.26 (0.14) | 3.09–3.35 | 2.83 (0.25) | 2.04–3.09 |
| Nursing manager ability, leadership and support | 3.06 (0.31) | 2.38–3.49 | F(34,1594) = 13.12* | 2.95 (0.05) | 2.91–3.00 | 2.61 (0.31) | 1.96–3.21 |
| Staffing and resource adequacy | 2.50 (0.32) | 1.90–3.14 | F(34,1593) = 11.94* | 2.81 (0.06) | 2.77–2.88 | 2.40 (0.19) | 2.07–2.65 |
| Collegial nurse/physician relations | 2.92 (0.20) | 2.44–3.38 | F(34,1594) = 6.09* | 3.00 (0.02) | 2.99–3.02 | 2.76 (0.24) | 2.07–2.99 |
| Composite score | 2.85 (0.23) | 2.31–3.30 | F(34,1594) = 14.99* | 2.98 (0.03) | 2.95–3.00 | 2.62 (0.18) | 2.15–2.85 |
| PES-NWI mean values: ranging from 1 = “unfavourable” to 4 = “favourable”; °Results from one-way analysis of variance testing for statistically significant differences between the 35 Swiss hospitals; *P<0.001 | |||||||
| Table 3:Description of the Swiss RN4CAST nurse sample (N = 1,633) | |
| Variables | Swiss nurses (N = 1,633) |
| Age in years – mean (SD) | 35.20 (10.00) |
| Female – % (n) | 91.70 (1,466) |
| Employment status <90% | 48.5 |
| RN per language region | |
| German-speaking – n (%) | 1,074 (65.9) |
| French-speaking – n (%) | 401 (24.6) |
| Italian-speaking – n (%) | 155 (9.5) |
| RN per unit type | |
| Surgical units – n (%) | 731 (44.8) |
| Medical units – n (%) | 789 (48.4) |
| Mixed medical/surgical units (only German-speaking region) – n (%) | 110 (6.8) |
| Nurses with a Bachelor's Degree in nursing or higher – % (n) | 9.7 (151) |
| Nurses trained in Switzerland – n (%) | 1278 (78) |
| Length of experience in years – mean (SD) | 11.09 (9.50) |
| Length of employment years – mean (SD) | 8.07 (8.04) |
To our knowledge this is the first study describing nurse work environment quality across a large national sample of Swiss acute care hospitals and comparing findings with evidence from international Magnet research using standard assessment scores. Our study provides an initial insight regarding the extent to which Swiss acute care facilities support excellence in nursing practice and foster nurses’ ability to provide high quality of care inferred from the quality of their nurse work environment, a key characteristic of Magnet status. Overall, compared to Magnet hospitals abroad, Swiss hospitals perform excellently and show strong markers of supportive nurse work environments (i.e., those associated with superior patient and nurse outcomes) [3, 11–15].
For some of the 35 hospitals, the PES-NWI composite and sub-dimension scores were congruent with or superior to “Magnet nurse work environments”, while others fell significantly below the Magnet standards. Interestingly, the subscale “Nursing manager ability” in Swiss acute care exceeded the level of Magnet hospitals, suggesting positive management and leadership styles among nurse managers, recognition of achievements, and active support of nurses in conflict situations.
Such positive appraisals of the nurse leaders is a particularly significant finding, as leadership quality is known to impact nurse performance, empowerment, retention and satisfaction, and has even been associated with patient outcome indicators, such as 30-day mortality [16, 44–46]. However, the current Magnet model, refined in 2007, emphasises “transformational leadership” as one of its 5 key components. Transformational leadership identifies and communicates vision and values, which the work group is then encouraged to work towards [47]. Cummings et al. [48] linked this type of leadership with factors reflecting individual, team and organisational productivity and effectiveness.
Unfortunately, the PES-NWI’s leadership subscale does not explicitly cover all elements of transformational leadership. Baseline data from a quasi-experimental study investigating the impact of a clinical leadership programme in a small convenience sample of 14 nurse leaders revealed that some elements of transformational leadership, such as “inspiring a shared vision” are less present in Swiss hospital settings [49]. To investigate the extent to which elements of transformational leadership are present in a national sample of Swiss acute-care hospitals, further cross-sectional studies will be necessary as this is an aspect that emerges as highly relevant for a favourable nurse-work environment.
