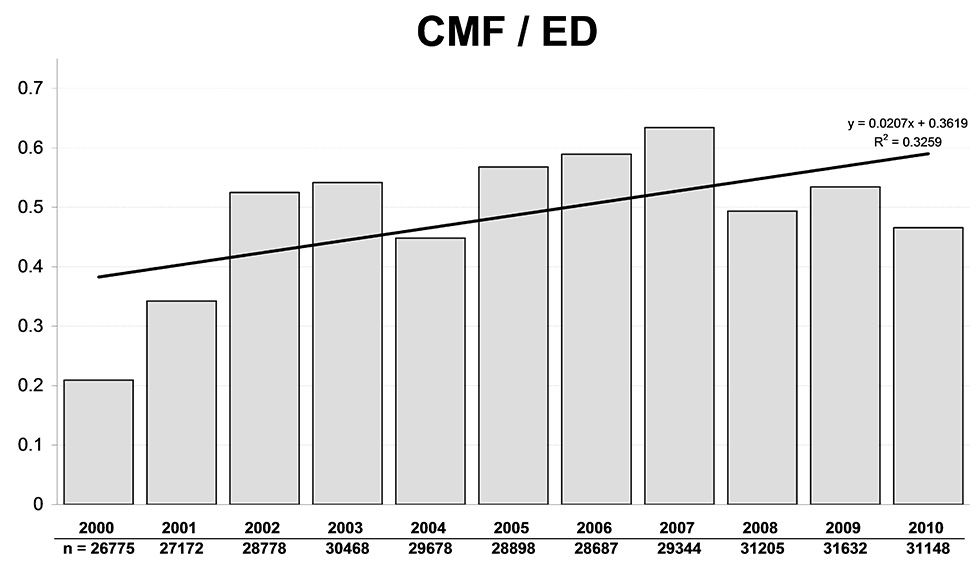
Figure 1
CMF injuries as a percentage of all ED visits.
DOI: https://doi.org/10.4414/smw.2012.13687
Data from a Swiss university hospital
Interpersonal violence comprises family and community violence [1, 2] and involves the same classic risk factors as those applicable to a multitude of public health problems, namely socioeconomic factors, including problems with inequality and clashes between different cultures [1]. Victims of interpersonal violence frequently suffer head and face injuries, and it has been shown that the severity and number of major head injuries increased in the early 2000s [3]. Fatal outcome rates (i.e. mortality rates) are readily available for high-income countries [4, 5], but reliable data on non-fatal outcomes of interpersonal violence are scarce worldwide and researchers have largely to rely on estimates [1, 3, 4, 6–9]. It is estimated that interpersonal violence is responsible for 0.2% of disability-adjusted life years (DALYs) overall, ranking 53rd of all causes and rising to 2.5% of total DALYs and 4.3% to total mortality in men aged between 15 and 44 years in high-income European countries [1, 4]. As the consequences of interpersonal violence predominantly concern young people, they may have a much higher economic impact than can be gleaned from mortality rates or DALYs alone (e.g. high opportunity costs, a lifetime of psychological distress/disability) [10]. The effective economic impact of violence in Switzerland is virtually unknown: Miller et al. estimated the total costs of violence for the United States in 2001 at US$ 329.8 billion, and thus 3.3% of US gross domestic product [11]. A study for England and Wales estimated the total costs as US$ 40.2 billion in 2000 or US$ 773 per capita [12]. Extrapolated to the Swiss population in 2000, this would correspond to annual costs of violence for Switzerland of US$ 5.4 billion. Regarding head injuries, recent research has chiefly focused on facial trauma alone or has included only certain types of injury [13–15]. The purpose of the present study was to describe the epidemiological features of cranio-maxillofacial (CMF) injuries due to interpersonal violence as recorded in patients at the emergency department (ED) of Bern University Hospital, based on outlines of their injury patterns.
