
Figure 1
Distribution of number of antihypertensive agents per patient. Total population n = 122. The majority of patients received a monotherapy.
DOI: https://doi.org/10.4414/smw.2012.13693
Data on patients with arterial hypertension (AH) from the US and Europe show insufficient blood pressure (BP) control, even though effective antihypertensive treatments as well as guideline recommendations are available [1]. Considering that AH is the most prevalent cardiovascular risk factor worldwide [2] and that even mild AH is associated with increased risk of cardiovascular morbidity and mortality [3, 4], it is important to emphasise the need for strict BP control [5] and to get deeper insight into factors that hinder its achievement.
Most of the international data on BP control originate from national surveys, population based studies or secondary care, despite the fact that the majority of patients are treated in a primary care (PC) setting. Data on patients with uncontrolled AH in PC in Switzerland are limited and vary, reporting AH control rates among patients with pharmacotherapy between 12.5% to 50% [6, 7]. Even the studies performed in the PC setting of countries in which the general practitioner (GP) holds a strong gate-keeping function [8, 9] are often restricted to certain ages or to already existing antihypertensive medications. Since the gate-keeping system in Switzerland is not generally established and is limited to certain insurance models which are currently chosen by the minority of the population, direct knowledge transfer is limited.
Therefore, the objective of this study is to investigate the characteristics of patients with insufficiently controlled BP in Swiss PC and to assess factors associated with uncontrolled BP.
Data originated from baseline data of the on-going pragmatic “CoCo”-Trial: Colour-coded Blood Pressure Control (Trial Registration Number: NCT01013467) [10] that investigates the effect of a colour coded BP monitoring on adherence and BP control. GPs were recruited via direct emailing, announcing the study in a Swiss PC journal and by information events. Patients were recruited by their participating GP.
– BP >140 mm Hg systolic and/or >90 mm Hg diastolic in the practice measurement (two consecutive measurements carried out in the practice, measured by the GP or practice assistant at the start of the study. Both measurements must meet the inclusion criteria with the second measurement qualifying for inclusion). 140 mm Hg systolic and/or 90 mmHg diastolic was chosen as cut-off according to current Swiss guidelines for the treatment of AH [11]
– No change in AH medication within the last month
– Patient able to perform self-monitoring
– Written informed consent
– Insufficient knowledge of the German language for instruction and BP recording with a booklet
– BP above 180 mm Hg systolic and/or 110 mm Hg diastolic (due to safety/risk considerations)
– Serious general or psychological illness (malignant tumours, serious depressive episodes or evidence of dementia)
GPs asked all consecutively appearing patients with known AH and fitting inclusion criteria for consent to participate in the study. Also patients without known diagnoses of AH who underwent routine BP measurement at the practice where asked for consent to participate in the study if the practice measurement was >140 mm Hg systolic or >90 mm Hg diastolic and no exclusion criteria existed. The inclusion and exclusion criteria were low threshold in order to reflect real life situation. Inclusion began in October 2009 and ended in March 2011.
In accordance with guidelines [12, 13] two consecutive oscillometric BP readings were performed in seated position after a resting period of at least 5 minutes. The physicians all used the same validated BP measuring devices (Mio-Star Cardioplus 500) which were provided by the Institute of General Practice and Health Services Research. GPs were instructed to choose appropriate cuffs according to the upper-arm circumference of the patients.
Additional socio-demographic and clinical information (age, weight, height, smoking habits, years of education [starting in primary school], previous home-BP-measurement [HBPM]) were collected. Antihypertensive medication was classified as follows: Angiotensin receptor blockers (ARB), Calcium channel blockers (CCB), Beta-blockers (BB), Angiotensin converting enzyme inhibitors (ACEI), diuretics and other antihypertensive drugs.
The anonymous data forms were faxed to the project leaders and data was entered by an independent employee. All patients gave written informed consent.
The study protocol was approved by the ethics committee of Zurich (Kantonale Ethikkommission (KEK) Zürich (EK-1738).
