DOI: https://doi.org/10.4414/smw.2012.13697
Bacterial meningitis is a rare complication of trans-sphenoidal surgery [1]. The present paper reports a case of postoperative pneumococcal meningitis with fatal cerebral vasculitis.
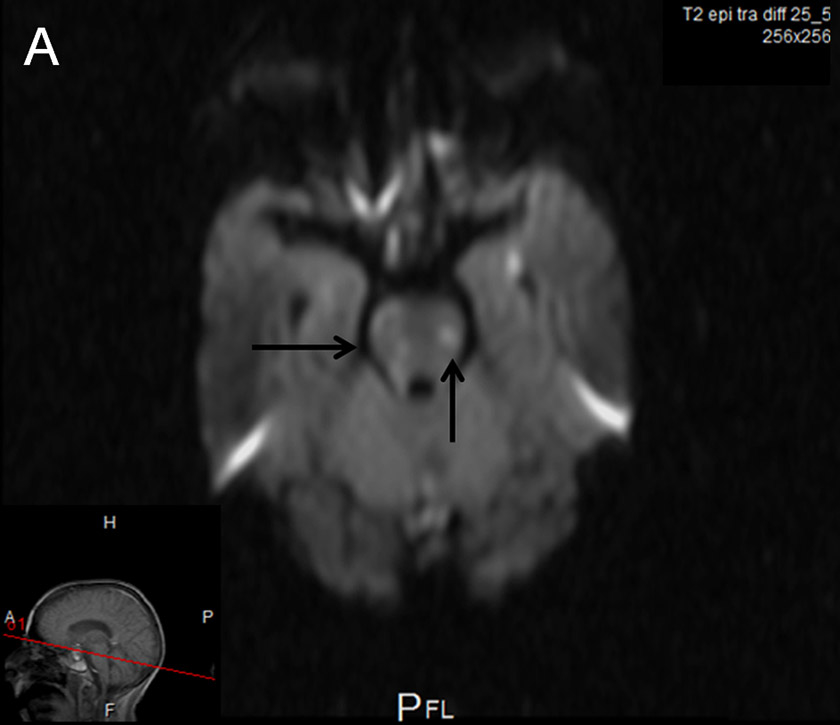
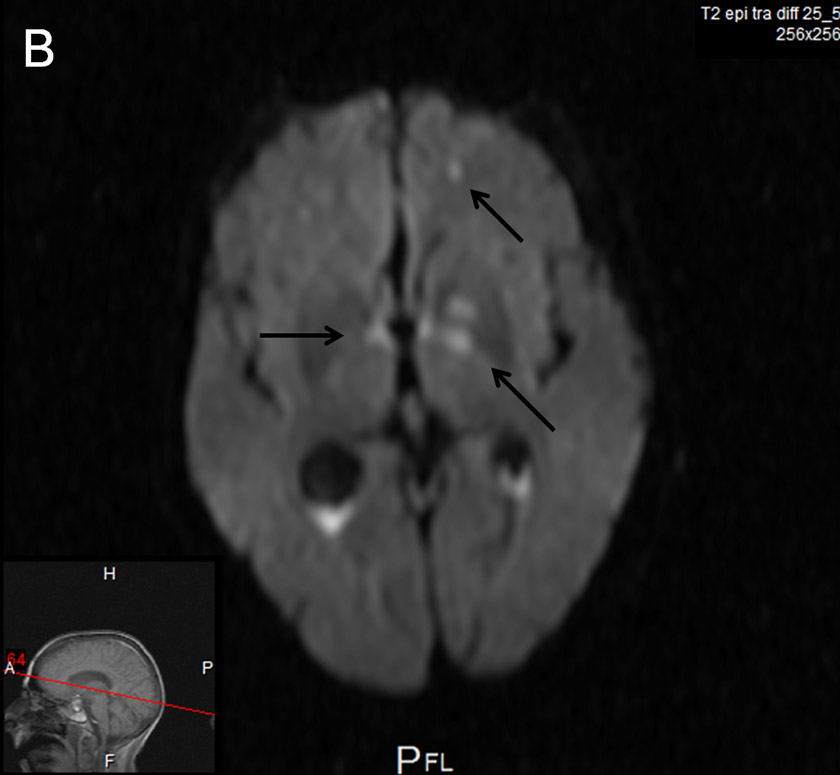
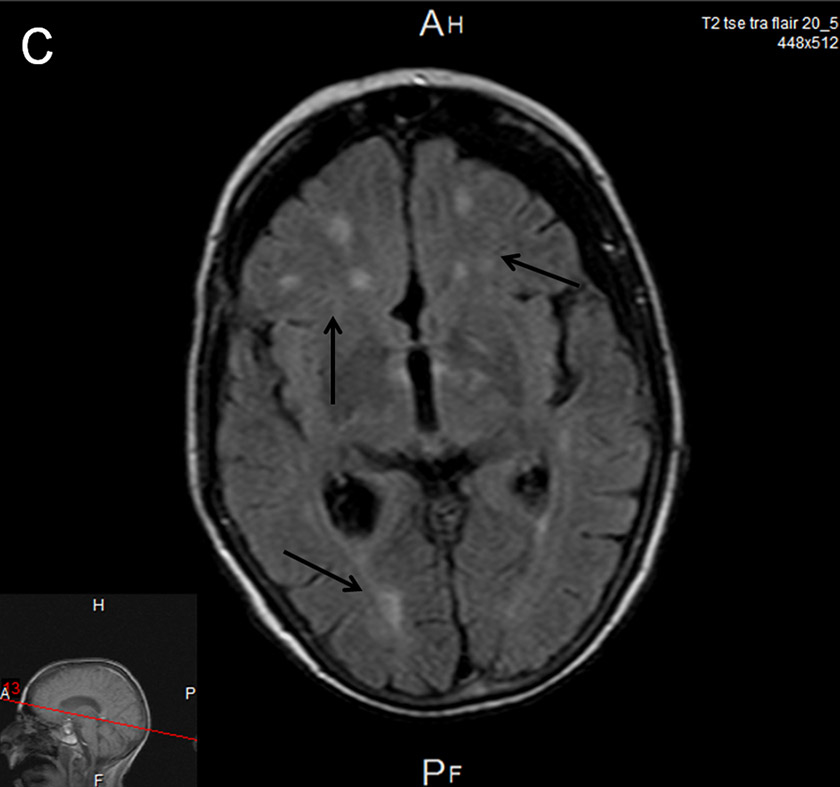
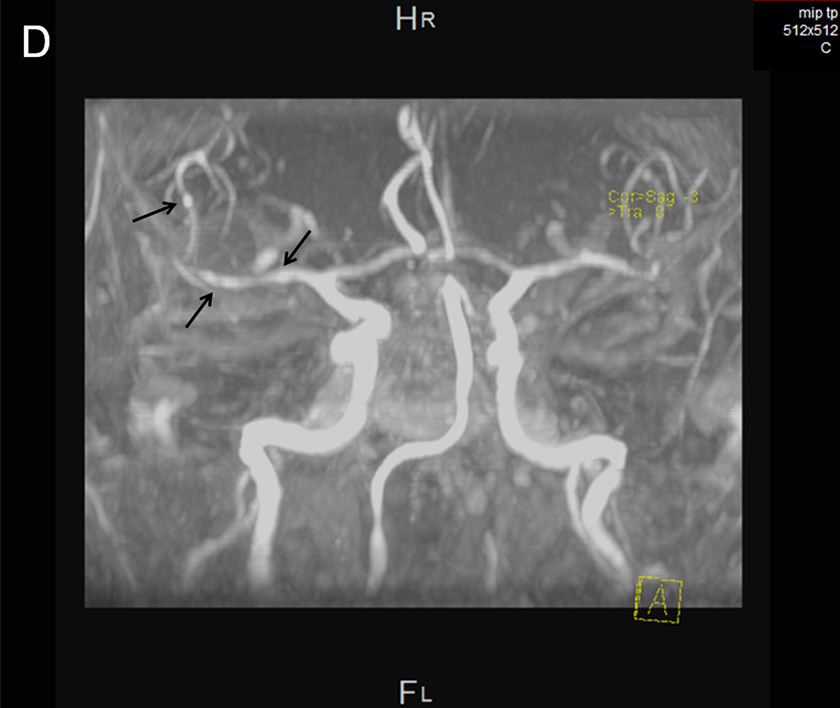
Figure 1
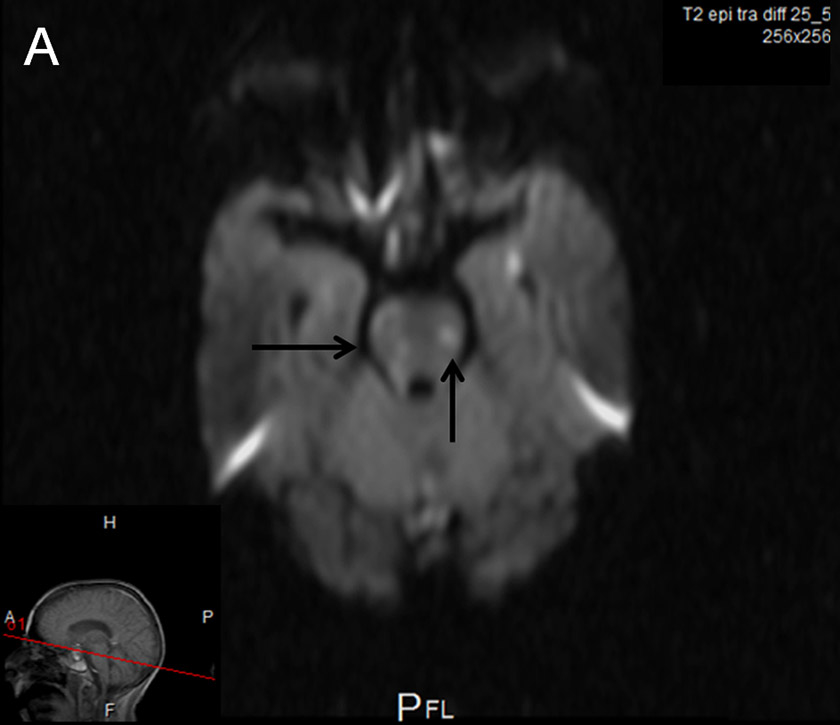
Cerebral MRI.
A, B Axial diffusion-weighted images: Areas of ischaemic necrosis in the pons (A), and thalami and basal ganglia bilaterally (B).
C Axial FLAIR image: Areas of ischaemia in the subcortical anterior and posterior territories.