The study was conducted in an inner city ED with approximately 30,000 annual visits. The ED at Bern University Hospital is the only Level 1 accident and emergency unit in a rural catchment area with a population of nearly 1 million providing service for all insurance classes with 24-hour coverage. During the study period the size of the population of the city and canton of Bern slightly increased (3.9% and 3.8% respectively; see supplementary online table 1), and a centrally located ED opened in the inner city, but without closure of nearby hospital services providing care for patients with CMF injuries. Two authors (APB, JK) performed a retrospective analysis of data prospectively collected during an 11-year period between 1 January 2000 and 31 December 2010, using our SAP patient database, in which all ED visits are registered and which is accessible by classified key word search, as described previously [3]. The study was approved by the institutional review board and data were collected, stored, analysed and shared in strict adherence to the ethics committee standards of Inselspital Bern. Patients with the key words “Schlägerei” (brawl), “Gewalt” (violence), “Messerstecherei” (stabbing), “Schiesserei” (shootout), and “häusliche Gewalt” (domestic violence) were included (n = 1,585). We compared two time periods, viz. 2000–2004 versus 2005–2010. Baseline demographic data and the following clinical data were extracted: type and location of cranio-maxillofacial injuries (table 1), cause of injury/instruments used, use of alcohol and drugs and concomitant injuries due to direct violence against the respective body part. We included only the most dangerous instruments used against the head. Generic entries (e.g. “fight”) were classified as “body parts”.
In the case of a soft tissue injury above a fracture, an entry was made only for the more severe injury. Multiple entries for one structure were made if multiple unrelated injuries to that structure had occurred (e.g. multiple non-communicating orbital fractures). Communicating injuries (e.g. fractures of the zygoma involving the maxillary sinus) were considered a single injury. For anatomical definitions see supplementary online table 2. Cranial injuries were subdivided into severe and mild injuries (table 1).
Rates and median values were tested for changes over time using the Cochran-Armitage trend test. Levels of statistical significance were defined as p <0.05. All tests were two-sided. The statistical analyses were performed with SAS version 9.0 (SAS Institute Inc. Heidelberg, Germany).
| Table 1: Type and location of cranial and maxillofacial injuries. | ||||
| Category | Components | Category | Components | |
| Region of maxillofacial injury* | Cheek Chin Ear Eye Eyeball Eyelid Face (unspecified) Infraorbital Le Fort I Le Fort II Le Fort II-III Le Fort III Lip Mandible Maxilla Maxillary sinus Mouth Nasal bone Nasal bone/septum Nose Orbit Orbit/maxillary sinus Periorbital Supraorbital Zygoma Zygoma/maxillary sinus Zygoma/orbit | Types of maxillofacial injury | Abrasion Contusion Contusio bulbi Bite Dentoalveolar damage Erythema by irritant gas Fracture Laceration | |
| Type of cranial injury | Mild | Abrasion Mild traumatic brain injury Erythema by irritant gas Extracranial contusion Injury of auditory meatus Laceration Perforation of tympanic membrane | ||
| Severe | Basal skull fracture Basal skull fracture / pneumocranium Contusio labyrinthi Intermediate traumatic brain injury Intracranial haemorrhage Skull fracture Skull fracture/pneumocranium Severe traumatic brain injury | |||
| Region of concomitant injury | Left lower extremity Left upper extremity Neck Right lower extremity Right upper extremity Trunk | Instrument used against head | Blunt object Body part Irritant gas Sharp object** | |
| * Middle, right or left added where applicable. ** e.g. knives, broken bottles, glass shards. | ||||
| Table 2: Age distribution. | |||||||
| All patients | Males | Females | Ratio M:F | ||||
| N | % of referrals | N | % of males | N | % of females | ||
| Age group <18 | 68 | 4.3 | 63 | 4.3 | 5 | 4.5 | 12.6:1 |
| Age group 18–25 | 715 | 45.1 | 669 | 45.4 | 46 | 41.1 | 14.5:1 |
| Age group 26–35 | 446 | 28.1 | 420 | 28.5 | 26 | 23.2 | 16.2:1 |
| Age group 36–45 | 240 | 15.1 | 219 | 14.9 | 21 | 18.8 | 10.4:1 |
| Age group >45 | 116 | 7.3 | 102 | 6.9 | 14 | 12.5 | 7.3:1 |
| Total | 1,585 | 100.0 | 1,473 | 100.0 | 112 | 100.0 | 13.2:1 |
For the 11-year study period, 1,585 patient referrals to the ED were enrolled in the study. The median age at the time of admission was 26 (range 12–82) years, with 116 (7.3%) patients >45 years (table 2); 1473 (92.9%) were males, 191 (12.1%) were students/trainees and 1,025 (64.7%) were Swiss citizens. Overall, 943 (59.5%) of referrals occurred at weekends. Over time, the frequency of CMF injuries and maxillofacial injuries as a percentage of all ED visits significantly increased from 0.21% to 0.47% (p trend <0.001; see fig. 1;) and from 0.34% to 0.68% (p trend <0.001) respectively.