Continuous variables were tested for normal distribution by the Shapiro-Wilk test and presented accordingly as median and interquartile range (IQR) or as mean and standard deviation (SD), categorical data are presented as frequencies. We compared patient and GP characteristics using non parametric (wilcoxon rank sum) and parametric (unpaired t-test) tests, depending on normal distribution tests. Univariate linear regression analyses were performed to investigate the relationship between systolic and diastolic BP and all available patient characteristics. To investigate the independent association between BP measures and patient characteristics, multiple linear regression was applied. For the multiple linear regression models the same patient characteristics were considered as for the univariate analyses, irrespective of the significance levels based on the univariate analysis. The possibility of a non-linear relationship between BP measurements and the number of antihypertensive agents was taken into account by introducing a quadratic term of the predictor variable into the model. The purpose of introducing the quadratic term was to investigate the possibility of diminishing efficacy of multiple combination therapy on BP control. Goodness of fit (R2) was compared between models (i.e. linear- and non-linear modelling) by F-tests. We further used multilevel regression analysis with the GP as cluster level thus taking into account that patient observations are not independent, i.e. observations in one cluster tend to be more similar to each other than to individuals in the rest of the sample. The amount of clustering (i.e., the variation that is explained by the GP level) was assessed by calculating the intraclass correlation coefficient (ICC) ranging from 0% (i.e., no evidence for clustering) to 100% (i.e., all the variation in BP difference is explained on GP level). A two-sided alpha of 0.05 was set as level of significance for all comparisons.
All analyses were calculated using the STATA statistical package, version 11.2 (Stata Incorporation, College Station, TX, USA).
Between end of October 2009 and March 2011, 122 patients were included in the study.

Figure 1
Distribution of number of antihypertensive agents per patient. Total population n = 122. The majority of patients received a monotherapy.
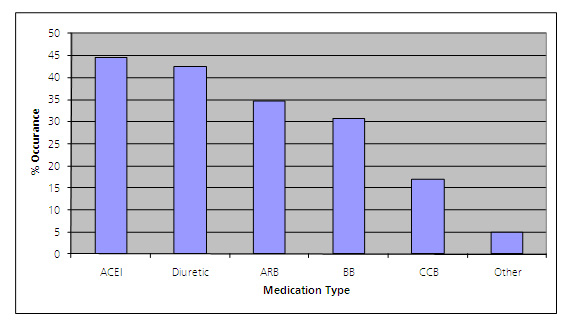
Figure 2
Overall distribution of antihypertensive agents. Other refers to imidazolin receptor antagonist (= moxonidin; causes blood pressure lowering by central adrenergic stimuli with resulting reduction in peripheral vascular resistance). ACEI and diuretics were the overall most commonly prescribed antihypertensive substances.
BB = beta blockers; CCB = calcium channel blockers; ARB = angiotensin receptor blockers; ACEI = angiotensin converting enzyme inhibitors.
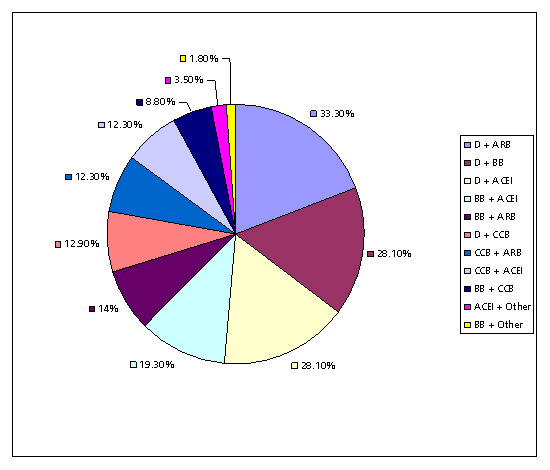
Figure 3
Distribution of antihypertensive dual drug combinations. Composition of dual combination therapies used in the study population (n = 57 with 2 or more antihypertensive drugs). Other refers to imidazolin receptor antagonist. The most commonly prescribed dual drug combination was diuretics with angiotensin receptor blockers.
D = diuretics; BB = beta blockers; CCB = calcium channel blockers; ARB = angiotensin receptor blockers; ACEI = angiotensin converting enzyme inhibitors.