On average the Swiss scores on another sub-dimension of the PES-NWI, “Nursing staffing and resources adequacy”, were rated lowest, approaching Non-Magnet ratings. Initial international results from the RN4cast study revealed that, on average, the 12 participating European countries had a patient-to-RN ratio of 9.1:1 (SD = 1.7). Switzerland, with a patient-to-RN ratio of 7.9:1 (SD = 1.5) scored favourably, ranking in the middle of the 12 countries. The highest staffing levels were reported for Norway (Mean 5.4:1; SD = 1.0) and the lowest for Germany (Mean 13.0:1; SD = 2.3) [37]. Still, among our Swiss sample, a proportion of hospitals scored unfavourably regarding staffing levels. Nursing care can be regarded as a “surveillance system” within healthcare organisations [9, 10] with shortages either of nurses or of well-educated nurses having been associated with higher mortality and increased nurse-sensitive adverse events [10, 50, 51]. Thus, investments in adequate staffing contribute to patient safety and care quality; it is the duty of CEOs and CNOs to ensure adequate nurse staffing levels – which, not coincidentally, comprise an important element of favourable nurse work environments [52, 53].
Our results on the Swiss PES-NWI subscale score “Nurse participation in hospital affairs” showed that Swiss RNs are currently afforded only limited involvement in hospital policy and decision-making or see few opportunities to serve on hospital and nurse committees, but that they might reasonably expect more. Engaging nurses in hospital affairs and reviews of organisational performance has been shown to improve efficiency and effectiveness significantly at the unit level [54, 55]. In recently published reports, the Institute of Medicine (USA) and the Prime Minister’s Commission on the Future of Nursing and Midwifery (UK) recognised that involving nursing staff in policy and decision making is essential for current and future healthcare challenges [1, 56]. In view of implementing and evaluating innovative solutions and care models to meet the needs of an ageing population, managing chronic illness, restructuring care facilities and improving patient outcomes, empowering nursing staff and integrating their voices in multiple levels of decision-making is crucial in all countries, including Switzerland [57].
Favourable work environments can change quickly; creating and sustaining them requires on-going structural and cultural transformation and constant nurturing [47]. Globally, the current financial and human resources challenges in healthcare are raising fear among healthcare professionals, including nurses. In Switzerland, for example, the recent introduction of SwissDRGs (Diagnosis-Related Groups) threatens to increase patient-to-nurse ratios at the expense of care quality and patient safety. Based on lessons learned from the implementation of DRGs in Germany [58], such visionless cost-cutting – instead of system interventions – can quickly deteriorate the quality of the nurse work environment, which is a key system factor in optimising patient-, nurse- and cost-related outcomes [59].
Given the need to assess the impact of SwissDRG-style “natural experiments” in healthcare, in addition to monitoring patient outcomes, it might be useful to track system factors related to nursing care, such as the nurse work environment. Current national benchmarking strategies in Swiss acute care settings focus only on nurse-sensitive outcomes (e.g., patient falls, pressure ulcers). While important – and novel – those national quality measures are insufficient to capture the full picture of nursing care quality. Nurse-sensitive measures must also include data on organisational structures and processes related to patient safety and the quality of nursing care. For example, the National Database of Nursing Quality Indicators® (NDNQI®) – a US national registry dedicated to nurse sensitive-measures at the unit level [60] – might inspire Swiss healthcare policy makers to continuously collect national data on structural (e.g., the quality of the nurse work environment) and process-related indicators (e.g., implicit rationing of nursing care) [61–63].
Several precautions should be considered regarding this study’s results. First, although we carried out a structured literature review following the PRISMA guideline [64], this was not a systematic literature review. Given our second research aim, we focused on descriptive PES-NWI data only, and not on effect sizes, to compute meta-analyses for example. Therefore, our review cannot fulfil all quality criteria of systematic reviews [64]. Second, although the RN4cast study included a national sample of Swiss hospitals, it did not use randomised sampling techniques in all stages of the sampling process and included only acute-care hospitals with 60 or more beds to achieve a sample size of at least 50 RNs per hospital. Therefore, regional hospitals were relatively under-represented. Third, the current study used survey data from RNs working on general medical, surgical and mixed medical-surgical units, and used aggregated data as a proxy measure for hospitals’ nurse work environments. Although the tested units represent the largest clinical group within acute-care hospitals, the generalisability and transferability of our findings to other acute-care settings (e.g., ICU’s, emergency departments or psychiatric clinics) should be considered with caution. Fourth, the conception and deployment of the PES-NWI originates in research on “Magnet hospitals” conducted in the 1980s. Although the PES-NWI reflects important elements of the nurse work environment in Magnet hospitals, it does not cover all components of the updated Magnet Model [65], regarding transformational leadership for example. Thus, it might be necessary to evaluate the new Magnet Model, to update existing theories on the quality of the nurse work environment in Magnet hospitals using qualitative research methods, and to revise the PES-NWI accordingly. Finally, based on previous studies on the quality of nurses’ work environment in European hospital settings [31–34], the assumption underlying this study was that elements of favourable nurse work environment, such as the case in Magnet hospitals, have the same cross-cultural meaning in European and Swiss hospitals. It is a major limitation of this study that it is unclear to what extent the Magnet concept as a whole is directly transferable to Swiss and other European healthcare settings. Although we benchmark results on the nurse work environment from Swiss hospitals against published results from international Magnet hospital research, it was not our intention to designate Swiss hospitals with Magnet status or not. Although, Swiss hospitals appeared in a favourable light compared to accredited “Magnet hospitals”, these results need to be interpreted with caution due to the potential cross-cultural differences in meaning of the nurse work environment between Switzerland and English-speaking countries, such as USA, Canada or Australia. Further analysis and comparison of the international RN4Cast data will help to better understand the quality of Swiss hospital work environments in the context of European hospital settings.