D MR angiography: Arrows highlight arterial irregularities suggestive of vasculitis.
A 79-year-old woman underwent elective trans-nasal trans-sphenoidal resection of a pituitary macro-adenoma, having been placed on oral hydrocortisone replacement therapy. At induction she received 1 g amoxicillin and 200 mg clavulanic acid (Augmentin® 1.2 g) and hydrocortisone 100 mg intravenously (IV). Surgery was complicated by a small arachnoid leak which was closed immediately.
24 hours later the patient complained of headache, became drowsy and displayed signs of meningism. Cerebral CT showed no bleeding or meningeal enhancement. CSF examination revealed 512 white cells/mm3 (99% neutrophils), moderate Gram positive cocci and sparse Gram negative rods; glucose <0.1 mmol/l, protein 14,860 mg/l (reference values 150–460 mg/l) and lactate 22.86 mmol/l. Ceftazidime 3 × 2 g and vancomycin 2 × 1 g IV were commenced empirically; 4 hours later dexamethasone 3 × 8 mg IV was added. Pure growth of S. pneumoniae serotype 15 was isolated from CSF and blood cultures. Antibiotic treatment was changed to ceftriaxone 2 × 2 g IV. By day 4 of treatment the patient’s consciousness level had improved and dexamethasone was reduced to hydrocortisone 1 × 25 mg as maintenance therapy.