Data on 122 adult patients with uncontrolled AH (above 140 mm Hg systolic and/or 90 mm Hg diastolic) [11] was collected. In table 1 the detailed study population characteristics can be appreciated. 43.8% of the patients were overweight (BMI between 25 and 30 kg/m2), 34.7% were obese (BMI 30 kg/m2 and more), median BMI was 28.3 kg/m2 (IQR 25.3–31.7). Slightly greater than half (52.1%) of patients were persistent (21.5%) or ex-smokers (30.6%). The mean systolic and diastolic BP was 157 and 92 mm Hg (SD 15.3 and 9.7). The majority performed HBPM at the time of inclusion into the study (65.6%). 60.0% of patients met inclusion criteria for both systolic and diastolic BP, 36.7% only for systolic and 3.3% only for diastolic BP. Data on patients receiving and not receiving pharmacological AH treatment were pooled for all further analyses since at the time of inclusion into the study besides diastolic BP no difference in patient characteristics (e.g., HBPM, gender, age, BMI, education pulse rate, smoking status and systolic BP) existed.
88.5% of the patients received antihypertensive treatment, in 41.8% a mono-therapy, followed by a dual therapy (30.3%). 16.4% received three or more antihypertensive agents. In total, 46.7% of patients with uncontrolled AH received 2 or more antihypertensive agents (fig. 1).
The overall most commonly prescribed antihypertensive agents were ACEI (44.6%), followed by diuretics (42.6%) and ARB (34.7%), BB (30.7%) and CCB (16.8 %) (fig. 2). ACEI were the most commonly prescribed monotherapy (39.2%), followed by ARB (29.4%), BB (17.7%), diuretics (9.8%) and CCB (6.9%).
The most established dual drug combinations were diuretic + ARB (33.3%), followed by diuretic + ACEI, as well as diuretic + BB (both 28.1%) (fig. 3).
The univariate regression analyses of patient characteristics influencing systolic and diastolic BP are presented in table 2. Smoking status (former and current compared to never smokers) was significantly and positively associated with systolic BP, whereas BMI only showed a trend for positive association (p = 0.071). The number of antihypertensive agents showed no linear relationship with systolic BP. However, taking into account a non-linear association (i.e., including a quadratic term) revealed a significant association between systolic BP and number of antihypertensive agents. Amount of antihypertensive agents (linear as well as non-linear term) and age were significantly associated with lower diastolic BP, whereas BMI and pulse rate were positively associated with diastolic BP.
The multivariate analyses for patient characteristics influencing systolic and diastolic BP are presented in table 3. Smoking status (current compared to never smokers), BMI and age were independently and positively associated with higher systolic BP. There was a significant and independent negative association between systolic BP and number of antihypertensive agents. The non-linear (quadratic) term of the number of AH agents was significantly and positively associated with systolic BP, suggesting a decrease of the incremental efficacy of additional antihypertensive substances in lowering systolic BP. Age and the number of antihypertensive substances were independently and negatively associated with diastolic BP. Goodness of fit for the multivariate model (R2) was significantly increased when a non-linear association between systolic BP and number of BP medications was taken into account, resulting in R2 values of 21.6% (linear model) and 30.0% (non-linear model), respectively (p = 0.01 for comparison). For diastolic BP the non-linear model did not result in an increased goodness of fit in the multivariate model. Corresponding R2values for linear and non-linear model were 31.7% and 33.7% (p = 0.10 for comparison). The main findings of the multivariate analyses concerning independent associations between patient characteristics and BP were not changed when additionally controlled for the GP as potential cluster effect: In a multilevel regression analysis no clustering effect of GPs on systolic (ICC = 0.04%, p = 0.998) and diastolic (ICC = 10.50%, p = 0.237) BP could be found. The mean number of patients included by GPs in to the study was 4.06 (range 1–8).