On average, Swiss nurses appraise their work environments positively: the majority of the 35 Swiss hospitals included in this study received work environment ratings comparable to those of Magnet hospitals. Swiss RNs in acute care are therefore well-positioned to improve patient outcomes, both by delivering high care quality and by contributing to new and innovative models of care. However, we found statistically significant variability regarding the quality of nurse work environment. RNs expressed unmet expectations regarding participation in hospital affairs and staffing and resources adequacy. For hospitals with mixed and unfavourable work environment ratings, the Magnet concept offers an approach to develop and sustain favourable nurse work environments.
In order to reduce the variability in Swiss hospitals’ nurse work environments and to facilitate learning from the best, national monitoring and benchmarking on nurse work environment quality and other important nurse-sensitive indicators related to patient safety and quality of care might be useful. It can permit follow-ups over time and gauge the impact of on-going economic incentives such as the implementation of Swiss DRGs. Further research is needed to explore (1.) which organisational assets facilitate high quality in Swiss hospitals’ nurse work environments, (2.) to what extent elements of transformational leadership are present in Swiss acute-care hospitals, and (3.) how the quality of the nurse work environments in Swiss hospitals (e.g., staffing levels) are related to nurse and patient outcomes.
1 Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. Washington D.C.: The National Academies Press; 2010.
2 Aiken LH, Poghosyan L. Evaluation of “magnet journey to nursing excellence program” in Russia and Armenia. J Nurs Scholarsh. 2009;41(2):166–74.
3 Kelly LA, McHugh MD, Aiken LH. Nurse Outcomes in Magnet¬Æ and Non-Magnet Hospitals. J Nurs Adm. 2011;41(10):428–33 10.1097/NNA.0b013e31822eddbc.
4 Lake ET, Friese CR. Variations in nursing practice environments: relation to staffing and hospital characteristics. Nurs Res. 2006;55(1):1–9.
5 Cowden T, Cummings G, Profetto-McGrath J. Leadership practices and staff nurses’ intent to stay: a systematic review. J Nurs Manag. 2011;19(4):461–77.
6 Flinkman M, Leino-Kilpi H, Salantera S. Nurses’ intention to leave the profession: integrative review. J Adv Nurs. 2010;66(7):1422–34.
7 Stone PW, Hughes R, Dailey M. Creating a safe and high-quality health care environment patient safety and quality: an evidence-based handbook for furses. Hughes RG, editor. Rockville MD2008.
8 Shermont H, Krepcio D. The impact of culture change on nurse retention. J Nurs Adm. 2006;36(9):407–15.
9 Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037–45.
10 Blegen MA, Goode CJ, Spetz J, Vaughn T, Park SH. Nurse staffing effects on patient outcomes: safety-net and non-safety-net hospitals. Med Care. 2011;49(4):406–14.
11 Lucero RJ, Lake ET, Aiken LH. Nursing care quality and adverse events in US hospitals. J Clin Nurs. 2010;19(15-16):2185–95.
12 Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93.
13 Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290(12):1617–23.
14 Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38(5):223–9.
15 Spence Laschinger HK, Leiter MP. The impact of nursing work environments on patient safety outcomes: the mediating role of burnout/engagement. J Nurs Adm. 2006;36(5):259–67.
16 Cummings GG, Midodzi WK, Wong CA, Estabrooks CA. The contribution of hospital nursing leadership styles to 30-day patient mortality. Nurs Res. 2010;59(5):331–9.