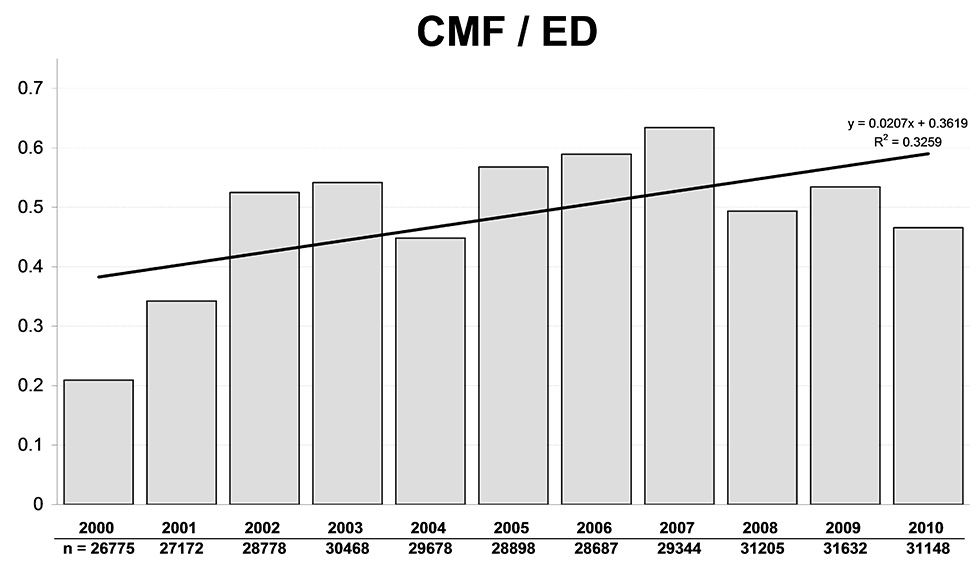
Figure 1
CMF injuries as a percentage of all ED visits.
The most frequently used instruments were parts of the attacker’s body, accounting for 1,396/1,646 (83.4%) of instruments, followed by blunt objects (210/1646; 12.8%), sharp objects (29/1,646; 1.8%) and irritant gas (11/1646; 0.7%). Over time, parts of the attacker’s body were used significantly more frequently as instruments as a percentage of all instruments used in CMF (2000: 78.9%, 2010: 88.9%; p trend = 0.009).
A total of 736 patients with injuries to the neurocranium (273 patients with isolated neurocranial and 463 with combined neurocranial and maxillofacial injuries) and 849 patients with isolated maxillofacial injuries were referred, including 72/736 (9.8%) patients with severe cranial injuries. In all, 816/2,305 (35.4%) maxillofacial injuries were located in the middle, 861/2,305 (37.4%) on the left side and 584/2,305 (25.3%) on the right side of the face (44 not specified). Concomitant injuries were registered in 572/1,585 (36.1%) patients and 645/1,585 (40.7%) were under the influence of drugs or alcohol when sustaining their CMF injury. In all, 28/1,585 (1.8%) were referred due to domestic violence; 25/28 were females, even though females accounted for only 112/1,585 (7.1%) patients.
There were several statistically significant changes from the first (2000–2004) to the second time period (2005–2010): the ratio of weekend: working day referrals increased from 0.81–1.1 to 1.5–2.3 (p <0.001); the numbers of patients with injuries of the neurocranium increased from 268/598 (44.8%) to 468/987 (47.7%) (p <0.001) and the annual average of 4.2 referrals per year with severe cranial injuries doubled to 8.5 (p = 0.010); the average of 163.6 maxillofacial injuries per year rose to 247.8 per year (p <0.001) and the number of maxillofacial injuries per patient rose from 1.37 to 1.51 from the first to the second period (p = 0.015). The proportion of patients who had consumed alcohol or other drugs increased from 213/598 (35.6%) to 432/987 (43.7%) (p = 0.001).