30 GPs from three German speaking cantons, mainly urban (n = 10) and suburban (n = 13) areas of Switzerland (rural n = 7) participated in the study. Significantly more GPs were male (73.3% vs 26.7 %, p <0.05). Thirteen GPs worked in single handed and 17 in group practices. They were all either specialised in internal (n = 15) or general medicine (n = 15). The female participants were significantly younger (median 50 vs 58.5 years, IQR 40–51 vs 48–62, p <0.05) and worked a significantly shorter period of time in the practice (median 2 vs 26, IQR 1–17 vs 3–27, p <0.05), even though the time since completion of the board examination was comparable between the genders (overall mean 28 years). Male and female GPs worked mainly full time, female GPs were more likely to use electronic patient records (EPR) (71.4% vs 23.8%, p <0.05). EPRs have been implemented in practice routine, on average, for 3.5 years (IQR 1–6 years).
| Table 1: Patient characteristics. | |
| Age (years) | 64 (54.8–72.0) |
| Male (%) | 50 |
| BMI (kg/m2) Normal (BMI 18.5–25 kg/m2), (%) Overweight (BMI 25–30 kg/m2), (%) Obese (BMI >30 kg/m2), (%) | 28.3 (25.3–31.7) 21.5 43.8 34.7 |
| Smoking status (%) Never smoked Stopped smoking Still smoking | 47.9 30.6 21.5 |
| Education (years) | 10.0 (8.25–14.0) |
| Previous home BP-measurement (%) | 65.6 |
| Antihypertensive treatment (%) | 82.8 |
| Systolic BP (mm Hg) | 157.3 (15.3) |
| Diastolic BP (mm Hg) | 91.9 (9.7) |
| Pulse rate (per minute) | 75.0 (11.1) |
| Continuous variables are presented as median (IQR) or mean (SD). | |
| Table 2: Patient characteristics and univariate influence on systolic and diastolic blood pressure. | ||||
| Characteristics | Univariate analysis systolic BP | Univariate analysis diastolic BP | ||
| Regression coefficient | 95% CI | Regression coefficient | 95% CI | |
| Home-BP-measurement (ref = no) | 0.54 | –5.83 to 6.92 | –2.13 | –6.12 to 1.86 |
| Gender (ref = male) | –2.98 | –8.89 to 2.92 | –1.14 | –4.88 to 2.58 |
| Linear Number of antihypertensive agents | 0.53 | –2.53 to 3.59 | –3.51 | –5.36 to –1.67* |
| Nonlinear Number of antihypertensive agents linear term Quadratic Term Number of antihypertensive agents | –12.48 4.10 | –22.56 to –2.39* 1.06 to 7.14* | –9.43 1.86 | –15.57 to –3.28* 0.01 to 3.71* |
| Age (years) | 0.13 | –0.10 to 0.36 | –0.33 | –0.46 to –0.20* |
| BMI (kg/m2) | 0.55 | –0.05 to 1.15 | 0.45 | 0.08 to 0.82* |
| Education (years) | –0.57 | –1.26 to 0.13 | –0.21 | –0.65 to 0.22 |
| Ex-smoker (ref = non-smoker) | 8.62 | 1.93 to 15.30* | –0.81 | –5.20 to 3.57 |
| Current smoker (ref = non-smoker) | 9.46 | 2.24 to 16.67* | 1.79 | –2.95 to 6.53 |
| Pulse rate (counts/min) | –0.12 | –0.38 to 0.13 | 0.16 | 0.00 to 0.31* |
| *p <0.05 | ||||
| Table 3: Patient characteristics and multivariate influence on systolic and diastolic blood pressure. | ||||
| Characteristics | Multivariate analysis systolic BP | Multivariate analysis diastolic BP | ||
| Regression coefficient | 95% CI | Regression coefficient | 95% CI | |
| Home-BP-measurement (ref = no) | –0.37 | –6.67 to 5.92 | 2.58 | –1.2 to 6.44 |
| Gender (ref = male) | –2.56 | –8.19 to 3.06 | –1.62 | –5.07 to 1.83 |
| Number of antihypertensive agents | –15.58 | –25.48 to –5.68* | –7.97 | –14.04 to –1.90* |
| Quadratic term Number of antihypertensive agents | 4.92 | 1.98 to 7.86* | 1.51 | –0.29 to 3.32 |
| Age (years) | 0.37 | 0.13 to 0.61* | –0.25 | –0.40 to –0.10* |
| BMI (kg/m2) | 0.78 | 0.18 to 1.38* | 0.11 | –0.25 to 0.47 |
| Education (years) | –0.41 | –1.06 to 0.24 | –0.30 | –0.70 to 0.10 |
| Ex-smoker (ref = non-smoker) | 6.03 | –0.52 to 12.58 | –2.27 | –6.28 to 1.75 |
| Current smoker (ref = non-smoker) | 13.17 | 6.10 to 20.19* | –0.82 | –5.12 to 3.47 |
| Pulse rate (counts/min) | –0.09 | –0.33 to 0.15 | 0.08 | –0.07 to 0.22 |
| *p <0.05 | ||||
Our study in patients with uncontrolled AH in Swiss PC showed that in this real life setting about 40% of patients were under single pharmacological treatment. We further found a non-linear (quadratic) relationship between the number of antihypertensive agents and systolic BP. Age, overweight and smoking resulted as predominant factors associated with the level of systolic BP in patients having insufficient BP control.