17 Dewing J. Implications for nursing managers from a systematic review of practice development. J Nurs Manag. 2008;16(2):134–40.
18 McGillis Hall L, Peterson J, Baker GR, Brown AD, Pink GH, McKillop I, et al. Nurse staffing and system integration and change indicators in acute care hospitals: evidence from a balanced scorecard. J Nurs Care Qua. 2008;23(3):242–52.
19 Lundmark VA. Magnet environments for professional nursing practice patient safety and quality: an evidence-based handbook for nurses. Hughes RG, editor. Rockville MD2008.
20 Newhouse RP. Examining the support for evidence-based nursing practice. J Nurs Adm. 2006;36(7-8):337–40.
21 Kramer M, Maguire P, Brewer BB. Clinical nurses in Magnet hospitals confirm productive, healthy unit work environments. J Nurs Manag. 2011;19(1):5–17.
22 Tschannen D, Kalisch BJ. The impact of nurse/physician collaboration on patient length of stay. J Nurs Manag. 2009;17(7):796–803.
23 Gajewski BJ, Boyle DK, Miller PA, Oberhelman F, Dunton N. A multilevel confirmatory factor analysis of the Practice Environment Scale: a case study. Nurs Res. 2010;59(2):147–53.
24 Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–88.
25 Aiken LH, Patrician PA. Measuring organizational traits of hospitals: the Revised Nursing Work Index. Nurs Res. 2000;49(3):146–53.
26 Warshawsky NE, Havens DS. Global use of the Practice Environment Scale of the Nursing Work Index. Nurs Res. 2011;60(1):17–31.
27 Middleton S, Griffiths R, Fernandez R, Smith B. Nursing practice environment: how does one Australian hospital compare with magnet hospitals? Int J Nurs Pract. 2008;14(5):366–72.
28 Kim H, Capezuti E, Boltz M, Fairchild S. The nursing practice environment and nurse-perceived quality of geriatric care in hospitals. West J Nurs Res. 2009;31(4):480–95.
29 Chen YM, Johantgen ME. Magnet hospital attributes in European hospitals: a multilevel model of job satisfaction. Int J Nurs Stud. 2010;47(8):1001–12.
30 Aiken LH, Buchan J, Ball J, Rafferty AM. Transformative impact of Magnet designation: England case study. J Clin Nurs. 2008;17(24):3330–7.
31 Gunnarsdottir S, Clarke SP, Rafferty AM, Nutbeam D. Front-line management, staffing and nurse-doctor relationships as predictors of nurse and patient outcomes. a survey of Icelandic hospital nurses. Int J Nurs Stud. 2009;46(7):920–7.
32 Van Bogaert P, Meulemans H, Clarke S, Vermeyen K, Van de Heyning P. Hospital nurse practice environment, burnout, job outcomes and quality of care: test of a structural equation model. J Adv Nurs. 2009;65(10):2175–85.
33 Van Bogaert P, Clarke S, Roelant E, Meulemans H, Van de Heyning P. Impacts of unit-level nurse practice environment and burnout on nurse-reported outcomes: a multilevel modelling approach. J Clin Nurs. 2010;19(11-12):1664–74.
34 Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, et al. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int J Nurs Stud. 2007;44(2):175–82.
35 Sanderson S, Tatt ID, Higgins JP. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. 2007;36(3):666–76.
36 von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
37 Aiken LH, Sermeus W, Heede KVd, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012 2012-03-20 00:00:00;344.
38 Sermeus W, Aiken LH, Van den Heede K, Rafferty AM, Griffiths P, Moreno-Casbas MT, et al. Nurse Forecasting in Europe (RN4CAST): Rationale, design and methodology. BMC Nurs. 2011;10(1):6.
39 De Pedro-Gomez J, Morales-Asencio JM, Sese-Abad A, Bennasar-Veny M, Pericas-Beltran J, Miguelez-Chamorro A. Psychometric testing of the Spanish version of the Practice Environment Scale of the Nursing Work Index in a primary healthcare context. J Adv Nurs. 2011 Jun 29.
40 Liou S, Cheng C. Using the Practice Environment Scale of the Nursing Work Index on Asian nurses. Nurs Res. 2009;58(3):218–25.
41 Parker D, Tuckett A, Eley R, Hegney D. Construct validity and reliability of the Practice Environment Scale of the Nursing Work Index for Queensland nurses. Int J Nurs Pract. 2010;16(4):352–8.
42 Jones PS, Lee JW, Phillips LR, Zhang XE, Jaceldo KB. An adaptation of Brislin’s translation model for cross-cultural research. Nurs Res. 2001;50(5):300–4.