Two days later the patient became drowsy again with signs of upper brainstem dysfunction. Cerebral MRI showed meningeal enhancement and widespread punctate ischaemic-type lesions affecting vascular beds of both carotid and vertebral arteries bilaterally (fig. 1 A–C). MR angiography showed numerous irregularities of the distal arteries, suggestive of vasculitis (fig. 1D). Antibiotic treatment was broadened to include meropenem 3 × 2 g and dexamethasone was restarted but brainstem dysfunction did not improve. Supportive treatment was withdrawn and the patient died on day 21 post-surgery. Subsequent CSF cultures were sterile.
This 2-phase pattern of pneumococcal meningitis – initial improvement followed by subsequent neurological deterioration – has been described in community-acquired pneumococcal meningitis associated with both cerebral vasculitis and cerebral thrombosis [2]. Such vascular phenomena may represent an inflammatory continuum rather than distinct para-infectious processes.
Inflammation has an important role in the pathogenesis of pneumococcal meningitis. Upon antibiotic treatment, bacterial lysis products are released which trigger the host inflammatory response, enhancing bacterial killing but also risking host cell damage. The suppressive effect of corticosteroids in this context resulted in their inclusion as adjunctive therapy in pneumococcal meningitis [3]. However, steroids possess a subtle biphasic effect both suppressing and stimulating inflammation, as illustrated in human endotoxaemia models [4].
In our patient the probable mode of infection was direct bacterial inoculation from colonised nasal mucosa into the subarachnoid space during surgery. This inoculum probably induced a strong localised inflammatory response which was augmented by antibiotic-mediated bacterial lysis. According to the model of Yaeger et al. [4], this inflammatory response may have been exaggerated by the induction dose of hydrocortisone, resulting in local vasculitis. It is possible in this context that delaying immunosuppresive dexamethasone treatment in our patient influenced the outcome negatively, particularly as immediate high dose steroids have been recommended in cerebral vasculitis and if delayed cerebral thrombosis is suspected [2]. That said, the patient may have survived had the lesions not involved the brainstem; the cerebral hemisphere lesions, whilst numerous, were arguably of insufficient size to cause the profound neurological deficits observed clinically.
Whilst our case is unusual, the surgery we describe is not. There are several learning points. First, preoperative antibiotic prophylaxis should perhaps be prolonged in cases involving long surgical interventions or CSF leak. In our centre prolonged antibiotic prophylaxis has been observed to be of benefit (Giulieri et al., manuscript in preparation). It is noteworthy, however, that precise recommendations are lacking with regard to the duration of antibiotic prophylaxis in uncomplicated surgery, and data regarding complicated surgery are even sparser. Second, if postoperative pneumococcal meningitis occurs, particularly in patients on corticosteroid replacement therapy, steroid and antibiotic treatment should be given simultaneously and, in severe disease, steroids should perhaps be prolonged. Our case raises questions as to whether a ‘one size fits all’ antibiotic prophylaxis should be replaced by one tailored to patient group and intra-operative factors. Finally, our report is a reminder that, even with prompt antibiotic treatment, pneumococcal meningitis carries significant mortality.
Acknowledgement:We thank Bulent Bakar, MD, Department of Neurosurgery, Kirikkale University Faculty of Medicine, Kirikkale, Turkey, for information on his own case of postoperative meningitis.
1 McClelland S, 3rd, Hall WA. Postoperative central nervous system infection: incidence and associated factors in 2111 neurosurgical procedures. Clin Infect Dis. 2007;45(1):55–9.
2 Schut ES, Brouwer MC, de Gans J, Florquin S, Troost D, van de Beek D. Delayed cerebral thrombosis after initial good recovery from pneumococcal meningitis. Neurology. 2009;73(23):1988–95.
3 van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med. 2004;351(18):1849–59.
4 Yeager MP, Rassias AJ, Pioli PA, Beach ML, Wardwell K, Collins JE, et al. Pretreatment with stress cortisol enhances the human systemic inflammatory response to bacterial endotoxin. Crit Care Med. 2009;37(10):2727–32.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.
Authors’ contribution: K. E. A. Darling and J. Niederhauser contributed equally to this paper.