Although with these data and study design we cannot postulate a causal relation, a relation between BMI and smoking and insufficient BP control is to be presumed. In the literature elevated BMI and older age are known factors associated with high systolic BP [4, 14–16] and weight reduction has shown to significantly reduce systolic BP [17]. Our data are in line with these findings, where BMI and age were independent positive predictors for systolic BP when controlled for gender, HBPM, treatment and education. The observed inverse correlation between diastolic BP and age is a known phenomenon explained by the diminished elastic capacity of the large arteries with increasing age, leading to reduced distension during the systole and consequently lower diastolic BP [15, 18–20].
In our study smoking seemed to have the most significant effect on systolic BP with one third of the patients being former smokers and a fifth still active smokers. We did not find an association between diastolic BP and smoking, a finding which is in congruence with other epidemiological data in the literature [21]. However, interventional and epidemiological data on the effect of smoking cessation on BP have shown conflicting results [22].
Our conclusions on factors influencing BP control drawn from a study population only consisting of patients with uncontrolled AH seem justified when considering the results of a recent Swiss study also including patients with controlled AH (<140/90 mm Hg) [23]; there the BP control rate was higher in non-smokers and in patients with a BMI <25 kg/m2.
In our study population most patients performed HBPM before inclusion into the study and diastolic BP was linearly negatively associated with the amount of antihypertensive substances, suggesting good adherence with therapy.
It is known, that the efficacy of antihypertensive treatment proven in clinical trials is not always reflected in the real life of clinical practice [24]. Reasons for insufficient BP control are diverse, lack of adherence and insufficient self-monitoring have been shown to play an important role on the patients’ side [25–29], reluctance to intensify therapy can be a reason in patients and physicians [24]. In addition, among GPs uncertainness and scepticism whether guideline recommendations are always adequate for the individual patient exist [30].
Guidelines promote an early dual combination treatment [11, 12]. We observed a gap between this guideline recommendation and practice, since about half of the patients under pharmacological treatment and uncontrolled AH received only a monotherapy.
Overall, the most commonly prescribed antihypertensive agents were ACEI followed by diuretics and ARB, BB and CCB. As stated in Guidelines for the Management of AH [11, 12], randomised trials comparing antihypertensive substances show that for similar BP reductions, differences in the incidence of cardiovascular morbidity and mortality between different drug classes are small, thus strengthening the conclusion that their benefit largely depends on BP lowering per se. Depending on co-morbidities, there is evidence in favour of certain drug classes versus others either as initial treatment or as part of a combination. Also side effects may influence the choice of therapy. Since co-morbidities and side effects were not recorded in our data, no statement can be made concerning the guideline conformity with respect to the chosen substances, particularly the high use of beta-blockers as monotherapy.