43 Squires A, Aiken LH, van den Heede K, Sermeus W, Bruyneel L, Lindqvist R, et al. A systematic survey instrument translation process for multi-country, comparative health workforce studies. Int J Nurs Stud. 2012 Mar 23.
44 Lee H, Cummings GG. Factors influencing job satisfaction of front line nurse managers: a systematic review. J Nurs Manag. 2008;16(7):768–83.
45 Brady Germain P, Cummings GG. The influence of nursing leadership on nurse performance: a systematic literature review. J Nurs Manag. 2010;18(4):425–39.
46 Wong CA, Cummings GG. The relationship between nursing leadership and patient outcomes: a systematic review. J Nurs Manag. 2007;15(5):508–21.
47 Center ANC. Magnet Recognition Program: Application Manual. 2008.
48 Cummings GG, MacGregor T, Davey M, Lee H, Wong CA, Lo E, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2010;47(3):363–85.
49 Martin JS, McCormack B, Fitzsimons D, Spirig R. Evaluation of a clinical leadership programme for nurse leaders. J Nurs Manag. 2012;20(1):72–80.
50 Patrician PA, Loan L, McCarthy M, Fridman M, Donaldson N, Bingham M, et al. The association of shift-level nurse staffing with adverse patient events. J Nurs Adm. 2011;41(2):64–70.
51 Kane RL, Shamliyan T, Mueller C, Duval S, Wilt TJ. Nurse staffing and quality of patient care. Evid Rep Technol Assess (Full Rep). 2007;(151):1–115.
52 Rothberg MB, Abraham I, Lindenauer PK, Rose DN. Improving nurse-to-patient staffing ratios as a cost-effective safety intervention. Med Care. 2005;43(8):785–91.
53 Van den Heede K, Simoens S, Diya L, Lesaffre E, Vleugels A, Sermeus W. Increasing nurse staffing levels in Belgian cardiac surgery centres: a cost-effective patient safety intervention? J Adv Nurs. 2010;66(6):1291–6.
54 Havens DS, Johnston MA. Achieving Magnet hospital recognition: chief nurse executives and Magnet coordinators tell their stories. J Nurs Adm. 2004;34(12):579–88.
55 Drenkard K. The business case for Magnet. J Nurs Adm. 2010;40(6):263–71.
56 Nursing PMsCotFo. Front line care: the future of nursing and midwifery in England. Report of the Prime Minister’s Commission on the future of nursing and midwifery in England 2010.2010: Available from: http://webarchive.nationalarchives.gov.uk/20100331110400/http://cnm.independent.gov.uk/wp-content/uploads/2010/03/front_line_care.pdf.
57 Imhof L, Rüesch P, Schaffert R, Mahrer-Imhof R, Fringer A, Kerker-Specker C. Professionelle Pflege Schweiz: Perspektive 2020. Ein Grundlagenbericht.2010: Available from: http://www.sbk-asi.ch/pflege2020/201012_Lit_Perspektiven_2020_D.pdf.
58 Simon M. Stellenabbau im Pflegedienst der Krankenhäuser. Eine Analyse der Entwicklung zwischen 1991 und 2005.2007: Available from: http://www.fakultaet5.fh-hannover.de/fileadmin/media/doc/f5/papers/07-001.pdf.
59 Weinberg DB. Code green: money-driven hospitals and the dismantling of nursing: ILR Press; 2003.
60 Montalvo I. The National Database of Nursing Quality IndicatorsTM (NDNQI®). The Online Journal of Issues in Nursing [serial on the Internet]. 2007; 12(3): Available from: http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume122007/No3Sept07/NursingQualityIndicators.aspx.
61 Schubert M, Clarke SP, Aiken LH, de Geest S. Associations between rationing of nursing care and inpatient mortality in Swiss hospitals. Int J Qual Health Care. 2012 Mar 28.
62 Schubert M, Clarke SP, Glass TR, Schaffert-Witvliet B, De Geest S. Identifying thresholds for relationships between impacts of rationing of nursing care and nurse- and patient-reported outcomes in Swiss hospitals: a correlational study. Int J Nurs Stud. 2009;46(7):884–93.
63 Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care. 2008;20(4):227–37.
64 Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34.
65 American Nurses Credentialing Center. Magnet Recognition Program: application manual: American Nurses Credentialing Center; 2008.
Funding / potential competing interests: None of the authors has a conflict of interest regarding this sub-study. The research leading to these results has received funding from the European Union’s Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 223468.