Most of the patients referred to the ED with violence-related CMF injury were young males. The absolute number of injuries, the number of injuries per patient and the severity of head injuries increased over time. Neurocranial injuries were more severe and slightly more frequent; severe neurocranial injuries occurred twice as frequently in the later period.
Young males are known to be frequent victims and perpetrators of interpersonal violence, and the 15- to 44-year group is greatly overrepresented [1, 3, 4, 16]. Previous work including all types of interpersonal violence-related injuries showed a male-to-female ratio of 8.4:1 [3] versus 13.2:1 in the present investigation; males were more prone to suffer CMF injuries requiring medical attention in fights than are females. Males appear to be injured by more dangerous mechanisms, being more frequently injured with objects than are females [13]. In this study females are more common among older patients and the majority of victims of domestic interpersonal violence are women.
As previously shown, an increasing number of referrals occurred at weekends [3, 7]. Consumption of alcohol and other drugs is recognised as an independent risk factor for violent behaviour [1, 16]. The proportion of patients found to have consumed alcohol or other drugs was lower than in previous work on patients with facial fractures from interpersonal violence [15].
As shown by others, many risk factors and protection factors for interpersonal violence are similar to other forms of externalised problem behaviour (e.g. delinquency, substance abuse). Thus prevention of interpersonal violence should be part of general health promotion, with analogue goals for prevention of substance abuse and promotion of mental and physical health (e.g. promotion of individual, family and community connectedness) [17, 18].
Comparison of the 2000–2004 and 2005–2010 periods showed that the number of patients under drugs at the time of injury has increased. This may be due to two factors: on the one hand, the alcohol consumption of the Swiss population in general and of adolescents in particular has increased in recent years; and at risk drinking has been occurring more frequently, especially at weekends [5, 19]. On the other hand, the ED staff’s sensitivity to youthful alcohol consumption may have increased, resulting in more diligent recording of such findings.
The trend towards more severe head injuries seems to be continuing [3]. Although these numbers may seem relatively small, such injuries cause not only a huge loss of quality of life for the patient but also major medical and indirect costs [19]. The left side of the face has previously been found to be injured more often than the right side in cases of interpersonal violence, as around 95% of the population are right-hand dominant and the opponent’s left side is thus more accessible [13].
This investigation suffers from the limitations inherent in all retrospective studies, being reliant on data not specifically tailored towards its needs, while underreporting or misreporting may be possible. Additionally, patients were already pre-selected by the act of referral to a university hospital ED, as opposed to having sought assistance in one of the smaller EDs in Bern, in their general practitioner’s office or not at all.
Interpersonal violence is a global public health problem, and although violence-related head injuries are still less common in Switzerland than in other high-income countries, they appear to be increasing in number and severity. In order to clarify their full national impact, further research in other Swiss centres is necessary. Cranial and maxillofacial injuries chiefly affect young adults and thus impose a major economic burden on society. There are possible synergies for the implementation of violence prevention strategies along with other prevention objectives (e.g. for delinquency, substance abuse) in every age group and intervention area.
| Supplementary table 1: Size of population in the catchment area*. | |||
| Catchment area | Year | Size of Population | Change |
| Nearer area: city of Bern | 2000 | 126,752 | +3.9% |
| 2010 | 131,702 | ||
| Wider area: canton of Bern | 2000 | 943,735 | +3.8% |
| 2010 | 979,435 | ||
| *Reference: http://www.vol.be.ch | |||
| Supplementary table 2: Anatomical definitions. | |
| Anatomical structure | Definition |
| Maxillofacial region | Vertically: extending from the inferior limit of the mandible to the superior rim of the orbit. |
| Horizontally: including all structures anterior to the dorsal rim of the auricle, except the external auditory meatus. | |
| Superior part of the orbit | Although the superior part of the orbit is formed by the frontal bone, this was allocated to the face. |
| Cranial region | Superior to a line from above the orbits to the superior rim of the auricles. Injuries below that line were considered to be maxillofacial injuries frontally and to be neck injuries retroauricularly. |
| Retroauricularly all structures between the inferior border of the earlobe (e.g., mastoid). | |
Acknowledgments: The authors thank Sabina Utiger, Inselspital Bern, Switzerland for her administrative help and Mr Rodney Yeates for language editing.