Our adjusted results estimated an average decrease in systolic BP due to an antihypertensive monotherapy compared to no treatment of 10.66 mm Hg (i.e. –15.58 mm Hg of the linear term plus 4.92 mm Hg of the quadratic term) and an average diastolic decrease of 6.46 mm Hg (i.e. –7.97 mm Hg plus 1.51 mm Hg) (table 3). These effects are comparable to randomised trials comparing antihypertensive agents with placebo [31].
We observed a non-linear (quadratic) association between BP measures and number of antihypertensive substances which was stronger for systolic BP. These findings reflect the diminishing efficacy of multiple combination therapy on BP control; the incremental effect of an antihypertensive monotherapy declines with every additional substance, a conclusion also recently drawn by Justin et al. [32].
Multimorbidity and polypharmacy is a common problem in PC associated with increased risk of interactions and side effects. In this setting “more is not always better” [33]. Therefore the important goal of good BP control has to consider not only the most adequate and evidence based treatment but also has to reflect the benefits and risks. In addition, as shown in our study and mentioned above, other factors for insufficient BP control as overweight and smoking are frequent concomitant problems. Multifaceted interventions, including modification of lifestyle, with smoking cessation and weight reduction, should be raised implicitly and offered to patients, especially to the ones already receiving a dual antihypertensive combination therapy. From the management of other chronic diseases in PC, such as diabetes, it is known that interventions with the greatest positive effect on outcomes include support in behaviour change [30, 34–37].
Certain limitations concerning the generalisability of our data have to be taken into account: Previous studies from the PC setting have shown that variations between GPs occur [38–40], meaning that patient observations are not independent, i.e. observations in one cluster tend to be more similar to each other than to individuals in the rest of the sample. In our study population no such expected cluster effect was observed, meaning that the variations in patient observations are not explained by the attending GP. This finding might indicate that our GP population represents a special selection. Even though we could not find a GP clustering effect on BP, such effects cannot always be ruled out with certainty. Participating GPs differed from Swiss GP population statistics, performed by the Swiss Medical Association [41], in the following points: More than half of the participating GPs worked in group practices, whereas usually this is the case in one third of Swiss GPs. The number of GPs with electronic patient records was also higher than average, with 36% compared to the reported data of 13% in Switzerland [42, 43]. Only GPs from three cantons of the German speaking part of Switzerland were recruited for participation and most participants were located in urban or suburban areas. For Swiss standards, the participating GPs treated a proportionally large amount of patients in managed care or HMO systems [44]. On the other hand the gender and age distribution compared well with the annual statistics on GPs [41]. The participating physicians also reflected the traditional characteristics of a Swiss GP, specialising in internal or general medicine without additional specialisation.
Each participating GP received along with the study folder a list and instructions to register all patients they asked to participate and all patients who declined to participate. However, this list was not completed by the majority of GPs and therefore could not be considered for analysis. No patients were excluded by the study investigators. The GPs were responsible for making sure that the inclusion and exclusion criteria were met, hence, correct inclusion and exclusion has to be trusted. Nevertheless, the low-threshold inclusion criteria were strengths because they offered a view on real life PC patients with AH and on the spectrum of treatment. On the other hand, certain clinical details which could influence the reason for uncontrolled AH, e.g., renal function, hyperaldosteronism, effect of BP-influencing medications such as NSAR are lacking. Since the current manuscript concentrates on the baseline-measurements only performed at the practices white coat hypertension in some cases cannot be excluded. Nevertheless, it seems justified to rely on the presumption that GPs know about white coat hypertension and took this consideration into account before including the patient into the study.
From our study data no statements on the prevalence of uncontrolled AH in Swiss PC can be derived. But considering the existing data on high prevalence of (uncontrolled) AH in Switzerland [6, 7] and worldwide [1], our findings are of importance.
Smoking and high BMI are strong and independent factors associated with higher BP levels in patients with uncontrolled AH. A high rate of monotherapy and a decrease in the incremental gain on BP control when more antihypertensive agents are used highlight the importance of adequate pharmacological treatment as well as risk factor control.
Acknowledgements:We are very grateful to Kaba Dalla Lana, Anke Schickel and Barbara Portmann for the administrative help and to the GPs who recruited and followed patients. We want to thank Christian Häuptle, MD, from Kantonsspital St. Gallen for the support in recruiting participating GPs.
1 Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43(1):10–7.
2 Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
3 Chobanian AV. Isolated systolic hypertension in the elderly. N Engl J Med. 2007;357(8):789–96.
4 Kannel WB. Risk stratification in hypertension: new insights from the Framingham study. Am J Hypertension. 2000;13(Supplement 1):S3–10.
5 Jones DW, Hall JE. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and evidence from new hypertension trials. Hypertension. 2004;43(1):1–3.
6 http://www.gesundheitsfoerderung.ch/pdf_doc_xls/d/betriebliche_gesundheitsfoerderung/allgemeines/SGB_2007.pdf
7 Danon-Hersch N, Marques-Vidal P, Bovet P, Chiolero A, Paccaud F, Pécoud A, et al. Prevalence, awareness, treatment and control of high blood pressure in a Swiss city general population: the CoLaus study. Eur J Cardiovasc Prev Rehabil. 2009;16(1):66–72.
8 Paulsen MS, Sondergaard J, Reuther L, Larsen PS, Munck AP, Larsen PV, et al. Treatment of hypertension in general practice: a cross-sectional study of 5413 hypertensive patients. Family Practice. 2011.
9 Van der Niepen P, Dupont AG. Improved blood pressure control in elderly hypertensive patients: results of the PAPY-65 Survey. Drugs Aging. 2010;27(7):573–88 510.2165/11537350-000000000-000000000.
10 Steurer-Stey C, Zoller M, Chmiel Moshinsky C, Senn O, Rosemann T. Does a colour-coded blood pressure diary improve blood pressure control for patients in general practice: the CoCo trial. Trials. 2010;11:38.
11 http://swisshypertension.ch/guidelines.htm
12 Mansia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 ESH-ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 2007;16(3):135–232.
13 Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25(6):1105–87.
14 Kannel WB, D’Agostino RB, Sullivan L, Wilson PWF. Concept and usefulness of cardiovascular risk profiles. Am Heart J. 2004;148(1):16–26.
15 Smulyan H, Safar ME. Blood pressure measurement: retrospective and prospective views. Am J Hypertens. 2011;24:628–34.
16 Jankowski P K-JK, Czarnecka D, Brzozowska-Kiszka M, Styczkiewicz K, Loster M, Kloch-Badelek M, et al. Pulsatile but not steady component of blood pressure predicts cardiovascular events in coronary patients. Hypertension. 2008;51:848–55.
17 Yoon C, Jung H, Kim Y. Evaluation of an incentive-based obesity management program in a workplace. Int J Occup Saf Ergon. 2011;17(2):147–54.
18 Pede S, Lombardo M. Cardiovascular risk stratification. Systolic, diastolic or pulse pressure? Ital Heart J Suppl. 2001;2(4):356–8.
19 Nichols WW. Clinical measurement of arterial stiffness obtained from noninvasive pressure waveforms. Am J Hypertens. 2005;18(1 Pt 2):3S–10S.
20 Franklin SS, Gustin Wt, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308–15.
21 Primatesta P, Falaschetti E, Gupta S, Marmot MG, Poulter NR. Association between smoking and blood pressure: evidence from the Health Survey for England. Hypertension. 2001;37(2):187–93.
22 Li H, Tong W, Wang A, Lin Z, Zhang Y. Effects of cigarette smoking on blood pressure stratified by BMI in Mongolian population, China. Blood Pressure. 2010;19(2):92–7.
23 Brenner R, Waeber B, Allemann Y. Medical treatment of hypertension in Switzerland. The 2009 Swiss Hypertension Survey (SWISSHYPE). Swiss Med Wkly. 2011;141:w13169.
24 Ferrari P, Hess L, Pechere-Bertschi A, Muggli F, Burnier M. Reasons for not intensifying antihypertensive treatment (RIAT): a primary care antihypertensive intervention study. J Hypertens. 2004;22(6):1221–9.
25 Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med. 2004;164(7):722–32.