Authors’ contributions: Study concept and design: Businger, Krebs, Exadaktylos; Acquisition of data: Businger, Krebs; Analysis and interpretation of data: Krebs, Businger; Drafting of manuscript: Businger, Krebs, Exadaktylos; Critical revision of the manuscript for important intellectual content: Businger, Krebs, Schaller, Zimmermann, Exadaktylos; Administrative, technical and material support: Exadaktylos; Study supervision: Exadaktylos; Dr Exadaktylos had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
1 Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. The World Report on Violence and Health. Geneva: World Health Organization; 2002.
2 Waters H, Hyder A, Rajkotia Y, Basu S, Rehwinkel JA, Butchart A. The Economic Dimensions of Interpersonal Violence. Geneva: World Health Organization; 2004.
3 Exadaktylos AK, Häuselmann S, Zimmermann H. Are times getting tougher? A six year survey of urban violence-related injuries in a Swiss university hospital. Swiss Med Wkly. 2007;137:525–30.
4 Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global Burden of Disease and Risk Factors. Washington (DC): World Bank; 2006.
5 Statistisches Lexikon der Schweiz. Swiss Federal Statistical Office; [cited 2012 28 August]; Available from: http://www.bfs.admin.ch.
6 Waters HR, Hyder AA, Rajkotia Y, Basu S, Butchart A. The costs of interpersonal violence – an international review. Health Policy. 2005;73:303–15.
7 Exadaktylos A, Jonas C, Eggli S, Kohler HP, Zimmermann H. Violence in Bern. Swiss Med Wkly. 2001;131:527.
8 Exadaktylos AK, Evangelisti A, Anghern F, Keller U, Dopke K, Ringger A, et al. Measuring attitudes, behaviours, and influences in inner city victims of interpersonal violence (VIVs) – a Swiss emergency room pilot study. J Trauma Manag Outcomes. 2010;4:8.
9 Schreyer N, Carron PN, Demartines N, Yersin B. Stab wounds in a Swiss emergency department: a series of 80 consecutive cases. Swiss Med Wkly. 2010;140:w13058.
10 Rosenberg ML, Butchart A, Mercy J, Narasimhan V, Waters H, Marshall MS. Interpersonal Violence. In: Jamison D, Breman J, Measham A, editors. Disease Control Priorities in Developing Countries. 2nd ed. Washington (DC): World Bank; 2006.
11 Miller TR, Fisher DA, Cohen MA. Costs of juvenile violence: policy implications. Pediatrics. 2001;107:1–7.
12 Brand S, Price R. The economic and social costs of crime. 2000 [cited 2012 28 August]; Available from: http://webarchive.nationalarchives.gov.uk/20110218135832/rds.homeoffice.gov.uk/rds/pdfs/hors217.pdf
13 Eggensperger N, Smolka K, Scheidegger B, Zimmermann H, Iizuka T. A 3-year survey of assault-related maxillofacial fractures in central Switzerland. J CranioMaxillofac Surg. 2007;35(3):161–7.
14 Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J CranioMaxillofac Surg. 2003;31:51–61.
15 Lee KH. Interpersonal violence and facial fractures. J Oral Maxillofac Surg. 2009;67:1878–83.
16 Baier D, Pfeiffer C, Simonson J, Rabold S. Jugendliche in Deutschland als Opfer und Täter von Gewalt. Hannover: Kriminologisches Forschungsinstitut Niedersachsen; 2009.
17 Hahn R, Fuqua-Whitley D, Wethington H, Lowy J, Crosby A, Fullilove M, et al.; Task Force on Community Preventive Services. Effectiveness of universal school-based programs to prevent violent and aggressive behaviour: a systematic review. Am J Prev Med. 2007;33(2 Suppl):S114–29.
18 Prevention of youth violence [cited 2012 28 August]; http://www.ekm.admin.ch/de/dokumentation/doku/mat_jugendgewalt_d.pdf
19 Alcohol consumption and its resulting costs. Bern: Swiss Alcohol Board; [cited 2012 28 August]; Available from: http://www.eav.admin.ch/themen/00593/00597/index.html?lang=en.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.