26 De Geest S, Sabate E. Adherence to long-term therapies: evidence for action. Eur J Cardiovasc Nurs. 2003;2(4):323.
27 Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19(11):1190–6.
28 Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database of Systematic Reviews 2004(2):CD004804.
29 Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
30 Heisler M, Hogan MM, Hofer TP, Schmittdiel JA, Pladevall M, Kerr EA. When more is not better: treatment intensification among hypertensive patients with poor medication adherence. Circulation. 2008;117(22):2884–92.
31 Materson BJ, Reda DJ, Cushman WC, Massie BM, Freis ED, Kochar MS, et al. Single-drug therapy for hypertension in men – a comparison of six antihypertensive agents with placebo. N Engl J Med. 1993;328(13):914–21.
32 Timbie JW, Hayward RA, Vijan S. Diminishing efficacy of combination therapy, response-heterogeneity, and treatment intolerance limit the attainability of tight risk factor control in patients with diabetes. Health Services Research. 2010;45(2):437–56.
33 Cushman WC, Evans GW, Byington RP, Goff DC, Jr., Grimm RH, Jr., Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–85.
34 Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT, Assendelft WJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001;24(10):1821–33.
35 Houston Miller N, Hill M, Kottke T, Ockene IS. The multilevel compliance challenge: eecommendations for a call to action: a statement for healthcare professionals. Circulation. 1997;95(4):1085–90.
36 Qureshi NN, Hatcher J, Chaturvedi N, Jafar TH. Effect of general practitioner education on adherence to antihypertensive drugs: cluster randomised controlled trial. BMJ. 2007;335(7628):1030.
37 Verberk WJ, Kroon AA, Kessels AGH, de Leeuw PW. Home blood pressure measurement: a systematic review. J Am Coll Cardiol. 2005;46(5):743–51.
38 Weiner JP, Parente ST, Garnick DW, Fowles J, Lawthers AG, Palmer RH. Variation in office-based quality. JAMA: The Journal of the American Medical Association 1995;273(19):1503–8.
39 Krein SL, Hofer TP, Kerr EA, Hayward RA. Whom should we profile? Examining diabetes care practice variation among primary care providers, provider groups, and health care facilities. Health Services Research. 2002;37(5):1159–80.
40 Greenfield S, Kaplan SH, Kahn R, Ninomiya J, Griffith JL. Profiling care provided by different groups of physicians: effects of patient case-mix (bias) and physician-level clustering on quality assessment results. Ann Intern Med. 2002;136(2):111–21.
41 http://www.fmh.ch/themen/aerztedemographie/aerztestatistik.html
42 Rosemann T, Marty F, Bhend H, Wagner J, Brunner L, Zoller M. Utilisation of information technologies in ambulatory care in Switzerland. Swiss Med Wkly. 2010;140:w13088.
43 Chmiel C, Bhend H, Senn O, Zoller M, Rosemann T. The FIRE project: a milestone for research in primary care in Switzerland. Swiss Med Wkly. 2011;140:w13142.
44 http://www.santesuisse.ch/de/dyn_output_graphic_detail.html?content.cdid=12309&navid=416
Funding / potential competing interests: The study is funded by the Swiss academy of medical sciences (approved on 30 April 2011) and Uniscientia Stiftung, Vaduz. Blood pressure measurement devices at reduced price were provided by Melectronics, Switzerland. Funding sources had no influence on study design; on the collection, analysis, and interpretation of data; on the writing of the manuscript; or on the decision to submit the manuscript for publication. No other potential conflict of interest relevant to this article was reported.
Authors’ Contribution:C. Chmiel was a study investigator and wrote the drafts of the manuscript. C. Chmiel and O. Senn performed statistical analysis and interpreted data. C. Steurer-Stey and O. Senn were study investigators and substantially contributed to and reviewed the drafts of the manuscript. C. Steurer-Stey, M. Zoller, O. Senn, T. Rosemann developed the study protocol and were study investigators. C. Chmiel, V. Del Prete and M. Wang were responsible for data collection. All authors reviewed drafts of the manuscript, read and approved the final manuscript.